Digestive Trac • Winter 2012, Issue 5
description
Transcript of Digestive Trac • Winter 2012, Issue 5

DigestiveTracINSIDE THIS ISSUE:
A Multidisciplinary Approach to Evaluation of Abnormal Liver Tests and Symptoms
A New Epidemic: Fatty Liver Disease
Surgical Treatment of Liver Metastasis Doubles Five-Year Survival
Specialized InterventionalRadiology Provides AdditionalTreatment Options for Liver Disease
The Role of Medical and RadiationOncology in Liver Cancerand Metastasis
Implanted Port ProvidesAdded Safety and Comfort
DIGESTIVE DISEASES • WINTER 2012Issue 5

Scott L. Baker, MD, FACS, FASCRS Steven Condron, MD, MHES, FACPColorectal Surgery Gastroenterology and HepatologySurgical Institute of South Dakota Avera Medical Group GastroenterologySurgical Director of Avera Digestive Disease Institute Medical Director of Avera Digestive Disease Institute
Dear Colleagues,
Collaboration across a wide range of medical specialties often presents the best possibility for the most appropriate treatment plan and best outcomes. In the case of liver disease, the specialists of the Avera Digestive Disease Institute work in partnership with gastroenterologists, hepatologists, surgeons, interventional radiologists, medical and radiation oncologists as well as other specialties.
As is the case with many other diseases and conditions, outcomes are best when liver disease is caught and treated early. Liver disease is often silent as in the case of fatty liver disease. Significant damage can occur before intervention can take place. Partnership with primary care providers is important in screening patients who are at risk.
This issue of Digestive Trac is dedicated to liver disease.
Nonalcoholic fatty liver disease is extremely common – in fact, one-fourth of the population is estimated to have accumulated fat in the liver, and 3 percent have a more severe form known as NASH, nonalcoholic steatohepatitis, which can lead to significant inflammation and scarring, and ultimately liver failure, liver cancer, the need for liver transplant, or death. People with metabolic syndrome are most at risk, and liver enzyme screening is advised. Alcoholic and nonalcoholic fatty liver disease areamong the top reasons why patients present with abnormal liver enzyme tests; other possible reasons include biliary stones, obstructions or scarring, or malignant tumors in the biliary system. A multidisciplinary approach is helpful toward accurate diagnosis and the best treatment plan.
We at the Digestive Disease Institute are especially concerned for the continued monitoring of patients who have experienced colorectal cancer. Approximately 15 to 20 percent of patients who have had colorectal cancer will have some form of distant spread of their disease, and the liver is the most common site of distant spread. When metastatis is caught early, surgical management can be effective for a cure or prolonged survival. Other options include specialized interventional radiology procedures including radiofrequency ablation (RFA) and yttrium 90 radioembolization. Medical and radiation oncologists also play an important role in the treatment of liver malignancies.
We invite you to read about these specific aspects of our approach to the management of liver disease in this issue. It is our continuing goal, as well as our privilege, to work closely with primary care physicians for our patients’ best interest and continuity of care. Please feel free to contact us at (605) 322-7797 with questions or for more information.
Sincerely,
1

Avera Makes the Grade!Avera McKennan Hospital & University Health Center Achieves
Top Rankings in Gastrointestinal and General Surgical Care
Healthgrades has ranked Avera McKennan the No. 1 Hospital in South Dakota
for GI Services and GI Medical Treatment in 2013.
Healthgrades Awards for GI care:
n Top 5% in the Nation for Overall GI Services
n Top 5% in the Nation for GI Medical Treatment
n Top 5% in the Nation for General Surgery
n Ranked No. 1 in S.D. for General Surgery
n Ranked No. 1 in S.D. for GI Services and GI Medical Treatment n Five-Star Recipient for GI Procedures and Surgeries, Treatment of GI Bleed,
and Treatment of Bowel Obstruction
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g 2

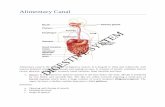
A Multidisciplinary Approach to Evaluation of Abnormal Liver Tests and Symptoms
When patients are referred with abnormal liver test results, a multidisciplinary team including gastroen-terologists, hepatologists and other sub-specialists at Avera collaborate to confirm a diagnosis and recommend a treatment plan for the best possible outcomes. There are a variety of reasons why a patient may have abnormal biochemical liver tests, specifically high levels of the enzymes AST (aspartate aminotransferase) and ALT (alanine aminotransferase) in the blood. The reason may be a primary hepatocellular process or a condition involving the pancreaticobiliary biliary system. The top reason for abnormally high transaminases is fatty liver disease – either alcoholic or nonalcoholic. The more serious form of nonalcoholic fatty liver disease (NAFLD), NASH (nonalcoholic steatohepatitis), is associated with metabolic syndrome, which also involves diabetes mellitus/insulin resistance, high blood pressure, high cholesterol and obesity. This disease has approached epidemic levels and careful attention should be directed toward diagnosis and treatment. A second reason for transaminitis is hepatitis C, common in the Baby Boomer generation. It spread predominantly before widespread testing of the blood supply began in the 1990s, and through IV drug use. Because it is a “silent disease,” patients can suffer liver damage and not know they are infected. For this reason, the Centers for Disease Control and Prevention now recommends that everyone born between 1945 and 1965 have a one-time blood test for hepatitis C. Fatty liver disease can be confirmed through imaging – ultrasound, CT or MRI – or liver biopsy, and hepatitis C can be confirmed through the hepatitis C antibody test.
Abnormal biochemical liver tests may also indicate an issue in the biliary system, including biliary stones, primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC), or a malignancy. Biliary stones, or choledocholithiasis, is the presence of one or more gallstones in the common bile duct that have migrated from the gallbladder. Primary biliary cirrhosis, thought to be an autoimmune disease, is a disease process in which the bile ducts in the liver become damaged and destroyed. Primary sclerosing cholangitis involves the inflammation, hardening and scarring of the bile ducts. A malignant blockage that has metastasized to the liver, originated in the biliary system, or occurred as a result of pancreatic cancer can also block this system, presenting itself in elevated liver enzymes.
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g3
“Multidisciplinary collaboration
between gastroenterologists and
hepatologists, as well as surgeons,
oncologists, interventional
radiologists and others allow
for the best possible diagnosis,
treatment and outcomes when
patients present with elevated
liver enzymes and other symptoms
of possible liver disease,” Dr.
Condron said.

However, multidisciplinary collaboration may come into play in the diagnosis and treatment of biliary disorders. Endoscopic retrograde cholangiopancreatography (ERCP) and direct fiberoptic cholangioscopy are among endoscopic procedures performed by gastroenterologists with Avera Medical Group Gastroenterology. ERCP may be indicated if patients present with elevated liver enzymes, jaundice, and right upper quadrant abdominal pain. The procedure can be both diagnostic and therapeutic. During ERCP, bile ducts can be examined with cholangioscopy, the use of a fiber optic endoscope for direct visualization of the biliary tree. In ERCP, physicians can visually diagnose a biliary condition, obtain tissue for biopsy, remove stones, identify and potentially treat obstructions (place a stent to restore biliary luminal patency). Through the Avera Digestive Disease Institute, ERCP is performed by Drs. Condron and Christopher Hurley with Avera Medical Group Gastroenterology.
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g 4
Dr. Steven Condron, Avera Medical Group Gastroenterology
Variceal bleeding can occur in patients with portal hypertension, most commonly caused by cirrhosis. In portal hypertension, when blood does not filter well through the portal vein, pressure builds and the body tries to find collateral pathways. This can lead to varices in the stomach and distal esophagus which can rupture and cause severe bleeding. These varices can be treated medically with beta blockers, or through an endoscopic intervention using variceal banding ligation. This procedure, performed by all gastroenterologists with Avera Medical Group Gastroenterology, uses endoscopy to place an elastic ring or band around an enlarged vein, cutting off blood flow through that vein. “Multidisciplinary collaboration between gastroenterologists and hepatologists, as well as surgeons, oncologists, interventional radiologists and others allow for the best possible diagnosis, treatment and outcomes when patients present with elevated liver enzymes and other symptoms of possible liver disease,” Dr. Condron said.

w w w . A v e r a D i g e s t i v e D i s e a s e . o r g
A New Epidemic: Fatty Liver Disease
Screening of special population groups can help prevent serious complications of common liver diseases, including nonalcoholic fatty liver disease (NAFLD).
Nonalcoholic fatty liver disease (NAFLD)Fatty liver disease is often equated with excessive alcohol intake, yet certain nonalcoholic patients are also at risk, especially if they suffer from “metabolic syndrome,” in that they deal with high blood sugar (diabetes mellitus) / insulin resistance, high cholesterol, obesity, and/or high blood pressure.
“If a patient is diabetic, with high blood cholesterol, high blood pressure and/or obesity, that patient is at risk to have nonalcoholic fatty liver disease,” said Dr. Hesham Elgouhari, hepatologist with Avera Medical Group Liver Disease Sioux Falls. Those at risk should be evaluated for NAFLD.
Nonalcoholic fatty liver disease is a liver disease in which fat accumulates in the liver. Because fatty liver disease also occurs as the result of alcohol use, NAFLD is distinguished by not being caused by excessive alcohol intake. “It is most often completely asymptomatic,” Dr. Elgouhari said. If people do have symptoms, they generally include malaise, fatigue, and upper abdominal discomfort. The disease is most often discovered if a liver enzymes test is high, or the liver appears enlarged and/or with fatty infiltration on ultrasound or other imaging tests.
Nonalcoholic fatty liver disease ranges from simple fatty liver (steatosis) to nonalcoholic steatohepatitis (NASH). In its more serious form of NASH, fatty liver disease can lead to significant inflammation and scarring, and ultimately liver cirrhosis, liver failure, l iver cancer and the need for l iver transplant or death.
5
“If fatty liver disease is diagnosed, the usual first step is to help a patient control the elements of metabolic syndrome – blood pressure, glucose, cholesterol – and most importantly lose weight,” Dr. Elgouhari said. “We do have medications, but medical science has yet to produce a medicine that everyone with NASH should be taking.”

w w w . A v e r a D i g e s t i v e D i s e a s e . o r g 6
“It is now the most common cause of chronic liver disease,” Dr. Elgouhari said. It’s estimated that approximately 3 percent of the population have NASH, or 10 million-plus people. NAFLD in some form is estimated to be present in about one-fourth of the general population. Most people with simple fatty liver disease do not develop serious complications, but because they are at risk, careful monitoring is important.
“If fatty liver disease is diagnosed, the usual first step is to help a patient control the elements of metabolic syndrome – blood pressure, glucose, cholesterol – and most importantly lose weight,” Dr. Elgouhari said. “We do have medications, but medical science has yet to produce a medicine that everyone with NASH should be taking.”
“The important thing to remember about this disease is that is very common in the general population. What we need to do is monitor and evaluate our patients to ensure they do not develop ser ious compl icat ions,” Dr. Elgouhar i said. “ I t ’s important for patients who are at risk to understand that in addition to the other health problems of metabolic syndrome like heart disease, their liver could be sick, too,” he added.
Dr. Hesham Elgouhari, hepatologist with Avera Medical Group Liver Disease Sioux Falls

Surgical Treatment of Liver Metastasis Doubles Five-Year Survival
Under the care of a specialized surgical team, patients with liver disease receive a high level of care, right here in Sioux Falls. This includes those patients with primary colorectal cancer that has metastasized to the liver.
“Colorectal cancer metastasizes to distant sites, includ-ing the liver, in approximately 15-20 percent of cases,” said Dr. Michael Person, surgeon with Surgical Institute of South Dakota. The liver is the most common site of distant spread, but colorectal cancer can also spread to sites such as the lungs. “With effective chemotherapy and surgery, the five-year survival can double,” stated Dr.
Tariq Khan, surgeon with Avera Transplant Institute. Intervention at the earliest point possible is critical.
“Metastatic cancer in the liver, secondary to colon cancer, is often viewed as terminal for which nothing can be done. Yet with specialized treatment and surgical intervention, we can give people added years and quality of life,” Dr. Khan said.
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g7
Dr. Michael Person, surgeon with Surgical Institute of South Dakota

After colorectal cancer is removed surgically and any recommended chemotherapy and radiation have taken place, it’s important for cancer patients to have continued surveillance for five years. “If cancer metastasizes, 90 percent of the time it happens during the first three years,” Dr. Person said. “After five years, the risk of return is low.”
Follow-up testing includes blood tests, X-rays, imaging scans and colonoscopies. If metastatic lesions on the liver are caught early, surgery is a good treatment option. Once too large a portion of the liver is involved or the disease is diffuse, surgery is not considered.
“The majority of liver metastases are found too late, and so it’s important for patients and primary care physicians to understand that if it does spread and we find it early, treatment can be effective for a cure or increased survival. The danger is when patients fall out of the post-cancer screening. Once symptoms appear, it is often too late,” Dr. Person said. “We want to manage this disease as a chronic illness – not as an acute illness that is life-threatening to the patient.”
In some cases, the liver metastases are identified at the time of surgery. In these cases, if resection is possible, surgery can take place at the same time. Or, the colon may be resected first, followed by the liver a few weeks later. “We decide this on a case-by-case basis,” Dr. Person said.
“Clearly the first choice for cure and greatest survival is surgical resection,” Dr. Person said. “Yet our goal is to remove all disease, and if this is not possible, we’re better off not to approach treatment surgically.” If the tumors are small and on the periphery of the liver, surgery can be performed minimally invasively through laparoscopy. Yet this decision is overshadowed by the top priority of removing all the cancer.
For cases not amenable to surgery, other options include chemotherapy, radiation, and specialized interventional radiology techniques.
The Digestive Disease Institute follows the National Comprehensive Cancer Network (NCCN) guidelines, which are the widely recognized standard for clinical policy in oncology. “In addition, as a tertiary care center, Avera McKennan has the depth of expertise and experience among our medical professionals to care for these difficult cases,” Dr. Person said.
Patients benefit greatly from the multidisciplinary digestive disease conference. “Anyone with metastatic disease has his or her case evaluated at this multidisciplinary conference. It is not just one person recommending treatment, it is the best possible option as determined by an entire team of experts.”
“The majority of liver metastases
are found too late, and so it’s
important for patients and
primary care physicians to
understand that if it does spread
and we find it early, treatment can
be effective for a cure or increased
survival. The danger is when
patients fall out of the post-cancer
screening. Once symptoms appear,
it is often too late,” Dr. Person
said. “We want to manage this
disease as a chronic illness – not
as an acute illness that is life-
threatening to the patient.”
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g 8

w w w . A v e r a D i g e s t i v e D i s e a s e . o r g9
Specialized Interventional Radiology Provide Additional Treatment Options for Liver Disease
When liver disease cannot be successfully treated surgically, interventional radiology offers the latest techniques that can improve survivorship or provide curative treatment.
Interventional radiology involves image-guided, minimally-invasive techniques to treat a wide range of conditions. “For both malignant and non-malignant liver disease, there are various techniques which may be applicable for an individual patient’s plan of care,” said Dr. Matthew Casey, interventional radiologist with Avera Medical Group Radiology Sioux Falls.
In the case of metastatic colon cancer, a multi-disciplinary team meets to discuss options for the patient. Three key IR treatments for malignant liver tumors are transarterial chemoembolization (TACE), radiofrequency ablation (RFA) and yttrium 90 radioembolization.
“Unlike other organs, the liver has a dual blood supply,” including the portal vein coming from the intestines carrying absorbed nutrients, and the hepatic artery. The hepatic artery supplies about one-third of blood to the liver, yet it is the primary blood supply for most tumors. Blocking blood supply through the hepatic artery often succeeds in cutting off the tumor’s blood supply, and the liver can continue to function with supply from the portal vein.
RFA can be curative, in fact, in appropriately selected patients with appropriate-sized tumors, RFA has been shown to be as effective as surgical removal. If the tumor
“Interventional radiology procedures can provide additional options to patients when surgery is not an option for addressing serious liver disease,” Dr. Casey said. “Our multidisciplinary team makes these recommendations on an individualized basis for the best possible outcome for each patient.”

is located near another organ or large blood vessels, RFA is not an option. Also, the tumor must be 5 cm or less in size. “We’re generally using RFA on inoperable tumors as an alternative to surgery. If the tumor can be surgically removed, that’s the gold standard. However, if we can do it, RFA has shown to be effective,” Dr. Casey said. RFA is performed in a CT scanner room or an angio suite. It has also been used during surgery.
In yttrium 90 radioembolization, interventional radiologists use fluoroscopy, or less commonly CT, to guide catheters through the blood vessels to the liver, and deliver radioac-tive microspheres directly to the tumor. This procedure is usually used for secondary liver malignancies, because metastatic tumors are not as hypervascular as hepatocel-lular carcinoma. It is better tolerated by patients, and is usually an outpatient procedure.
Avera McKennan is the only hospital in South Dakota offering this procedure. “It is regulated by the Nuclear Regulatory Commission, which has very stringent standards,” Dr. Casey said. Radioembolization is not curative, but it improves survival with minor and short-term side effects.
“Interventional radiology procedures can provide additional options to patients when surgery is not an option for addressing serious liver disease,” Dr. Casey said. “Our multidisciplinary team makes these recommendations on an individualized basis for the best possible outcome for each patient.”
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g 10
Dodd, Soulen, Kane, Livraghi, Lees, et al. 2000
Demonstrates use of radio frequency probe

The Role of Medical and RadiationOncology in Liver Cancer and Metastasis
Based upon the type and stage of cancer lesions in the liver, medical, surgical and radiation oncology therapies may contribute to curative treatment, as well as prolonged survival and palliative care.
With liver metastatic disease, the histology of the cancer in the liver dictates the type of treatment applied.
If there is a single lesion or two, a surgeon will try to remove the cancer surgically, as there are cases in which an isolated metastatic lesion can be removed and render the patient cancer-free.
If there are multiple lesions not amenable to surgery, the strategy is usually to go directly to chemotherapy. Surgery is most often considered if the limited metastatic lesions in the liver have spread from primary colorectal cancer. “We have more information on the effectiveness of surgery for colorectal liver metastasis than cancer that has spread from other primary sites, although the role of surgery in these cases is still being established,” said Dr. Addison Tolentino, medical oncologist with Avera Medical Group Oncology & Hematology.
Neoadjuvant chemotherapy may be recommended to help shrink tumors before surgery, and protect patients from an early spread of malignancy. Once colorectal
cancer has metastasized to the liver, it is often a systemic disease, with the possibility of cancer cells floating around in the system. Neoadjuvant chemotherapy provides the patient with systemic protection before a potentially curative surgical procedure. “We use a short course so as to not completely make the metastatic lesion disappear the the point it cannot be removed surgically,” Dr. Tolentino said, as surgical removal provides the best chance for highest outcomes.
Chemotherapy may also be used post-surgery as adjuvant therapy to reduce the risk of recurrence, or as conversion therapy to convert non-resectable tumors into resectable lesions.
Common chemotherapy regimens for colorectal cancer metastasis to the liver include FOLFOX (5-fluorouracil, Leucovorin and Oxaliplatin) with or without Bevacizumab and FOLFIRI (5FU, Leucovorin and Irinotecan) with or without Aflibercept. Panitumumab or Cetuximab are used for KRAS mutation positive colon cancer, and Regorafenib oral therapy in the case of failure of the above therapy. Common side effects of FOLFOX therapy include fatigue, nausea and diarrhea, loss of appetite, risk of infection/low white blood cell count, mouth sores, laryngeal spasm, difficulty swallowing or breathing, and hand-foot syndrome.
“In addition to medical oncology, radiation therapy has selected applications with malignant lesions on the liver,” said Dr. Barbara Schlager, radiation oncologist with Avera Medical Group Radiation Oncology.
Most commonly, radiation therapy is used to treat liver metastasis. An isolated or small group of metastases can be treated with a specialized radiation therapy known as SBRT, or Stereotactic Body Radiation Therapy. SBRT couples very accurate and precise targeting technology with a high dose of radiation. This targets radiation directly to the tumor to kill cancer cells, while minimizing radiation exposure to nearby normal tissue. Treatment can be completed in one to five fractions, with excellent outcomes and low risk of side effects.
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g11
Dr. Addison Tolentino, medical oncologist withAvera Medical Group Oncology& Hematology

The treatment process is very similar for patients to other forms of radiation therapy, except that they have to hold a position longer, and various restraints are available to help a patient stay in position. They may experience some nausea, depending on how close the target is to the stomach.
“This therapy is strong enough to eradicate a solitary tumor, but because other cancer cells are often lurking in the liver or other parts of the body, it generally is not curative,” Dr. Schlager said.
What SBRT and other advanced therapies have accomplished is improved survival for cancer patients who experience metastasis to the liver. In the past, if a patient had metastasis to the liver, they did not have prolonged survival. Studies have shown up to 92 percent two-year local control for liver metastases.
Through improved surgical techniques, chemotherapy and radiation therapy, patients with primary colorectal cancer that has metastasized to the liver are living longer. If the primary site is under control, it makes sense to treat metastasis if there are not multiple sites.
Additionally, a palliative application of radiation therapy is a low dose of external radiation to relieve pain in the case of a large number of lesions in the liver.
Most often, patients with primary liver cancer also have cirrhosis, or tumors are distributed throughout the liver. Because the liver is more sensitive to radiation, it’s possible to treat one portion with high doses of radiation, but not the whole liver. If patients have small hepatocellular lesions and do not want to undergo surgery, other treatments are available including radiation.
“Every patient case is evaluated individually in order to deliver the highest benefit to patients, without taking valuable time or adding risk for those patients that will not benefit,” Dr. Schlager said.
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g 12
Implanted Port ProvidesAdded Safety and Comfort
Cancer patients at the Avera Cancer Institute are often offered an implanted port, or Portacath, which is a reservoir which is implanted under the skin of the chest. A catheter comes off the port and goes into a main blood vessel either under the collar bone or in the neck.
“Chemotherapy patients need frequent IV access for both infusions and blood draws. Due to the effect of treatment on the veins, it can be difficult for staff to find a vein, causing discomfort to patients. Patients say they experience less pain and discomfort with the Portacath,” said Dr. Scott Baker, surgeon with Surgical Institute of South Dakota.
A Portacath functions similarly to a central line, except that it is all under the skin, reducing the risk of infection. “Landmarks” make it easy for the staff to find without multiple pokes. The self-sealing rubber of the reservoir can be punctured up to 1,000 times, so it can be in place for several years.
“A previous downfall to the portacath was the inability to accommodate IV contrast injections, but a new variation of implanted ports known as PowerPort provides this capability,” Dr. Baker said.
The port is implanted in a surgical suite under sedation and local anesthetic, with the aid of imaging guidance through ultrasound and X-ray. It is a same-day outpatient procedure, and can be used for IV access the same day.
PowerLoc® Safety Infusion Set
Palpation Points
PowerPort® Implantable Port
Catheter Skin
© Copyright 2007 C. R. Bard, Inc. All rights reserved. * Bard, PowerPort, PowerLoc, “Feel the New Standard of Care” and the color purple are trademarks and/or registered trademarks of C. R. Bard, Inc. or an affiliate.

Colorectal Surgery:Scott L. Baker, MD, FACS, FASCRS
Gastroenterology andHepatology:Steven Condron, MD, MHES, FACPCristina Hill Jensen, MDChristopher Hurley, MDLarry W. Schafer, MD, FACPDany Shamoun, MD
General Surgery:Scott L. Baker, MD, FACS, FASCRSMichael Bauer, MD, FACSWade E. Dosch, MD, FACSDavid Flanagan, MDThomas E. Fullerton, MDMichael Person, MD, FACSDavid A. Strand, MD, FACSBradley C. Thaemert, MD, FACSDonald J. Wingert, MD, FACS
Genetics: Nicole Mattila, CGC, MS
Hepatology:Hesham Elgouhari, MD, FACPMumtaz Niazi, MD
Multidisciplinary Team Includes the Following Areas of Specialty:
Medical Oncology:David Elson, MDMark R. Huber, MDMichael McHale, MDHeidi McKean, MDAddison R. Tolentino, MD
Pathology: Steven P. Olson, MD Bruce R. Prouse, MDRaed A. Sulaiman, MD
Radiation Oncology: Barbara Schlager, MDKathleen L. Schneekloth, MDJames Simon, MD
Radiology:Sabina Choudhry, MDBrad A. Paulson, MD
Research (Cancer clinical trials)
Transplant Surgery:Christopher Auvenshine, DOTariq N. Khan, MD
Urogynecology: Matthew A. Barker, MD, FACOG
w w w . A v e r a D i g e s t i v e D i s e a s e . o r g
If you have any questions or would like to make a referral to theAvera Digestive Disease Institute, call 605-322-7797.
13

To learn more, visit our website atwww.AveraDigestiveDisease.org
Go Online to Learn More!
14

Hours: 8 a.m. - 5 p.m. • 605-322-7797
To learn more, visit our website atwww.AveraDigestiveDisease.org
1325 S. Cliff AvenueSioux Falls, SD 57105
ADDI-26704-REVDE0512