Expansion of visceral leishmaniasis to northwest sub-Himalayan...
Transcript of Expansion of visceral leishmaniasis to northwest sub-Himalayan...

Visceral leishmaniasis (VL) is a systemic protozoandisease that is transmitted by phlebotomine sandflies andis endemic in eastern states of India, mainly Bihar, WestBengal and Orissa1. However, epidemiological shift fromeast to west is taking place and an increased numbers ofcases have been reported from natives of sub-Himalayanregion of Uttarakhand1-2 and Himachal Pradesh3. Accord-ing to a World Health Organization (2013) estimate, 1.3million new cases of leishmaniasis occur worldwide an-nually4. Expansion of VL into new areas is one of thechallenges in elimination of the disease from the region.Major risk factors of Leishmania distribution are socio-economic conditions, malnutrition, population mobility,and environmental and climate changes5. The possiblereasons for finding new foci of VL cases could be theimproved monitoring system, high index of suspicion andsubsequent improvement in diagnostic modalities, shift-ing of vector’s geographic range, development offavourable factors for vector expansion and leishmania-sis transmission.
We report four cases of VL diagnosed at a teachingtertiary care centre, located in the physiogeographic zoneof Shivalik and Lesser Himalayas of the State of HimachalPradesh over a period of four years. These patientshad never visited VL endemic regions in their life. Theclinical presentation was more or less classical infirst two patients. However, in third patient secondaryhemophagocytosis lymphohistiocytosis (HLH) was as-sociated with VL. Another patient had an atypical pre-sentation in the form of chronic diarrhoea and was unex-pectedly diagnosed as a case of intestinal leishmaniasisthrough the identification of the Leishman-donovan (LD)bodies in duodenal and colonic mucosa. These are thefirst reports of VL from the non-endemic northwesternhilly region of Chamba, Himachal Pradesh and adjoiningarea of Basholi in Jammu and Kashmir.
Case reportsAll the patients were native of Ravi River valley area
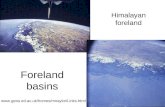
situated at an average altitude of 996 m (3268 ft) abovethe mean sea level (Fig. 1). Among the four patients threewere males and one female. The age distribution and yearof presentation are given in Table 1. The duration of symp-toms varied from 1–6 months. The presenting symptomsand signs are given in Table 1. The details of haematologyand biochemistry parameters at admission are shown inTable 2. All the four patients were negative for humanimmunodeficiency virus infection. All the patients deniedever visiting any endemic area of VL. Patient number 1and 2 had classical presentation of VL in the form of fe-ver, hepatosplenomegaly and pancytopenia. Patient num-ber 3, and 4 had atypical presentation which added to thediagnostic dilemma. In patient number 3, VL was foundto be associated with secondary HLH. On haematologicalinvestigations pancytopenia was observed. Liver func-tion tests showed transaminasemia. Bone marrow aspira-tion and biopsy revealed marked increase in histiocyteswith a prominent hemophagocytosis. Amastigote formsof Leishmania donovani were seen both intracellularlyand extracellularly (Fig. 2). The diagnosis of HLH wasestablished, as 6 out of 8 diagnostic criteria (5 out of 8are required) were fulfilled, viz. fever, splenomegaly, cy-topenia, hyperferritinemia, hypertriglyceridemia andhemophagocytosis in the bone marrow6. Patient number4 presented with chronic diarrhoea. VL was not a differ-ential diagnosis and was unexpectedly diagnosed as in-testinal leishmaniasis through the identification of the LDbodies in duodenal and colonic mucosa (Fig. 3). The mainpitfall in the diagnosis was that even with classical pre-sentation the first diagnosis was always other than kala-azar in all of the cases. The treatment received by thepatients and outcome is mentioned in Table 1.
DISCUSSION
Chamba district is topographically bounded by theDhauladhar and Zanskar ranges, south of inner Himalayas.The district is bordered by Jammu and Kashmir in the
J Vector Borne Dis 53, June 2016, pp. 188–191
Expansion of visceral leishmaniasis to northwest sub-Himalayan region ofIndia: A case series
Sujeet Raina1, Rashmi Kaul Raina2, Rajesh Sharma1, Baldev Singh Rana1, Anita Bodh2 &Manupriya Sharma2
1Department of Medicine; 2Department of Pathology, Dr Rajendra Prasad Government Medical College, Kangra, Himachal Pradesh, India
Key words Chamba; Jammu & Kashmir; kala-azar; Ravi River; visceral leishmaniasis

Raina et al: VL expension to northwest sub-Himalayan region of India 189
Fig. 1: (a) Study area showing geographic distribution of patients along River Ravi. Figures in parentheses indicate number of patients fromeach location; and (b) District map of Himachal Pradesh, India. Previously reported locations for VL are white squares and presentlocations are shown as red squares.
northwest and west, the Ladakh area of Jammu and Kash-mir, and Lahaul and Bara Banghal in the northeast andeast, Kangra in the southeast and Pathankot district ofPunjab in the south. The temperatures in summer varybetween 38°C (100°F) and 15°C (59°F), and in winter
Table 1. Patient profile of cases of visceral leishmaniasis
Patient Age (yr)/ Year Duration of Clinical presentation Treatment OutcomeNo. Gender symptoms
in months
1. 30/Female 2011 6 Fever Sodium stibogluconate ExpiredExertional dyspnoeaLoss of appetiteLoss of weightHepatomegalyMassive splenomegalyPancytopenia
2. 33/Male 2013 2 Fever Amphotericin-B RecoveredLoss of appetiteLoss of weightModerate splenomegalyPancytopenia
3. 40/Male 2014 1 Fever Amphotericin-B RecoveredHepatomegalyMassive splenomegalyPancytopeniaHemophagocytosis
4. 50/Male 2014 6 Fever – ExpiredChronic diarrhoeaLoss of weightHepatomegalyMassive splenomegalyBicytopenia
between 15°C (59°F) and 0°C (32°F). The average an-nual rainfall in the area is 785.84 mm (30.939 inch). TheVL has already been reported in southeast area ofHimachal Pradesh from the sub-alpine valley along theSutlej River that leads to the mountain deserts of the tribal

J Vector Borne Dis 53, June 2016190
district of Kinnaur and adjacent area of Shimla and Kulludistricts at an altitude of 924–2900 m above mean sealevel (Fig. 1). The current “hotspots” are at a distance of> 600 km from previously identified “endemic” areas ofthe state. The area has witnessed large scale deforesta-tion, construction activities, urbanization, establishmentof new residential colonies, creation of townships, for-mation of large water bodies in the form of dams andlakes. A major multipurpose project, Ranjit Sagar Damhas been built on the River Ravi. Further, hydroelectricpotential of the river has been exploited with the con-struction of five large and numerous small hydroelectricpower projects. Creation of job opportunities has causedmigration of manpower from Bihar, Nepal, Jharkhand andUttar Pradesh. The six species of Phlebotomus and 15species of Sergentomyia have been found in the northernmountain ranges of the Himalayas (Himachal Pradesh issituated in these ranges), with their distribution limitedto particular ecoclimatic zones7.
Survey of Phlebotomid sandflies from the Himalayanregion, India has established the presence of Phleboto-mus longiductus, P. major, Sergentomyia bailyi and S.montana (Diptera: Psychodidae) at an altitude of 1570 min the Tissa region of Chamba district7–8. While under-standing the ecosystem of phlebotomine vectors it hasbeen observed that VL vector P. argentipes produced highclusters around waterbody and dense forest in non-en-demic sites. These conditions are preferred as oviposi-tion and breeding places and favour the development ofvector9. Their role as a vector for transmission of VL, inthis particular region needs to be delineated by demon-strating similar strains of Leishmania in both the vectorand the human host. Environmental changes are occur-ring simultaneously during last two decades. Climatechange (systematic temperature increases by 0.01–0.04°C per year) is likely to increase the burden of infectiousdiseases in particular, to vector-borne tropical diseasesthat have historically been absent in the Himalayas10.
Leishmaniasis has been associated with climaticchange in developed nations of Europe5. In the Indiansubcontinent, VL is mainly caused by L. donovani andits transmission is assumed anthroponotic through the biteof the sandfly species P. argentipes11. We interpret ap-pearance of VL in this non-endemic area as an indicationof autochthonous transmission as there is no travel his-tory of the reported cases to endemic regions. However,what favours imported VL vis-à-vis indigenous transmis-sion in non-endemic areas is low frequency of casesamong children. It is still not clear whether the parasitehas come from intrusion into sylvatic cycle or introducedby migrant population. These immigrants could have been
Table 2. Haemogram and biochemistry profile at admission
Parameter Patient Patient Patient PatientNo. 1 No. 2 No. 3 No. 4
Haemoglobin (g%) 6.4 4.6 6.7 7.5TLC (cells/mm3) 2000 1300 600 2100DLC
Polymorphs 31 44 41 45Lymphocytes 66 49 44 46Monocytes 2 5 14 8Eosinophils 1 1 1 1
Platelets (per mm3) 99,000 26,000 36,000 134,000ESR (mm 1st hour) – 60 102 60Bilirubin
Total (mg/dl) 1.6 1 1.35 0.31Direct (mg/dl) 0.5 0.6 0.5 0.08
AST (IU) 147 194 256 24ALT (IU) 130 86 151 8Alkaline phosphatase (KAU) 689 86 475 152Serum Proteins
Total (g/dl) 6.2 5.5 7 7.1Albumin (g/dl) 2.5 1.9 2.5 3.5
Urea (mg/dl) 26 49 30 28Creatinine (mg/dl) 0.9 1.1 0.6 0.8Serum ferritin (ng/ml) – – 18,500 –Triglycerides (mg/dl) – – 274 –
Fig. 2: Bone marrow aspiration smear shows (a) Macrophages withengulfed erythroid cells and lymphocytes (hemophagocytosis);and (b) Megakaryocyte with engulfed LD bodies (Giemsa,×1000).
Fig. 3: Photomicrograph showing macrophages with abundantintracytoplasmic and extracellular bodies of leishmania: (a)Duodenal biopsy; and (b) Colonic biopsy (H and E, ×1000).

Raina et al: VL expension to northwest sub-Himalayan region of India 191
infected with L. donovani outside this region. The factthat all our patients had contracted the disease indig-enously is suggestive of a local vector and probably azoonotic reservoir. Concerns of potential animal reser-voirs in India are rising as evident by the increasingseroprevalence of rK 39 antigen tests in animals12. Do-mestic animals as reservoir hosts in VL transmission havebeen indicated in a recent study in Nepal13.
Furthermore, the genetic makeup of Leishmania iso-lates of this region should be studied and compared withother Indian isolates.
REFERENCES
1. Verma SK, Ahmed S, Shirazi N, Kusum A, Kaushik RM,Barthwal SP. Sodium stibogluconate-sensitive visceral leishma-niasis in the non-endemic hilly region of Uttarakhand, India.Trans R Soc Trop Med Hyg 2007; 101: 730–2.
2. Singh S, Biswas A, Wig N, Aggarwal P, Sood R, Wali JP. A newfocus of visceral leishmaniasis in sub-Himalayan (Kumaon) re-gion of northern India. J Commun Dis 1999; 31: 73–7.
3. Raina S, Mahesh DM, Kaul K, Satindra KS, Gupta D, SharmaA, et al. A new focus of visceral leishmaniasis in the Himalayas,India. J Vector Borne Dis 2009; 46: 303–6.
4. Leishmaniasis. Geneva, Switzerland: World Health Organiza-tion 2013. Available from: http://www.who.int/leishmaniasis/en/
Correspondence to: Dr Sujeet Raina, C–15, Type–V Quarters, Dr Rajendra Prasad Government Medical College Campus, Tanda HospitalRoad, Kangra–176 001, Himachal Pradesh, India.E-mail: [email protected]
Received: 13 March 2016 Accepted in revised form: 2 June 2016
(Accessed on May 10, 2014).5. Savoia D. Recent updates and perspectives on leishmaniasis. J
Infect Dev Ctries 2015; 9: 588–96.6. Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH,
Imashuku S, Ladisch S, et al. HLH-2004: Diagnostic and thera-peutic guidelines for hemophagocytic lymphohistiocytosis.Pediatr Blood Cancer 2007; 48: 124–31.
7. Kaul SM, Jain DC. Distribution of phlebotomine sandflies(Diptera: Psychodidae) according to the physiographic divisionsof India. J Commun Dis 1995; 27: 155–63.
8. Kulkarni SM, Bhat HR, Modi GB. Survey of phlebotomidsandflies from the Himalayan region, India (Diptera:Phlebotomidae). Indian J Med Res 1978; 67: 583–8.
9. Kesari S, Bhunia GS, Kumar V, Jeyaram A, Ranjan A, Das P. Acomparative evaluation of endemic and non-endemic regionof visceral leishmaniasis (Kala-azar) in India with groundsurvey and space technology. Mem Inst Oswaldo Cruz 2011; 106:515–23.
10. Sarkar S. Climate change and disease risk in the Himalayas. HimalJ Sci 2010; 6: 7–8.
11. Control of the leishmaniasis. WHO Tech Rep Ser 2010; No. 949:1–186.
12. Ho M, Siongok TK, Lyerly WH, Smith DH. Prevalence and dis-ease spectrum in a new focus of visceral leishmaniasis in Kenya.Trans R Soc Trop Med Hyg 1982; 76: 741–6.
13. Bhattarai NR, Van der Auwera G, Rijal S, Picado A, SpeybroeckN, Khanal B, et al. Domestic animals and epidemiology ofvisceral leishmaniasis, Nepal. Emerg Infect Dis 2010; 16:231–7.