Implant–abutment connections: influence of the design on...
Transcript of Implant–abutment connections: influence of the design on...
Implant–abutment connections: influence of the designon the microgap and their fatigue and fracture behavior of dentalimplants
F. J. Gil • M. Herrero-Climent • P. Lazaro •
J. V. Rios
Received: 29 December 2013 / Accepted: 28 March 2014
� Springer Science+Business Media New York 2014
Abstract Microgap between implant and abutment can
produce biological and mechanical problems such as peri-
implantitis and/or fatigue failures. The aim of this study
was to evaluate microgap size and fatigue behavior of
external and internal connections. In both systems the
torque to tighten the abutment screw of single crown
abutments was 45 Ncm. Fifty implants for each connection
type were studied. One subgroup (n = 5) was used by the
observation and evaluation of the microgap, other (n = 5)
was tested for fracture strength and the other (n = 40) was
subjected to dynamic loading. The internal connection
presents a lower microgap than the external ones. From
fatigue results, the external hexagon interface showed
superior result compared to the internal hexagon interfaces.
The tolerances in the internal connections are better and
favour the fatigue behavior but this factor alone is not
sufficient to improve the fatigue response in relation to the
external connections when the screw is subjected at the
same torque. The external system presents a higher value
of the area than the internal and it produces a better load
distribution. Microgaps and mechanical properties are very
important for the long-term behavior of the dental implants
and these aspects should be known by the implantologists.
1 Introduction
Most dental implant systems consist of two components: the
implant and the abutment. The first is the endosteal compo-
nent, which is placed in the first surgical phase, and the
second is the transmucosal connection, which is generally
attached after implant osseointegration to support the pros-
thetic restoration. Colonization of oral microorganisms
through gaps between these parts may produce soft tissue
inflammation or the failure of peri-implantitis treatment [1].
During chewing and biting, the prosthetic restoration
and the implant–abutment connection is affected by vari-
ous physiological forces, on a single molar implant this
might be about 120 N in the axial direction [2, 3]. In
addition, there might be a short force maximum up to an
average of 847 N for men and 595 N for women [4].
Cyclic loading forces during physiological function that do
not exceed the maximum strength of an implant–abutment
connection might loosen the implant–abutment connection
gradually or make it fail suddenly due to fatigue. The
reason for the fatigue failure is either a lack of force fitting
or form-closure of the connection design. The critical
reason for loosening of the implant–abutment connection is
the loss of preload at the abutment screw and the resulting
unscrewing or fatigue failure of the screw material [2].
An analysis has been recently published on implant
related complications which calculated a cumulative inci-
dence of connection related complications (screw loosen-
ing or fatigue) of 7.3 % after 5 years of clinical service [5].
Maeda et al. [6] and Khraisat [7, 8] studied the stress
distribution patterns between implants with external-hexa-
gon or internal-hexagon connection systems using in vitro
models. The results showed that almost the same force dis-
tribution pattern was found under vertical load in both sys-
tems. Fixtures with external-hexagon showed an increase in
F. J. Gil (&)
Department of Materials Science and Metallurgical Engineering,
ETSEIB, Universitat Politecnica de Catalunya, Av. Diagonal
647, 08028 Barcelona, Spain
e-mail: [email protected]
M. Herrero-Climent � P. Lazaro � J. V. Rios
Faculty of Dentistry, Universidad de Sevilla, C/Avicena s/n,
41004 Seville, Spain
123
J Mater Sci: Mater Med
DOI 10.1007/s10856-014-5211-7
strain at the cervical area under horizontal load, while
internal-hexagon fixtures the strain was at the fixture tip area.
Within limitations of the model study, it was suggested that
fixtures with internal-hexagonal showed widely spread force
distribution down to the fixture tip compared with external-
hexagon.
The problem of a microgap between implant and
abutment is biological and also mechanical. The biolog-
ical problem relates to the presence of bacteria that have
been found in the apical portion of the abutment screw [9,
10]; in vivo, this could produce a bacterial reservoir that
could interfere with the long-term health of the peri
implant tissues. The mechanical problem relates the mi-
cromovements and possible loosening or fracture due to
the fatigue of screw-retained abutments. Huang et al. [11]
studied the relationship between fractures surface mor-
phology and applied stress level for dental abutment
screw loaded in cyclic fatigue. They found a linear rela-
tionship between the number of cycles and the stress
applied to the screws.
The purpose of this study was to evaluate and compare
the implant–abutment microgaps for the two-piece abut-
ments for external hexagon joints (external connection) and
comparative for internal-cone joints with hexagon antiro-
tational device (internal connection). Furthermore, the
fatigue behavior was evaluated for each connection type.
The dental implants were sourced from the same implant
manufacturer, with identical surface and with the same
retention force of the connection screws.
2 Materials and methods
Two implant systems with the implant–abutment were
evaluated. The dental implants were fabricated by Klock-
ner� (SK2, with external connection and Essential Cone,
with internal connection). These specific systems are very
similar to other dental implants existing in the market with
comparable contact areas, and the results can be general-
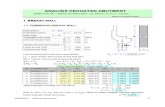
ized. Figure 1 illustrates the designs studied. In both sys-
tems the torque to tighten the abutment screw of single
crown abutments was 45 Ncm, leading to better force-fit.
Fifty dental implants for each connection type were stud-
ied. One subgroup (n = 5) was used for observation and
evaluation of the microgap, another subgroup (n = 5) was
tested for fracture strength and the remainder (n = 40) was
subjected to dynamic loading.
For evaluation of the microgaps, the implant–abutment
systems were embedded in a glycol methacrylate resin.
After polymerization, each specimen was sectioned along
its longitudinal axis with a high-precision diamond disc. A
total of three slides were obtained for each implant. The
samples were observed by scanning electron microscopy
(JEOL 6400, Japan) coupled with an analysis image sys-
tem. The sensitivity of the measures was 0.2 m. This
method is very similar at the technique to evaluate the
Fig. 1 a Implant–abutment with internal connection and b implant–
abutment with external connection
J Mater Sci: Mater Med
123
implant–abutment gap of an external hexagon implant
system as a function of radius proposed by Coelho [12].
Five flexural tests at 308 were conducted, at the selected
inclination, to determine the yield strength of the material
and the ultimate flexion strength. The resulting percentages
of yield strength that were obtained from these tests,
ranging from 60 to 90 %, were later used to perform fati-
gue tests to obtain the number of cycles until fracture.
The fatigue behavior and the fatigue limit of the pro-
totype were set using the Wohler’s curves (stress – number
of cycles) that describe the relation between the amplitude
of the cyclical tensions and the number of cycles to break.
During the test, the implant–abutment system was sub-
jected to both cyclical compressive and lateral forces,
without any lateral constraint. Forty specimens were tested.
The tests were performed in simulated body fluid [13] at
37 �C with the servo-hydraulic testing machine MTS
Bionix 858, which is specially designed to test biomaterials
because is equipped with triaxial stresses (tension, com-
pression and torsion). The torsion of 38 was applied in the
fatigue test, this value is the typical regarding the teeth
movement. This machine was equipped with a load cell
MTS of 10 KN, and controlled by means of a PC equipped
with the software TESTAR II�.
The tests were performed following the guidelines pre-
viously published by the FDA at the Class II Special
Controls Guidance Documents: Roots-form Endosseous
Dental Implants and Endosseous Dental Implants–Abut-
ments and the ISO 14801:2007. The tested implants sup-
ported an abutment that was in line with the axis of the
implant. The testing setup clamped the implant so that the
implant’s long axis made a 30� angle with the loading
direction of the testing machine and, consequently a flex-
ural load was applied (Fig. 2). The implants were fixed
with a 30� inclination from the z-axis of the traction–
compression machine. A 30� angle to the z-axis of the
tensile–compression machine is recommended by the
standards of the FDA as the most unfavorable position.
Moreover, the implant was placed 3 mm below the antic-
ipated crestal bone level, simulating 3 mm of bone
resorption.
The aim was to find the level of stress at which the
sample supported five million cycles, and which will be
considered the fatigue limit. Seven of the tests that were
carried out to determine the level of stress analyzed the
fatigue limit whilst three tests focused on the rest of the
tested stresses. The implants were loaded with a sinusoidal
function of fatigue at a frequency of 15 Hz and the rela-
tionship between maximum and minimum applied stress
was 10 %. The tests were performed at room temperature.
The obtained data was represented as number of cycles to
failure as a function of applied stress. The first stress
applied was 1450 N, a load lightly lower that the maximum
compressive strength, and the following loads decreased by
around a 10 %.
The data were statistically analysed using Student’s
t tests and one-way ANOVA tables with Tuckey’s multiple
comparison in order to evaluate statistically significant
differences between sample groups. The differences were
considered to be significant when P value \ 0.01. All
statistical analyses were performed with Minitab software
(Minitab release 13.0).
3 Experimental results
The gaps obtained are presented in Table 1. In some cases,
excellent adaptation between implant and screw-retained
abutment was observed as the separation distance was
lower than the bacteria diameter and consequently would
not permit infiltration of microorganisms. In some cases,
the connection is like cold-welding where the distance is
zero. The internal connection design presented a lower
Fig. 2 Scheme of the experimental setup during flexural and fatigue
tests
J Mater Sci: Mater Med
123
microgap than the external design with statistically sig-
nificant differences. In Fig. 3 we can observe an example
for each microgap connection type.
The fatigue behavior of each type of abutment–implant
connection can be observed in the S–N curves in Fig. 4.
Statistically, the external hexagon interface presented big-
ger fatigue long life than the internal hexagon interfaces.
A loss of retention between abutment and implant was
assessed as a failure. In all cases the failures were caused
by abutment screw loosening and later fracture, but not due
to destruction of the implant neck or shoulder. Analysis of
fractured screws by SEM revealed that the mode and the
region of fracture were the same for the two systems
evaluated. Fatigue striations were seen on the SEM
micrographs (Fig. 5). Such striations are an indication of
fatigue failure. Overloads or fast fracture zone, that is, the
portions of the components where final catastrophic failure
occurred were also observed. The fracture surfaces were
similar for all implants, as can be observed in Fig. 6. The
fractures are in the connection zone and fracture the body
of the implant. The international standards for fracture
fatigue behavior indicates that the fractures in the dental
implants must be localized in the connection abutment–
implant [14, 15].
4 Discussion
Binon and Curtis [16] indicated tolerances of manufactur-
ing as a reason for the described loose-fit of the prefabri-
cated parts and requested the manufacturer to improve the
fit of implants components. In loose-fit situations, the
possibility of horizontal movement and micro rotation
between implant and abutment screw and lower that the
forces to tighten it, micromovements could have led to a
progressive unscrewing of the abutment screw under con-
ditions dynamic loading. In our study, the main cause of
the high fatigue life of the external connection is due to the
size of the resistant section, the external system presents a
higher value of the area than the internal. This fact pro-
duces a better load distribution of the load and this is a
main factor that explains the differences in the mechanical
properties. The tolerances in the internal connections are
better and favour the fatigue behavior of the internal con-
nection system; however this factor is not sufficient to
improve the fatigue response in relation to the external
connections. Raoofi et al. [17] studied by finite element
analysis that the stress concentration decreased when the
internal surface area increase.
Many authors indicate that the external connections in
different implant–abutment systems present better fatigue
behavior due to the differences in force-fit in the connec-
tion design [2, 3, 5]. In all cases, the external connection
systems studied present a higher force-fit than the internal.
In this contribution, the force-fit was constant and conse-
quently this factor is not considered [1–3, 5].
Freitas-Junior et al. [18] evaluate the reliability and
failure modes of anterior single-unit restorations in internal
conical interface (ICI) implants using step-stress acceler-
ated life testing (SSALT). A number of implants were
used: Forty two ICI implants were distributed in two
groups (n = 21 each): AT-OsseoSpeedTM TX (Astra Tech,
Waltham, MA, USA) and another group SV-Duocon Sys-
tem Line, Morse Taper (Signo Vinces Ltda., Campo Largo,
PR, Brazil). The corresponding abutments were screwed to
Table 1 Measurements of the microgap for internal and external
connections
Type of connection Average of microgap (lm)
Internal 0.97 (0.09)
External 1.22 (0.08)
Each type of connection was measured in five different implants, the
total measures for each connection was 350. The result is the average
of all measurements and into brackets is the standard deviation. The
results present statistically differences with P \ 0.01
a
60 µm
0.4573 µm
0.4582 µm
4.673 µm 2.782 µm
60 µm
b
Fig. 3 Observation by optical microscope with image analysis the
microgap of two types of connections: a Internal and b external
J Mater Sci: Mater Med
123
the implants and standardized maxillary central incisor
metal crowns were cemented and subjected to SSALT in
water. Use-level probability Weibull curves and reliability
for a mission of 50,000 cycles at 200 N were calculated.
The tests showed no significant difference between the
groups tested (P [ 0.27) in all specimens of both designs
of ICI connection. The chief failure mode was abutment
fracture at the conical joint region and screw fracture at
neck’s region. Failure modes were similar.
The short external hexagon does not stabilize the con-
nection against lateral loads, and so the screws have to
absorb most of the load. This is usual in the implants with
height of the external hexagon around 0.6 mm. One reason
for the still good outcomes of this group may be the
improvements in screw design made by the manufacturer
and the increase of the height of the external hexagon. In
this study the height of the external hexagon was 1.8 mm.
This height produces an increase of the stability and an
increase of the flexural load transfer hexagon as shows the
scheme of Fig. 7.
Each implant–abutment interface has its advantages and
disadvantages. According to Maeda et al. [6] the external
hexagon interface has advantages such as suitability for the
two stage method, provision of an anti-rotation mechanism,
retrievability and compatibility among different systems.
However, increased screw loosening, component fracture,
and difficulty in seating abutments in deep subgingival
Fig. 4 S–N curves for each
connection type
Crack nucleation
Crack propagation
Fig. 5 Fracture surface observed by scanning electron microscope
Fig. 6 Fracture of the dental implants
J Mater Sci: Mater Med
123
tissues are problems commonly experienced with external
hexagon connectors.
The advantages of the internal hexagon following Ma-
eda are: ease in abutment connection, suitability for one
stage implant installation, higher stability and suitability
for single-tooth restoration, higher resistance to lateral
loads due to the lower centre of rotation and better force
distribution [6].
5 Conclusion
The internal connection had a smaller microgap than the
external ones with significant statistical differences. Very
good adaptation between the implant and the screw-
retained abutment were observed, in many cases the dis-
tances were smaller than the bacteria diameter and conse-
quently is not possible an infiltration of microorganisms.
The fatigue behavior of the external hexagon interface
presented superior result compared to the internal hexagon
interfaces. The high fatigue life of the external connection
is due to the size of the resistant section. This fact produces
a better load distribution of the load and this is a main
factor which explains the differences in the mechanical
properties.
Acknowledgments The authors are grateful to the CICYT
MAT2012-30706 and Generalitat de Catalunya (CTP Project) and
Andorra Government for funding the present work and to Klockner,
S.L. for kindly donating the material. The authors do not present any
interest conflict in this work
References
1. Steinebrunner L, Wolfart S, Bobmann K, Kern M. In vitro
evaluation of bacterial leakage along the implant–abutment
interface of different implant systems. Int J Oral Maxillofac
Implant. 2005;20:875–81.
2. Steinebrunner L, Wolfart S, Bobmann K, Kern M. Implant–
abutment interface design affects fatigue and fracture strength of
implants. Clin Oral Implant Res. 2008;19:1276–84.
3. Ritcher EJ. In vivo vertical forces on implants. Int J Oral Max-
illofac Implant. 1995;10:99–108.
4. Waltimo A. Studies on human bite force: a novel bite force
recorder and its clinical applications. Prosthetic dentistry. Hel-
sinki: Med-Habilitation; 1995. p. 199–210.
5. Pjetursson BE, Tan Y, Lang NP, Bragger U, Egger M, Zwahlen
M. A systematic review of the survival and complication rates of
fixed partial dentures (fpds) after an observation period of at least
5 years. Clin Oral Implant Res. 2004;15:625–42.
6. Maeda Y, Satoh T, Sogo M. In vitro differences of stress con-
centrations for internal and external hex implant–abutment con-
nections: a short communication. J. Oral Rehabil. 2006;33:75–8.
7. Khraisat A, Stegaroiu R, Nomura S, Miyakawa O. Fatigue
resistance of two implant/abutment joint designs. J Prosthet Dent.
2002;88:604–10.
8. Khraisat A. Stability of implant–abutment interface with a
hexagon mediated joint: failure mode and bending resistance.
Clin Implant Dent Relat Res. 2005;7(4):221–8.
9. Quirynen M, van Steenberghe D. Bacterial colonization of the
internal part of two stage implants: an in vivo study. Clin Oral
Implant Res. 1993;4(3):158–61.
10. Piatelli A, Scarano A, Paolantonio M. Fluids and microbial
penetration in the internal part of cement-retained versus screw-
retained implant–abutment connections. J Periodontol. 2001;72:
1146–50.
11. Huang HM, Tsai CM, Chang CC, Lin CT, Lee SY. Evaluation of
loading conditions on fatigue-failed implants by fracture surface
analysis. Int J Oral Maxillofac Implant. 2005;20(6):854–9.
12. Coelho AL, Suzuki M, Dibart S, Da Siva N, Coelho PG. Cross-
sectional analysis of the implant–abutment interface. J Oral
Rehabil. 2007;34(7):508–16.
13. Manero JM, Salsench J, Nogueras J, Aparicio C, Padros A,
Balcells M, Gil FJ, Planell JA. Growth of bioactive surfaces on
dental implants. Implant Dent. 2002;11:170–5.
14. Gil FJ, Aparicio C, Manero JM, Padros A. Influence of the height
of the external hexagon and surface treatment on fatigue life of
commercially pure titanium dental implants. Int J Oral Maxillofac
Implant. 2009;24:583–90.
15. Rodrıguez-Hernandez A, Juarez A, Engel E, Gil FJ. Streptococ-
cus sanguinis adhesion on titanium rough surfaces: effect of shot
blasting particles. J Mater Sci Mater Med. 2010;22:1913–22.
16. Binon PP, Curtis DA. A classification system to measure the
implant–abutment microgap. Int J Oral Maxillofac Implant. 2007;
22(6):879–85.
17. Raoofi S, Khademi M, Amid R, Kadkhodazadeh M. Moyahhedi
M.R. Comparison of the effect of three abutment–implant con-
nections on stress distribution the internal surface on dental
implants: a finite element analysis. J Dent Res Clin Dent Pros-
pect. 2013;7(3):132–9.
18. Freitas-Junior AC, Almeida EO, Bonfante EA, Silva NRFA,
Coelho PG. Reliability and failure modes of internal conical
dental implant connections. Clin Oral Implant Res. 2012;1:1–6.
doi:10.1111/j.1600-0501.2012.02443.x.
Fig. 7 Scheme of the influence of the external hexagon height of the
implant on the mechanical properties of the external connections
J Mater Sci: Mater Med
123














![Internal - Luciano Chinellato · AnyOne® Internal è -P_[\YL 3L]LS 7YVZ[OLZPZ EZ Post Milling Abutment Angled Abutment CCM Abutment Temporary Abutment [Titanium] Temporary Abutment](https://static.fdocuments.net/doc/165x107/5c038f7909d3f2156d8cd7fd/internal-luciano-anyone-internal-e-pyl-3lls-7yvzolzpz-ez-post-milling.jpg)