Dimensions of metai framework components of metai-ceramic … · 2019. 9. 13. · sized connectors...
Transcript of Dimensions of metai framework components of metai-ceramic … · 2019. 9. 13. · sized connectors...
-
Prosthodontics
Dimensions of metai framework components ofmetai-ceramic fixed partiai dentures constructed ina dental school setting
Ridwaan Omar, BSc, BDS, LDS RCS, MSc, FRACDS, FDS RCSEdVTahq Abduljabbar, BDS, MS, PhD /̂Khalil AI-AN, BDS, MSc /̂Michael SmyihVRaied El-Agourî
Objectives: Th9 aims of this study were to measure the dimensions of connectors and retainer copings ofm9tal-ceramic fixed partial denture (FPD) frameworks and to explore, by means ol a questionnaire, thefactors viewed by technicians as important in their planning and provision of such dimensions. Methodand materials: Using two calliper devices, measurements were made of 66 consecutive FPDs under pro-duction in a dental schooi-based iaboratory. The dimensions ot 176 connectors and 124 retainers wereanalyzed with reference to FPD length and to number ot pontics in a span. Questionnaires were com-pietedby ail 14 technicians working in the fixed prosthodontics section ot the laboratory. Results: Thelargest mean verticai connector dimensions were in the anterior regions of both arches, while the largestmean horizontal dimensions were in the posterior regions. Dimensions were unrelated to FPD size andlength of interabulment span. The minimum thickness of the retainer coping walis was generaily beicw op-timal recommendations. Availabie space was the factor most commcniy cited by technicians as dictatingthe dimensions that they applied. Conclusion: Dimensions were generally smaiier than current recom-mendations, which the questionnaire responses indicate are largely due to space constraints.(Quintessence Int 2004:35:820-825)
Key words: connector, dentai technician, fixed partiai denture, framework, metal-ceramic restoration
CLINICAL RELEVANCE: The frequent finding of under-sized connectors and retainer thicknesses of FPD frame-works, in relation to published recommendations, couldpresent an increased risk tor technical failures. Alter-natively, the relatively infrequent occurrence ol suchcauses of clinical failure in loilow-up studies suggests thatmore needs to be known about the appropriateness olstandards currently recommended lor PPD Iramewcrkdimensions.
•'Professor, Department of Prosthetic Dental Sciences, College of Denlistry,King Saud University, Riyadh, Saudi Araöia.
'Assrstarl Protessor, Department ot Prosthetic Dental Sciences, College otDentistry, King Saud University, Riyadh, Saudi Arabia.
^Leclurer, Department of Prosthetic Dental Sciences, College of Dentistry,King Saud University, Riyadh, Saudi Arabia.
'Regis lered Dental Technician and Instructor, Dental LaBoraloiyTechnicians'Training Program, College of Denlistry, King Saud University,Riyadh, Saudi Arabia.
Reprint requests: Dr Ridwaan Omar, Department ol Prosthetic DentalSciences, College ol Dentistry, King Sajd University, PO Box 60169,Riyadh 11545, Saudi Arabia, E-mail: romar,[email protected]
When a fixed partial denture {FPD) is subjected tofunctional loading, the transferred forces giverise to stress and, in turn, to strain within the struc-ture. Several factors can influence the resulting stressdistrihution and may include the magnitude and direc-tion of applied force, the design, dimensions, and ma-terial composition of the FPD, as well as variations inthe biomechanical response of the tooth-supportingtissue complex.̂ In determining the dimensions of anFPD, there is a prerequisite to maximize rigidity so asto avoid the introduction of such strain levels thatcould bring about permanent deformation, even undereonditions of maximum stress.̂ Furthermore, the FPDneeds to he able to withstand the repeated, yet accept-able, levels of strain caused by functional loading overprolonged periods of time. If such strains continuouslyexceed two thirds of the ultimate stress limit value ofthe material(s), there exists the likelihood of fractureoccurring due to fatigue.' On the basis of laboratorystudies performed under defined conditions, recom-mendations have been made for minimum connectordimensions,* as well as retainer coping thielmess,^ thatwould be consistent with successful long-term func-tion. It should be noted, however, that the conditions
820 Volume 35, Number 10, 2004
-
• Omar et al •
under which such recommendations may be valid arequite specific.
Technical failures of FPDs have been reported,^-'*and while they do not constitute the most commoncause of overall clinical failure, their occurrence may,to some extent, be due to certain mechanical and/orproduction shortcomings.''' Differences have beennoted in the prevalence of technical failures amongstudies carried out in varied settings and on variouslydesigned and sized FPDs.
The dimensions of connectors of metal-ceramicFPD metal frameworks under construction in a com-mercial dental laboratory setting have been shown tobe smaller than recommended minimal require-ments.'^ Retainer coping thickness was also found tobe generally less than optimal, and the overall indica-tion from a questionnaire survey conducted among agroup of experienced dental technicians working inthe same environment, was that they considered avail-able space to be the critical factor influencing their de-cisions about framework dimensions.'^ In view of tbeapparent risk tbat under-dimensioning of FPD frame-works poses to clinical outcome, it would be interest-ing to know whether FPDs prescribed, designed, andfabricated in a dental scbool environment are anycloser to recommended standards.
It was tbe purpose of tbis study to meastire the con-nector dimensions and retainer coping thicknesses ofthe frameworks of metal-ceramic FPDs under produc-tion in a dental scbool-based production dental labo-ratory. Additionally, tbe factors that technicians re-garded as influential in their decisions about thedimensions to provide for FPD frameworks were qual-itatively explored.
METHOD AND MATERIALS
All the metal-ceramic FPDs that were fabricated inthe production dental laboratory of the College ofDentistry, King Saud University, Riyadh, Saudi Arabia,during May and June 2002, were included in the study,subject to the following inclusion criteria: a minimumnumber of three connected units in the FPD; the stageof metal finishing prior to porcelain applicationshould have been reached; all retainers should havebeen planned for full porcelain occlusai coverage; andany planned soldering should not have been pail ofthe prescription.
Two features of the metal frameworks meeting thecriteria were examined: vertical and horizontal dimen-sions of connectors were measured using a modifieddigital sliding calliper (Ultra, Demurger Group), andthe metal thickness on the occlusai, buccal, and lingualaspects of retainer copings was measured using a dial
gauge calliper (Scbnelltaster). Each instrument had aresolution of 0.02 mm. A bevelled modification made tothe beaks of tbe sliding calliper ensured that tbey couldbe passively accommodated in tbe connector region.The accuracy of eacb instrument was tested in a pilotstudy and found to be acceptable, with both the slidingand dial callipers producing accuracies of ± 0.05 mm.Three examiners independently carried out all measure-ments after a period of training and calibration in theuse of the two measuring instruments, and the mean oftheir measurements was used in the subsequent resultsanalysis. Each examiner was blind to the identity of thedental technician. Inter- and intraexaminer differenceswere obtained from repeated measurements on 10FPDs. Mean differences of < 0.1 mm were consideredto be acceptable.
Connector sizes were determined with the frame-work in place on the working cast to ensure that mea-surements were being made with reference to thelikely direction of occlusai loading, as indicated by theopposing tooth inclinations.'' Measurements wererecorded to the nearest 0.1 mm. Retainer coping thick-ness was recorded at the point of least thickness for allaspects measured and, additionally, for buccal and lin-gual surfaces, 2 mm coronal to the cervical margin.Complex FPDs, such as those involving more than oneedentulous span, were treated as separate interabut-ment segments for the purpose of subsequent analyses.Connector dimensions were analyzed with respect totheir location in the arch, their relationships with thenumber of units in the PPD, and with tbe number ofpontics in tbe segment. Frequencies of coping thick-ness were also analyzed. All statistical analyses wereperformed using SPSS version 11 software (SPSS).
As a corollary to tbe study, a questionnaire was dis-tributed to all 14 dental tecbnicians working in tbefixed prosthodontics section in the same laboratory.Its purpose was to gain an insigbt into tbe factors tbatthey perceived to be important in the design of metalframeworks for FPDs. The questions explored the fac-tors that influence their decisions about framework di-mensions, their perception of the possible roles oflength of span and occlusion in influencing desired di-mensions, methods used to measure dimensions,methods used to compensate for perceived dimen-sional inadequacies, their experience of technical fail-ure, and their overall experience in the field.
RESULTS
The number of FPDs meeting the inclusion criteriawas 66, comprising 176 connectors, 124 retainers, and98 pontics, including some single cantilevers. Themean number of abutments per pontic was 1.3. All
Quintessence In ter nation a i 821
-
65-160-55'
.9 50-
1 "'S-ê 35-•E 3 0 -ë 25-S. 20-
15-10-5-OJ
62• Occlusai •B Buccal H• Linguai ^^ |
2621 • ?n
3 3 3
1 I R F '''1212 r^(H r
HM M B 1
••'•m •• 1 1 • _0.10-0.19 0.20-0.29 0.30-0.39 0.40-^^.4^ > 0.50
Coping thickness (mm)
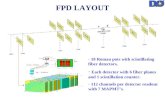
Fig 1 Percent distribution ot minimum tnicknessranges (mm) recorded on three walis of 124 retaineroopings.
frameworks were constructed of high nohle metal al-loys's and followed established protocol.
A majority of copings had a lingual thickness ex-ceeding 0.5 mm (61%), while fewer had a buccal (40%)or an occlusal (45%) thickness exceeding this dimen-sion (Fig 1). In all the sites measured, dimensions aslow as the 0.20-0.29-mm range were recorded.
The mean vertical dimension of connectors of max-illary anterior FPDs (3.0 mm) was greater than forposterior FPDs (2.7 mm) (Fig 2a). This was also tbecase for mandibular FPDs, witb anterior prostheseshaving a mean vertical connector dimension of 3.5mm and posterior ones of 2.9 mm (Fig 2b). Horizontalconnector dimensions had a reverse pattern in bothmaxillary and mandibular FPDs, sucb that maxillaryanterior and posterior FPDs had mean widtbs of 2.5mm and 3.6 mm, respectively, and mandibular ante-rior and posterior FPDs had mean widths of 2.0 mmand 3.6 mm, respectively (see Fig 2). No relationshipwas found between either the vertical or the horizon-tal connector dimension and the number of units inthe FPD (Fig 3). Similarly, there was no demonstrablerelationship between connector dimensions and thenumber of interabutment pontics, including can-tilevers, in FPD segments (Fig 4).
The questionnaire was completed by all those ap-proached, and although the 100% response rate is nu-merically excellent, there are drawbacks to its generalinterpretation due to the small sample size. On thequestion of the main determinant of connector size,respondents were equally split between those whosaid they generally used the available space and tbosewho followed the manufacturers' recommendations ortheir own experience. All tried, however, to maximizethe vertical height whenever possible. Half of tbem
used a measuring device for size determination, whiletbe rest used it sometimes or seldom. Most said theyincreased the size of connectors proportionately withthe FPD size and that they reduced connector sizewhen the FPD was to be opposed by a removableprostbesis. All technicians said they would speak tothe dentist if they believed the necessary dimensionscould not be acbieved. Levels of experience in fixedprostbodontics among tbe group fell into two cate-gories; about one half had 4 to 6 years' experience,and the other half 12 to 20 years. Technical failures re-lated to incorrect connector dimensions were rarelyencountered by the group, witb most individuals re-porting sucb an occurrence about once in 3 to 5 years.
DISCUSSION
Based on published experimental work, the minimumconnector dimensions permissible for FPD metalframeworks have been recommended as 4.1 mm inheight and 4.0 mm in width for a single molar repiace-ment, and 2.9 mm in height and 3.0 mm ¡n width for amaxillary anterior tooth replacement.* It should benoted that the figures quoted are drawn from tablesfor illustrative purposes only, and that a range of otherheight/width dimensional combinations, for examplea 4.7/3.0 mm height/width comhination for a molarreplacement, are also theoretically feasible. At tbesame time, it is well recognized that proportionatelylarger dimensions are needed for longer spans.''^
In comparison with these theoretic recommenda-tions, the mean posterior connector heights in this sam-ple were conspicuously lower at 2.7 mm and 2.9 mmfor maxillary and mandibular arches, respectively, al-
822 Voiume 35. Numbei 10, 2D04
-
• Omar et ai
Fig 2 Vertical and hofizontal dimensions of 176 con-neotors of metai fiameworks of fixed partiai denturesaooording to tootti sites (mm): (a) maxilla, (b)mandible. Tooth sites are based on ttie FDI tooth num-bering system
Fig 3 Conneotor dimensions (mm] witti reference tofixed partial denture lengtti (mm).
Fig 4 Conneotor dimensions (mm) with reterenoe tonumber ot interabutment or cantilever pontics (mni).
6.0
5.0
4.0
3.0
2.0
1.0
0.0
11 Verticai
1¿ • Horizontal
ÍMMÚtB/17, 17/16, 16/15, 15/14, 14/13, 13/12, 12/11, 11/2128/27 27/26 26/25 25/24 24/23 23/22 22/21n = 3 n=9 n ^ t 7 n = 19 n ^ 10 n = 7 n = 12 n = 7
Maxiliary sites
38/37, 37/36, 36/35, 35/34, 34/33, 33/32, 32/31, 31/4148/47 47/46 46/45 45/44 44/43 43/42 42/41n = 4 n = 21 n = 26 n = 12 n = 3 n = 2 n - 2 n = 1
Mandibular sites
^ 8.01 7.0^ 6.0.1 5.0i 4.0E 3.0c 2.01 1.0
0.0
2.8 ^ H
-J ^
n Vertical• Horizontal
^ \ ^Ê-n = 4 n = 5
No. of units
8.0i§ 7.0^ 6 . 0o 5.0.
.£ 3.0
Mea
n c
b b
0.0
2.8 ^ H1 ^^M
1 pontic
lu Vertical• Horizontai
'-' H 2.7 B^ [ ^ ,
2 pontics 3 ponticsNo. of pontics/cantilevers
2.9 ^ H
, , ^cantiieuer
Quintessence internationai 323
-
• Oinaí el di
though their widths of 3,6 mm were closer to the 4-mmrecomtncndation. Conversely, anterior connectors wereclose to the theoretic value in their mean heights, butlower in terms of width. This pattern of connector di-mensional proportions for posterior and anterior re-gions is at variance with normally directed occlusalforces, which require greater height to resist axially di-rected forces in the posterior region, and greater widthto resist horizontally directed forces in the anterior re-gion," The antagonistic goal of maximizing FPD rigidityin the presence of anatomic constraints poses a chal-lenge to the clinician and the technician, resulting in apossible compromise of recommended standards.'^
In this study, there was also a tendency for retainercoping thickness to be below recommended values. Athickness of less than 0.5 mm, as found in the majorityof coping walls examined except the lingual wall, sug-gests an inherent potential for strain to occur not onlyin function/' but during fabrication itself, eg, duringporcelain firing,̂ " In the latter instance, marginal fitmay be adversely affected, which could lead to fractureand dissolution of the luting cement, plaque retention,and secondary caries,^" as well as periodontal dis-ease, '̂ The potential for late failure of the porcelain-to-metal bond due to residual strain is also evident.-
There was close agreement between the dentalschool-based results of this study and those obtainedin a commercial dental laboratory setting.'' Such aconsensus does not support the idea that the possiblyhigh standards that may derive from an educationalenvironment could favor more optimal dimensioningthan would a commercial laboratory setting.Regarding the factors viewed by technicians as beingof importance in their determination of a connectordimension for a given situation, the qualitative find-ings in both the current group and the commerciallybased group'^ showed that, while technicians seemedto strive for recommended dimensions, available spacewas the overriding guiding factor.
Although technicians stated they increased dimen-sions in line with the total length of the FPD, as wellas with interabutment span, analysis of the resuHsfailed to show any such significant relationship (Figs 3and 4). A similarly insignificant association betweenFPD length and connector dimension was also thecase in the previously cited study,''^ Studies haveshown that FPDs of greater length and poorer abut-ment-pontic ratios have greater risks for mechanicalfailure,'̂ '̂ ^ The probably more favorable mean abut-ment-pontic ratio of 1,3 to 1 in the present samplecotild be seen as reducing such risks, and thus perhapsas justifying the dimensions appiied. It was notewor-thy that most of the current technicians were preparedto reduce dimensions if there was a perceived reduc-tion of occlusal load, such as if the FPD was to be op-
posed by a removable prosthesis. Research has, how-ever, refuted such an assumption, with the load distri-bution caused by a complete maxillary denture oppos-ing a distal cantilever FPD sbown to be even moreunfavorable than with natural maxillary teeth,^'
Given the apparent under-dimensioning of connec-tors and retainer thickness with reference to theoreticnorms noted in this study and elsewhere," a relativelymore frequent occurrence of mechanically related fail-ures in follow-up reports of FPDs in clinical servicemight be expected.*'""' One reason for this not beingthe case may be a degree of under-reporting on thebasis that only overt manifestations of technical failureare usually included in the category. However, giventhe nature of flexure of a beam in response to loading,it is evident that a number of indirect effects can comeabout, some of which may present as outcomes far re-moved from those of a typical design or dimensioningerror. It couid also be that early failures, most likelythe resuh of diagnostic or fabrication errors, may notbe systematically included in some of the long-termstudies, and that those FPDs that do survive the earlyperiod, have greater odds of longer-term survival."The reasons for insurance claims for early cotnplica-tions of FPDs confirm a high proportion of metalframework fractures, loss of retention, porcelain frac-tures, and tooth/root fractures, all of which may con-ceivably be due to framework under-dimensioning,'̂ '̂ *
On the other hand, the recommendations for mini-mum connector sizes are based upon experimentsusing gold-soldered joints,-' wbich are considered infe-rior in strength to cast connectors.^ Thus, it might wellbe that no realistic formula yet exists for a relationshipbetween the magnitude of loading forces, the frame-work dimensions, and the threshold values for perma-nent deformation of the various components of thefunctioning FPD system.̂ On this basis, it is clear thatmore needs to be ltnown about the appropriateness ofcurrent recommended norms with respect to FPDconnector dimensioning, which studies of a prospec-tive nature could best clarify.
REFERENCES
1, Lundgren D, Laurell L. BiorTiechanical aspects of fixedbridgework supported by natural teeth and endosseous im-plants. Periodontol 2000 t994;4;23-40.
2, Glantz P-0, Nyman S, Technical and biophysical aspects offixed partial dentures for patients with reduced periodontalsupport, J Prosthet Dent f982;47;47-51,
3, Hammerle C, Success and failure of fixed bridgework,Periodontol 2000 1994;4:'H-51.
4, Erhardson S, Carlsson J, Wictorin L, Fracture mechanics ofdental gold soldered joints [in Swedish], Swed Dent J1980;suppl 5:1-62.
824 Volume 35. Number 10, 2004
-
• Omar et al
5. Walton ]N, Gardner FM, Agar JR, A survey of crown andfixed partial denture failures: Length of service and reasonsfor replacement. ] Prosthet Dent 1986 ;56:416-421.
6. Randow K, Glantz P-0, Zöger B. Technical failures andsome related clinical complications in extensive fixedprosthodontics. Acta Odontol Scand 1986;44:241-255.
7. Karlsson S. Failures and length of service in fixed prostho-donlics after long-term function, A longitudinal clinicalstudy. Swed Dent ] 1989;13:1S5-192.
8. Foster LV. Failed conventional bridgework from generaldental practice; Clinical aspects and treatment needs of 142cases, Br Dent J 1990;168;199-201.
9. Palmqvist S, Swartz B. Artificial crowns and fixed partialdentures 18 to 23 years after placement. Int ] Prosthodont1993,6:279-285.
10. Glantz P-0, Nilner K, Jendresen MD, Sundberg H, Qualityof fixed prosthodontics after 15 years. Acta Odontol Scand1993:51:247-252.
11. Lindquist E, Karlsson S. Success rate and failures for fEiedpartial dentures after 20 years of service. Part I. Int JProsthodont 1998;11;133-13S-
12. Öwall B, Cronstrom R. First two-year complications of fixedpartial dentures, eight units or more. Swedish GuaranteeInsurance claims. Acta Odontol Scand 2000;58:72-76.
13. Glantz P-0, Nilner K, Jendresen MD, Sundberg H. Qualityof fixed prosthodontics after twenty-two years. ActaOdontol Scand 2002;60:213-21S.
14. Bergman B. Prognosis for prosthodontlc treatment of par-tially dentate patients. In: Owall B, Käyser AF, Carlsson GE¡eds]. Prosthodontics: Principles and Management Strate-gies. London: Mosby-Wolfe, 1996:149.
15. Johansson M, Mosharraf S, Karlsson S, Carlsson GE. Adental laboratory study of the dimensions of metal frame-works for fixed partial dentures. Eur J Prosthodont Restor-ative Dent 2000;8:75-78,
16, O'Brien WJ, Dental Materials and Their Selection, ed 2.Chicago: Quintessence, 1997:225-235.
17 Laurell L, Lundgren D, Falk H, Hugoson A. Long-termprognosis of extensive polyunit cantilevered fixed partialdentures. J Proslhet Dent 1991 ¡66:545-552.
18. Goldstein GR, Wesson A, Schweitzer K, Cutler B. Flexioncharacteristics of four-unit fixed partial denture frameworksusing holographic interferometry. J Prosthet Dent 1992;67:609-613,
19. Yamashita J, Shiozawa I, Takakuda K. A comparison of invivo and in vitro strain with posterior fixed partial dentures.J Prosthet Dent 1997;77:250-255.
20. Faucher RR, Nicholls JI. Distortion related to margin designin porcelain-fused-to-metal restorations. J Prosthet Dent1980;43:149-154.
21. Felton DA, Kenoy BE, Bayne SC, Wirthman GP. Effect of invivo crown margin discrepancies on periodontal health, JProsthet Dent 1991:65:357-364.
22. Leempoel PJB, Käyser AF, Van Rossum GMJM, De HaanAFJ. The survival rate of bridges. A study of 1674 bridges in40 Dutch general practices. J Oral Rehabii 1995;22:327-330,
23. Fallí H, Laurell L, Lundgren D. Occlusal force in dentitionswith mandibular implant-supported fixed cantilever pros-theses occluding with complete dentures. Int J MaxillofacImplants 1989:4:55-62.
24. Owall B, Cronstrom R, René N. Prosthodontic claims in theSwedish Patient Insurance Scheme. Acta Qdontol Scand1992:50:365-374,
Quintessence International825