Hypercortisolemia also has been shown to have an …repository.edgehill.ac.uk/7827/1/Lipid...
Transcript of Hypercortisolemia also has been shown to have an …repository.edgehill.ac.uk/7827/1/Lipid...

Lipid Metabolism and Hormonal Interactions: Impact on Cardiovascular Disease & Healthy Aging
Populations in developed nations are aging gradually; it is predicted that by 2050 almost one
quarter of the world’s population will be over 60 years, more than twice the figure at the turn
of the 20th century. Although we are living longer this does not mean the extra years will be
spent in good health. Cardiovascular diseases are the primary cause of ill health and their
prevalence increases with age. Traditionally lipid biomarkers have been utilized to stratify
disease risk and predict the onset of cardiovascular events. However, recent evidence
suggests that hormonal interplay with lipid metabolism could have a significant role to play
in modulating cardiovascular disease risk. This review will explore recent findings which
have investigated the role hormones have on the dynamics of lipid metabolism. The aim is to
offer an insight into potential avenues for therapeutic intervention.
Keywords: Aging, cardiovascular disease, growth hormones, leptin, lipid metabolism, stress hormones
Due to improvements in health care, medicine and living standards, the proportion of the
aged population in the developed world is increasing gradually. It is predicted that by the year
2050 ~22% of the world’s population will be over 60 years, more than twice the figure at the
turn of the 20th century[1]. In the United Kingdom (UK), life expectancy at the start of the
20th century was 50.4 and 53.9 years for males and females respectively, while at the end of
the 20th century the corresponding numbers had risen dramatically to 74.6 and 79.6 years,
respectively[2]. This trend has gained further momentum in the 21st century. Based on the
most recently available data, a child born in England or Wales between 2010-2012 can expect
to live to 79.1 years if male and 89.2 years if female[3]. It has also been revealed that
1
2
3
4
5
6
7
8
9
10
11
12
13
14
1516
17
18
19
20
21
22
23
24
25
26

between 1971 and 2009 the proportion of the UK population >=75 years increased from 4.7%
to 7.8% and this figure is projected to rise to 11.7% by 2031[4](FIGURE 1). There are also
now five-times more people aged over 85 years in the UK than there were in 1951[2] and it is
predicted that by 2018 the number of individuals aged 65 years or over will outnumber those
below 16 years. It is anticipated that by the year 2051 almost 25% of the UK population will
be over 65 years, while 5% of the UK population will be over 85 years[3]. These trends are
not confined to the UK; the USA has also witnessed a demographic change. In 1950s
America, 8.1% of the population consisted of those individuals >=65 years. As of 2012 this
figure stands at 13.7% and is predicted to rise to ~20.2% by 2050[5]. Remarkably it is
estimated that by 2050, Japan’s population will be made up of 40% of people >=65 years,
making it the most rapidly aging nation[6]. China will also be confronted with an
overwhelming challenge as the number of people >=60 years is predicted to reach ~350
million by 2050[6].
Such dramatic alterations in population demographics present a major challenge to
governments, scientists and health professionals alike, because as the population ages it is
becoming increasingly important to develop strategies to deal with the high incidence of
disease in older people. In the UK those ≥65 years are the main users of the National Health
Service (NHS)[7]. In the USA it has been well established that personal health care costs rise
sharply with age, as the oldest old consume up to three times more health care per person
than those aged between 65-74 years [8]. To help relive the health care burden brought about
by an aging population the Japanese government introduced compulsory public long-term
care insurance to help relive the health care burden brought about by an aging population [9].
1
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51

Among the chronic conditions that hamper older people and prevent them benefitting
from a healthy extra few years of life; diseases of the heart and circulatory system, which are
referred to as cardiovascular disease (CVD) are the most common. The reason is that
although death rates from CVD have halved in the last two decades; its prevalence still
increases markedly with advancing age (FIGURE 2) [10]. For example in the UK CVD was
the principal cause of death in 2009, accounting for ~ 200,000 fatalities and its morbidity
remained constant in older age groups [11]. This costs the UK economy > £30 billion per
annum[12], therefore, it is clear that maintaining cardiovascular (CV) health is of central
importance in those countries with an aging population.
Despite the availability of a large number of risk factors for CVD, traditionally health
professionals have relied on lipid biomarkers markers as the gold standard determinant of
CVD risk. The reason is a long established relationship between plasma cholesterol levels
and CVD risk [13]. The biological underpinnings of this relationship are in part due to the
strong association that exists between elevated total cholesterol/low density lipoprotein
cholesterol (LDL-C) and atherosclerosis[14]. Atherosclerosis is a vascular process which is
considered the underlying pathological explanation for coronary heart disease (CHD) and
stroke which are the principle clinical manifestations of CVD. Unlike total cholesterol and
LDL-C, high density lipoprotein cholesterol (HDL-C) has been suggested to have an anti-
atherogenic role to play in reducing CVD risk. This becomes apparent in patients who have
HDL-C levels below 35 mg/dL, as their relative risk of CHD can be almost three times higher
than normal[15, 16]. Mechanistically HDL-C plays a role in reducing CVD risk by taking
part in reverse cholesterol transport (RCT), a process which offers the only route for removal
of excess cholesterol from the body[17]. Its role begins when it acquires excess cholesterol
from the cell membranes of peripheral tissue, this result in the generation of cholesteryl ester-
rich, mature HDL particles. These mature HDLs then transfer the excess cholesterol to the
2
52
53
54
55
56
57
58
59
60
61
62
63
64
65
66
67
68
69
70
71
72
73
74
75
76
77

liver where it is taken up by hepatocytes and eventually removed from the body via hepatic
conversion into bile acids and subsequent fecal excretion. Recently the lead author developed
a computational model which consolidated the importance of RCT for sustaining whole-body
cholesterol balance during aging[18]. The findings from computational investigations such as
this are important because as outlined RCT acts to ‘fight’ against the arterial deposition of
cholesterol[15, 16]. Moreover it has been recognized that such approaches are needed to
unravel the myriad of mechanistic interactions associated with complex nutrient mediated
biological systems such as lipid metabolism[19].
Lipid based CV risk factors are not exclusively cholesterol based; for over two
decades there has been an established association between circulating triglyceride (TG) levels
and CVD risk. For example, in a recent epidemiological investigation it was found that the
long-term stability of TG values as a correlate for CHD was similar to those of total
cholesterol and blood pressure combined[20]. Mechanistically it remains uncertain how
elevated TGs contribute to CVD risk, however triglyceride-rich lipoproteins (TRLs) have
been tentatively associated with the process of atherosclerosis [21].
It is clear the CVD detection kit of the health professional comes well equipped with a
suite of lipid based parameters that play a key role in the risk stratification and prognosis of
CV events in their patients. It could be argued however, that blood lipids only contribute to
CVD pathologies in a proximate manner and that other underlying factors are the real cause
of CVD. The aim of this paper is to critically appraise the current evidence connecting
hormonal crosstalk with lipid metabolism. The emphasis will be on individuals with a risk of
dyslipidemia due to abnormal hormonal behavior and how this interplay contributes to their
3
78
79
80
81
82
83
84
85
86
87
88
89
90
91
92
93
94
95
96
97
98
99
100
101

overall cardiovascular health. The goal of the paper is to help reveal potential avenues for
therapeutic intervention so that CVD does not persist into old age.
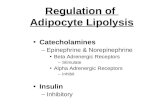
Adipose tissue lipolysis and hormonal interplay
The vast majority of the body’s TGs are located in white adipose tissue. When required
metabolically TGs stored in adipose tissue are broken down to fatty acids and glycerol by
lipolysis [22] (FIGURE 3). Once released into the bloodstream the free fatty acids (FFAs) are
transported to peripheral tissues that require energy for their oxidation. Adipose tissue
lipolysis is the main controller of the body’s supply of fat energy as it controls the release of
FFAs into the circulation[23]. In a healthy adult the basal rate of lipolysis during the fasting
state is determined by hormone sensitive lipase (HSL). HSL is in turn regulated by insulin, a
peptide hormone synthesized by the β-cells of the pancreatic islets. The relationship between
these two hormones plays a crucial role in maintaining fatty acid metabolism. The proximity
of this relationship is emphasized after a meal when insulin is released into the blood and its
presence results in the inhibition of HSL. Thus, the close interaction between insulin and
HSL is responsible for dictating the availability of FFAs to the entire body from white
adipose tissue[24, 25] (FIGURE 3). Further evidence of this interconnectivity is provided
when the HSL gene is knocked out in mice, as this has been shown to result in a reduction in
the sensitivity of insulin [26].
A number of studies have shown an association between dyslipidemia and insulin
resistance (IR). For instance, it has been demonstrated that increased adipocyte lipolysis
augments the hepatic removal of FFAs from the circulation, which in turn causes very low
density lipoproteins (VLDLs) secreted from the liver to have an elevated TG content and
subsequent hypertriglyceridemia; a physiological phenomenon that often accompanies IR
4
102
103
104
105
106
107
108
109
110
111
112
113
114
115
116
117
118
119
120
121
122
123
124
125
126

[27]. The etiology of IR is further complicated by genetic polymorphisms, obesity, nutrition,
smoking, chronological age, inadequate physical activity (PA), and pharmacological
interactions. Among these it is acknowledged that obesity is probably the single most
important contributor to IR [28]. However, from the perspective of this review, it is important
to consider the glucocorticoid interactions which contribute to or even cause IR.
Cortisol
Cortisol is a glucocorticoid (GC) hormone that is released in response to stress and is the end
product of the hypothalamic-pituitary-adrenal (HPA) axis [29, 30]. The synthesis of cortisol
from cholesterol in the adrenal gland is stimulated by adrenocorticotropic hormone (ACTH),
released from the pituitary. Production of ACTH is in turn stimulated by corticotrophin-
releasing hormone (CRH) released by the hypothalamus. Cortisol inhibits the secretion of
CRH, resulting in negative-feedback inhibition of ACTH secretion. Under normal conditions,
cortisol has widespread actions which help to maintain homeostasis after stress. Cortisol
molecules reach all tissues, including the brain, readily penetrating cell membranes to interact
with ubiquitous glucocorticoid receptors (GRs), through which they exert a myriad of diverse
actions. For example, cortisol acts as a physiological antagonist to insulin by promoting
gluconeogenesis; it also promotes the breakdown of lipids, proteins and mobilization of
extra-hepatic amino acids[30]. However, recent evidence strongly suggests that continual
exposure to cortisol leads to abnormal insulin levels, which subsequently impinge on lipid
metabolism. For instance, it has been shown that alterations to adipocyte metabolism, which
result in both lipid mobilization and lipid storage are the result of a decline in insulin
sensitivity caused by hypercortisolemia [30].
5
127
128
129
130
131
132
133
134
135
136
137
138
139
140
141
142
143
144
145
146
147
148
149
150

Recently, in order to establish the molecular mechanism(s) by which cortisol
antagonistically affects insulin, Park and colleagues examined the metabolic production of
cortisol and its biological functions in developing muscle tissue known as myotubes[31].
Their hypothesis centered on the dysregulation of the enzyme 11β-hydroxysteroid
dehydrogenase 1 (11β-HSD1) which catalyzes GCs into their active form. Myotubes were
supplemented with cortisone to catalyze 11β-HSD1 conversion into cortisol, which in turn
inhibited phosphorylation of protein kinase B (Akt) in response to insulin treatment; resulting
in a reduced uptake of insulin-induced glucose. The results were consolidated by the
application of an inhibitor to the enzyme 11β-HSD1 which reversed the antagonizing effects
of cortisol on insulin action[31]. Their results suggest that 11beta-HSD1 dysregulation in
adipose and muscle tissues could be involved in the development of IR. Rectifying this
impairment could potentially be a worthwhile means of improving insulin regulation.
Hypercortisolemia also has been shown to have an impact on a broad range of CV
parameters. For example, it has been shown that there is an association between elevated
cortisol levels and the redistribution of body fat [32]. Moreover, Rosmond and Björntorp
have shown that impairment of the HPA axis can be used as a predictor of CVD by
measuring serum insulin, TGs, LDL-C and HDL-C along with anthropometric
measurements[33]. This detrimental interaction is compounded by age related changes in the
HPA axis as evidenced by Knoops et al who reported that HPA axis activity showed reduced
variability in older age independent of CV risk factors[34]. Similar findings were reported by
Jokinen and Nordstrom. In this longitudinal study of patients with mood disorder, higher
baseline serum cortisol predicted CVD death in male patients. This group also reported that
among older adults, men respond to psychological stress with greater increases in cortisol and
this greater activation of the HPA axis could translate into an elevated risk for CVD[35].
6
151
152
153
154
155
156
157
158
159
160
161
162
163
164
165
166
167
168
169
170
171
172
173
174
175

Hormonal interaction with lipoprotein lipase
Lipoprotein lipase (LPL) is a hydrolytic enzyme synthetized in a variety of tissues, including
cardiac, skeletal and adipose[36]. LPL is responsible for the enzymatic hydrolysis of the TG
core of circulating lipoproteins, including chylomicrons, and VLDL (FIGURE 3). For
instance, absorbed chylomicrons are released into the blood stream via the lymph and as they
pass through the capillaries of peripheral tissue, their TGs are hydrolyzed by LPL. The FFAs
are then absorbed by the peripheral tissue, while the glycerol backbone of the TGs is
returned, via the blood, to the liver and kidneys. Due to the hydrolysis of the core lipids,
chylomicrons reduce in size to become chylomicron remnants which are taken up by the
liver. It is known that nutrient status/state affects LPL; however its regulation is also
significantly influenced by a variety of hormonal interactions. For example,
hypercortisolemia has been correlated with a reduction in lipolysis; something that was
recognized by Samra and colleagues in the late 1990s when it was found that
hypercortisolemia caused a reduction in arterialized plasma TG concentrations[37].
More recently, Sakayama et al. (2012) investigated whether cortisol inhibited cell
proliferation and the expression of LPL in cultures of a human osteosarcoma cell line[38].
The effect of cortisol exposure on the expression of LPL was assessed by quantifying the
activity and mass of LPL. Interestingly, it was found that the rate and activity of LPL were
lower in the cortisol-treated cultures than in the untreated cultures. This study was significant
because it indicated that cortisol inhibited LPL synthesis, and therefore its activity[38]. Other
studies have also suggested a relationship between GC exposure and LPL activity. An
important much older study that is worth outlining examined GR status in adipose tissue from
omental and steroid converting (sc) abdominal adipose tissue in addition to investigating the
activity of LPL. It was found that LPL activity in omental adipose tissue was ~820 nmol
FFA/h.g in both sexes, whereas LPL activity in sc adipose tissue was two to four-fold lower.
7
176
177
178
179
180
181
182
183
184
185
186
187
188
189
190
191
192
193
194
195
196
197
198
199
200

Moreover, LPL activity in sc adipose tissue was two-fold higher in women than in men and a
positive correlation between LPL activity and glucocorticoid binding was also found [39].
More tentative evidence has associated the HPA axis to LPL dysregulation via association
with acute stress[40]. Moreover, dysregulation of the HPA axis has also been linked with
metabolic syndrome in a variety of population groups[41, 42]. These studies strengthen the
case for a role of GCs in LPL dysregulation. However, the evidence is not completely in
favor of a mechanistic relationship between GCs and LPL dysregulation, as a recent study by
Xu and colleagues found that rats suffering from hypercortisolemia had increased adipocyte
lipolysis[43]. In addition, it has been found that when cortisol is administered in combination
with growth hormone (GH), cortisol increased both systemic and regional lipolysis in
humans[44]. To conclude, the available data on how GCs affects lipolysis/LPL activity is
both contradictory and controversial.
The catecholamines epinephrine and norepinephrine have also been show to affect the
activity of LPL by stimulating LPL expression in resting muscle[45]. This is suggested to
occur when catecholamines activate β-adrenergic receptors (β-ARs) stimulating cyclic
adenosine monophosphate (cAMP) levels to rise in adipocytes and triggering lipolysis[46].
Recently, Horton et al (2009) have suggested that women may be more sensitive to beta-
adrenergically mediated systemic lipolysis. In a three day study which compared the effects
of peripherally infused catecholamine’s and lipolysis rate by using infused glycerol; the
authors were able to demonstrate a significant gender difference mainly due to a significantly
greater glycerol turnover during the first 30 minutes of each infusion[47]. Similar to GCs,
catecholamines have also been shown to decrease the activity of LPL. As far back as the
early 1990s, Ong and colleagues used primary cultures of rat adipocytes to establish a
8
201
202
203
204
205
206
207
208
209
210
211
212
213
214
215
216
217
218
219
220
221
222
223
224

decrease in LPL activity that was dependent on the concentration of epinephrine that the cells
were exposed to[48].
Following this investigation a number of other in vitro studies have echoed these
findings and there is an expanding body of data suggesting that obesity is synonymous with
blunted whole-body catecholamine dependent lipolysis. For example, Horowitz and Klein
quantified whole-body and regional lipolytic and adipose tissue blood flow sensitivity to
epinephrine in eight lean and 10 upper body obese (UBO) women. It was found that basal
whole body free fatty acid rate of appearance (FFA Ra) and glycerol rate of appearance
(glycerol Ra) were both greater in obese compared with lean subjects. Epinephrine infusion
significantly increased FFA Ra and glycerol Ra in lean but not obese subjects. In addition,
lipolytic and adipose tissue blood flow (ATBF) sensitivity to epinephrine was blunted in
abdominal but not femoral subcutaneous adipose tissue of obese compared with lean subjects.
It is suggested that lipolytic sensitivity to epinephrine is blunted in women with UBO due to
decreased sensitivity in upper body but not lower body subcutaneous adipose tissue [49].
Jocken et al (2008) then investigated beta-adrenergic stimulation on whole-body and
abdominal subcutaneous adipose tissue lipolysis in lean and obese men and found that in vivo
beta-adrenergically mediated lipolytic response is disrupted systematically and in abdominal
subcutaneous adipose tissue of obese versus lean men[50]. Most recently, Mowers et al have
suggested that pathophysiological obesity is mediated by a chronic inflammatory state, which
in turn is attenuated by the noncanonical IκB kinases IKKε and tank binding kinase 1(TBK1)
enzymes involved in the cellular inflammation response in white adipose tissue. Treatment of
adipocytes with specific inhibitors of these kinases restored β-adrenergic signaling and
lipolysis modulated by tumor necrosis factor alpha (TNFα) and the immune-stimulant
Polyinosinic:polycytidylic acid (Poly (I:C)) [51]. These findings suggest a potential anti-
9
225
226
227
228
229
230
231
232
233
234
235
236
237
238
239
240
241
242
243
244
245
246
247
248

inflammatory therapeutic avenue to re-sharpen catecholamrine lipolysis which merits further
exploration.
It is important to acknowledge that other physiological factors including nutrition, PA
and age can all influence the rate of release of glycerol and FFAs from both adipocyte and
non-adipocyte tissue. For instance, aging has been associated with a decrease of between 55-
60% in LPL activity[52-55] which has been associated with hypertriglyceridemia[56, 57].
Interestingly, it has been shown that over expression of LPL in the skeletal muscle of mice
decreases plasma-TG concentrations, increases HDL-C levels and prevent hyperlipidemia
and obesity in rodents[58, 59]. Thus, based on evidence such as this, it could be suggested
that age associated increases in TG concentration could be underpinned by a decrease in the
activity of LPL. It is possible that PA could help to address such changes in LPL with age, as
a study in young rats has shown that PA associated with walking and standing was especially
important for maintaining a high level of LPL activity[55]. Moreover, in humans it has been
shown that PA can induce LPL in muscle independent of adrenergic-receptor signaling.
Considerable crosstalk also exists between insulin and LPL activity. Specifically, insulin has
been found to provoke LPL gene transcription during adipocyte differentiation. Insulin is also
a regulator of LPL activity and controller of LPL mRNA levels via both posttranscriptional
and posttranslational mechanisms[60, 61].
Growth hormone and IGF-1
Growth hormone (GH) a nocturnal stress hormone with a diversity of metabolic functions
stimulates cell growth, renewal and reproduction in both males and females[62]. GH
operates in concert with Insulin-like growth factor 1 (IGF-1) as part of the IGF1/GH axis.
Once GH is released from the pituitary gland, it circulates in the blood to increase IGF-I
10
249
250
251
252
253
254
255
256
257
258
259
260
261
262
263
264
265
266
267
268
269
270
271
272
273

production in many tissues, leading to a rise in blood IGF-I. Circulating IGF-1 in turn
inhibits further pituitary GH secretion. In humans circulating GH levels peak during
adolescence followed by a continuous decline after 30 years of age at a rate of ∼1% per year
until it reaches negligible levels in those >=60 years [63]. From a longevity perspective,
significant recent attention has focused on the interplay between these two hormones [64].
This interest has centered on mutations in genes involved in this pathway having an effect on
longevity in a wide variety of organisms[65]. IGF-1 is part of a family which includes a range
of insulin-like growth factors (IGFs). IGFs differ from insulin in that they do not circulate
freely in the plasma as they are bound to a network of IGF-binding proteins (IGFBPs).The
interactivity between GH and IGF-1 focuses on IGF-1 regulating GH synthesis via negative
feedback. Both IGF-1 and GH signaling affect a plethora of metabolic pathways; however we
will focus on how their behavior impinges on the dynamics of lipid metabolism.
If cholesterol metabolism and GH interaction is examined it is firstly important to
appreciate that there are a number of changes which cholesterol metabolism can undergo with
age. The clinical manifestation of these perturbations are demonstrated by population studies
which have shown that LDL-C rises with age in both males and females[66]. The reason for
an increase in LDL-C in so many individuals across both genders remains unknown, as there
is there is a paucity of mechanistic evidence and the issue is complicated by inter-individual
differences in nutritional status and PA within the population sample. What is known is that
there is a gradual reduction in the fractional clearance rate of LDL-C from the circulation
with age [67-70]. This is consolidated by evidence that both the number and sensitivity of
hepatic low density lipoprotein receptors (HLDLr) in certain species decreases with age[71].
Recent evidence consolidates these long established findings and also suggested that the
magnitude of change in the activity of the LDL receptor(LDLr) is tissue specific and sex
11
274
275
276
277
278
279
280
281
282
283
284
285
286
287
288
289
290
291
292
293
294
295
296
297
298

dependent[72]. A further putative mechanistic alteration concerns the gradual decline in the
removal of cholesterol from the body via bile acids[73]. Rodent studies have also
demonstrated that the conversion of cholesterol to bile acids declines with age[74-76].
It has been suggested that the age related changes in cholesterol metabolism discussed
above can be attributed to a decrease in GH which is a feature of sarcopenia[77]. As evidence
of this, GH has been shown to increase LDLr and HMG-CoA reductase mRNA expression in
mesangial cells [78]. Additionally, a study which used human liver biopsy specimens from
gallstone patients showed that GH was able to induce HLDLrs two-fold. This was also
accompanied by a 25% decrease in total serum cholesterol[79].Experiments in
hypophysectomised rats have also shown that GH is a regulator of the activity of the rate-
limiting enzyme in bile acid synthesis [80]. This is interesting, as rodent studies have
demonstrated that cholesterol absorption efficiency increases markedly with age[74, 81].
There are also sex differences in cholesterol absorption efficiency, suggesting that other
hormones such as estrogen could modulate cholesterol absorption [82]. From the perspective
of IGF-1, findings have centered on homologs of the scavenger receptor of the B class (SR-
BI), which is a receptor for HDL that mediates cellular uptake of HDL cholesteryl ester
(HDL-CE) and is thus central to RCT. For example in rodents continuous infusion of IGF-1
has been shown to decrease the activity of this receptor[83, 84], tentatively linking IGF-1
with RCT regulation.
If the effects of GH and IGF-1 on adipose tissue dynamics/TG turnover are examined,
there are a number of factors to consider. Firstly, GH stimulates adipocyte differentiation, a
process whereby nascent cells mature into large lipid laden adipocytes. The significance of
this is emphasized when GH deficient subjects are studied, as they suffer from a decreased
12
299
300
301
302
303
304
305
306
307
308
309
310
311
312
313
314
315
316
317
318
319
320
321
322
323

volume of adipocytes, which is only rectifiable by hormonal intervention[85]. Moreover,
growth hormone deficient patients have lower levels of adiponectin[86] when compared to
normal individuals[87]. Adiponectin is an important regulator of fatty acid metabolism will
be discussed in further detail in the next section. GH also affects insulin signaling and it is
putatively suggested that GH exposure is the necessary precursor which allows cells to
become responsive to insulin[88]. GH also provokes lipolysis in adipose tissue which could
be mediated by augmenting LPL expression and/or HSL activity. GH is also released in
response to PA and hypoglycemia and could interact to inhibit leptin; a hormone synthesized
in adipocyte tissue which has been strongly associated with obesity[89] and which will be
explored in further detail in the nutrition and medication section.
Adiponectin and CVD
Adiponectin, an adipocyte-secreted adipokine plays an important role in metabolic and CV
homeostasis[90]. Adiponectin has been shown to be involved in protecting the CV system,
although the mechanisms responsible for this cardio-protective effect are not completely
understood. One way in which it could mediate its protective role is via improving insulin
sensitivity. Awazawa and colleagues (2011) showed that mechanistically adiponectin is
capable of up regulating hepatic insulin receptor substrate 2; a molecule which is a key
modulator of both insulin and IGF-1[91]. Adversely it has been found that in older
populations high adiponectin levels have been demonstrated to have undesirable patient
outcomes. Beatty et al. (2012) reported higher levels of adiponectin were associated with
heart failure and mortality among patients with existing ischemic heart disease[92]; and in a
longitudinal investigation of determinants of CVD in older adults Kizer et al. (2012) also
found an association between adiponectin and mortality, particularly in those with greater
baseline CV dysfunction [93].
13
324
325
326
327
328
329
330
331
332
333
334
335
336
337
338
339
340
341
342
343
344
345
346
347
348

Thyroid Hormones
It has long been established that the catabolic activities of both triiodothyronine (T3) and
thyroxin (T4) has an impact on the physiological dynamics of lipid metabolism. Specifically
they mediate their whole-body influence on lipid metabolism by binding to both the α and β
thyroid receptor which is located ubiquitously throughout the body. Their actions have been
show to lower total and LDL-C and also affect adipocyte biology. Mechanistically, it remains
unclear how thyroid hormones modulate lipid metabolism, however Goldberg et al (2012)
recently proposed that thyroid hormone reduces cholesterol via a non-LDL receptor-mediated
pathway. The authors tested if LDLr expression was required for cholesterol reduction by
treating control and LDLr-knockout mice with two different forms of thyroid hormone. High
doses of the hormones significantly lowered total and VLDL/LDL cholesterol. The reduction
was not associated with increased protein or mRNA expression of the hepatic lipoprotein
receptors LDLr-related protein 1 or scavenger receptor-B1[94]. Recent evidence has also
indicated that thyroid stimulating hormone (TSH) has also been associated with changes to
many of the parameters of lipid metabolism. TSH is responsible for provoking the thyroid
gland into secreting thyroxin into the circulation; where the majority of it binds to proteins in
blood serum while the remaining ~1% circulates as free T4. Recent evidence for the
association between TSH and lipid metabolism comes from a cross-sectional study by Chin et
al. (2014) where lipid and thyroid hormones levels in 708 men were quantified to examine
for correlations between them. It was found that TSH levels were significantly associated
with TG. Free T4 levels were also significantly associated with total cholesterol, LDL-C and
HDL-C [95].
14
349
350
351
352
353
354
355
356
357
358
359
360
361
362
363
364
365
366
367
368
369
370
371
372
373

Nutrition and medication
Diet and medication also have a role to play in contributing to the interplay between lipid
metabolism and hormones. For instance, ingestion of drugs including glucocorticoids, beta
adrenergic antagonists and thiazide diuretics exacerbate IR and dysregulate lipid metabolism.
Evidence of this comes from a large meta-analysis of clinical trial data indicating that
diuretics cause increases in both total and LDL-C. Moreover this analysis suggests that beta
adrenergic antagonists raise TGs. Conversely, it was found that α-adrenergic-antagonists
beneficially affected total cholesterol and modestly raised HDL-C in younger individuals[96].
One caveat is that these findings varied depending on population groups.
Considerable recent focus has centered on leptin, a hormone which is a key regulator
of nutrient intake and which is known to mediate lipid metabolism. Leptin is secreted mainly
by white adipose tissue and acts as a regulator of appetite[97]. Mechanistically leptin operates
by binding to receptors on leptin-responsive neurons of the arcuate nucleus in the mediobasal
hypothalamus decreasing their activity and provoking the brain into releasing a signal that
indicates satiety. Thus, in the short term (the fasting state) leptin concentrations drop while a
brief period of overfeeding provokes an increase in leptin. Therefore, leptin increases in
obesity and decreases during fasting and it has been found that blood circulation levels of
leptin are proportional to adipose tissue mass[98, 99]. Furthermore, it has been found that
leptin can increase skeletal muscle lipoprotein lipase and postprandial lipid metabolism in
mice[100]. Its actions may not be confined to LPL, as recently an independent significant
association was found between IR and leptin concentrations in a population study based in
China[101]. This raises the possibility of leptin being a future biomarker for impaired insulin
sensitivity/the initial stages of pathophysiological obesity. Research in to leptin-lipid
crosstalk is ongoing. However, plasma leptin levels have been correlated with other markers
15
374
375
376
377
378
379
380
381
382
383
384
385
386
387
388
389
390
391
392
393
394
395
396
397
398

of CV health most notably C-reactive protein[102]. However more recently, the European
Male Aging Study reported no relationship between this inflammatory marker and leptin
resistance[103]
By far the most studied dietary regime in aging research is caloric restriction (CR).
CR usually refers to diets providing an energy intake 30%-40% less than the base line
unrestricted intake. It does not lead to malnutrition due to lack of vitamins, minerals or
essential biomolecules and has been shown to improve health at all ages and extend life span
in a variety of organisms[104]. Its potential efficacy in humans remains to be fully
determined. The most concrete evidence to date is provided by experiments by the
Comprehensive Assessment of Long- Term Effects of Reducing Calorie Intake (CALORIE)
[105, 106]. This six year CR diet to assess atherosclerosis risk factors in males and females
(35–82 years) compared to age-matched healthy individuals on typical American diets
(control group) resulted in lowered total cholesterol, LDL cholesterol, triglycerides and
fasting insulin levels[107]. These results are interesting and offers the possibility of CR being
used as a future intervention to improve CV health. Recently, a more traditional dietary
regime with similarities to CR was used to investigate adrenergic and insulin-mediated
regulation of lipolysis in subcutaneous adipose tissue in obese women. The women were
subjected to a six month dietary regime which comprised of a one month very low-calorie
diet (VLCD) followed by a two-month low-calorie diet (LCD) and three month weight
maintenance (WM) diet. The dietary interventions resulted in body weight reduction and
improved insulin sensitivity. Moreover there was an adrenaline-induced increase in lipolysis;
highest in the VLCD and LCD compared with baseline conditions. The lipolysis rate returned
to pre-diet levels during WM [108]. The findings of the study center on women, and studies
16
399
400
401
402
403
404
405
406
407
408
409
410
411
412
413
414
415
416
417
418
419
420
421
422

of this nature are crucial as dyslipidemia in older people is more common in women than
men[109].
Women versus men
Dyslipidemia is more common in older females than males, with almost half of females over
65 years having elevated total cholesterol levels compared to almost a quarter of males[109].
Despite this in the UK death rates from myocardial infarction remains consistently higher in
males than in females across age strata[12]. There are many possible explanations for this
difference; for example as mentioned above there is a sex difference in cholesterol absorption
efficiency. This suggests female sex hormones have a part to play in dyslipidemia in women.
For instance, estrogen significantly augments the output of biliary bile salt, cholesterol and
bile-flow rate. Thus, high levels of estrogen could impact the dynamics of enterohepatic
circulation. In addition hormonal dependent changes to cholesterol absorption are likely to be
a factor in female age-related dyslipidemia. This is logical when it is considered the risk of
CVD increases after the menopause, although it remains to be determined precisely whether
pre or post menopause is the most effective time point for optimal CVD risk reduction [110].
Interestingly a recent study suggests transdermal estradiol (E2) and not oral conjugated
equine estrogen (CEE) may be an effective way of improving vascular atherosclerosis risk in
females [111, 112]. Moreover aerobic training was recently shown to have a positive
influence on the neuro-endocrine system in females[113].
17
423
424
425
426
427
428
429
430
431
432
433
434
435
436
437
438
439
440
441
442
443
444445446447
448
449

Conclusions
To conclude, developed populations are aging which poses a number of health related
challenges; most notably the persistence of CVD into old age. Historically, lipid biomarkers
have been used to predict CVD risk. However, physiological changes that occur during the
ageing process are multi-dimensional and involve the interaction of a myriad of biological
systems with lipid metabolism to modulate the behavior of key lipid based parameters.
Therefore it may no longer be appropriate to rely on the traditional lipid parameters to define
CVD risk in an aging population. This is apparent from the evidence presented in this paper
which highlights the significant role hormonal interactions have on lipid metabolism. Given
that the average lifespan is increasing worldwide and is set to continue to rise; further
understanding of the age-related mechanistic relationships between lipid metabolism and
hormones are certainly merited. This could lead to therapeutic targets which help to prevent
the age dependent pernicious interactions between hormones and lipid metabolism, thus
reducing CVD risk and ultimately promoting healthy aging.
Expert commentary
It is vital that hormonal crosstalk with lipid metabolism is recognized as a modulator of
dyslipidemia. This is crucial as it is highly probable that dyslipidemia in older people is a
result of metabolic changes that have begun much earlier in life. According to the current
clinical evidence, there are several hormones that offer the possibility of improving CVD risk
prediction. These candidates also offer potential therapeutic avenues in the near future. A
goal of aging research in general, is to prolong healthy life-span by identifying strategies that
could prevent or delay CVD. Finding the appropriate regime for each individual, based on
their circumstances is critical to achieving a long life spent in good health. Prevention is the
key to healthy living: starting life healthy, staying healthy and maintaining the lowest risk
18
450
451
452
453
454
455
456
457
458
459
460
461
462
463
464465466467468
469
470
471
472
473
474
475
476

throughout life. Health promotion programs should target people of all ages, since the risk of
CVD starts early in life and increases with age. With an aging global population, identifying
CVD risk earlier in life or developing novel therapeutic avenues that help prevent the onset of
dyslipidemia in older people would have significant benefits for society as a whole.
Five-year view
There is little doubt life expectancy will continue to increase in the next five years
both globally and in the UK.
With an aging population and increases in the prevalence of obesity/metabolic
syndrome, it is highly probable that significant numbers of older people will have
either diagnosed or undiagnosed CV morbidity.
CV morbidity in older people will inevitably continue to be underpinned by
dysregulated lipid metabolism.
It is likely that novel indicators and risk factors for dyslipidemia and/or CVD will be
used to predict the onset of CV morbidity with aging. It is possible based on current
evidence that they will center on hormonal interplay with lipid metabolism.
How successful we are at developing interventions will ultimately be an important
determinant of quality of life in older people.
Key issues
Developed populations are aging gradually and this presents a number of problems.
CVD mortality rates have halved in the last two decades, but morbidity among older
people persists.
Dysregulation of lipid metabolism has historically been used as a risk for CVD.
The mechanisms that underpin age-related dyslipidemia are incompletely understood.
19
477
478
479
480
481482483484485
486
487
488
489
490
491
492
493
494
495
496
497
498
499
500
501
502
503
504

CVD is not a pathology caused by one single biological change; instead, it is more
likely the result of a combination of several factors.
Exploring the hormonal interplay with lipid metabolism is one such factor that could
help to further elucidate the mechanisms. This will lead to novel risk factors for
CVD/cardio metabolic risk.
For stress hormones to be used as a risk factor, an improved understanding of the
effects of stress hormones on the regulation of adipose tissue metabolism is
fundamental in order to establish the clinical connection between psychological stress
and the dysregulation of lipid metabolism.
Recent evidence points at several other hormonal candidates that could be used, for
instance leptin levels could be utilized due to its ability to predict IR and other cardio-
metabolic risk factors independent of obesity.
GH measurement in older people could also have an important role to play in
reducing CVD risk.
Dietary intervention could help to normalize the dyslipidemia in middle age.
Careful monitoring of estrogen or hormonal intervention might improve
postmenopausal dyslipidemia in females.
References
20
505
506
507
508
509
510
511
512
513
514
515
516
517
518
519
520
521
522
523
524
525
526
527
528
529
530
531
532

1. WHO; US National Institute of Aging: Global Health and Ageing. 2011.2. Amaranayake, N., et al., Social Trensds 30: Office For National Statistics, 2000, The Stationary
Office 3. Statistical Bulletin: Life expectancy at birth and at age 65 for local areas in England and
Wales, 2010-12, UK-Office for National Statistcs. 2013.4. Beaumont, J., Population Social Trends 41, O.f.N. Statistics, Editor 2011.5. Shrestha, L.B. and E.J. Heisler, The Changing Demographic Profile of the United States, CRS,
Editor 2011. p. 1-21.6. UN, World Population Prospects the 2012 Revision, Volume 2: Demographic Profiles, E.S.
Affiars, Editor 2013, United Nations.7. Age UK : Improving later life. Understanding the Oldest Old, 2013.8. Alemayehu, B. and K.E. Warner, The lifetime distribution of health care costs. Health Serv
Res, 2004. 39(3): p. 627-42.9. Campbell, J.C. and N. Ikegami, Long-term care insurance comes to Japan. Health Aff
(Millwood), 2000. 19(3): p. 26-39.10. Web site- Public Health England (ERPHO until the 1st of April 2013) Excel data file P3043
Chronic disease prevalence by age, sex SHA and UK country in 2008 final web. Downloaded on the 4th of February 2014 (data used in Figure 2), 2013.
11. Scarborough, P., et al., Trends in coronary heart disease, 1961-2011, B.H. Foundation, Editor 2011.
12. Townsend, N., et al., Coronary heart disease statistics A compendium of health statistics 2012 edition, B.H.F.H.P.R. Group, Editor 2012, British Heart Foundation
13. Tattersall, M.C., et al., Trends in low-density lipoprotein cholesterol goal achievement in high risk United States adults: longitudinal findings from the 1999-2008 National Health and Nutrition Examination Surveys. PLoS One, 2013. 8(4): p. e59309.
14. Arai, H., Oxidative modification of lipoproteins. Subcell Biochem, 2014. 77: p. 103-14.15. Assmann, G., P. Cullen, and H. Schulte, The Munster Heart Study (PROCAM). Results of
follow-up at 8 years. Eur Heart J, 1998. 19 Suppl A: p. A2-11.16. Cooney, M.T., et al., HDL cholesterol protects against cardiovascular disease in both genders,
at all ages and at all levels of risk. Atherosclerosis, 2009. 206(2): p. 611-6.17. Ginter, E. and V. Simko, New promising potential in fighting atherosclerosis: HDL and reverse
cholesterol transport. Bratisl Lek Listy, 2013. 114(3): p. 172-6.18. Mc Auley, M.T., et al., A whole-body mathematical model of cholesterol metabolism and its
age-associated dysregulation. BMC Syst Biol, 2012. 6(1): p. 130.19. Mc Auley, M.T., et al., Nutrition Research and the Impact of Computational Systems Biology.
Journal of Computer Science and Systems Biology, 2013. 6: p. 271-285.20. Sarwar, N., et al., Triglycerides and the risk of coronary heart disease: 10,158 incident cases
among 262,525 participants in 29 Western prospective studies. Circulation, 2007. 115(4): p. 450-8.
21. Schwartz, E.A. and P.D. Reaven, Lipolysis of triglyceride-rich lipoproteins, vascular inflammation, and atherosclerosis. Biochim Biophys Acta, 2012. 1821(5): p. 858-66.
22. Langin, D., Adipose tissue lipolysis as a metabolic pathway to define pharmacological strategies against obesity and the metabolic syndrome. Pharmacol Res, 2006. 53(6): p. 482-91.
23. Dinel, A.L., C. Kolditz, and D. Langin, Metabolism of Fatty Acids in Adipocytes, in Novel Insights into Adipose Cell Functions, Y. Christen, K. Clément, and B.M. Spiegelman, Editors. 2010, Springer Berlin Heidelberg. p. 21-43.
24. Lass, A., et al., Lipolysis - a highly regulated multi-enzyme complex mediates the catabolism of cellular fat stores. Prog Lipid Res, 2011. 50(1): p. 14-27.
25. Zechner, R., et al., Adipose triglyceride lipase and the lipolytic catabolism of cellular fat stores. J Lipid Res, 2009. 50(1): p. 3-21.
21
533534535536537538539540541542543544545546547548549550551552553554555556557558559560561562563564565566567568569570571572573574575576577578579580581582583

26. Kraemer, F.B. and W.J. Shen, Hormone-sensitive lipase knockouts. Nutr Metab (Lond), 2006. 3: p. 12.
27. Reaven, G., Insulin resistance and coronary heart disease in nondiabetic individuals. Arterioscler Thromb Vasc Biol, 2012. 32(8): p. 1754-9.
28. Reaven, G.M., Insulin resistance: the link between obesity and cardiovascular disease. Med Clin North Am, 2011. 95(5): p. 875-92.
29. McAuley, M.T., et al., A mathematical model of aging-related and cortisol induced hippocampal dysfunction. BMC Neurosci, 2009. 10: p. 26.
30. Peckett, A.J., D.C. Wright, and M.C. Riddell, The effects of glucocorticoids on adipose tissue lipid metabolism. Metabolism, 2011. 60(11): p. 1500-10.
31. Park, S.Y., J.H. Bae, and Y.S. Cho, Cortisone induces insulin resistance in C2C12 myotubes through activation of 11beta-hydroxysteroid dehydrogenase 1 and autocrinal regulation. Cell Biochem Funct, 2013.
32. Howlett, T.A., L.H. Rees, and G.M. Besser, Cushing's syndrome. Clin Endocrinol Metab, 1985. 14(4): p. 911-45.
33. Rosmond, R. and P. Bjorntorp, The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med, 2000. 247(2): p. 188-97.
34. Knoops, A.J., et al., Age-related changes in hypothalamic-pituitary-adrenal axis activity in patients with manifest arterial disease. Endocrine, 2010. 37(1): p. 231-8.
35. Jokinen, J. and P. Nordstrom, HPA axis hyperactivity and cardiovascular mortality in mood disorder inpatients. J Affect Disord, 2009. 116(1-2): p. 88-92.
36. Jiang, Y.Z., et al., [New insights in regulation factors of lipoprotein lipase]. Yi Chuan, 2013. 35(7): p. 830-8.
37. Samra, J.S., et al., Effects of physiological hypercortisolemia on the regulation of lipolysis in subcutaneous adipose tissue. J Clin Endocrinol Metab, 1998. 83(2): p. 626-31.
38. Sakayama, K., et al., Effect of cortisol on cell proliferation and the expression of lipoprotein lipase and vascular endothelial growth factor in a human osteosarcoma cell line. Cancer Chemother Pharmacol, 2008. 61(3): p. 471-9.
39. Pedersen, S.B., M. Jonler, and B. Richelsen, Characterization of regional and gender differences in glucocorticoid receptors and lipoprotein lipase activity in human adipose tissue. J Clin Endocrinol Metab, 1994. 78(6): p. 1354-9.
40. Casanovas, A., et al., Retroperitoneal white adipose tissue lipoprotein lipase activity is rapidly down-regulated in response to acute stress. J Lipid Res, 2007. 48(4): p. 863-8.
41. Park, S.B., et al., Association of cortisol and the metabolic syndrome in Korean men and women. J Korean Med Sci, 2011. 26(7): p. 914-8.
42. Ward, A.M., et al., Cortisol and the metabolic syndrome in South Asians. Clin Endocrinol (Oxf), 2003. 58(4): p. 500-5.
43. Xu, C., et al., Direct effect of glucocorticoids on lipolysis in adipocytes. Mol Endocrinol, 2009. 23(8): p. 1161-70.
44. Djurhuus, C.B., et al., Additive effects of cortisol and growth hormone on regional and systemic lipolysis in humans. Am J Physiol Endocrinol Metab, 2004. 286(3): p. E488-94.
45. Pedersen, S.B., et al., Epinephrine stimulates human muscle lipoprotein lipase activity in vivo. Metabolism, 1999. 48(4): p. 461-4.
46. Carmen, G.Y. and S.M. Victor, Signalling mechanisms regulating lipolysis. Cell Signal, 2006. 18(4): p. 401-8.
47. Horton, T.J., et al., Greater systemic lipolysis in women compared with men during moderate-dose infusion of epinephrine and/or norepinephrine. J Appl Physiol (1985), 2009. 107(1): p. 200-10.
48. Ong, J.M., et al., Epinephrine inhibits lipoprotein lipase gene expression in rat adipocytes through multiple steps in posttranscriptional processing. Mol Endocrinol, 1992. 6(1): p. 61-9.
22
584585586587588589590591592593594595596597598599600601602603604605606607608609610611612613614615616617618619620621622623624625626627628629630631632633

49. Horowitz, J.F. and S. Klein, Whole body and abdominal lipolytic sensitivity to epinephrine is suppressed in upper body obese women. Am J Physiol Endocrinol Metab, 2000. 278(6): p. E1144-52.
50. Jocken, J.W., et al., Effect of beta-adrenergic stimulation on whole-body and abdominal subcutaneous adipose tissue lipolysis in lean and obese men. Diabetologia, 2008. 51(2): p. 320-7.
51. Mowers, J., et al., Inflammation produces catecholamine resistance in obesity via activation of PDE3B by the protein kinases IKK{varepsilon} and TBK1. Elife, 2013. 2(0): p. e01119.
52. Niemi, T. and E.A. Nikkila, Effect of age on the lipemia clearing activity of serum after administration of heparin to human subjects. J Gerontol, 1957. 12(1): p. 44-7.
53. Brodows, R.G. and R.G. Campbell, Effect of age on post-heparin lipase. N Engl J Med, 1972. 287(19): p. 969-70.
54. Bey, L., et al., Reduced lipoprotein lipase activity in postural skeletal muscle during aging. J Appl Physiol (1985), 2001. 91(2): p. 687-92.
55. Hamilton, M.T., et al., Plasma triglyceride metabolism in humans and rats during aging and physical inactivity. Int J Sport Nutr Exerc Metab, 2001. 11 Suppl: p. S97-104.
56. Watts, G.F., E.M. Ooi, and D.C. Chan, Demystifying the management of hypertriglyceridaemia. Nat Rev Cardiol, 2013. 10(11): p. 648-61.
57. Wang, H. and R.H. Eckel, Lipoprotein lipase: from gene to obesity. Am J Physiol Endocrinol Metab, 2009. 297(2): p. E271-88.
58. Shimada, M., et al., Overexpression of human lipoprotein lipase protects diabetic transgenic mice from diabetic hypertriglyceridemia and hypercholesterolemia. Arterioscler Thromb Vasc Biol, 1995. 15(10): p. 1688-94.
59. Jensen, D.R., et al., Prevention of diet-induced obesity in transgenic mice overexpressing skeletal muscle lipoprotein lipase. Am J Physiol, 1997. 273(2 Pt 2): p. R683-9.
60. Semenkovich, C.F., et al., Insulin regulation of lipoprotein lipase activity in 3T3-L1 adipocytes is mediated at posttranscriptional and posttranslational levels. J Biol Chem, 1989. 264(15): p. 9030-8.
61. Goldberg, I.J., R.H. Eckel, and N.A. Abumrad, Regulation of fatty acid uptake into tissues: lipoprotein lipase- and CD36-mediated pathways. J Lipid Res, 2009. 50 Suppl: p. S86-90.
62. Vijayakumar, A., et al., Biological effects of growth hormone on carbohydrate and lipid metabolism. Growth Horm IGF Res, 2010. 20.
63. Hermann, M. and P. Berger, Hormonal changes in aging men: a therapeutic indication? Exp Gerontol, 2001. 36(7): p. 1075-82.
64. Sattler, F.R., Growth hormone in the aging male. Best Practice & Research Clinical Endocrinology & Metabolism, 2013. 27(4): p. 541–555.
65. Ziv, E. and D. Hu, Genetic variation in insulin/IGF-1 signaling pathways and longevity. Ageing Res Rev., 2011. 10(2): p. 201-4.
66. Abbott, R.D., et al., Joint distribution of lipoprotein cholesterol classes. The Framingham study. Arteriosclerosis, 1983. 3(3): p. 260-72.
67. Miller, N.E., Why does plasma low density lipoprotein concentration in adults increase with age? Lancet, 1984. 1(8371): p. 263-7.
68. Grundy, S.M., G.L. Vega, and D.W. Bilheimer, Kinetic mechanisms determining variability in low density lipoprotein levels and rise with age. Arteriosclerosis, 1985. 5(6): p. 623-30.
69. Ericsson, S., et al., Influence of age on the metabolism of plasma low density lipoproteins in healthy males. J Clin Invest, 1991. 87(2): p. 591-6.
70. Sniderman, A.D., et al., Regulation of plasma LDL: the apoB paradigm. Clin Sci (Lond), 2010. 118(5): p. 333-9.
71. Mahley, R.W. and T.L. Innerarity, Lipoprotein receptors and cholesterol homeostasis. Biochim Biophys Acta, 1983. 737(2): p. 197-222.
23
634635636637638639640641642643644645646647648649650651652653654655656657658659660661662663664665666667668669670671672673674675676677678679680681682683

72. Segatto, M., et al., Age- and sex-related differences in extra-hepatic low-density lipoprotein receptor. J Cell Physiol, 2011. 226(10): p. 2610-6.
73. Einarsson, K., et al., Influence of age on secretion of cholesterol and synthesis of bile acids by the liver. N Engl J Med, 1985. 313(5): p. 277-82.
74. Uchida, K., et al., Age-related changes of bile acid metabolism in rats. Arch Gerontol Geriatr, 1990. 10(1): p. 37-48.
75. Uchida, K., et al., Age-related changes in cholesterol and bile-acid metabolism in spontaneously hypertensive rats. Arch Gerontol Geriatr, 1982. 1(2): p. 171-91.
76. Uchida, K., et al., Age-related changes in cholesterol and bile acid metabolism in rats. J Lipid Res, 1978. 19(5): p. 544-52.
77. Corpas, E., S.M. Harman, and M.R. Blackman, Human growth hormone and human aging. Endocr Rev, 1993. 14(1): p. 20-39.
78. Machado, M.O., et al., Growth hormone increases low-density lipoprotein receptor and HMG-CoA reductase mRNA expression in mesangial cells. Nephron Exp Nephrol, 2003. 93(4): p. e134-40.
79. Rudling, M., et al., Importance of growth hormone for the induction of hepatic low density lipoprotein receptors. Proc Natl Acad Sci U S A, 1992. 89(15): p. 6983-7.
80. Rudling, M., P. Parini, and B. Angelin, Growth hormone and bile acid synthesis. Key role for the activity of hepatic microsomal cholesterol 7alpha-hydroxylase in the rat. J Clin Invest, 1997. 99(9): p. 2239-45.
81. Hollander, D. and D. Morgan, Increase in cholesterol intestinal absorption with aging in the rat. Exp Gerontol, 1979. 14(4): p. 201-4.
82. Wang, H.H., N.H. Afdhal, and D.Q. Wang, Overexpression of estrogen receptor alpha increases hepatic cholesterogenesis, leading to biliary hypersecretion in mice. J Lipid Res, 2006. 47(4): p. 778-86.
83. Cao, W.M., et al., Insulin-like growth factor-i regulation of hepatic scavenger receptor class BI. Endocrinology, 2004. 145(12): p. 5540-7.
84. Leiva, A., et al., Mechanisms regulating hepatic SR-BI expression and their impact on HDL metabolism. Atherosclerosis, 2011. 217(2): p. 299-307.
85. Bengtsson, B.A., et al., Treatment of adults with growth hormone (GH) deficiency with recombinant human GH. J Clin Endocrinol Metab, 1993. 76(2): p. 309-17.
86. Li, Z.P., et al., [Serum leptin, adiponectin, visfatin levels in adult GHD patients and correlation studies]. Sichuan Da Xue Xue Bao Yi Xue Ban, 2013. 44(4): p. 588-91.
87. Swarbrick, M.M. and P.J. Havel, Physiological, pharmacological, and nutritional regulation of circulating adiponectin concentrations in humans. Metab Syndr Relat Disord, 2008. 6(2): p. 87-102.
88. Garten, A., S. Schuster, and W. Kiess, The insulin-like growth factors in adipogenesis and obesity. Endocrinol Metab Clin North Am, 2012. 41(2): p. 283-95, v-vi.
89. Liu, Y., et al., Inhibitory effect of leptin on growth hormone secretion of GH3 cells: involvement of cell proliferation, apoptosis and intracellular free Ca2+. Cytokine, 2009. 46(2): p. 245-50.
90. Lim, S., M.J. Quon, and K.K. Koh, Modulation of adiponectin as a potential therapeutic strategy. Atherosclerosis, 2014. 233(2): p. 721-728.
91. Awazawa, M., et al., Adiponectin enhances insulin sensitivity by increasing hepatic IRS-2 expression via a macrophage-derived IL-6-dependent pathway. Cell Metab, 2011. 13(4): p. 401-12.
92. Beatty, A.L., et al., Adiponectin is associated with increased mortality and heart failure in patients with stable ischemic heart disease: data from the Heart and Soul Study. Atherosclerosis, 2012. 220(2): p. 587-92.
24
684685686687688689690691692693694695696697698699700701702703704705706707708709710711712713714715716717718719720721722723724725726727728729730731732

93. Kizer, J.R., et al., Associations of total and high-molecular-weight adiponectin with all-cause and cardiovascular mortality in older persons: the Cardiovascular Health Study. Circulation, 2012. 126(25): p. 2951-61.
94. Goldberg, I.J., et al., Thyroid hormone reduces cholesterol via a non-LDL receptor-mediated pathway. Endocrinology, 2012. 153(11): p. 5143-9.
95. Chin, K.Y., et al., The relationships between thyroid hormones and thyroid-stimulating hormone with lipid profile in euthyroid men. Int J Med Sci, 2014. 11(4): p. 349-55.
96. Kasiske, B.L., et al., Effects of antihypertensive therapy on serum lipids. Ann Intern Med, 1995. 122(2): p. 133-41.
97. Keen-Rhinehart, E., K. Ondek, and J.E. Schneider, Neuroendocrine regulation of appetitive ingestive behavior. Front Neurosci, 2013. 7: p. 213.
98. Maffei, M., et al., Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med, 1995. 1(11): p. 1155-61.
99. Considine, R.V., et al., Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med, 1996. 334(5): p. 292-5.
100. Donahoo, W.T., et al., Leptin increases skeletal muscle lipoprotein lipase and postprandial lipid metabolism in mice. Metabolism, 2011. 60(3): p. 438-43.
101. Zuo, H., et al., Association between serum leptin concentrations and insulin resistance: a population-based study from China. PLoS One, 2013. 8(1): p. e54615.
102. Koh, K.K., et al., Efonidipine simultaneously improves blood pressure, endothelial function, and metabolic parameters in nondiabetic patients with hypertension. Diabetes Care, 2007. 30(6): p. 1605-7.
103. Rutter, M.K., et al., Epidemiological evidence against a role for C-reactive protein causing leptin resistance. Eur J Endocrinol, 2013. 168(1): p. 101-6.
104. Guarente, L., Calorie restriction and sirtuins revisited. Genes Dev, 2013. 27(19): p. 2072-85.105. Stewart, T.M., et al., Comprehensive Assessment of Long-term Effects of Reducing Intake of
Energy Phase 2 (CALERIE Phase 2) screening and recruitment: methods and results. Contemp Clin Trials, 2013. 34(1): p. 10-20.
106. Rickman, A.D., et al., The CALERIE Study: design and methods of an innovative 25% caloric restriction intervention. Contemp Clin Trials, 2011. 32(6): p. 874-81.
107. Fontana, L., et al., Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A, 2004. 101(17): p. 6659-63.
108. Koppo, K., et al., Catecholamine and insulin control of lipolysis in subcutaneous adipose tissue during long-term diet-induced weight loss in obese women. Am J Physiol Endocrinol Metab, 2012. 302(2): p. E226-32.
109. Grundy, S.M., et al., Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Arterioscler Thromb Vasc Biol, 2004. 24(8): p. e149-61.
110. Manson, J.E., et al., Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women's Health Initiative randomized trials. JAMA, 2013. 310(13): p. 1353-68.
111. Sumino, H. and M. Murakami, [Investigation of atherosclerosis in postmenopausal women: alteration of atherosclerosis-associated factors and vascular atherosclerosis by oral and transdermal estrogen replacement]. Rinsho Byori, 2013. 61(3): p. 256-62.
112. Rossouw, J.E., et al., Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA, 2007. 297(13): p. 1465-77.
113. Izzicupo, P., et al., Effects of ACE I/D polymorphism and aerobic training on the immune-endocrine network and cardiovascular parameters of postmenopausal women. J Clin Endocrinol Metab, 2013. 98(10): p. 4187-94.
25
733734735736737738739740741742743744745746747748749750751752753754755756757758759760761762763764765766767768769770771772773774775776777778779780781
782

Annotated references
**
Mc Auley, M.T., et al., A whole-body mathematical model of cholesterol metabolism and its age-associated dysregulation. BMC Syst Biol, 2012. 6(1): p. 130.
Interesting mathematical model that demonstrates that a better understanding of lipid metabolism and aging can only be achieved by studying its many mechanistic interactions
**
Chin, K.Y., et al., The relationships between thyroid hormones and thyroid-stimulating hormone with lipid profile in euthyroid men. Int J Med Sci, 2014. 11(4): p. 349-55.
**
Worthwhile paper that demonstrates the potential of TSH has a therapeutic means of acting on both TG and LDL-C
**
Goldberg, I.J., et al., Thyroid hormone reduces cholesterol via a non-LDL receptor-mediated pathway. Endocrinology, 2012. 153(11): p. 5143-9.
Worthwhile paper that investigates a potential hormonal centered means for lowering LDL-C
List of Figures
Figure 1: The aging UK demographic. By the year 2031 it is predicted that almost 12% of the UK population will 75 years of age or older. Despite this demographic shift, this does not mean that these extra years will be spent as healthy ones (Source of data: Reference 3)
Figure 2: The overall prevalence of selected chronic conditions, as a function of age for the UK population for 2008. CHD and stroke; the principle clinical manifestations of CVD are the most common conditions in older people. Data source: Public Health England (Reference 101)
Figure 3: Schematic representation of lipolysis and lipogenesis and their interplay with a variety of hormones. These interactions are discussed in detail in the main body of the paper. T shaped arrows
26
783
784
785
786
787
788
789790
791
792793
794
795796
797
798799
800
801802
803
804
805
806807808
809810811
812
813814

represent inhibition, round headed arrows represent effectors while arrow heads represent synthesis or conversion of a metabolite/hormone.
List of Abbreviations
adipose tissue blood flow(ATBF), adrenocorticotropic hormone (ACTH), caloric restriction (CR), cardiovascular disease (CVD), cholesteryl ester transfer protein (CETP)Comprehensive Assessment of Long- Term Effects of Reducing Calorie Intake (CALORIE) conjugated equine estrogen (CEE), corticotrophin-releasing hormone (CRH)free fatty acids ( FFAs), Growth hormone deficiency (GHD), glucocorticoid (GC) ) growth hormone (GH), glucocorticoid receptor (GR), glucocorticoid receptors (GRs) high density lipoprotein cholesterol(HDL-C) ,hormone sensitive lipase (HSL), hypothalamic-pituitary-adrenal (HPA) axis, IGF-binding proteins (IGFBPs), insulin resistance (IR) lecithin:cholesterol acyltransferase (LCAT),lipoprotein lipase (LPL), low density lipoprotein cholesterol (LDL-C), low-calorie diet (LCD) (WM), protein kinase B(Akt) reverse cholesterol transport (RCT), scavenger receptor of the B class (SR-BI), steroid converting (sc) ,Subcutaneous adipose tissue(SCAT) ,The rate of appearance (Ra), ,transdermal estradiol (E2) ,triacylglycerol’s (TGs), triglyceride-rich lipoproteins (TRLs), Triglycerides(TG), upper body obesity(UBO) , very low-calorie diet (VLCD), very low-density lipoproteins (VLDL), 11β-hydroxysteroid dehydrogenase 1 (11β-HSD1)
27
815816
817
818
819
820821822823824825826827828829830831832833