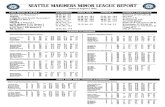
DMART Space Infections 08.06.14
description
Transcript of DMART Space Infections 08.06.14
Fascial Spaces
These areas are potential spaces that do not exist in healthy people but become filled with
purulent exudate during infections.
Contemporary Oral and Maxillofacial Surgery, 4th Edition
Fascial Space Infections
• Usually caused by odontogenic infection eroding through cortical bone.
• Usually erode through thinnest bone.• Space invaded determined by muscle
attachment.
Today’s Outline
1. General Information2. Fascial Space Infections
– Infections associated with any tooth– Infections associated with Maxillary teeth– Infections associated with Mandibular teeth– Infections associated with deep fascial spaces of
the neck (secondary fascial spaces)3. Management of Fascial Space Infections
General Information
• Indigenous bacteria usually causative of infection– Staph – Skin– Normal Oral Flora – Odontogenic Infections
• Aerobic Gram Positive Cocci• Anaerobic Gram Positive Cocci• Anaerobic Gram Negative Rods
• Only Aerobic Infections 5-7%• Only Anaerobic Infections 33-35%• MIXED Infections 60%
General Information
• Anaerobic 75%
– Gram-positive cocci 30%• Streptococcus 33%• Peptostreptococcus 65%
– Gram-negative cocci (Veillonella) 4%
– Gram-positive rods 14%• Eubacterium• Lactobacillus• Actinomyces• Clostridia
– Gram-negative rods 50%• Bacteroides 75%
-Porphymonas ginivalis -Prevotella intermedia
• Fusobacterium 25%
– Miscellaneous 6%
• Aerobic 25% Gram-positive cocci 85%
Streptococcus 90% Group D Streptococcus 2% Staphylococcus 6% Eikenella 2%
Gram-negative cocci (Neisseria) 2%
Gram-positive rods (Corynebacterium) 3%
Gram-negative rods (Haemophilus) 6%
Misc 4%
Progression of Infection
• Inoculation– First 3 days, normal color and feel– Presence of edema– Mild malaise and pain
• Cellulitic Process– Days 3-7, hot, red, firm, extremely tender– Serosanguineous tissue fluid– Severe malaise and pain, show cardinal signs of
inflammation
Progression of Infection
• Abscess– > 5 days, fluctuant to palpation– Pus pocket, yellowish color with red periphery– Moderate to severe malaise and pain
• Resolution– After spontaneous or surgical drainage
Aerobic Gram (+) => Anaerobic Gram ( - ) => increase in Beta-lactamase
Cellulitis vs. Abscess
• Cellulitis– Acute Onset– Severe, Generalized Pain– Large area with diffuse
borders– Doughy to indurated on
palpation– Little or No Pus– More Serious– Aerobic Bacteria
• Abscess– Chronic Process– Localized Pain– Small area with well
circumscribed borders– Fluctuance on palpation– Presence of Pus– Less Serious– Anaerobic Bacteria
Today’s Outline
1. General Information2. Fascial Space Infections
– Infections associated with any tooth– Infections associated with Maxillary teeth– Infections associated with Mandibular teeth– Infections associated with deep fascial spaces of
the neck (secondary fascial spaces)3. Management of Fascial Space Infections
Space Buccal
Ant. Border
Corner of mouth
Post. Border
Masseter, pterygo-mand sp.
Sup. Border
Maxilla, infraorb. sp.
Inf. Border
Mandible, skin
Medial/ Deep
Subcut- aneous
Lateral/ Superficial
Buccinat.
Likely causes
Mx can. Mx molar Md can.
Contents Parotid d. Ant. Fac a/v, trans fac a/v, buccal fat
Neigh-boring spaces
Infraorb, Pterygom, Infratemp
Approach for I&D
Intra (sm) Extra (lg)
- Potential space between skin laterally and
Buccinator medially.- Usually caused by Maxillary molar infection
but can be caused by Mandibular molar- Clinically, does not extend past inferior
border of mandible- I&D: subperiosteal dissection through
extraction site or through vestibular mucosa
Buccal
1. Fascial Space Infections– Infections associated with Maxillary teeth
• Infraorbial/Canine• Infratemporal/Deep temporal• Cavernous sinus thrombosis
Space Infra-orbital
Ant. Border
Nasal cartillage
Post. Border
Buccal space
Sup. Border
Quad. Labii sup.
Inf. Border
Oral mucosa
Medial/ Deep
Quad labii sup.
Lateral/ Superficial
Lev ang oris, maxilla
Likely causes
Mx cuspid
Contents Angular a/v, infraorbial n
Neigh-boring spaces
Buccal
Approach for I&D
Intraoral
1) Potential space between levator anguli oris and levator labii superioris muscles
2) Causes loss of nasolabial angle facially
3) Drainage may occur inferior to medial canthus of eye
4) I&D: High in vestibule
Infraorbital
Space Infra- temporal / Deep temporal
Ant. Border
Maxilla
Post. Border
Middle Cranial Fossa
Sup. Border
Base of skull
Inf. Border
Lateral Pterygoid
Medial/ Deep
Lateral pterygoidplate
Lateral/ Superficial
Continuous with deep temporal space
Likely causes
Mx molars
Contents Pterygoid plx, mx a/v, V3
Neigh-boring spaces
Buccal Sup.Temp Inf. Petr sinus
Approach for I&D
Intraoral Extraoral
1) Posterior to maxilla, below skull base2) Caused by maxillary third molar infections3) Contents include maxillary artery and
pterygoid plexus (infection may track to dural sinuses)
4) Rare in isolation5) I&D: Vertical incision
medial to anterior ramus, superior dissection along medial coronoid
Infratemporal/Deep Temoral
Cavernous Sinus Thrombosis
- Life threatening infection caused by retrograde flow of odontogenic infection through valve-less veins in head.
- Vascular inflammation caused by bacteria stimulate clotting pathways.- Occurs anteriorly through inferior or superior ophthalmic veins and posteriorly through
emissary veins and pterygoid plexus.- Lateral Rectus (CNVI) Palsy: Impaired extraocular movements laterally.- Treatment is immediate antibiotic therapy and removal of infection whenever possible.
1. Fascial Space Infections– Infections associated with Mandibular teeth
• Submandibular• Sublingual • Submental• Pterygomandibular• Submasseteric
Submental
- Infections from mandibular incisors erode through
lingual plate apical to mentalis muscle
- Isolated submental space infections uncommon,
usually caused by spread of submandibular space
infection.
- Discrete swelling noted in central submandibular
region
- I&D: Extraoral transverse incison.
Space Sub-mental
Ant. Border
Inf border of md.
Post. Border
Hyoid
Sup. Border
Mylohyoid
Inf. Border
Inv. fascia
Medial/ Deep
Inv fascia
Lateral/ Superficial
Ant bellies digastric
Likely causes
Md inc, symphysis frxr
Contents Ant. Jug v, lymph nodes
Neigh-boring spaces
Submandibular
Approach for I&D
Extraoral
Space Submandibular
Ant. Border
Ant belly digastric,
Post. Border
Post belly digastric, stylohy, stylophar.
Sup. Border
Inf/Med mandible
Inf. Border
Digastric tendon
Medial/ Deep
Mylohyoid, hyoglossus, sup const mm
Lateral/ Superficial
Platysma
Likely causes
Md molars
Contents Submand gl, facial a/v, lymph nodes
Neigh-boring spaces
Subling, Subment, Buccal, Lat phary
Approach for I&D
Extraoral
Submandibular - Can be progress rapidly into deeper spaces. - May cause elevation, swelling, induration and displacement of the tongue. - Extraoral swelling usually obvious, inferior border of mandible not visible. - Associated with trismus, drooling, dysphagia, dyspnea. - I&D: extraoral incision parallel to inferior border 1-2 cm below to avoid structures.
Space Sub-lingual
Ant. Border
Lingual mandible
Post. Border
Submand space
Sup. Border
Oral mucosa
Inf. Border
Mylohyoid
Medial/ Superfical
Tongue muscles
Lateral/ Deep
Lingual mandible
Likely causes
Md bicusp Md molar direct trauma
Contents Sublng gl, whartons lingual n. sublng a/v
Neigh-boring spaces
Submand, Lat phar, Viscera
Approach for I&D
Intra/Extr
Sublingual
- Intraoral swelling leads to tongue elevation.- Extraoral swellings uncommon- Progressively becomes bilateral- Posterior border of space communicates with
submandibular space leading to larger infections- I&D: anterior/posterior incision near lingual cortex
avoiding Wharton’s, Lingual a/n
Ludwig’s Angina
- Bilateral cellulitis of Submaxillary space (comprised of submental, sublingual and submandibular spaces).
- May cause respiratory distress and airway obstruction, often times rapidly from epiglottis edema.
- Severe swelling, tongue elevation and board like induration noted.
- May cause severe anxiety, furthering respiratory distress.
Space Pterygo-mandibular
Ant. Border
Buccal space
Post. Border
Parotid gland
Sup. Border
Lateral pteryg m.
Inf. Border
Inf border mandible
Medial/ Deep
Medial Pterygoid
Lateral/ Superficial
Asc ramus mandible
Likely causes
Md 3rds, Md angle frxr
Contents V3, Inf alv. a/v
Neigh-boring spaces
Buccal, Lat phar, Masseteric, Temp.
Approach for I&D
Intraoral Intra/Extr
Pterygomandibular
- Site of inferior alveolar nerve block. May be caused by needle tract infection.- Little or no facial swelling is involved- Intraoral swelling seen on anterior tonsillar pillar on affected side + deviation of uvula contralaterally- Significant trismus usually noticed- I&D: Intraoral vertical incision lateral to raphe, disect along
medial surface of ramus. Beware lingual nerve.
Space Sub-masse-teric
Ant. Border
Buccal space
Post. Border
Parotid gland
Sup. Border
Zygomatic arch
Inf. Border
Inf border mandible
Medial/ Deep
Asc ramus mandible
Lateral/ Superficial
Masseter
Likely causes
Md 3rds Md angle frxr
Contents Masseteric a/v
Neigh-boring spaces
Buccal Pterygomandular, Temporal
Approach for I&D
Intraoral Intra/Extr
(Sub)Masseteric
- Commonly results from spread of buccal space infection or pericoronitis of mandibular third molars.
- Moderate to severe trismus due to inflammation of masseter muscle
- Mandibular angle fracture may cause infection- CT/MRI often helpful in identification- Submassetric + Pterygomanidbular + Temporal
Spaces = Masticator Space- I&D: Extraoral posterior to mandibular angle
1. Fascial Space Infections– Infections associated with deep fascial spaces of
the neck• Lateral pharyngeal• Retropharyngeal• Danger
Space Lateral Phar-yngeal
Ant. Border
Pterygomand raphe
Post. Border
Carotid sh., scalene fascia, parotid
Sup. Border
Skull base
Inf. Border
Hyoid bone
Medial/ Deep
Phary Const, retrophar space
Lateral/ Superficial
Medial pterygoid,
Likely causes
Md 3rds, tonsillar infxn
Contents Carotid a, Int Jug v, Vagus n, Cervical SNS chain
Neigh-boring spaces
Pterygom Submand Sublingual Retrophar
Approach for I&D
Intra Intra/Extr
Lateral Pharyngeal Space
- Pterygomandibular, submandibular or sublingual space infections may spread first into this space.
- Primary clinical findings include trismus, dysphagia and fever.
- Lateral swelling of the neck usually seen between angle of mandible and sternocleidomastoid.
- Complications include internal jugular thrombosis, erosion of carotid artery and compression of CN IX,X,XII.
Space Lateral Phar-yngeal
Ant. Border
Sup/Mid Constrictor mm.
Post. Border
Carotid sheath, scalene fascia
Sup. Border
Skull base
Inf. Border
Hyoid bone
Medial/ Deep
Phary Const, retrophar space
Lateral/ Superficial
Medial pterygoid
Likely causes
Md 3rds, tonsillar infxn
Contents Carotid a Int Jug v Vagus n Cerv SNS chain
Neigh-boring spaces
Pterygom Submand Sublingual Retrophar
Approach for I&D
Intra Intra/Extr
Lateral Pharyngeal I&D
- Intraorally, vertical incision medial to raphe, dissect along medial side of medial pterygoid m. - Intraoral drainage is risky
- Extraorally, incise anterior and inferior to the angle of the mandible, dissect superiorly and medially along the deep surface of the medial pterygoid m.
- Also extraorally anterior to SCM
Space Retropharyngeal
Ant. Border
Sup/Mid Constrictor mm.
Post. Border
Alar fascia
Sup. Border
Skull base
Inf. Border
Alar/pre-vert fascia near C6-T4
Medial/ Deep
Midline
Lateral/ Superficial
Carotid sheat, lateral pharyng sp.
Likely causes
Spread from primary space
Contents Potential space
Neigh-boring spaces
Lateral pharyngeal, danger space
Approach for I&D
Retropharyngeal Space
- Essentially a potential space between prevertebral (posterior) and viseral (anterior) fascial compontents.
- Infections may track down through superior mediastinum space causing mediastinitis.
Mediastinitis can lead to compression of the heart and lungs, interfere with
neurologic control of heart and lungs via CN X compression, spread to lungs,
trachea and abdominal cavity.
Danger Space (Space 4): Immediately posterior to retropharyngeal space
separated by thin Alar fascia. Infections from Danger space may track inferiorly
into posterior mediastinum.
Space Retropharyngeal
Ant. Border
Sup/Mid Constrictor mm.
Post. Border
Alar fascia
Sup. Border
Skull base
Inf. Border
Alar/pre-vert fascia near C6-T4
Medial/ Deep
Midline
Lateral/ Superficial
Carotid sheat, lateral pharyng sp.
Likely causes
Spread from primary space
Contents Potential space
Neigh-boring spaces
Lateral pharyngeal, danger space
Approach for I&D
Retropharyngeal Incision & Drainage
• Intraorally through vertical incision in the mucosa of the pharyngeal wall lateral to midline (+/- through lat pharyngeal), caution with pus aspiration
• Extraorally with incision parallel to SCM along ant border, below hyoid. Retract carotid sheath, finger dissection
Space Buccal Infra-orbital
Infratemporal/ Deep Temporal
Sub-mental
Submandibular
Sub-lingual
Pterygo-mandibular
Sub-masse-teric
Lateral Phar-yngeal
Retropharyngeal
Pre tracheal
Ant. Border
Corner of mouth
Nasal cartillage
Maxilla Inf border of md.
Ant belly digastric,
Lingual mandible
Buccal space
Buccal space
Sup/Mid Constrictor mm.
Sup/Mid Constrictor mm.
Sterno-thyroid fascia
Post. Border
Masseter, pterygo-mand sp.
Buccal space
Middle Cranial Fossa
Hyoid Post belly digastric, stylohy, stylophar.
Submand space
Parotid gland
Parotid gland
Carotid sheath, scalene fascia
Alar fascia Retrophar space
Sup. Border
Maxilla, infraorb
Quad. Labii sup.
Base of skull Mylohyoid Inf/Med mandible
Oral mucosa
Lateral pteryg m.
Zygomatic arch
Skull base Skull base Thyroid cartillage
Inf. Border
Mandible, skin
Oral mucosa
Lateral pterygoid
Inv. fascia Digastric tendon
Mylohyoid Inf border mandible
Inf border mandible
Hyoid bone Alar/pre-vert fascia
Superior media-stinum
Medial/ Deep
Subcut- aneous
Quad labii sup.
Lateral pterygoidplate
Inv fascia Mylohyoid, hyoglossus, sup const mm
Tongue muscles
Medial Pterygoid
Asc ramus mandible
Phary Const, retrophar space
Midline Sterno-thyroid fascia
Lateral/ Superficial
Buccinat. Lev ang oris, maxilla
Continuous with deep temporal space
Ant bellies digastric
Platysma Lingual mandible
Asc ramus mandible
Masseter Medial pterygoid
Carotid sheat, lateral pharyng sp.
Viseral fascia
Likely causes
Mx can. Mx molar Md can.
Mx cuspid Mx molars Md inc, symphysis frxr
Md molars Md bicusp Md molar direct trauma
Md 3rds, Md angle frxr
Md 3rds Md angle frxr
Md 3rds, tonsillar infxn
Spread from primary space
Spread form primary or retropharyngeal space
Contents Parotid d. Ant. Fac a/v, trans fac a/v, buccal fat
Angular a/v, infraorbial n
Pterygoid plx, mx a/v, V3
Ant. Jug v, lymph nodes
Submand gl, facial a/v, lymph nodes
Sublng gl, whartons lingual n. sublng a/v
V3, Inf alv. a/v
Masseteric a/v
Carotid a Int Jug v Vagus n Cerv SNS chain
Potential space
Potential space
Neigh-boring spaces
Infraorb, Pterygom, Infratemp
Buccal Buccal Sup.Temp Inf. Petr sinus
Submandibular
Subling, Subment, Buccal, Lat phary
Submand, Lat phar, Viscera
Buccal, Lat phar, Masseteric, Temp.
Buccal Pterygomandular, Temporal
Pterygom Submand Sublingual Retrophar
Lateral pharyngeal
Retropharyngeal
Approach for I&D
Intra (sm) Extra (lg)
Intraoral Intraoral Extraoral
Extraoral Extraoral Intra/Extr Intraoral Intra/Extr
Intraoral Intra/Extr
Intra Intra/Extr
Intra/Extra Intra/Extra
Today’s Outline
1. General Information 2. Fascial Space Infections
– Infections associated with any tooth– Infections associated with Maxillary teeth– Infections associated with Mandibular teeth– Infections associated with deep fascial spaces of
the neck (secondary fascial spaces)3. Management of Fascial Space Infections
1) Determine Severity
2) Host Defenses
4) Treat Surgically
5) Medical Support
3) Setting of Care
7) Complete Follow Up
6) Antibiotic Regimen
Management of Fascial Space Infections
1Determine Severity of Infection
• History of present illness very important• Location
• Thorough clinical examination important• Rate of progression
• Onset of symptoms compared to current signs and symptoms.
• Potential for airway compromise• Evaluate for stridor/coarse airway sounds, posture (chin
elevation, forward lean)
2Evaluate Host Defenses
- Diabetes, steroid therapy, organ transplants, malignancy, chemotherapy, chronic renal disease, malnutrition, alcoholism, end stage AIDS.
- Febrile patients at risk for dehydration which may lead to increased cardiovascular and respiratory demands.
3Choose Setting of Care
- General Indications for hospital admission- Temperature elevation > 101F- Dehydration- Airway obstruction threat (moderate/high severity spaces)- Need for general anesthesia
- Inability to achieve adequate local anesthesia- Secure airway
4Treat Surgically
- Good communication with anesthesia team for airway management
- Early surgical intervention advocated- Consider needle decompression to reduce risk of abscess rupture
into airway (especially pterygomandibular, lateral pharyngeal, submandibular, sublingual). - Small incisions and blunt dissection- never close beaks in
wound- Make use of CT scans- Finger as a dissection tool- Culture & Sensitivity testing
- Communication with lab essential
Extraoral Sites for I&D of Deep Space Infections
A) Temporal
B) Submental Submandibular
C) Submandibular Masseteric
D) Lateral Pharyngeal Retropharyngeal
E) Retropharyngeal
5Support Medically
- Goal is to return patient to homeostasis- Fluid balance/electrolyte balance- Nutrition- Increased metabolic demands- Fever control- studies show initial temperature at
presentation correlated to length of hospital stay- Hydration - Ambulation- Utility of labs- WBC, Prealbumin, CRP
6Choose and Prescribe Antibiotic Properly
InpatientAmpicillin + sulbactamAmpicillin + metronidazoleClindamycinThird Generation Cephalosporin Moxifloxacin/Levofloxacin
OutpatientPCN, Amoxicillin, Augmentin - + 80% effectiveness Clindamycin- rapidly rising resistance Azithromycin Moxifloxacin- > 18 year old
7Evaluate the Patient Frequently
- Outpatient- Evaluate 2 days post op - May remove drain if symptoms improving
- Inpatient- Daily wound care, irrigation- Culture & Sensitivity - Ideal improvement within 48-72 hours
Treatment Failure
- Inadequate Surgery - Depressed host defenses - Foreign body - Antibiotic problems
References
• Ghali, GE, Larsen PE, Waite, DP. Peterson’s Principles of Oral and Maxillofacial Surgery, 2nd Edition. BC Decker
• Hupp, James R.. Contemporary Oral and Maxillofacial Surgery, 5th Edition. Mosby, 032008.
• Langlais, Robert P.. Color Atlas of Common Oral Diseases, 3rd Edition. Lippincott Williams & Wilkins, 012003.
• Neville, Brad W.. Color Atlas of Clinical Oral Pathology, 2nd Edition. Williams & Wilkins, 011999
• Liebgott, Bernard. The Anatomical Basis of Dentistry, 2nd Edition. Mosby, 012001. 5.2.1.3