Dötsch 2001
-
Upload
damian-rojas -
Category
Documents
-
view
216 -
download
1
description
Transcript of Dötsch 2001
-
Exposure to Endogenous Estrogens During Lifetime
Jrg Dtsch1, Helmuth G. Drr 1, Ludwig Wildt 2
1 Klinik fr Kinder und Jugendliche, Friedrich-Alexander-University Erlangen-Nrnberg,Loschgestrasse 15, 91054 Erlangen, Germanye-mail: [email protected]
2 Universittsfrauenklinik, Friedrich-Alexander-University Erlangen-Nrnberg, Loschge-strasse 15, 91054 Erlangen, Germany
The present review summarizes data on the time course and physiological function of thethree major endogenous estrogens estrone (E1), 17b-estradiol (E2), and estriol (E3) duringthe different phases of life in the human female and male. During fetal life, E3 is the mostabundant estrogen produced by the fetoplacental unit. E3 affects cerebral development,leads to breast gland swelling in both girls and boys and promotes uterine growth up to a sizethat is not reached again until puberty. In infancy and childhood estrogen levels are low be-fore the ovaries are stimulated to increase the production of E2 at puberty. In the complexcourse of maturation, the onset of puberty is characterized by a gradually increasing pulsatilesecretion of hypothalamic gonadotropin-releasing hormone followed by a gradual rise of cir-culating gonadotropin levels. Increasing E2 concentrations in girls promote development offemale sex characteristics, menarche, behavioral changes, pubertal growth spurt and finallythe closure of epiphysal growth zones. Throughout fertile life of the human female, ovarianE2 remains the major endogenous estrogen. It is produced by the granulosa cells of the grow-ing follicle as well as by the corpus luteum. Among other functions, it is important for en-dometrial proliferation, as a prerequisite for blastocyst implantation and pregnancy. E2 in-duces growth of the uterus and maturation of the breast. E2 production declines graduallyduring late reproductive life; as a consequence, menstrual bleeding ceases with menopause.During postmenopause, the predominant endogenous estrogen is E1, which is mainly pro-duced by adipose tissue from androgenic precursors secreted by the ovarian stroma and theadrenal gland. Decreased estrogen concentrations lead to atrophy of the inner and outer gen-italia, osteoporosis, an increased risk of cardiovascular disease, hot flashes and emotional in-stability.
In summary, exposure to endogenous estrogens during lifetime in the female varies byseveral orders of magnitude. The time course of estrogen concentration is characterized by ahigh-estrogen environment during pregnancy, a decline following birth to the low levels dur-ing prepuberty. Onset of sexual maturation is indicated by the rising levels of E2 reachingadult concentrations some years after menarche.
Keywords. Estradiol, Estriol, Estrone, Menopause, Puberty
1 Introduction and Physiology of Estrogen Metabolism . . . . . . . 83
1.1 Biochemistry of Endogenous Estrogens . . . . . . . . . . . . . . . 831.2 Action of Estrogens in the Target Cell . . . . . . . . . . . . . . . . 851.3 Physiology of Estrogen Action . . . . . . . . . . . . . . . . . . . . 85
CHAPTER 5
The Handbook of Environmental Chemistry Vol. 3, Part LEndocrine Disruptors, Part I(ed. by M. Metzler) Springer-Verlag Berlin Heidelberg 2001
-
2 Estrogens in Fetal Life, Infancy and Prepubertal Childhood . . . 86
2.1 Fetus and Neonate . . . . . . . . . . . . . . . . . . . . . . . . . . . 862.2 Infancy and Childhood . . . . . . . . . . . . . . . . . . . . . . . . 86
3 Role of Estrogens During Puberty . . . . . . . . . . . . . . . . . . 87
3.1 Female Puberty . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 873.2 Male Puberty . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 88
4 Role of Estrogens in the Adult Woman and Man During Reproductive Age . . . . . . . . . . . . . . . . . . . . . . . . . . . . 88
4.1 Estrogens During Menstrual Cycle Regulation of the Ovarian and Uterine Function . . . . . . . . . . . . . . . . . . . . 88
4.2 Estrogen Regulation of the Mucosal Immune System . . . . . . . . 894.3 Estrogen Effects Outside the Reproductive System . . . . . . . . . 894.4 Adverse Effects of Endogenous Estrogens . . . . . . . . . . . . . . 894.5 Role of Endogenous Estrogens for the Fertile Man . . . . . . . . . 90
5 Role of Estrogens in Conception and Pregnancy . . . . . . . . . . 90
5.1 Conception and Blastocyst Implantation . . . . . . . . . . . . . . . 905.2 Estrogen Production in Pregnancy . . . . . . . . . . . . . . . . . . 905.3 Impact of Estrogens on the Mother During Pregnancy . . . . . . . 925.4 Role of Estrogens for Lactation . . . . . . . . . . . . . . . . . . . . 93
6 Menopause and Postmenopause . . . . . . . . . . . . . . . . . . . 93
6.1 Physiology and Estrogen Concentrations . . . . . . . . . . . . . . 936.2 Consequences of Decreasing Estrogen Concentrations
During Menopause . . . . . . . . . . . . . . . . . . . . . . . . . . . 94
7 Tables of Concentrations of Estrogens During Different Phases of Life . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 95
8 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 98
Abbreviations
cAMP cyclic adenosine monophosphateDHEA dehydroepiandrosteroneDHEAS dehydroepiandrosterone sulfateE1 estroneE2 17b-estradiolE3 estriolERa estrogen receptor alphaERb estrogen receptor betaFSH follicle-stimulating hormone
82 J. Dtsch et al.
-
GnRH gonadotropin-releasing hormone16a-HO-DHEA 16a-hydroxydehydroepiandrosterone16a-HO-DHEAS 16a-hydroxydehydroepiandrosterone sulfateIgA immunoglobulin AIgG immunoglobulin GLH luteinizing hormoneSHBG sex hormone-binding globulin
1Introduction and Physiology of Estrogen Metabolism
1.1Biochemistry of Endogenous Estrogens
The most important endogenous estrogens in humans are 17b-estradiol (E2),estrone (E1) and estriol (E3, Fig. 1). They all are steroids consisting of 18 carbonatoms and characterized by an aromatic A ring. For the specific estrogen effectthe aromatic A ring and hydroxy groups at positions 3 and 17 are indispensable.
Exposure to Endogenous Estrogens During Lifetime 83
Fig. 1. Chemical structures of the three most important endogenous estrogens estradiol,and estrone estriol
-
E2, the most potent and important estrogen in non-pregnant women, is pre-dominantly produced by the granulosa cells of the active follicle from andro-gens delivered by the theca interna (two-cell hypothesis). During pregnancy, E3produced from androgenic precursors provided by the fetus and the mother, re-spectively, represents the major estrogen [1]. E1, the third of the major endoge-nous estrogens, exists in metabolic equilibrium with E2 due to the action of17b-hydroxysteroid dehydrogenase. In the classic pathway, the estrogen synthe-sis starts from cholesterol provided by lipoproteins (Fig. 2).
Estrogens are biologically inactivated and excreted after sulfation or glu-curonidation, respectively, allowing renal excretion of the inactivated steroids.Although considerable amounts of conjugated estrogens are excreted into thebile, only a small fraction appears in the feces. The majority of the conjugates isreabsorbed after hydrolysis by bacteria from the gastrointestinal tract (entero-hepatic circulation).
The majority of E2 (98%) circulates bound to albumin or to sex hormone-binding globulin (SHBG), a specific carrier protein that binds estrogens and androgens with high affinity.
84 J. Dtsch et al.
Fig. 2. Enzymatic steps in the classical pathway of estradiol biosynthesis in the ovary
-
1.2Action of Estrogens in the Target Cell
Estrogens can enter their target cells via passive diffusion through the cellmembrane. There is, however, increasing evidence for an active transport me-diated by a specific importer localized within the plasma membrane. Aftertransport through the cell membrane, estrogens bind to specific receptors lo-cated within the nucleus of the target cells [2, 3]. There are two different recep-tors for E2: estrogen receptor alpha (ERa) and estrogen receptor beta (ERb)that can form heterodimers exhibiting different affinities to specific DNA se-quences termed estrogen response elements [47]. As evidenced by knockoutmice experiments, the ERa appears to be more important for gene transcrip-tion in the target tissues. ERb knockout mice are less severely affected resultingpredominantly in subfertility [4]. In conjunction with a number of local growthfactors, estrogens stimulate growth and differentiation of tissues and organs.See Chap. 1 for a detailed description of estrogen action in target cells.
The estrogenic activity of E1, E2 and E3 varies considerably when expressedon a molar basis. While E2 represents the most active compound, exerting allestrogenic effects, the biological activity of E3 and E1 appears to be muchlower.
E2 induces the transcription of its own receptors and stimulates the biosyn-thesis of progesterone receptors as a prerequisite of progesterone action.Conversely, progesterone and other progestins inhibit the transcription of es-trogen receptors. Therefore, progestins exhibit an anti-estrogenic effect.
1.3Physiology of Estrogen Action
Estrogens are responsible for the emergence of secondary sex characteristics.These include breast development, typical female body proportions, distribu-tion of subcutaneous adipose tissue and the characteristic estrogen-dependentchanges of the female genital tract. Target organs for the estrogens are the ex-ternal genitalia, vagina, uterus, fallopian tubes and the ovaries. Target tissuesoutside the reproductive organs are, among others, skin including its annexes,bones, the cardiovascular system, the central nervous system, and the liver.
In the reproductive organs, endogenous estrogens promote cell proliferation.Blood flow, water retention, and the accumulation of amino acids and proteinsare increased. The uterine cervix is stimulated by estrogens to secrete mucus.Estrogens stimulate alveolar growth of the breast; however, for full maturationof the mammary gland the additional action of progestins, prolactin as well asglucocorticoids and insulin are necessary.
Exposure to Endogenous Estrogens During Lifetime 85
-
2Estrogens in Fetal Life, Infancy and Prepubertal Childhood
2.1Fetus and Neonate
The fetus is exposed to very high estrogen concentrations due to the enormousE3 production by the placenta (see below). Estrogens in fetal life seem to be im-portant for the development of a number of functions, including brain devel-opment [8, 9]. Newborn female as well as male knockout mice for ERa have se-vere abnormalities of the reproductive tract: female mice exhibit a hypoplasticuterus and hemorrhagic ovaries [4, 10], whereas male mice show testicular dys-genesis. Both genders are infertile. On the other hand, ERb knockout mice havea normal phenotype and only female mice are subfertile. The knockouts of bothreceptors show an even more severe phenotype than the ERa knockouts.
However, in humans estrogens do not appear to be essential for fetal survival,placental growth, or male and female sexual differentiation. This is concludedfrom studies on estrogen deficiency due to mutations in the aromatase gene andestrogen resistance due to disruptive mutations in the estrogen receptor gene[11]. Also sulfatase deficiency does not lead to an abnormal fetal development.
Quite frequently, human newborns of both sexes exhibit hypertrophy of thebreast glands. Since lactation is initiated by a drop of circulating estrogens, thesudden decline of serum estrogen levels after clamping the umbilical cord mayeven lead to temporary mammary secretion called witchs milk. In newbornfemale babies the uterine size is much larger than that of older infants and in-volutes to about one third of its birth size during the following 612 months.Intrauterine endometrial proliferation induced by estrogens may result in with-drawal bleeding in the female newborn [12]. The vaginal epithelium right afterbirth resembles that of the fertile woman, exhibiting low pH and glycogen stor-age. After the first week of life there is a significant rise of gonadotropin con-centrations due to the drop of estrogen levels and the loss of the feedback inhi-bition on pituitary gonadotropin secretion. As a consequence, pulsatile secre-tion of gonadotropin-releasing hormone (GnRH) promotes the release offollicle-stimulating hormone (FSH), resulting in follicular growth in the new-born girls ovary as may be demonstrated by ultrasonography. On the average,E2 levels in newborn girls are slightly higher than in boys as a consequence ofthe increased ovarian activity.
2.2Infancy and Childhood
Until the end of the second year of life the pulsatile GnRH secretion continu-ously diminishes, resulting in a decline of pituitary gonadotropin secretion anda reduction of ovarian stimulation. In toddlers, GnRH release is severely re-duced as indicated by the low-amplitude, low-frequency peaks of luteinizinghormone (LH) that occur every three to four hours during sleep [13]. E2 con-centrations are usually at or below the detection limit, although newer, more
86 J. Dtsch et al.
-
sensitive assays for the detection of E2 show certain fluctuations during that period of life. Using an ultrasensitive assay, elevated E2 concentrations can bedetected in girls with idiopathic premature telarche [14].
Between the sixth and ninth year of life, the hypothalamic activity increasesslowly as reflected by the increase of the number and amplitude of FSH and LHpulses. Via a G-protein-coupled receptor, FSH increases intracellular cyclicadenosine monophosphate (cAMP) concentrations leading to an induction ofthe aromatase that is essential for estrogen synthesis. However, FSH and estro-gen levels still remain low until the onset of puberty.
3Role of Estrogens During Puberty
3.1Female Puberty
In female infancy and childhood, the activity of the hypothalamic pulse gener-ator that directs GnRH release is almost completely inhibited and LH and FSHserum levels are low. Small increases of serum E2 are sufficient to further in-hibit pituitary gonadotropin secretion. The mechanisms inhibiting hypothala-mic GnRH release are not known at present [15, 16] nor are the mechanisms re-sulting in the release of inhibition during puberty [17]. From studies in ovariec-tomized primates it is known that estrogens are not decisive for the activationof the GnRH pulse generator but rather have modulating effects on gonado-tropin release [18]. As a consequence of ovarian stimulation by gonadotropins,E2 levels in serum increase. In conjunction with adrenal as well as ovarian an-drogens, pubic hair develops. Ovaries, uterus, the fallopian tube, vagina, andbreast glands grow under the influence of E2. In puberty stage 34 according toTanner, when E2 levels of approximately 40 pg/mL (140 nmol/L) are reached,the endometrium has sufficiently proliferated to allow withdrawal bleedings af-ter gestagen administration. However, the first menstrual bleeding, the menar-che, is usually a result of a temporary slight drop in E2 concentrations leadingto an estrogen withdrawal hemorrhage. In Europe, menarche occurs around amean age of 13.4 (1115.6) years. Interestingly, 150 years ago the mean age ofmenarche was 17 years [19, 20].
While there is no doubt that estrogens as well as androgens have profoundeffects on behavior, controversy persists as to whether these effects are perma-nent (imprinting) or not [2123]. The classic example of brain imprinting bysex steroids, the androgen-induced permanent inactivation of the LH surgemechanism described in the laboratory rodent, does not seem to occur in pri-mates or in humans [24, 25].
One important role of endogenous E2 is the promotion of growth and epi-physial closure to induce growth arrest. Estrogen deficiency due to mutations inthe aromatase gene and estrogen resistance due to disruptive mutations in theestrogen receptor gene lead to absence of the pubertal growth spurt, delayedbone maturation, unfused epiphyses, continued growth into adulthood andvery tall adult stature in both sexes [11].
Exposure to Endogenous Estrogens During Lifetime 87
-
3.2Male Puberty
In about 60% of healthy pubertal boys there is clinically visible development ofbreast tissue that is called gynecomastia of puberty. Although these boys havenormal serum concentrations of E2, testosterone, LH and FSH, an increased ra-tio of E2 to testosterone has been reported [26]. However, this observation hasnot been confirmed in more recent studies. Other investigators have observedelevated E2 concentrations in the early morning hours. Breast swelling in boysmay also be explained by the combined effects of an androgen-induced declinein hepatic SHBG synthesis and the higher affinity of SHBG for testosterone ascompared to E2, resulting in a shift of the balance between androgens and es-trogens in favor of estrogenic hormones as long as androgen levels in plasmahave not yet reached final adult levels [27, 28].
Estrogens increase the number of prolactin receptors in breast tissue. Also,E2 has a direct effect on the growth of mammary ducts. In some boys there is afamilial increase in the extraglandular aromatization of C19-steroids raisingserum E1 concentrations and increasing the incidence of gynecomastia [29]. Inaddition to the extraglandular estrogen synthesis, e.g., in adipose tissue, E2 isproduced in testicular tissue leading to E2 concentrations in the pubertal boythat are much higher than those found before puberty.
Estrogen deficiency due to mutations in the aromatase gene and estrogen re-sistance due to disruptive mutations in the estrogen receptor gene have no ef-fect on normal male sexual maturation in puberty [11].
4Role of Estrogens in the Adult Woman and Man During Reproductive Age
4.1Estrogens During the Menstrual Cycle Regulation of the Ovarian and Uterine Function
Increasing concentrations of FSH induce the aromatization of androgens in thegranulosa cells of the ovary, thus elevating E2 concentrations. E2 and FSH in-crease the FSH receptor concentration of the granulosa cells of the ovarian fol-licle. The peripheral E2 concentrations increase further and lead, together withovarian inhibin, to a feedback inhibition of FSH secretion. When E2 levels ex-ceed a certain threshold for a defined period of time, indicating the full matu-ration of the ovarian follicle, a massive increase of pituitary LH and FSH secre-tion is induced resulting in ovulation and corpus luteum formation. However,the growth of preovulatory follicles can proceed with minimal concentrationsof LH and FSH in the presence of low peripheral estrogen levels [30]. Oocytematuration and fertilization may proceed independently of ambient estrogenlevels. This leads to the assumption that estrogens exert a minimal autocrine-paracrine function [31].
88 J. Dtsch et al.
-
The rising E2 levels in the follicular phase result in proliferation of the uterineendometrium and in an increase of the number of glands. There is an increase inthe amount and a change in the physicochemical properties of the cervical mu-cus (Spinnbarkeit). The decline of E2 and progesterone in the late luteal phaseleads to a loss of endometrial blood supply and eventually to the onset of menses.
4.2Estrogen Regulation of the Mucosal Immune System
The mucosal immune system in the female reproductive tract is the first line ofdefense against pathogenic organisms. Immunoglobulin A (IgA) and IgG levelsin uterine secretions change markedly during the rat estrous cycle, with higherlevels measured at ovulation than during any other stage of the cycle [32].Whenovariectomized animals are treated with E2, IgA and IgG levels markedly riserelative to untreated controls. These results underline the role of estrogens inthe regulation of the local uterine defense mechanisms, enabling a pathogen-free environment for the implantation of the blastocyst.
4.3Estrogen Effects Outside the Reproductive System
The protective effects of endogenous estrogens against disorders of the cardio-vascular system, the skeletal system and central nervous functions have beenthoroughly investigated with respect to the estrogen deficiency after meno-pause. Therefore, these aspects will be discussed in the section on the meno-pause. It should be stated, however, that young women with estrogen deficiencydue to mutations in the aromatase gene and estrogen resistance due to disrup-tive mutations in the estrogen receptor gene achieve no normal bone mineralmass and have disturbances in insulin sensitivity and lipid homeostasis [11].Similar observations were made in young women with amenorrhea.
4.4Adverse Effects of Endogenous Estrogens
Despite the protective effects of estrogens on many organ systems in adultwomen, it is well known that some effects on the breast and the uterine en-dometrium are undesirable. Long-lasting uterine exposure to E2 alone resultsin endometrial hyperplasia and may ultimately promote endometrial cancer.The role of endogenous estrogens for the development of breast cancer is lessclear. Estrogen receptor variants and mutations have been shown to be associ-ated with a higher risk of breast cancer [33]. It could be demonstrated by anumber of groups that blocking of the estrogen-receptor by the anti-estrogentamoxifen lowers the recurrence of breast cancer or reduces the size of the tu-mor. Moreover, the additional production of estrogens by the adipose tissuemay enhance the risk of breast cancer in premenopausal as well as post-menopausal women [34]. However, it is not clear to what extent these observa-tions depend on changes in the metabolism of progestins.
Exposure to Endogenous Estrogens During Lifetime 89
-
4.5Role of Endogenous Estrogens for the Fertile Man
The role of estrogens in the genesis of gynecomastia during puberty has alreadybeen discussed. However, elevated estrogen concentrations may also lead togynecomastia in the adult man. A typical example is found in hepatic cirrhosisthat results in a reduced hepatic ability to conjugate active estrogens and to ren-der them inactive.
Endogenous estrogens are absolutely necessary for the reproductive capabil-ities in mice. Knockout experiments clearly show that male mice lacking the es-trogen receptor alpha are infertile [10]. These mice exhibit atrophy of the testesand dysmorphogenesis of the seminiferous tubule. The prenatal development ofthe reproductive tract, however, is not affected by the estrogen receptor knock-out. In human males, however, estrogen deficiency due to mutations in the aro-matase gene and estrogen resistance due to disruptive mutations in the estro-gen receptor gene is predominantly associated with reduced bone mass and delayed epiphysial closure [10, 11].
5Role of Estrogens in Conception and Pregnancy
5.1Conception and Blastocyst Implantation
In the ovary, follicles grow under the influence of gonadotropins and local growthfactors. During the normal menstrual cycle, only one follicle of the cohort ofgrowing follicles reaches the preovulatory stage while the remaining follicles un-dergo atresia. In humans, the E2 levels rapidly increase during the last five daysbefore ovulation.After ovulation, the ruptured follicle luteinizes and the resultingcorpus luteum secretes progesterone and E2. E2 secretion is increased during theluteal phase, corresponding to the increase in progesterone. The magnitude of theE2 secretion increase during the luteal phase, however, is not as high as during thefollicular phase [35]. The time course of E2, progesterone, LH, FSH and prolactinsecretion during the menstrual cycle is shown in Fig. 3.
After conception, E2 plays an important role for the implantation of the blas-tocyst in the uterus. It has been shown in ovariectomized rodents that the pre-exposition of the uterus to progesterone alone does not lead to a successful im-plantation of the blastocyst [36]. Implantation can be induced in ovariec-tomized mice and rats by doses of estrogens that are much smaller than thoseneeded for behavioral changes [37]. The estrogen action is mediated by growthfactors at the local sites [36].
5.2Estrogen Production in Pregnancy
The regulation of estrogen production during pregnancy has been thoroughlyinvestigated two to three decades ago. Prior to four weeks of gestation, the ma-
90 J. Dtsch et al.
-
jority of E2 secreted into maternal blood is synthesized in the maternal ovaries[38].After the fourth postovulatory week, however, bilateral oophororectomy orsurgical removal of the corpus luteum does not diminish the levels of estrogensexcreted in urine [39]. By seven weeks of gestation, the majority of estrogensentering both maternal and fetal compartments is of placental origin [40].
Near term, estrogen production is 1000 times the average daily estrogen pro-duction in normal ovulatory women. As a consequence, the maternal plasmaconcentration of E3, the most important estrogen in pregnancy, reaches levelsat term that are 1000-fold those in the plasma of non-pregnant women [41].Similarly, the maternal E2 and E1 concentrations in plasma increase from50100 pg/mL (on average) to 30,000 pg/mL at term [42]. Fifty percent of E2near term is derived from fetal adrenal dehydroepiandrosterone sulfate(DHEAS) and 50% from maternal DHEAS (Fig. 4). On the other hand, 90% ofE3 in maternal plasma is produced by the placenta from fetal plasma 16a-hy-
Exposure to Endogenous Estrogens During Lifetime 91
Fig. 3. Estradiol (E2) concentrations during the normal menstrual cycle in relation to prog-esterone (Prog), LH, FSH and follicle size
-
droxydehydroepiandrosterone sulfate (16a-HO-DHEAS) and only 10% from allother sources. 16a-HO-DHEAS is produced by the fetal liver by sulfation of16a-hydroxydehydroepiandrosterone (16a-DHEA), which is synthesized by thefetal adrenal gland. Due to the absence of 17a-hydroxylase (see Fig. 2), the denovo synthesis of estrogen from cholesterol or C21 steroids in human placenta isimpossible [1]. 8090% of the steroids produced in the placenta are secretedinto the maternal blood [1]. Details of the synthesis of estrogens in the placentaand of the function of the fetoplacental unit are shown in Fig. 4.
5.3Impact of Estrogens on the Mother During Pregnancy
The elevated estrogen concentrations during pregnancy induce the synthesis oftransport proteins like thyroxin-binding globulin, transcortin and SHBG in theliver. Due to the high exposure to E3 in pregnancy, a number of tissues are stim-ulated to proliferate. In particular, uterine size increases up to 300-fold, an ef-fect that is not observed in ERa knockout mice [10]. The development of thebreast ducts is also highly stimulated. Together with a number of other hor-mone systems that are activated in pregnancy, E3 is the predominant estrogenin pregnancy leading to water and electrolyte retention and a number of other
92 J. Dtsch et al.
Fig. 4. Estrogen biosynthesis in the human placenta. Estriol, quantitatively the most impor-tant estrogen produced by the placenta, is synthesized from 16a-hydroxydehydroepiandros-terone sulfate (16a-HO-DHEAS), which is predominantly supplied by fetal blood. Estradiol isalso produced by the normal placenta from dehydroepiandrosterone sulfate (DHEAS) pro-vided by fetal and maternal blood [1]
-
well known gestational changes. However, at least in the human female, E3 doesnot appear to be of critical importance for the maintenance of pregnancy, sincesulfatase deficiency, a disorder resulting in extremely low E3 concentrations inmaternal plasma, has no apparent adverse effect on the course of pregnancy.
5.4Role of Estrogens for Lactation
During pregnancy, the role of the endogenous estrogens is to stimulate thegrowth of breast gland ducts [43], whereas the alveolar development is pre-dominantly induced by progesterone. The high E3 concentrations later in preg-nancy delay the actual onset of lactation. Therefore, only after removal of theplacenta as the major source of estrogen synthesis, does the effect of prolactinon milk production become evident. Induction of milk production and galac-torrhea have also been observed after betamethasone administration for pro-phylaxis of the respiratory distress syndrome of the neonate. Betamethasone isknown to reduce E3 serum levels [44]. Similar effects on lactation are observedafter a rapid decline of E3 serum levels related to fetal distress.
6Menopause and Postmenopause
6.1Physiology and Estrogen Concentrations
Over the past ten years, the menopause has probably been the most investigatedfield of research dealing with endogenous and exogenous estrogens [45]. Onlythe role of estrogens and antiestrogens in the treatment of breast cancer hasbeen of similar interest. Menopause is defined as the last spontaneous men-struation. In Europe, the mean age of menopause is 51 years. In contrast tomenarche, the age of menopause has not changed throughout the last century.Approximately five years prior to the absolute failure of ovarian hormone pro-duction, the first clinical indicators of disturbances of estrogen and proges-terone production manifest with irregular menstrual bleedings. This phase isreferred to as premenopause [46]. Whereas progesterone production drops rel-atively fast during that phase (Fig. 5), E2 synthesis decreases more gradually.These hormonal changes reflect the loss of ovarian follicles that may be stimu-lated. In addition, ovarian blood vessels show regressive changes and eventuallyobliterate.
With the progression of menopause, the E2 levels in the circulation decreaseconsiderably until they reach concentrations that are frequently below 20 pg/mL. These concentrations are insufficient to induce adequate endometrial pro-liferation and subsequent menstrual bleeding. Ovariectomy in postmenopausalwomen does not lead to a further decrease in E2 concentrations, indicating theabsolute loss of ovarian function [47]. Because the negative feedback on pitu-itary gonadotropin secretion is lost, there is a significant continuous increase inserum LH and FSH concentrations (Fig. 5).
Exposure to Endogenous Estrogens During Lifetime 93
-
However, even after menopause there is endogenous estrogen production.One source of small amounts of E2 is the adrenal cortex. In addition, androgenprecursors like DHEA, DHEAS, testosterone and androstenedione are the sub-strates for E1 synthesis by the enzyme aromatase in adipose tissue [48]. Thereis a positive relationship between the amount of adipose tissue and the aro-matase activity. As a consequence, overweight postmenopausal women showhigher serum E1 levels than their lean peers. Therefore, some of these womenhave clear signs of estrogen effects in their target organs.
6.2Consequences of Decreasing Estrogen Concentrations During Menopause
The earliest symptoms of the imminent menopause are menopausal hot flashes.These are characterized by an abrupt increase of skin temperature associatedwith tachycardia, flushing of the skin and sweating. They are caused by anabrupt change of the setpoint of the hypothalamic temperature center to alower level, resulting in peripheral vasodilation and increased sweating that ismediated by sympathetic nerve activity as part of a compensatory mechanismregulating body temperature. It has been demonstrated that the administrationof exogenous estrogens but not progestins may reverse the menopausal hotflashes [49].
Apart from these immediate consequences of E2 withdrawal, the target or-gans suffer from a lack of estrogens and show a number of adverse reactionsduring the postmenopausal phase. Two major organ systems that are affectedby these changes are the cardiovascular system and the skeletal system [50]. The
94 J. Dtsch et al.
Fig. 5. Schematic drawing of the mean serum levels of E2 and E1 in relation to progesterone(P), LH, and FSH during pre- and postmenopause (modified according to ref. [56])
-
cardiovascular system of the fertile woman is considerably less susceptible toarteriosclerosis than that of their male peers. This is at least partially due to aninteraction of estrogens with the nitric oxide system that protects against theemergence of arteriosclerotic plaques [51]. Moreover, there are favorable im-pacts on plasma lipids as well as anti-platelet and antioxidant effects [52]. Assoon as estrogen serum levels drop in the postmenopausal phase, there is arapid increase in the formation of arteriosclerosis in all arterial vessels and asubstantial increase in the risk of myocardial infarction or cerebrovascularthrombosis.
In fertile women between age 30 and 40 years, the annual loss of the bonemass ranges from 0.5 to 1 percent. Due to the lack of E2, this process is acceler-ated up to 10% in the first year after menopause, if estrogens are not replaced.Apart from the mineral components of the skeletal system, the organic sub-stances, i.e., predominantly collagen type I, are removed [53].As a consequence,the risk of bone fractures increases dramatically within the first 1020 years af-ter menopause. Certainly, the loss of bone mass is not exclusively caused by thelack of estrogens. It is also influenced by a lack of physical activity, poor calciumintake and decreasing concentrations of growth hormone.
One novel aspect of the adverse effect of E2 withdrawal during menopause isthe impairment of cognitive functions. Basic neuroscience studies have eluci-dated mechanisms of action of estrogens on the structure and function of brainareas known to be critically involved in memory. Controlled clinical studiesshow that the administration of estrogens to postmenopausal women enhancesverbal memory and maintains the ability to learn new materials. These obser-vations are supported by investigations of healthy, elderly women and by astudy in which younger women received a gonadotropin-releasing-hormoneanalogue that suppressed ovarian function [8, 9].
As a consequence of the collagen type I loss, the skin is affected by the ces-sation of adequate estrogen supply as well. Water content decreases and the epi-dermis becomes thinner. There is also an atrophy of the secretory componentsof the skin. Vagina, uterus and breasts involute as a consequence of estrogenwithdrawal. These organs decrease in size and especially the vagina is more sus-ceptible to trauma. Similar changes are seen in bladder and urethra. Due to theinvolution of these organs, there is a higher incidence of functional urinary in-continence in postmenopausal women.
Because of all these complications, estrogen replacement therapy is generallyrecommended. The correct hormonal treatment, including careful monitoringof its side effects (like an increased susceptibility for breast cancer), may reducegeneral mortality by 3050% [45].
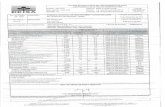
7Tables of Concentrations of Estrogens During Different Phases of Life
It has to be emphasized that the determination of plasma estrogen levels variesconsiderably with the method used. Therefore, three conditions are compulsoryfor any specific assay measuring the three major endogenous estrogens E2, E1and E3:
Exposure to Endogenous Estrogens During Lifetime 95
-
(1) reference values must be provided for every assay,(2) the reference values must not be related to the age but to the different de-
velopmental stage, i.e., puberty and menopause, and(3) the assay must be specific.
The reference values shown below in Tables 13 were established using ra-dioimmunoassay after chromatographic separation. Lately, ultrasensitive assaysfor the determination of E2 concentrations have been introduced. Under certainpathophysiological situations like the premature telarche these new assays al-low for discrimination even in prepubertal girls [14].
96 J. Dtsch et al.
Table 1. Serum estradiol (E2) concentrations during infancy, childhood, different stages ofpuberty according to Tanner [54], and adulthood [55]
Age/Phase Reference values Reference values (conventional units) (SI units)
Girls 1 week7 months < 755 pg/mL < 26201 pmol/L612 months < 744 pg/mL < 26162 pmol/L2nd year < 724 pg/mL < 2688 pmol/L27 years < 712 pg/mL < 2644 pmol/LP I and > 7 years < 720 pg/mL < 2673 pmol/LP II < 735 pg/mL < 26129 pmol/LP III 760 pg/mL 26220 pmol/LP IV 1293 pg/mL 44341 pmol/LP V 12250 pg/mL 44918 pmol/L
Boys 1 week7 months < 725 pg/mL < 2692 pmol/L612 months < 719 pg/mL < 2670 pmol/L2nd year < 717 pg/mL < 2661 pmol/L27 years < 711 pg/mL < 2640 pmol/LP I and > 7 years < 714 pg/mL < 2651 pmol/LP II < 715 pg/mL < 2655 pmol/LP III 826 pg/mL 2996 pmol/LP IV 932 pg/mL 33118 pmol/LP V 1239 pg/mL 44142 pmol/L
Women Follicular phase 30300 pg/mL 1101100 pmol/LOvulation 300400 pg/mL 11001450 pmol/LLuteal phase > 130 pg/mL > 470 pmol/LPostmenopause < 20 pg/mL < 70 pmol/L
Men < 50 pg/mL < 180 pmol/L
-
Table 2. Serum estrone (E1) concentrations during infancy, childhood, different stages ofpuberty according to Tanner [54], and adulthood [55]
Age/Phase Reference values Reference values (conventional units) (SI units)
Girls 1 week7 months < 727 pg/mL < 26100 pmol/L612 months < 716 pg/mL < 2660 pmol/L2nd year < 714 pg/mL < 2652 pmol/L27 years < 717 pg/mL < 2663 pmol/LP I and >7 years < 729 pg/mL < 26107 pmol/LP II < 737 pg/mL < 26137 pmol/LP III 853 pg/mL 26196 pmol/LP IV 1053 pg/mL 44285 pmol/LP V 12142 pg/mL 44525 pmol/L
Boys 1 week7 months < 721 pg/mL < 2678 pmol/L612 months < 721 pg/mL < 2678 pmol/L2nd year < 718 pg/mL < 2668 pmol/L2X7 years < 713 pg/mL < 2648 pmol/LP I and >7 years < 719 pg/mL < 2670 pmol/LP II 1130 pg/mL 41111 pmol/LP III 1131 pg/mL 41115 pmol/LP IV 1541 pg/mL 56152 pmol/LP V 2147 pg/mL 78174 pmol/L
Women fertile phase 20182 pg/mL 74673 pmol/Lpostmenopause 1580 pg/mL 53280 pmol/L
Men 2248 pg/mL 81178 pmol/L
Table 3. Estriol (E3) concentrations in the maternal serum during the course of gestation [55]
Week of gestation Reference values (conventional units) Reference values (SI units)
20 1.33.2 ng/mL 4.511.1 nmol/L21 1.33.6 ng/mL 4.512.5 nmol/L22 1.44.0 ng/mL 4.913.9 nmol/L23 1.44.4 ng/mL 4.915.3 nmol/L24 1.55.0 ng/mL 5.217.4 nmol/L25 1.65.2 ng/mL 5.618.0 nmol/L26 1.85.6 ng/mL 6.219.4 nmol/L27 2.06.0 ng/mL 6.920.8 nmol/L28 2.26.5 ng/mL 7.622.6 nmol/L29 2.46.9 ng/mL 8.323.9 nmol/L30 2.67.2 ng/mL 9.025.0 nmol/L31 2.87.7 ng/mL 9.726.7 nmol/L32 2.98.4 ng/mL 10.129.1 nmol/L33 3.010.0 ng/mL 10.434.7 nmol/L34 3.212.0 ng/mL 11.141.6 nmol/L35 3.513.8 ng/mL 12.147.9 nmol/L36 4.016.0 ng/mL 13.955.5 nmol/L37 4.818.0 ng/mL 16.762.5 nmol/L38 5.519.5 ng/mL 19.167.7 nmol/L39 6.020.0 ng/mL 20.869.4 nmol/L40 6.420.3 ng/mL 22.270.4 nmol/L41 6.720.0 ng/mL 23.269.4 nmol/L42 6.019.5 ng/mL 20.867.7 nmol/L
-
8References
1. Casey ML, MacDonald PC (1992) Alterations in steroid production by the human pla-centa. In: Pasqualini JR, Scholler R (eds), Hormones and fetal pathophysiology. MarcelDekker, New York, p 251
2. Grody WW, Schrader WT, OMalley BW (1985) Endocrin Rev 3:1413. Lipsett MB (1986) Steroid hormones. In: Yen SSC, Jaffe RB (eds), Reproductive en-
docrinology. Saunders, Philadelphia, p 1404. Couse JF, Korach KS (1999) Endocrin Rev 20:3585. Bhat RA, Harnish DC, Stevis PE, Lyttle CR, Komm BS (1998) J Steroid Biochem Mol Biol
67:2336. Couse JF, Lindzey J, Grandien K, Gustafsson JA, Korach KS (1997) Endocrinology
138:46137. Taylor JA, Lewis KJ, Lubahn DB (1998) Mol Cell Endocrinol 145:618. Sherwin B (1998) Proc Soc Exp Biol Med 217:179. McEwen BS, Alves SE (1999) Endocrin Rev 20:279
10. Korach KS, Couse JF, Curtis SW,Washburn TF, Lindzey J, Kimbro KS, Eddy EM, MigliaccioS, Snedeker SM, Lubahn DB, Schomberg DW, Smith EP (1996) Recent Prog Horm Res51:159
11. MacGillivray MH, Morishima A, Conte F, Grumbach M, Smith EP (1998) Horm Res 49(Suppl 1) :2
12. Rey-Stocker I (1997) Weibliche Keimdrsen. In: Stolecke H (ed), Endokrinologie desKindes und Jugendalters. Springer, Berlin Heidelberg New York, p 153
13. Kelch RP, Khoury SA, Hale PM (1987) The episodic secretion of hormones. In: CrowleyWF, Hoffer JG (eds), Churchill-Livingston, New York, p 187
14. Klein KO, Mericq V, Brown-Dawson JM, Larmore KA, Cabezas P, Cortinez A (1999) JPediatr 134:190
15. Kulin HE, Grumbach MM, Kaplan SL (1969) Science 166:101216. Grumbach MM, Kaplan SL (1990) The neuoendocrinology of human puberty: an ont-
genetic perspective. In: Grumbach MM, Sizonenko, Aubert ML (eds), Control of the onsetof puberty. Williams and Wilkins, Baltimore, p 1
17. Ruf KB (1973) J Neurol 204:9518. OByrne KT, Chen MD, Nishihara M, Williams CL, Thalabard JC, Hotchkiss J, Knobil E
(1993) Neuroendocrinology 57:58819. Tanner JM (1973) Nature 243:9520. Tanner JM, Eveleth PB (1985) Changes at age in menarche in Scandinavian countries,
18401978. In: Berenberg SR (ed), Puberty, biologic and psychosocial components. HEStenfert Krose, Leiden, p 256
21. Beyer, Wozniak A, Hutchinson JB (1993) Neuroendocrinology 58:67322. Balthazart J, Ball GF (1995) Trends Endocrinol Metab 6:2123. Balthazart J, Foidart A (1983) J Steroid Biochem Mol Biol 44:52124. Karsch FJ, Dierschke DJ, Knobil E (1973) Science 179:48425. Lopez FJ, Merchenthaler I, Liposits Z, Negro-Vilar A (1996) Cell Mol Neurobiol 16:12926. Moore DC, Schlaepfer LV, Paunier L, Sizonenko PC (1984) J Clin Endocrinol Metab 58:49227. Large DM, Anderson DC (1979) Clin Endocrinol 11:50528. Large DM, Anderson DC, Laing I (1980) Clin Endocrinol 12:29329. Berkovitz GD, Guerami A, Brown TR, MacDonald PC, Migeon CJ (1985) J Clin Invest
75:176330. Taylor AE, Whitney H, Hall JE; Martin K, Crowley WF Jr (1995) J Clin Endocrinol Metab
80:154131. Shoham Z, Schachter M (1996) Fertil Steril 65:68732. Wira CR, Stern JE (1992) Endocrine regulation of the mucosal immune system in the fe-
male reproductive tract. In: Pasqualini JR, Scholler R (eds), Hormones and fetal patho-physiology. Marcel Dekker, New York, p 343
98 J. Dtsch et al.
-
33. Murphy LC, Dotzaw H, Leygue E, Douglas D, Coutts A, Watson PH (1997) J SteroidBiochem Mol Biol 62:363
34. Kuller LH (1995) Public Health Rev 23:15735. Lenton EA (1988) Pituitary and ovarian hormones in implantation and early pregnancy.
In: Chapman M, Grudzinskas G, Chard T (eds), Implantation. Springer, Heidelberg, p 1736. Dey SK, Paria BC, Andrews GK (1991) Uterine EGF ligand receptor circuitry and its role
in embryo-uterine interactions during implantation in the mouse. In: Strauss JF, Lyttle CR(eds), Uterine and embryogenic factors in early pregnancy. Alan R. Liss, New York, p 211
37. Yoshinaga K (1994) Endocrinology of implantation. In: Tulchinsky D, Little AB (eds),Maternal/fetal endocrinology. WB Saunders Company, Philadelphia, p 336
38. Siiteri PK, MacDonald PC (1963) J Clin Endocrinol Metab 26:75139. Csapo AI, Pulkkinen MO, Wiest WG (1973) Am J Obstet Gynecol 15:75940. MacDonald PC, Siiteri PK (1965) J Clin Invest 44:46541. Tulchinsky D, Hobel CJ, Korenman SG (1971) Am J Obstet Gynecol 111:31142. Lindberg BS, Johannon EDB, Nilsson BA (1974) Acta Obstet Gynecol Scand 32:2143. Topper YJ (1970) Recent Progr Horm Res 26:28744. Kjer JJ, Hess J (1983) Acta Obstet Gynecol Scand 62:30745. Greendale GA, Lee NP, Arriola ER (1999) Lancet 353:57146. Treolar AE, Boynton RE, Behn BG, Brown DW (1967) Int J Fertil 12:7747. Judd HL, Koreman SG (1982) Effects of aging on reproductive function in women. In:
Koreman SG (ed), Endocrine aspects of aging. Elsevier Biomedical, Amsterdam, p 16348. Longcope C, Pratt JH, Schneider SH, Fineberg SE (1978) J Clin Endocrinol Metabol 46:14649. Meldrum DR, Shamonk IM, Frumar AM, Tataryn IV, Shang RJ, Judd HL (1979) Am J
Obstet Gynecol 135:71350. Leidenberger (1992) Endokrinologie der perimenopausalen bergangsphase, der
Menopause und des Seniums. In: Klinische Endokrinologie fr Frauenrzte. Springer,Berlin Heidelberg New York, p 101
51. Bell DM, Johns TE, Lopez LM (1998) Ann Pharmacother 32:45952. Maxwell SR (1998) Basic Res Cardiol 93 Suppl 2 :7053. Brincat M, Monitz CF, Kabalan S (1987) Br J Obstet Gynaecol 94:12654. Bidlingmaier F, Butenandt O, Knorr D (1977) Pediatr Res 11:9155. Allolio B, Schulte HM (1996) Praktische Endokrinologie. Urban und Schwarzenberg,
Mnchen, p 73456. Rudolf K (1996) Klimakterium-hormonelle Substitution. In: Allolio B, Schulte HM (eds),
Praktische Endokrinologie. Urban und Schwarzenberg, Mnchen, p 470
Exposure to Endogenous Estrogens During Lifetime 99

![[XLS] Web view1234 2001 10/1/1952 1235 2001 7/1/1964 1236 2001 8/1/1960 1237 2001 3/1/1965 1238 2001 4/1/1953 1239 2001 5/1/1964 1240 2001 6/1/1965 1241 2001 7/1/1957 1242 2001 9/1/1959](https://static.fdocuments.net/doc/165x107/5b0d7ea47f8b9a2c3b8d448b/xls-view1234-2001-1011952-1235-2001-711964-1236-2001-811960-1237-2001-311965.jpg)