INFECTIOUS DISEASE Copyright © 2019 Metal-captured ...Christopher Swale1, Alexandre Bougdour1,...
Transcript of INFECTIOUS DISEASE Copyright © 2019 Metal-captured ...Christopher Swale1, Alexandre Bougdour1,...
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
1 of 11
I N F E C T I O U S D I S E A S E
Metal-captured inhibition of pre-mRNA processing activity by CPSF3 controls Cryptosporidium infectionChristopher Swale1, Alexandre Bougdour1, Audrey Gnahoui-David2, Julie Tottey2, Sonia Georgeault3, Fabrice Laurent2*, Andrés Palencia1,4*†, Mohamed-Ali Hakimi1*†
Cryptosporidium is an intestinal pathogen that causes severe but self-limiting diarrhea in healthy humans, yet it can turn into a life-threatening, unrelenting infection in immunocompromised patients and young children. Severe diarrhea is recognized as the leading cause of mortality for children below 5 years of age in developing countries. The only approved treatment against cryptosporidiosis, nitazoxanide, has limited efficacy in the most vulnerable patient populations, including malnourished children, and is ineffective in immunocompromised individuals. Here, we investigate inhibition of the parasitic cleavage and polyadenylation specificity factor 3 (CPSF3) as a strategy to control Cryptosporidium infection. We show that the oxaborole AN3661 selectively blocked Cryptosporidium growth in human HCT-8 cells, and oral treatment with AN3661 reduced intestinal parasite burden in both immuno-compromised and neonatal mouse models of infection with greater efficacy than nitazoxanide. Furthermore, we present crystal structures of recombinantly produced Cryptosporidium CPSF3, revealing a mechanism of action whereby the mRNA processing activity of this enzyme is efficiently blocked by the binding of the oxaborole group at the metal-dependent catalytic center. Our data provide insights that may help accelerate the development of next-generation anti-Cryptosporidium therapeutics.
INTRODUCTIONCaused by the protozoan Apicomplexa parasite Cryptosporidium, cryptosporidiosis is a widespread water-borne infection in humans and animals that poses important public health problems (1–5). Once ingested, Cryptosporidium parvum oocysts excyst in the gastro-intestinal tract, releasing infective sporozoites that invade intestinal epithelial cells and mature into trophozoites, which progress through asexual replication to form type 1 meronts (fig. S1A). These mero-zoites infect new epithelial cells and undergo a second asexual cycle of replication before committing their sexual cycle that will end up with the production of a high number of infectious oocysts released in the feces. In their oocyst form, the most relevant species to humans, C. parvum (Cp) and Cryptosporidium hominis (Ch), are extremely resist-ant to chlorine-based water disinfectants, and there are currently no vaccines available against these parasites. The standard-of-care nitazoxanide (NTZ) has limited efficacy in high-risk groups, most notably in HIV-positive immunocompromised patients, immuno-suppressed patients, and young infants, where the disease can de-velop into chronic and life-threatening diarrhea. This lack in therapeutic options underlines the need for new classes of drugs to treat this infection as well as the discovery and validation of Cryptosporidium protein targets (6–8).
Benzoxaboroles are boron-containing compounds that have potent and broad-spectrum antimicrobial activity (9). AN3661 and the other 6- or 7-derivatized benzoxaboroles were previously shown to inhibit
apicomplexan parasite growth by targeting the parasitic enzyme cleavage and polyadenylation specificity factor 3 (CPSF3) (10, 11). Mutagenesis and forward genetic studies using AN3661 revealed that single amino acid variants within parasitic CPSF3 (some of them redundant to both species) enabled Toxoplasma gondii and Plasmodium falciparum parasites to resist the AN3661 treatment. The human homolog of CPSF3 (also known as CPSF73) associates with the multisubunit cleavage and polyadenylation complex and was shown to be the endonuclease responsible for cleavage before polyadenylation of nascent pre-mRNAs (12, 13). Other groups found that CPSF3 is also likely the putative target of benzoxaboroles in trypanosomatid parasites (14, 15). However, the molecular basis of the inhibition mechanism of CPSF3 in all these pathogens remains unknown. In this work, we evaluate the efficacy of AN3661 against Cryptosporidium and use an integrated structural biology approach to understand the molecular details of the CPSF3 inhibition mech-anism and its selectivity to parasitic CPSF3.
RESULTSIn vitro activity of AN3661 and selectivity toward Cryptosporidium strainsWe evaluated AN3661 (Fig. 1A) for its effectiveness against C. parvum growth after infection of intestinal cells. To this end, we generated two C. parvum strains (INRA and IOWA strains) expressing Nluc that exhibited different growth rates in vitro in intestinal epithelial cells (fig. S1B). We compared the ability of AN3661 to inhibit the fast-growing C. parvum INRA strain in human ileocecal HCT-8 cells to the clinical compound NTZ, as well as KDU691, a specific inhibitor of phosphatidylinositol 4-kinase (16, 17) that represents the most potent anti-Cryptosporidium molecule to date. The half-maximal effective concentration (EC50) of AN3661 at 24 hours postinfection (pi) was similar to that of KDU691 (0.08 and 0.06 M, respectively), and both compounds were more efficient than NTZ (EC50, 2.55 M) (Fig. 1B). In addition, AN3661 consistently conferred superior inhibition
1Institute for Advanced Biosciences (IAB), Host-Pathogen Interactions and Immunity to Infection, INSERM U1209, CNRS UMR 5309, University Grenoble Alpes, 38000 Grenoble, France. 2INRA, Université François Rabelais de Tours, Centre Val de Loire, UMR1282 ISP, Laboratoire Apicomplexes et Immunité Mucosale, 37380 Nouzilly, France. 3Plateforme des Microscopies, Université et CHRU de Tours, 37000 Tours, France. 4Institute for Advanced Biosciences (IAB), Structural Biology of Novel Drug Targets in Human Diseases, INSERM U1209, CNRS UMR 5309, University Grenoble Alpes, 38000 Grenoble, France.*Corresponding author. Email: [email protected] (M.-A.H.); [email protected] (A.P.); [email protected] (F.L.)†These authors contributed equally to this work.
Copyright © 2019 The Authors, some rights reserved; exclusive licensee American Association for the Advancement of Science. No claim to original U.S. Government Works
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
2 of 11
rates at around 1 M (84 to 94%) compared with KDU691 (56 to 75%) and presented no apparent detrimental effects to host cells at 100 M, indicating that the selectivity index (SI) was well above 600. The C. parvum INRA and Nluc strains were equally susceptible to AN3661 in all experiments. Furthermore, electron microscopy of
infected HCT-8 cells revealed abnormal parasite development and no mature type 1 meronts (the parasite stage that follows the first replication in epithelial cells) in AN3661-treated cells at 20 hours pi (fig. S1C). Collectively, these data show that AN3661 has a fast mechanism of action and is highly selective for C. parvum strains.
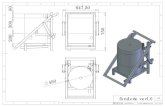
Fig. 1. Efficacy against C. parvum in cell culture and mouse mod-els. (A) Chemical structure of AN3661 with positions numbered as used in the text. (B) Comparative inhibitory activity of AN3661, KDU691, and NTZ against C. parvum (Cp) INRA Nluc strain in human ileocecal HCT-8 cells. The effect of AN3661 in reducing parasitic load in cells was monitored by the luminescence signal of transgenic Nluc parasites (each concentration point represents the average of six measurements). Curves cor-responding to AN3661-, KDU691-, and NTZ-treated parasites are in magenta, blue, and brown, re-spectively. Estimated EC50 mea-surements are shown. (C) Schematic representation of the 5-day oral dosage of AN3661 (20 mg/kg) in 7-day-old neonatal mice infected with 5 × 105 oocysts. The degree of infection was monitored by counting the oocysts in the small intestine of the animals at 4 or 6 dpi (n = 6 to 7 per group). Mann-Whitney test, ***P < 0.001 and **P < 0.005. (D) Schematic representation of the 7-day oral dosage of AN3661 (20 mg/kg) in IFN−/− adult mice infected with 5 × 105 oocysts. Kinetics of parasite excretion were monitored by measuring the number of oocysts in the feces of each mouse (n = 4 to 8 per group). (E) SEM imaging of ileum of adult immunocompromised IFN−/− mice was performed at the end of the experiment at 8 dpi for AN3661-treated and untreated mice. (F) Single-dose treatment of AN3661 in neonatal mice at 5 dpi preceding the peak of infection. Infection was monitored 24 hours after AN3661 adminis-tration (n = 9 per group; Mann- Whitney test, **P < 0.005). (G) SEM imaging of ileum of neonatal mice was performed at the end of the experiment (F) at 6 dpi. (H) Single- dose treatment of AN3661 in immunocompromised adult mice (IFN−/−) treated at 4 dpi (20 mg/kg). Infection was monitored 24 hours after AN3661 administration (n = 11 to 12 per group; Mann-Whitney test, **P < 0.005). (I) Evaluation of the minimal single dose of AN3661 required to reduce C. parvum infection in neonatal mice (n = 7 to 8 per group). Kruskal-Wallis test, *P < 0.01 and **P < 0.005. (J) Comparison of the efficacy between AN3661 (20 mg/kg) and NTZ (200 mg/kg) to limit C. parvum infection in IL12p40−/− (p40−/−) mice by one or two oral administrations. Parasite excretion was monitored by measuring the number of oocysts in the feces of each mouse at 4 and 5 dpi (n = 6 to 8 per group; Kruskal-Wallis test, **P < 0.005; ns, nonsignificant). All points are median ± SEM.
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
3 of 11
In vivo efficacy of AN3661 in C. parvum–infected miceWe then investigated whether this potent in vitro inhibition trans-lated to Cryptosporidium infections in vivo using neonatal wild-type and adult immunodeficient (IFN−/− and IL12p40−/−) mouse models that mimic infection in children and in immunocompromised pa-tients, respectively (18). When orally dosed at 20 mg/kg in a 5-day treatment starting 1 day postinfection (dpi), AN3661 reduced the number of oocysts in the intestine of neonatal mice to hardly de-tectable amounts (below the detection limit or undetected), both at the beginning (4 dpi) and at the peak of infection (6 dpi) (Fig. 1C). The same dose over a 7-day oral treatment course in adult immuno-compromised mice also maintained oocyst excretion at barely detectable amounts (Fig. 1D and fig. S1D) even in the IFN−/− mice that were greatly infected by the parasite, as revealed by scanning electron microscopy (SEM) (Fig. 1E).
This substantial reduction in parasite load in the ileum led us to evaluate the curative capacity of a single dose of AN3661 in neo-natal mice infected by C. parvum. Parasite replication was completely blocked (P < 0.0005) by a single dose of AN3661 orally administered at 3 dpi, the day preceding the first oocyst release (fig. S1E). When AN3661 was orally administrated the day preceding the peak of infection (5 dpi), the compound significantly reduced (P < 0.005) parasite load up to 80% (Fig. 1F). In this regard, the ileum of treated neonates almost never exhibited mature meronts, unlike in untreated mice (Fig. 1G). Similarly, a single-dose oral administration of AN3661 to heavily infected adult mice significantly reduced parasite load up to 55% (P < 0.005) and 87% (P < 0.05) in IFN−/− and IL12p40−/− mice, respectively (Fig. 1H and fig. S1F). Last, we evaluated the lowest efficient dose able to reduce infection in neonate model and found that at 0.4 mg/kg, there was a statistically significant reduction (P 99%) in all C. parvum species, with two amino acid variants, M12/V12 and E314/D314, found distal to the active site. We then crystallized and determined high-resolution crystal structures of unbound ChCPSF3 and a complex with AN3661 at 1.6- and 2.0-Å resolution, respectively (table S1).
Overall structure of ChCPSF3ChCPSF3 folds into a metallo-beta-lactamase (MBL) domain (resi-dues 1 to 232), a beta-CASP domain (residues 233 to 419), and an RNA specificity domain (residues 431 to 480) (Fig. 2, A to C). At the interface of these three domains, we observed two zinc atoms that are presumably involved in catalysis. Although we did not add exogenous zinc during sample preparation or in the crystallization buffer, the affinity of the recombinantly expressed ChCPSF3 to the zinc atoms was high enough to allow the metal to be captured from the expression media. The architecture of the MBL domain consists of a repeated / topology bearing four motifs coordinating the zinc atoms (numbered 1 to 4). This / sandwich is completed by the insertion of sheets 13 and 15 of the beta-CASP domain. A unique feature of this CPSF3 endonuclease is the presence of the three additional catalytic motifs (12), which also participate in the coordination of the two zinc atoms: the A motif in the loop con-necting the MBL and beta-CASP domain, the B motif in the loop bridging the beta-CASP domain and the RNA specificity domain, and, lastly, the C motif in between the -13 and -6 of the RNA specificity domain (fig. S2B). However, the most unique aspect of ChCPSF3 is a long loop within the MBL domain that is folded upon the main RNA groove and is likely to play an important regulatory role for substrate access to the catalytic site (Fig. 2, B and C). We note that this loop is also found in both Plasmodium and Toxoplasma parasites, two of the closest Cryptosporidium relatives, but is absent in human CPSF73 (fig. S2B). On the basis of the available structures of zinc-dependent ribonucleases (RNases) sharing an MBL fold bound to mRNA, we docked a short mRNA substrate at the catalytic site of ChCPSF3. This showed that the scissile phosphate bond (Pi-1) is well exposed to a key water molecule (w3) that is presumably activated or oriented by the highly conserved aspartic acid residue (D87) (figs. S2 and S3). On the other side of this water molecule, a conserved histidine residue (H423) (fig. S2B) could act as the proton donor for the cleaved mRNA leaving the group after catalysis. The coordination sphere of the zinc atoms at the catalytic site adopts an octahedral configuration facilitated by conserved histidine and aspartic acid residues and is completed by three water molecules (Fig. 3). This coordination of the water molecules resembles the arrangement found in bacterial MBLs such as VIM (Verona integrin- encoded MBL), IMP (imipenemase), and NDM (New Delhi MBL) (19). Furthermore, it is also different to human CPSF73, where only a single water molecule and a phosphate are found at the catalytic site (12). An outer layer to the residues directly coordinating the zinc atoms makes a hydrophobic belt formed by the residues F84, V182, A185, F264, Y230, and Y385, which may stabilize the catalytic site and thereby increase the affinity for the zinc ions (fig. S4, A and B). An equivalent rearrangement is found in carbonic anhydrase II and was shown to play a crucial role for correct catalysis (20).
AN3661 inhibition mechanism of CPSF3The high-resolution crystal structure of the ChCPSF3-AN3661 complex unveils the molecular basis of inhibition of the metal- dependent mRNase activity of CPSF3 in Cryptosporidium parasites. The oxaborole AN3661 binds directly to the CPSF3 catalytic site and interacts with the zinc atoms via the two hydroxyls and the oxygen-1 of the oxaborole ring (Fig. 3, A and B and fig. S5), at the same time displacing the water molecules involved in catalysis (Fig. 3C). Additional key interactions are shown in Fig. 3D and are fully detailed in fig. S6. These include direct hydrogen bonds by
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
4 of 11
oxygen-1 and hydroxyls to residues H181 and H423, and water- mediated interactions between the carboxylate oxygens in position 7 and residues F264 and I266. Key hydrophobic contacts are made between carbons 3 and 4 of AN3661 and the aromatic Y385, between carbon-1 and V35, and between the ethyl of AN3661 and F264. Therefore, the inhibition mechanism consists of the capturing of the metal-dependent mRNase activity of CPSF3 by the negatively charged boron that adopts a tetrahedral configuration and increases its nucleophilicity toward the metal center. This allows completion of the octahedral coordination of the zinc atoms with optimal metal coordination distances (2.1 to 2.3 Å) that efficiently competes with the catalytic water molecules (Fig. 3, E and F) and blocks the cleavage of the Pi–Pi-1 phosphate bond of the mRNA substrate (fig. S3B). For a summary of the proposed inhibition mechanism, see movie S1.
The carboxyethyl group of AN3661 packs against a less favorable rotamer of F264, a conformation that is already preadopted in
unbound ChCPSF3. This is because of the presence of E137, a residue within the insertion that is idiosyncratic to api-complexan enzymes and is absent in the human CPSF3 (figs. S2B and S7, A to D). Conversely, the equivalent residue in human CPSF3 (F241) adopts a dif-ferent conformation, which is not com-patible with the binding of AN3661 (fig. S7, B to F). Presumably, this structural difference that typifies apicomplexan enzymes contributes to the selectivity of AN3661 toward CPSF3 and might explain the lack of toxicity of this ox-aborole. It is also possible that the se-lective inhibition of CPSF3 in parasites is achieved through allosteric changes within the whole CPSF complex (see Fig. 4C).
On the basis of the high sequence conservation of residues at the AN3661 binding site of ChCPSF3 within the apicomplexan phylum and beyond in Trypanosoma enzymes (fig. S8), we built homology models using the structures of ChCPSF3 presented in this work (Fig. 4, A to D). In all cases, the docking of oxaboroles into the catalytic site of CPSF3 was favorable (Fig. 4, A and B). These include Scyx6759 and acoziborole (Scyx-7158), the latter being the most promising oxaborole in clinical development for the treatment of human African trypanosomiasis (21, 22). Based on the structural simi-larities between AN3661 and acoziborole, as well as on the AN3661 binding pocket, we predicted that the binding mode of acoziborole to Trypanosoma brucei CPSF3 is equivalent to that of AN3661. Specifically, the oxaborole group of acoziborole would bind to the metal center of T. brucei
CPSF3 similarly as in ChCPSF3, whereas the 6-benzamide sub-stitution would likely pack against F266 (Fig. 4C). Our struc-tures also explain the resistance mechanisms that allowed pointing out CPSF3 as the target of oxaboroles (10, 11). Forward genetic approaches performed on T. gondii and P. falciparum identified point mutations in CPSF3 conferring resistance to oxaboroles (fig. S2B). Although most of the resistant mutations clustered in the MBL domain of CPSF3, none of the mutations that were found in the residues at the catalytic site establish direct polar contacts to AN3661. Instead, the mutations were located in the outer hydrophobic belt around the residues coordinating the zinc atoms, highlighting the importance of this outer layer for the integrity of the CPSF3 AN3661 binding site (figs. S2B and S4A). Combined with previous findings, our results provide evidence showing that the CPSF3 inhibition mechanism by AN3661 in Cryptosporidium is a shared mechanism across other parasite species.
Fig. 2. Structure of C. hominis CPSF3 in the ligand-free (apo) form. (A) Linear domain architecture of the ChCPSF3 construct showing the MBL domain (blue), beta-CASP domain (green), RNA specificity domain (orange), and apicomplexan- specific insertion (magenta). The same color code is used in all figures. (B) Ribbon representations of the crystal structure of ChCPSF3 rotated 180° with respect to each other, with zinc atoms 1 and 2 (violet spheres) bound at the interface formed by the MBL domain, the beta-CASP domain, and the RNA specificity domain. Sheets and helices are numbered as in the primary sequence representation shown in fig. S2. (C) Surface representation rotated 180° (top) and 90° (bottom) showing the side and top views of the disposition of ChCPSF3 domains with respect to the catalytic site with Zn1-Zn2 metal atoms.
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
5 of 11
In vitro endonuclease activity of recombinant ChCPSF3 and inhibition by AN3661We next performed activity assays to in-vestigate whether ChCPSF3 has an endog-enous endonuclease function. We designed a 5′, 3′-biotinylated Cryptosporidium pre-mRNA substrate (Fig. 4E) containing the polyadenylation signal and a cleavage site (CA) 20 nucleotides further down-stream and measured the cleavage re-action by the luminescent conjugate of streptavidin. The mRNA degrada-tion over 4 hours is correlated with the increase in ChCPSF3 protein concen-tration (Fig. 4F). To test the protective effect of AN3661, we used the same test with serial dilutions of AN3661. Pro-tection of the mRNA was observed by increasing the concentration of AN3661 (Fig. 4F), although the high apparent half maximal inhibitory concentration IC50 value (14 mM) was observed well above the range of the in vitro EC50.
DISCUSSIONCryptosporidium represents a major health issue today for several reasons. First, it is a water-borne parasite, highly resist-ant to most chlorine-based disinfec-tants that are globally used in standard water treatment procedures. Transmis-sion of this parasitosis is therefore not exclusive to low-income countries but is highly widespread in countries where water treatment and disposal infra-structures are limited. Second, although not a life-threatening diarrhea in healthy adults, cryptosporidiosis develops into a chronic and life-threatening condition for immunocompromised individuals and young malnourished children. Unfor-tunately, the only available treatment, NTZ, has limited efficacy to fully elimi-nate the parasite infection in these cases.
Here, we demonstrate that the use of the oxaborole AN3661 efficiently treats cryptosporidiosis in relevant mice models, and together with these results, we de-tail the structural and biochemical basis of the inhibition.
Together with the crystal structures of the target protein CPSF3 presented here, our biochemical data show that ChCPSF3 is a bona fide endonuclease that retains pre-mRNA processing activity. A discrepancy was, however, observed with regard to the measured IC50 when
Fig. 3. Structure of the complex ChCPSF3-AN3661 and CPSF3 inhibition mechanism. (A) Overall surface repre-sentation of the complex formed by ChCPSF3 with AN3661, shown as a violet transparent surface and indicated with a white arrow. (B) Zoomed-in view of the ChCPSF3 catalytic with AN3661. AN3661 is shown as a magenta stick repre-sentation covering a violet surface. Zinc atoms are displayed as dark purple spheres. Key residues coordinating the Zn atoms are numbered and shown as white sticks. Interactions are represented by dashed green lines. (C) Zoomed-in view of the catalytic site of the unbound ChCPSF3 structure in the same orientation as the complex ChCPSF3-AN3661 shown in (B). Water molecules 1 to 3 are shown as red spheres. (D) Additional interactions established by AN3661 at the catalytic site of CPSF3. Direct hydrogen bonds to protein residues and hydrogen bonds mediated by water molecules 17 and 20 are shown as dashed green lines. Hydrophobic contacts between AN3661 and residues F264, Y385, and V35 are shown as transparent white surface (protein) and white dots (AN3661). Residue S421, which mediates an interaction to AN3661 (fig. S6), was omitted for clarity. (E) Schematic representation of the metal center in the unbound ChCPSF3 structure showing a octahedral coordination sphere facilitated by H/D protein residues and three water molecules. Metal-protein/water interactions are shown as green dashed lines, and distances are shown in angstroms. (F) Same orientation as in (E) with AN3661 bound at the catalytic site of the ChCPSF3-AN3661 complex.
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
6 of 11
compared with the EC50 reflecting a certain experimental gap between the biochemistry and cellular biology. This gap could be explained by either the buffer conditions required for protein stability and activity not being optimal for AN3661 binding [100 mM KCl, 10% glycerol, 30-min preincubation of CPSF3 in 5 mM CaCl2 as described by (12)], or the fact that CPSF3 was ex-pressed in bacteria as a single protein outside of its fully assembled CPSF com-plex. For these reasons, recombinant ChCPSF3 may only display residual mRNase activity. Moreover, the catalytic site is observed in a closed state within the crystallographic structure, poten-tially limiting the entry of the RNA sub-strate, a feature previously described for human CPSF73 as well (12).
Evidence of a direct mechanism of action is however brought by the unam-biguous electron density of AN3661 within the highly conserved catalytic site, com-bined with the genetic resistant mutants in CPSF3 found across apicomplexan and trypanosamid species (10, 11, 14, 15). These observations demonstrate that oxaboroles bind directly to the catalytic site of CPSF3 and probably inhibit its mRNA process-ing activity, thereby reducing parasite growth.
Further studies on the whole CPSF complex will likely be required to correlate the in vitro IC50 with the in vivo EC50 values. In this respect, recent crystal and cryo–electron microscopy structures of CPSF subcomplexes revealed an impor-tant basis for the specificity in the recog-nition of mRNA and key differences at least between human and yeast (23–26). However, none of these structures con-tained the endonuclease subunit CPSF3. Thus, our structures of ChCPSF3 provide an opportunity for future structural studies to understand the assembly of CPSF3 within higher entity complexes.
AN3661 has some chemical similari-ties to the 3-aminomethyl benzoxaborole AN6426, which was proven by genetic, biochemical, and structural studies to in-hibit the leucine-tRNA synthetase (LeuRS) in Cryptosporidium (27), showing that ox-aboroles can target different pathways through variations in their chemistry. Polypharmacology by AN3661 to other targets in Cryptosporidium cannot be fully excluded because no biochemical approach has yet shown a strong inhibition of the
Fig. 4. Structural predictions of oxaborole compatible binding to CPSF3 across parasitic species and endo-nuclease protection assay of ChCPSF3. (A) Structure of the Cryptosporidium CPSF3-AN3661 complex presented in this work, with AN3661 (violet) as a transparent surface and stick representation. The inset shows a zoomed-in view of AN3661 and the key residues involved in the interaction with AN3661. The same is shown for the binding of AN3661 or related oxaboroles to the calculated structural models of T. gondii CPSF3 (B), T. brucei CPSF3 (C), and P. falciparum CPSF3 (D). (E) Schematic representation of the double-biotinylated 37–base pair (bp) meth-RS used in conjunction with the streptavidin/horseradish peroxidase (HRP) conjugate that together produce a luminescent signal through the processing of luminol into a ground-state dianion. (F) Northern blotting of 37-bp biotinylated meth-RS (detected by the streptavidin HRP conjugate) in the absence or presence of increasing concentrations of CPSF3, at constant CPSF3 concentration, or with decreasing amounts of AN3661 (100 to 0.75 mM). After band integration, calculated RNA conservation ratios (1 being nondegraded and 0 being fully degraded) were plotted against AN3661 concentrations and fitted with four-parameter curves. The apparent IC50 was calculated as the mean of duplicate experiments.
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
7 of 11
cleavage and polyadenylation activity in vitro. However, the data presented here combined with previous studies strongly suggest that CPSF3 is the main target of AN3661 in Cryptosporidium. The overall conservation of CPSF3 catalytic core in Apicomplexa and its essential function toward pre-mRNAs render likely that inhibition of CPSF3 in Cryptosporidium is responsible for the antiparasitic activity of AN3661. In addition, we can now better interpret the distribution of mutations in apicomplexan CPSF3 conferring resistance to AN3661. As evidence by the place where AN3661 binds to, all previously described resistant mutations in T. gondii and P. falciparum could act in a distal and allosteric manner on the ability of AN3661 to bind the catalytic site of parasitic CPSF3 (10, 11). This also indicates that the probability for resistance-conferring mutations to appear in the inner catalytic pocket residues that contact directly AN3661 is quite low, because of the essentiality of these same residues in proper CPSF3 catalytic function.
We present an inhibitor of Cryptosporidium, AN3661, which rapidly reduces oocysts in feces that has better efficacy than NTZ, showing therapeutic effects on day 1 after treatment administration. AN3661 presented an oral efficacy in a single-dose administration and ex-hibited an SI higher than 600-fold in human ileocecal adenocarci-noma cells (HCT-8). Thus, AN3661 complies well with all the criteria heralded for new anti-Cryptosporidium drugs (28, 29). Together with the recently discovered inhibition of phosphatidylinositol 4-kinase (16, 17), inhibition of the CPSF3-dependent mRNA processing activity by oxaboroles provides an alternative approach for the development of future anti-Cryptosporidium drugs. Furthermore, as the CPSF3 AN3661 binding pocket is highly conserved throughout apicomplexan parasites, the structural data provided here will guide the optimization and development of future oxaborole derivatives, potentially open-ing the way to a potential pan-apicomplexan treatment. Last, CPSF3 targeting may also provide opportunities for drug discovery not only in infectious diseases but also in human diseases associated to the deregulation of mRNA processing by CPSF proteins.
There are some limitations to our study. The gap between the observed biochemical inhibition and in vivo efficacy suggests that the inhibitory process may be more elaborate than suspected. In the invading parasite, the inhibition process happens in the context of a full CPSF complex performing the cleavage and polyadenylation activity where the interplay between CPSF3 and its other subunits of the complex is still poorly understood. Although expected to show a comparable efficacy on C. hominis, in vivo testing will be required as subtle sequence changes with CPSF3 or other proteins involved in the inhibition process could modify the dose response and specificity of AN3661 against this strain. Data showing the direct causal link between CPSF3 inhibition and the selective efficacy on Cryptosporidium are also lacking in this study. However, recently developed strategies enabling for the cultivation and genetic manip-ulations of Cryptosporidium (30, 31) may answer these questions through direct genetic studies. Last, despite the observed low toxicity in cell culture and during short treatment time frames in mice, we will need to investigate the putative toxicity of the AN3661 over the long term, a prerequisite before any clinical phase trial.
MATERIALS AND METHODSStudy designThe objectives of this study were to assess the effectiveness and therapeutic potential of AN3661 against Cryptosporidium and to under-stand the mechanism of action of AN3661 toward Cryptosporidium
CPSF3. We designed in vivo experiments to compare intestinal par-asite burden in both immunocompromised and neonatal mouse models untreated or treated by AN3661, KDU69, gold standard NTZ, or a vehicle control. Details of animal age and sex are provided below. All rodents were randomized into treatment groups. Animal age and sex used in in vivo experiments are provided below and in the figure legends. AN3661-target interactions were validated and characterized through x-ray crystallography and biochemical studies. Where applicable, sample sizes, blinding schemes, and replicates are provided in this section and in the figure legends.
Cells and parasitesHuman ileocecal adenocarcinoma cells (HCT-8) were purchased from the American Type Culture Collection and cultured in RPMI 1640 with glutamine supplemented with 10% fetal bovine serum, 1 mM sodium pyruvate, penicillin (50 U/ml), and streptomycin (50 g/ml). C. parvum INRA strain (Unité mixte de recherche - Infectiologie et santé publique) was maintained by regular passage in newborn calves and purified as previously described (32). C. parvum INRA (UMR-ISP) and IOWA (Sterling Parasitology Laboratory, University of Arizona) strains were engineered to produce Nluc-expressing parasites via trans-fection with plasmids “TK_Eno_Nluc-Neo_TK” and “Aldo_Cas9_Ribo+U6TKguide#1” (gifts from B. Striepen at the University of Pennsylvania, USA) according to (30). Briefly, 108 C. parvum oocysts were suspended in 1 ml of 0.75% sodium taurocholate prepared in phosphate-buffered saline (PBS) (pH 7.4) and kept at 15°C for 10 min before incubation at 37°C for 45 min. Parasites were then washed in PBS, and unexcysted oocysts were removed by filtration through a 5-m Minisart syringe filter (Sartorius). After excystation, 5 × 107 sporozoites were suspended in 90 l of SF buffer (SF Cell Line 4D-Nucleofector kit, Lonza) and mixed with 100 g of DNA in a final volume of 100 l. Parasites were then electroporated in 100-l Nucleocuvette vessels (Lonza) using the program EH100 on the AMAXA Nucleofector 4D device (Lonza). Immediately after electro-poration, sporozoites were suspended in PBS, directly injected into the small intestine of four IFN−/− mice through abdominal surgery, and submitted to paromomycin selection (16 mg/ml) as described pre-viously (30). Animal experimental procedures (APAFIS #8900) were approved by the Loire Valley ethical review board (CEEA VdL, committee no. 19). Mouse feces were mixed with potassium di-chromate (2% in water), and oocysts were then purified through serial filtration steps (630-, 315-, 100-, and 20-m sieves), followed by flo-tation on magnesium sulfate (density, 1.2), sucrose density gradient, and 20-min treatment in 0.3% sodium hypochlorite. Transgenic C. parvum lines were maintained in our experimental facilities by passages in IFN−/− mice under paromomycin selection.
Cryptosporidium EC50 determination and cell toxicityHCT-8 cells were grown to confluence in white 96-well plates (Thermo Scientific Nunc MicroWell), infected with freshly purified N-luc–expressing oocysts [multiplicity of infection (MOI), 1], and incubated with different AN3661 concentrations. The compound 7-(2-carboxyethyl)-1,3-dihydro-1-hydroxy-2,1-benzoxaborole (AN3661) was purchased from ChemPartner, NTZ was purchased from Sigma, and KDU691 was provided by Novartis.
Because of their poor solubility, NTZ and KDU691 stock solu-tions were prepared at 100 mM in dimethyl sulfoxide (DMSO). AN3661 was prepared at 100 mM in 50% DMSO. After 3 hours, cell cultures were washed twice, and media were replaced with the same
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
8 of 11
AN3661 concentration and further incubated for 24 or 48 hours. Culture supernatant was removed from the wells (six replicates for each concentration), and 200 l of Nano-Glo lysis buffer containing 1:50 of Nano-Glow substrate (Promega) was added to the wells. After 3 min of incubation, luminescence was measured with GloMax-Multi+ (Promega) and analyzed with Instinct software. EC50 was calculated with GraphPad Prism software from the dose-response inhibition curve.
To determine the cytotoxic concentration 50% (CC50) of AN3661 on HCT-8 cells at 24-hour incubation, an MTS assay was used [CellTiter 96 AQueous One Solution Cell Proliferation Assay (MTS), Promega]. The SI of AN3661 was calculated as SI = CC50/EC50.
Animal ethics statementIFN−/− and IL12p40−/− mice from a C57BL/6 genetic background were purchased from the Jackson laboratory and acclimated and maintained in animal facilities at the Plateforme d’Infectiologie Expérimentale de Tours (PFIE). Wild-type C57BL/6 mice were purchased from Janvier Labs and acclimated and maintained under similar conditions. All experiments were conducted in accordance with the guidelines of the Directive 2010/63/EU of the European Parliament and of the Council in the facilities of the PFIE (UE-1277, INRA Centre Val de Loire, Nouzilly, France). All experimental pro-cedures (APAFIS #11396 and #8900) were approved by the Loire Valley ethical review board (CEEA VdL, committee no. 19).
In vivo efficacy of compoundsAN3661 and NTZ solutions were prepared in the following vehicle: 1% (w/w) carboxymethylcellulose (CMC; Sigma), 0.1% (w/w) Tween 80 (VWR), and Milli-Q water. The vehicle article solution was pre-pared by slowly dispensing the required amount of CMC powder on the water under high agitation to avoid clumping. Tween 80 was added to the CMC solution afterward. All solutions were prepared at room temperature. Solutions of AN3661 (2 mg/ml) and NTZ (20 mg/ml) were prepared by including the required AN3661 amount and following the same procedure as with the vehicle. AN3661 solutions were homogenized for intervals of 5 min, and homogenization was stopped before suspension began to rise in temperature. The pH of the AN3661 solution was adjusted to 6.0 by adding sodium hydroxide (about 2% of batch volume) and stirring for an additional 30 min. NTZ solution was adjusted to pH 8.0 and stirred overnight. All the solutions were continuously and vigorously vortexed for a minimum of 5 min at room temperature before the start of dosing and throughout the dosing procedure.
Seven-day-old wild-type neonatal mice were infected by oral gavage with 5 × 105 oocysts of C. parvum INRA strain and treated orally with 20 l of treatment suspension or sham treated with 20 l of vehicle solution. The degree of infection in individual neonatal mice was assessed by determining the number of oocysts in the intestinal contents (33). Adult mice aged 6 to 10 weeks were infected with 5 × 105 oocysts of the C. parvum INRA strain and treatment or vehicle administered by oral gavage in 100- or 200-l volume de-pending on the experiment. In all experiments, oocysts were quan-tified in fecal pellets of individual mice collected daily for 2 hours according to a published protocol (34).
Electron microscopyTransmission electron microscopyHCT-8 cells were grown to confluence on Transwell chambers of 0.4-m pore size, infected with C. parvum INRA (MOI, 30) for 2 hours,
and washed, and monolayers were fixed in 4% paraformaldehyde and 1% glutaraldehyde in 0.1 M phosphate buffer (pH 7.3). The fixed monolayers were then washed in phosphate buffer and post-fixed by incubation with 2% osmium tetroxide for 1 hour. Samples were then fully dehydrated in a graded series of ethanol solutions and embedded in Epon resin. Ultrathin sections were stained with 5% uranyl acetate and 5% lead citrate, and observations were made with a transmission electron microscope (JEOL 1011).Scanning electron microscopyIleal tissue samples were fixed by incubation for 24 hours in 4% paraformaldehyde and 1% glutaraldehyde in 0.1 M phosphate buffer (pH 7.3). Samples were then washed in phosphate buffer, postfixed by incubation with 2% osmium tetroxide for 1 hour, fully dehydrated in a graded series of ethanol solutions, and dried in hexamethyldisilane. Last, samples were coated with 40-Å platinum using a GATAN PECS 682 apparatus before observation under a Zeiss Ultra plus FEG-SEM scanning electron microscope.
Protein expression and purificationThe ChCPSF3 construct (1 to 482) based on the C. hominis sequence (GenBank accession no. CUV07592.1; CryptoDB Gene ID: CHUDEA8_460) was codon optimized and DNA synthesized by GeneScript. The synthetic gene was then inserted within a modified pET30-a(+) vector (Novagen) using Nde I and Xho I sites, resulting in an N-terminal tobacco etch virus (TEV) protease cleavable site fused to a 8xHis tag. Transformation was performed into chemically competent BL21(DE3)- CodonPlus-RIL bacteria (Stratagene), which were incubated on ice with 1 g of the pET30-a(+) ChCPSF3 plasmid for 10 min followed by a heat shock at 42°C for 45 s, preincubated for 45 min in Luria- Bertani medium (LB) at 37°C, and then spread on an LB agar plate containing kanamycin (Kan) and chloramphenicol (Chlo) and incu-bated for 12 hours. A single colony was then picked to inoculate an LB/Kan/Chlo 50-ml preculture grown for 16 hours. Five milliliters of grown preculture was then used to inoculate 1-liter flasks of Terrific Broth medium (Formedium) containing Chlo/Kan. Cultures were grown at 37°C until reaching an OD600 (optical density at 600) of 0.5 to 0.8 and induced by adding 0.7 mM IPTG (isopropyl--d- thiogalactopyranoside) (VWR), and then further incubated at 18°C for 14 hours. After incubation, cells were centrifuged for 25 min at 3000g, the supernatant was discarded, and the pellet was used for pro-tein purification or flash frozen in liquid nitrogen and kept at −80°C.
Purification was performed on pellets of 3-liter culture resuspended in 200 ml of lysis buffer containing 250 mM NaCl, 50 mM tris (pH 8), 2 mM beta-mercaptoethanol (BME), and 1 complete anti-protease cocktail (Roche) tab per 50 ml of buffer. Lysis was performed using 10-min pulsed sonication (15 s on, 30 s off) at 50% amplitude over ice. After sonication, the lysate was centrifuged at 4°C for 1 hour at 15,000g, and the pellet was discarded. All the following steps were subsequently performed at 4°C.
Before incubation with 5 ml of preequilibrated nickel-charged nitrilotriacetic acid (Ni-NTA) resin, the clarified lysate was supple-mented with 30 mM imidazole. Batch incubation was performed for 30 min at 4°C with gentle stirring. After incubation, the resin was retained on a vertical column and then washed with 3 × 20 ml of wash buffer containing 250 mM NaCl, 50 mM tris (pH 8), 2 mM BME, and 30 mM imidazole. We then performed direct elution with 1.5-ml fractionations using a buffer containing 150 mM NaCl, 50 mM tris (pH 8), 5 mM BME, and 300 mM imidazole. Fractions of interest were pooled and dialyzed overnight at 4°C in 50 mM NaCl, 50 mM
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
9 of 11
tris (pH 8), and 15 mM BME in the presence of histidine-tagged TEV protease [produced at the European Molecular Biology Lab-oratory (EMBL)] at a concentration of 0.1 mg/ml using a 20-kDa cutoff dialysis cassette (Thermo Scientific).
After dialysis, the entire sample was flown through 1 ml of Ni-NTA resin to remove any uncleaved ChCPSF3 and His-TEV and then directly pumped through the liquid chromatography system (Akta Pure, GE Healthcare) onto an HL-Mono-Q 5-ml column (GE Healthcare) preequilibrated with the same buffer as for dialysis. The column was washed with 5 column volumes of the same buffer and then eluted with a gradient of NaCl, 40 ml in length, going from 50 mM to 1 M. Absorbance monitoring (280 nm) was performed for the entirety of the elution, and 1.5-ml fractions were collected throughout the whole elution. Fractions of interest, checked by SDS–polyacrylamide gel electrophoresis (PAGE), were collected, pooled, and concentrated to 600 l using a 30-kDa cutoff concen-trator (Amicon Ultra, Millipore). After concentration, the sample was injected on an S200 (GE Healthcare), with a running buffer containing 150 mM NaCl, 50 mM tris (pH 8), and 1 mM BME, and eluted in a single homogeneous peak. Peak fractions were then pooled and concentrated with a 30-kDa concentrator to 15 mg/ml. A full ultraviolet absorbance scan was performed and revealed no nucleic acid presence in the final sample (A260/A280 = 0.6). The sample was then flash frozen and stored at −80°C for subse-quent use.
Initial crystallization experiments were carried out at the High Throughput Crystallisation Laboratory (HTX Lab) of the EMBL Grenoble (35). Microcrystals were tested for x-ray diffraction using the Crytal Direct technology (36). Macroscopic crystals were man-ually grown by a hanging drop vapor diffusion. In each well, a 1-l drop of purified ChCPSF3 at a concentration varying from 3 to 6 mg/ml was mixed with 0.8 l of precipitant mother liquor consisting of 17% (v/v) polyethylene glycol 4000, 10% (v/v) isopropanol, and 100 mM Hepes (pH 7.5). Hanging drops were set up in 24-well VDX plates (Hampton Research) containing 500 l of mother liquor in each well. Crystal growth was obtained after 3 days of incubation at 4°C; in all cases, crystals grew as macroscopic needle clusters. To increase needle thickness, microseeding of previously obtained crystals combined with lower protein concentration enabled lower nucleation rates, resulting in bigger needles. Apo ChCPSF3 crystals were grown with the addition of 10 mM taurine (Sigma-Aldrich), which also limited the nucleation rate. Cocrystallization of ChCPSF3 with AN3661 was obtained with the same precipitation mother liquor condition but with the addition of AN3661 at 1 mM within the protein sample. When harvested, crystals were fished in Hampton cryo-loops and cryoprotected in mother liquor with an additional 22% glycerol. AN3661 (1 mM) was also added to the cryoprotectant solution of the AN3661-CPSF3 cocrystals.
Crystal diffraction was performed at the European Synchro-tron Radiation Facility (ESRF) beamlines ID30-B and ID29, both equipped with PILATUS 6M detectors (Dectris). For both struc-tures, fine slicing helical collection was privileged. Indexing and integration were performed using the XDS program suite. Molecular replacement solutions were obtained with the Phaser (CCP4 program) using a homology model of ChCPSF3 built by using the human CPSF73 structure [Protein Data Bank (PDB) code: 2IZT] as a template. The initial solution was then improved through cycles of manual adjusting in Coot (37) and refined using Refmac5 (38).
In vitro endonuclease activity assaysThe double-biotinylated meth-RS (methionyl-tRNA synthetase) oli-gonucleotide (5′-biotin-AGCAAUAAAAAGAGACGGACAGAC-UAAGGCAAGUAGA-3′-biotin) was synthesized by Integrated DNA Technologies. All reactions were carried out in a final volume of 20 l in 50 mM tris (pH 7.5), 100 mM KCl, 10% glycerol, and 1 mM BME. Before dilution and incubation with RNA, ChCPSF3 was incubated with 5 mM CaCl for 30 min at 30°C, as previously described (12). Reactions were stopped by heating at 95°C for 1 min, followed by the addition of 5 l of 5X gel loading buffer [6 M urea, 2 mM EDTA, 10 0.1% bromophenol blue, 0.1% xylene cyanol blue, and 10 mM tris (pH 7.5)]. Eight microliters of sample was loaded onto prerun 15-well Urea PAGE gels (Sigma-Aldrich) and then run at 12 W in tris-borate EDTA buffer. Staining was performed with a 0.05% methylene blue solution. When performing North-ern blot detection, 2 nM dual biotinylated RNA was incubated with increasing concentrations of ChCPSF3 for 2 hours at 27°C, after which reactions were stopped and urea PAGE gels were run as de-scribed above. Liquid electrotransfer was performed at 4°C for 1 hour 30 min at 40 mA on Hybond-N+ membranes (Amersham). After transfer, biotin revelation was performed with the Chemi-luminescent Nucleic Acid Detection Module Kit (Thermo Fisher Scientific), and membrane luminescence acquisition with the C-DiGiT scanner (Li-COR). Band signal integration was performed using ImageJ, and obtained intensity values from replicate assays were background subtracted, converted to a conserved ratio (1 being fully conserved and 0 being fully degraded) by dividing a given point value by the integrated intensity of nondegraded RNA, plotted, and fitted with a four- parameter nonlinear regression curve in GraphPad Prism.
Sequence homology modeling and structural representationC. hominis, P. falciparum, T. gondii, T. brucei, and Homo sapiens CPSF3 sequence alignments were done using ClustalW by includ-ing the predicted MBL domain, the beta-CASP domain, and the RNA specificity domain. Representations of crystal structures were done in PyMOL, the video representation was done using Chimera, and the flat representation of the interactions between ChCPSF3 and AN3661 was done in LigPlus. The structural models of P. falciparum, T. gondii, and T. brucei were calculated according to published protocols (39) using the protein backbone atoms of the complex ChCPSF3-AN3661 (this work) as a template. Docking of the oxaboroles was done in Coot by matching their atomic coordinates to those of AN3661 followed by energy minimization (37).
The structural model of the complex bound to a short RNA con-taining the cleavage site was done by using as a template the structure of unbound ChCPSF3 (this work) and docking the mRNA bound to bacterial RNase Z/J structures (PDB codes: 3IEM, 5A0T, and 4XWW). For correct placing of the mRNA, the structures of bacterial RNases were aligned to ChCPSF3 using their MBL fold to the backbone range 24 to 123 of ChCPSF3 with the LSQ module of Coot, and mutating the U-U-U to a C-A-C to better represent the mRNA cleavage site.
Statistical analysesStatistical analyses were performed using GraphPad Prism software. Two-group analyses were performed using the Mann-Whitney nonparametric t test. For multigroup analyses, we used the non-parametric Kruskal-Wallis followed by Dunn’s multiple comparison.
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
10 of 11
For all analyses, a P value equal to or less than 0.05 was considered significant.
SUPPLEMENTARY MATERIALSstm.sciencemag.org/cgi/content/full/11/517/eaax7161/DC1Fig. S1. Growth of Nluc C. parvum strains in epithelial cells and efficacy of AN3661 in adult IL12p40−/− and neonatal mice.Fig. S2. Domain architecture and sequence conservation of C. hominis CPSF3.Fig. S3. Structural model of ChCPSF3 with an mRNA substrate docked into the catalytic site.Fig. S4. Hydrophobic belt around the residues coordinating the Zn atoms and stereo view of the electron density of metals.Fig. S5. Stereo view of the catalytic site of ChCPSF3 with electron density of AN3661.Fig. S6. Detailed view of the interactions established by AN3661 at the catalytic site of ChCPSF3.Fig. S7. Structural differences between Cryptosporidium and human CPSF3.Fig. S8. Conservation of the CPSF3 AN3661-binding site in apicomplexan and trypanosomatid parasites.Fig. S9. Summary of mRNA processing machinery and inhibition of parasite CPSF3 by oxaboroles.Table S1. Crystallographic data and refinement statistics.Movie S1. Proposed inhibition mechanism of CPSF3 by the benzoxaborole AN3661.
View/request a protocol for this paper from Bio-protocol.
REFERENCES AND NOTES 1. D.-A. T. Shirley, S. N. Moonah, K. L. Kotloff, Burden of disease from cryptosporidiosis.
Curr. Opin. Infect. Dis. 25, 555–563 (2012). 2. D. L. Liu, S. Oza, D. Hogan, Y. Chu, J. Perin, J. Zhu, J. E. Lawn, S. Cousens, C. Mathers,
R. E. Black, Global, regional, and national causes of under-5 mortality in 2000–15: An updated systematic analysis with implications for the Sustainable Development Goals. Lancet 388, 3027–3035 (2016).
3. K. L. Kotloff, J. P. Nataro, W. C. Blackwelder, D. Nasrin, T. H. Farag, S. Panchalingam, Y. Wu, S. O. Sow, D. Sur, R. F. Breiman, A. S. G. Faruque, A. K. M. Zaidi, D. Saha, P. L. Alonso, B. Tamboura, D. Sanogo, U. Onwuchekwa, B. Manna, T. Ramamurthy, S. Kanungo, J. B. Ochieng, R. Omore, J. O. Oundo, A. Hossain, S. K. Das, S. Ahmed, S. Qureshi, F. Quadri, R. A. Adegbola, M. Antonio, M. J. Hossain, A. Akinsola, I. Mandomando, T. Nhampossa, S. Acácio, K. Biswas, C. E. O’Reilly, E. D. Mintz, L. Y. Berkeley, K. Muhsen, H. Sommerfelt, R. M. Robins-Browne, M. M. Levine, Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): A prospective, case-control study. Lancet 382, 209–222 (2013).
4. J. A. Platts-Mills, S. Babji, L. Bodhidatta, J. Gratz, R. Haque, A. Havt, B. J. J. McCormick, M. McGrath, M. P. Olortegui, A. Samie, S. Shakoor, D. Mondal, I. F. N. Lima, D. Hariraju, B. B. Rayamajhi, S. Qureshi, F. Kabir, P. P. Yori, B. Mufamadi, C. Amour, J. D. Carreon, S. A. Richard, D. Lang, P. Bessong, E. Mduma, T. Ahmed, A. A. A. M. Lima, C. J. Mason, A. K. M. Zaidi, Z. A. Bhutta, M. Kosek, R. L. Guerrant, M. Gottlieb, M. Miller, G. Kang, E. R. Houpt; MAL-ED Network Investigators, Pathogen-specific burdens of community diarrhoea in developing countries: A multisite birth cohort study (MAL-ED). Lancet Glob. Health 3, e564–e575 (2015).
5. WHO report, WHO | World health report Report 2017, (WHO Report, 2017); https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-disease [accessed 21 December 2018].
6. B. Amadi, M. Mwiya, J. Musuku, A. Watuka, S. Sianongo, A. Ayoub, P. Kelly, Effect of nitazoxanide on morbidity and mortality in Zambian children with cryptosporidiosis: A randomised controlled trial. Lancet 360, 1375–1380 (2002).
7. B. Amadi, M. Mwiya, S. Sianongo, L. Payne, A. Watuka, M. Katubulushi, P. Kelly, High dose prolonged treatment with nitazoxanide is not effective for cryptosporidiosis in HIV positive Zambian children: A randomised controlled trial. BMC Infect. Dis. 9, 195 (2009).
8. W. Checkley, A. C. White Jr., D. Jaganath, M. J. Arrowood, R. M. Chalmers, X.-M. Chen, R. Fayer, J. K. Griffiths, R. L. Guerrant, L. Hedstrom, C. D. Huston, K. L. Kotloff, G. Kang, J. R. Mead, M. Miller, W. A. Petri Jr., J. W. Priest, D. S. Roos, B. Striepen, R. C. Thompson, H. D. Ward, W. A. Van Voorhis, L. Xiao, G. Zhu, E. R. Houpt, A review of the global burden, novel diagnostics, therapeutics, and vaccine targets for cryptosporidium. Lancet Infect. Dis. 15, 85–94 (2015).
9. C. T. Liu, J. W. Tomsho, S. J. Benkovic, The unique chemistry of benzoxaboroles: Current and emerging applications in biotechnology and therapeutic treatments. Bioorg. Med. Chem. 22, 4462–4473 (2014).
10. A. Palencia, A. Bougdour, M.-P. Brenier-Pinchart, B. Touquet, R.-L. Bertini, C. Sensi, G. Gay, J. Vollaire, V. Josserand, E. Easom, Y. R. Freund, H. Pelloux, P. J. Rosenthal, S. Cusack, M.-A. Hakimi, Targeting Toxoplasma gondii CPSF3 as a new approach to control toxoplasmosis. EMBO Mol. Med. 9, 385–394 (2017).
11. E. Sonoiki, C. L. Ng, M. C. S. Lee, D. Guo, Y.-K. Zhang, Y. Zhou, M. R. K. Alley, V. Ahyong, L. M. Sanz, M. J. Lafuente-Monasterio, C. Dong, P. G. Schupp, J. Gut, J. Legac, R. A. Cooper,
F.-J. Gamo, J. DeRisi, Y. R. Freund, D. A. Fidock, P. J. Rosenthal, A potent antimalarial benzoxaborole targets a Plasmodium falciparum cleavage and polyadenylation specificity factor homologue. Nat. Commun. 8, 14574 (2017).
12. C. R. Mandel, S. Kaneko, H. Zhang, D. Gebauer, V. Vethantham, J. L. Manley, L. Tong, Polyadenylation factor CPSF-73 is the pre-mRNA 3′-end-processing endonuclease. Nature 444, 953–956 (2006).
13. K. Ryan, O. Calvo, J. L. Manley, Evidence that polyadenylation factor CPSF-73 is the mRNA 3′ processing endonuclease. RNA 10, 565–573 (2004).
14. D. Begolo, I. M. Vincent, F. Giordani, I. Pöhner, M. J. Witty, T. G. Rowan, Z. Bengaly, K. Gillingwater, Y. Freund, R. C. Wade, M. P. Barrett, C. Clayton, The trypanocidal benzoxaborole AN7973 inhibits trypanosome mRNA processing. PLOS Pathog. 14, e1007315 (2018).
15. R. J. Wall, E. Rico, I. Lukac, F. Zuccotto, S. Elg, I. H. Gilbert, Y. Freund, M. R. K. Alley, M. C. Field, S. Wyllie, D. Horn, Clinical and veterinary trypanocidal benzoxaboroles target CPSF3. Proc. Natl. Acad. Sci. U.S.A. 115, 9616–9621 (2018).
16. U. H. Manjunatha, S. Vinayak, J. A. Zambriski, A. T. Chao, T. Sy, C. G. Noble, G. M. C. Bonamy, R. R. Kondreddi, B. Zou, P. Gedeck, C. F. Brooks, G. T. Herbert, A. Sateriale, J. Tandel, S. Noh, S. B. Lakshminarayana, S. H. Lim, L. B. Goodman, C. Bodenreider, G. Feng, L. Zhang, F. Blasco, J. Wagner, F. J. Leong, B. Striepen, T. T. Diagana, A Cryptosporidium PI(4)K inhibitor is a drug candidate for cryptosporidiosis. Nature 546, 376–380 (2017).
17. C. W. McNamara, M. C. S. Lee, C. S. Lim, S. H. Lim, J. Roland, A. Nagle, O. Simon, B. K. S. Yeung, A. K. Chatterjee, S. L. McCormack, M. J. Manary, A.-M. Zeeman, K. J. Dechering, T. R. S. Kumar, P. P. Henrich, K. Gagaring, M. Ibanez, N. Kato, K. L. Kuhen, C. Fischli, M. Rottmann, D. M. Plouffe, B. Bursulaya, S. Meister, L. Rameh, J. Trappe, D. Haasen, M. Timmerman, R. W. Sauerwein, R. Suwanarusk, B. Russell, L. Renia, F. Nosten, D. C. Tully, C. H. M. Kocken, R. J. Glynne, C. Bodenreider, D. A. Fidock, T. T. Diagana, E. A. Winzeler, Targeting Plasmodium PI(4)K to eliminate malaria. Nature 504, 248–253 (2013).
18. S. L. M. Arnold, R. Choi, M. A. Hulverson, D. A. Schaefer, S. Vinayak, R. S. R. Vidadala, M. C. McCloskey, G. R. Whitman, W. Huang, L. K. Barrett, K. K. Ojo, E. Fan, D. J. Maly, M. W. Riggs, B. Striepen, W. C. Van Voorhis, Necessity of bumped kinase inhibitor gastrointestinal exposure in treating Cryptosporidium infection. J. Infect. Dis. 216, 55–63 (2017).
19. M. F. Mojica, R. A. Bonomo, W. Fast, B1-Metallo--Lactamases: Where do we stand? Curr. Drug Targets 17, 1029–1050 (2016).
20. J. A. Hunt, C. A. Fierke, Selection of carbonic anhydrase variants displayed on phage. Aromatic residues in zinc binding site enhance metal affinity and equilibration kinetics. J. Biol. Chem. 272, 20364–20372 (1997).
21. R. T. Jacobs, B. Nare, S. A. Wring, M. D. Orr, D. Chen, J. M. Sligar, M. X. Jenks, R. A. Noe, T. S. Bowling, L. T. Mercer, C. Rewerts, E. Gaukel, J. Owens, R. Parham, R. Randolph, B. Beaudet, C. J. Bacchi, N. Yarlett, J. J. Plattner, Y. Freund, C. Ding, T. Akama, Y.-K. Zhang, R. Brun, M. Kaiser, I. Scandale, R. Don, SCYX-7158, an orally-active benzoxaborole for the treatment of stage 2 human African trypanosomiasis. PLOS Negl. Trop. Dis. 5, e1151 (2011).
22. R. T. Jacobs, J. J. Plattner, B. Nare, S. A. Wring, D. Chen, Y. Freund, E. G. Gaukel, M. D. Orr, J. B. Perales, M. Jenks, R. A. Noe, J. M. Sligar, Y.-K. Zhang, C. J. Bacchi, N. Yarlett, R. Don, Benzoxaboroles: A new class of potential drugs for human African trypanosomiasis. Future Med. Chem. 3, 1259–1278 (2011).
23. A. Casañal, A. Kumar, C. H. Hill, A. D. Easter, P. Emsley, G. Degliesposti, Y. Gordiyenko, B. Santhanam, J. Wolf, K. Wiederhold, G. L. Dornan, M. Skehel, C. V. Robinson, L. A. Passmore, Architecture of eukaryotic mRNA 3′-end processing machinery. Science 358, 1056–1059 (2017).
24. M. Clerici, M. Faini, R. Aebersold, M. Jinek, Structural insights into the assembly and polyA signal recognition mechanism of the human CPSF complex. eLife 6, e33111 (2017).
25. M. Clerici, M. Faini, L. M. Muckenfuss, R. Aebersold, M. Jinek, Structural basis of AAUAAA polyadenylation signal recognition by the human CPSF complex. Nat. Struct. Mol. Biol. 25, 135–138 (2018).
26. Y. Sun, Y. Zhang, K. Hamilton, J. L. Manley, Y. Shi, T. Walz, L. Tong, Molecular basis for the recognition of the human AAUAAA polyadenylation signal. Proc. Natl. Acad. Sci. U.S.A. 115, E1419–E1428 (2018).
27. A. Palencia, R.-J. Liu, M. Lukarska, J. Gut, A. Bougdour, B. Touquet, E.-D. Wang, X. Li, M. R. K. Alley, Y. R. Freund, P. J. Rosenthal, M.-A. Hakimi, S. Cusack, Cryptosporidium and Toxoplasma parasites are inhibited by a benzoxaborole targeting leucyl-tRNA synthetase. Antimicrob. Agents Chemother. 60, 5817–5827 (2016).
28. C. D. Huston, T. Spangenberg, J. Burrows, P. Willis, T. N. C. Wells, W. van Voorhis, A proposed target product profile and developmental cascade for new cryptosporidiosis treatments. PLOS Negl. Trop. Dis. 9, e0003987 (2015).
29. U. H. Manjunatha, A. T. Chao, F. J. Leong, T. T. Diagana, Cryptosporidiosis drug discovery: Opportunities and challenges. ACS Infect. Dis. 2, 530–537 (2016).
30. S. Vinayak, M. C. Pawlowic, A. Sateriale, C. F. Brooks, C. J. Studstill, Y. Bar-Peled, M. J. Cipriano, B. Striepen, Genetic modification of the diarrhoeal pathogen Cryptosporidium parvum. Nature 523, 477–480 (2015).
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/cgi/content/full/11/517/eaax7161/DC1https://en.bio-protocol.org/rap.aspx?eid=10.1126/scitranslmed.aax7161https://www.who.int/news-room/fact-sheets/detail/diarrhoeal-diseasehttps://www.who.int/news-room/fact-sheets/detail/diarrhoeal-diseasehttp://stm.sciencemag.org/
-
Swale et al., Sci. Transl. Med. 11, eaax7161 (2019) 6 November 2019
S C I E N C E T R A N S L A T I O N A L M E D I C I N E | R E S E A R C H A R T I C L E
11 of 11
31. G. Wilke, L. J. Funkhouser-Jones, Y. Wang, S. Ravindran, Q. Wang, W. L. Beatty, M. T. Baldridge, K. L. VanDussen, B. Shen, M. S. Kuhlenschmidt, T. B. Kuhlenschmidt, W. H. Witola, T. S. Stappenbeck, L. D. Sibley, A stem-cell-derived platform enables complete Cryptosporidium development in vitro and genetic tractability. Cell Host Microbe 26, 123–134.e8 (2019).
32. S. Lacroix-Lamandé, R. Mancassola, M. Naciri, F. Laurent, Role of gamma interferon in chemokine expression in the ileum of mice and in a murine intestinal epithelial cell line after Cryptosporidium parvum infection. Infect. Immun. 70, 2090–2099 (2002).
33. M. Barrier, S. Lacroix-Lamandé, R. Mancassola, G. Auray, N. Bernardet, A.-M. Chaussé, S. Uematsu, S. Akira, F. Laurent, Oral and intraperitoneal administration of phosphorothioate oligodeoxynucleotides leads to control of Cryptosporidium parvum infection in neonatal mice. J. Infect. Dis. 193, 1400–1407 (2006).
34. S. Lacroix, R. Mancassola, M. Naciri, F. Laurent, Cryptosporidium parvum-specific mucosal immune response in C57BL/6 neonatal and gamma interferon-deficient mice: Role of tumor necrosis factor alpha in protection. Infect. Immun. 69, 1635–1642 (2001).
35. N. Dimasi, D. Flot, F. Dupeux, J. A. Márquez, Expression, crystallization and X-ray data collection from microcrystals of the extracellular domain of the human inhibitory receptor expressed on myeloid cells IREM-1. Acta Crystallogr. Sect. F Struct. Biol. Cryst. Commun. 63, 204–208 (2007).
36. U. Zander, G. Hoffmann, I. Cornaciu, J.-P. Marquette, G. Papp, C. Landret, G. Seroul, J. Sinoir, M. Röwer, F. Felisaz, S. Rodriguez-Puente, V. Mariaule, P. Murphy, M. Mathieu, F. Cipriani, J. A. Márquez, Automated harvesting and processing of protein crystals through laser photoablation. Acta Crystallogr. D Struct. Biol. 72, 454–466 (2016).
37. P. Emsley, K. Cowtan, Coot: Model-building tools for molecular graphics. Acta Crystallogr. D Biol. Crystallogr. 60, 2126–2132 (2004).
38. G. N. Murshudov, A. A. Vagin, E. J. Dodson, Refinement of macromolecular structures by the maximum-likelihood method. Acta Crystallogr. D Biol. Crystallogr. 53, 240–255 (1997).
39. K. Arnold, L. Bordoli, J. Kopp, T. Schwede, The SWISS-MODEL workspace: A web-based environment for protein structure homology modelling. Bioinformatics 22, 195–201 (2006).
Acknowledgments: We acknowledge the EMBL HTX facility (Grenoble), the EMBL Protein Expression and Purification Facility (Heidelberg), and the ESRF staff for support with the macromolecular crystallography beamlines. We acknowledge U. Manjunatha and T. Diagana for providing KDU691, and B. Striepen and A. Sateriale for the valuable advice to set up
Cryptosporidium transgenesis. We also acknowledge the Experimental Infectiology Platform: PFIE, UE-1277, INRA Centre Val de Loire, Nouzilly, France. We are very thankful to C. Beaugé’s team for rearing the mice, and G. Fort for the technical support. We thank the teams of E. Guitton and T. Chaumeil, particularly F. Sarcé-Faurie, for following up on the mice, and veterinarians J. Cognié and N. Kasal-Hoc for animal surgery. Funding: The work was supported by ERC Consolidator grant no. 614880 HostingTOXO (to M.-A.H), the Laboratoire d’Excellence (LabEx) ParaFrap (ANR-11-LABX- 0024; to M.-A.H., A.P., and C.S.), the ANR grant no. RC18114CC (to A.P.), the FINOVI grant no. RC17039CC (to A.P.), and the IDEX-IRS program of the University of Grenoble Alpes grant no. 7C043IAB (to A.P). The structural biology work was supported by the iNEXT program grant no. 653706 (to A.P.), funded by the Horizon 2020 program of the European Union. Cryptosporidium transgenesis work was supported by an INRA young researcher starting grant to J.T. Author contributions: M.-A.H., F.L., and A.P. conceptualized the research. A.P. and M.-A.H. performed bioinformatic predictions and analysis. C.S. and A.P. expressed, purified, crystallized, and collected crystallographic data of ChCPSF3. A.P. and C.S. analyzed data and determined crystal structures. C.S. performed endonuclease activity and inhibition assays. C.S. and A.B. conducted genetic work in T. gondii on CPSF3 mutated forms. A.P. prepared drug formulations for the animal studies, and F.L. designed in vivo studies and conducted animal experiments together with A.G.-D. A.G.-D. performed in vitro experiments with C. parvum transgenic strains generated by J.T. S.G. performed the electron microscopy studies. All the authors discussed the approved the results. M.-A.H., F.L., A.P., and C.S. wrote the paper. All authors contributed to the editing of the final version. Competing interests: The authors declare that they have no competing interests. Data and materials availability: All data associated with this study are present in the paper or the Supplementary Materials. The crystal structure of unbound ChCPSF3 is deposited to the Protein Data Bank in Europe (PDBe) with the accession number 6Q5A; the structure of the complex formed by ChCPSF3 with AN3661 is deposited with the accession number 6Q55.
Submitted 16 April 2019Accepted 18 October 2019Published 6 November 201910.1126/scitranslmed.aax7161
Citation: C. Swale, A. Bougdour, A. Gnahoui-David, J. Tottey, S. Georgeault, F. Laurent, A. Palencia, M.-A. Hakimi, Metal-captured inhibition of pre-mRNA processing activity by CPSF3 controls Cryptosporidium infection. Sci. Transl. Med. 11, eaax7161 (2019).
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/
-
infectionCryptosporidiumMetal-captured inhibition of pre-mRNA processing activity by CPSF3 controls
Andrés Palencia and Mohamed-Ali HakimiChristopher Swale, Alexandre Bougdour, Audrey Gnahoui-David, Julie Tottey, Sonia Georgeault, Fabrice Laurent,
DOI: 10.1126/scitranslmed.aax7161, eaax7161.11Sci Transl Med
insight into how oxabaroles inhibit apicomplexan parasites.parasitic pre-mRNA processing. This study proposes a potential treatment against cryptosporidiosis and provides
by the benzoxabarole resulted from inhibition ofCryptosporidium(CPSF3) suggested that the selective targeting of of the benzoxabarole bound to the active site of parasitic cleavage and polyadenylation specificity factor 3 both neonatal and immunocompromised mouse models of infection. Biochemical assays and a cocrystal structurefound to be effective against other apicomplexans, controlled cryptosporidiosis better than the standard of care in
. show that a benzoxabarole, previouslyet aland treatment can be ineffective in vulnerable patient groups. Swale causes potentially life-threatening gastrointestinal symptoms,CryptosporidiumThe apicomplexan parasite
CryptosporidiumControlling
ARTICLE TOOLS http://stm.sciencemag.org/content/11/517/eaax7161
MATERIALSSUPPLEMENTARY http://stm.sciencemag.org/content/suppl/2019/11/04/11.517.eaax7161.DC1
CONTENTRELATED
http://stm.sciencemag.org/content/scitransmed/12/563/eaba8412.fullhttp://stm.sciencemag.org/content/scitransmed/12/563/eaba0565.fullhttp://stm.sciencemag.org/content/scitransmed/11/488/eaau8581.fullhttp://stm.sciencemag.org/content/scitransmed/10/464/eaam7019.fullhttp://stm.sciencemag.org/content/scitransmed/11/491/eaav3523.full
REFERENCES
http://stm.sciencemag.org/content/11/517/eaax7161#BIBLThis article cites 38 articles, 9 of which you can access for free
PERMISSIONS http://www.sciencemag.org/help/reprints-and-permissions
Terms of ServiceUse of this article is subject to the
registered trademark of AAAS. is aScience Translational MedicineScience, 1200 New York Avenue NW, Washington, DC 20005. The title
(ISSN 1946-6242) is published by the American Association for the Advancement ofScience Translational Medicine
of Science. No claim to original U.S. Government WorksCopyright © 2019 The Authors, some rights reserved; exclusive licensee American Association for the Advancement
by guest on June 18, 2021http://stm
.sciencemag.org/
Dow
nloaded from
http://stm.sciencemag.org/content/11/517/eaax7161http://stm.sciencemag.org/content/suppl/2019/11/04/11.517.eaax7161.DC1http://stm.sciencemag.org/content/scitransmed/11/491/eaav3523.fullhttp://stm.sciencemag.org/content/scitransmed/10/464/eaam7019.fullhttp://stm.sciencemag.org/content/scitransmed/11/488/eaau8581.fullhttp://stm.sciencemag.org/content/scitransmed/12/563/eaba0565.fullhttp://stm.sciencemag.org/content/scitransmed/12/563/eaba8412.fullhttp://stm.sciencemag.org/content/11/517/eaax7161#BIBLhttp://www.sciencemag.org/help/reprints-and-permissionshttp://www.sciencemag.org/about/terms-servicehttp://stm.sciencemag.org/