Damage Control Resuscitation Gregory W. Jones M.D. CDR MC USN Naval Hospital Camp Pendleton.
-
Upload
amelia-park -
Category
Documents
-
view
226 -
download
2
Transcript of Damage Control Resuscitation Gregory W. Jones M.D. CDR MC USN Naval Hospital Camp Pendleton.

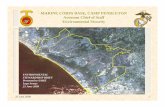
Damage Control Damage Control ResuscitationResuscitation
Gregory W. Jones M.D.Gregory W. Jones M.D.
CDR MC USNCDR MC USN
Naval Hospital Camp PendletonNaval Hospital Camp Pendleton

“Damage Control Resuscitation represents the most important advance in trauma care for hospitalized civilian and military casualties from this war.”
Cordts, Brosch and Holcomb, J Trauma, 2008

AcknowledgmentAcknowledgment
Thanks toThanks to
COL Jay Johannigman, MC, USAF, for his COL Jay Johannigman, MC, USAF, for his significant contributions to this significant contributions to this presentation.presentation.

Case DataCase Data
25 year old SGT involved in IED blast25 year old SGT involved in IED blast
Tourniquet applied at scene one hour agoTourniquet applied at scene one hour ago
Systolic BP 90Systolic BP 90
Mental Status: Awake, confusedMental Status: Awake, confused
Blood oozing from superficial woundsBlood oozing from superficial wounds
Temp 96 FTemp 96 F

Patient AssessmentPatient Assessment
Sick or Not SickSick or Not Sick
What are reliable criteria for initial What are reliable criteria for initial assessment? assessment?
Which criteria can predict outcomes and Which criteria can predict outcomes and direct therapy?direct therapy?

New Diagnostic criteriaNew Diagnostic criteriaAvoids the “but he looked good” Avoids the “but he looked good”
phenomenonphenomenon
New Diagnostic criteriaNew Diagnostic criteriaAvoids the “but he looked good” Avoids the “but he looked good”
phenomenonphenomenon
Within the first five minutes in the EDWithin the first five minutes in the ED
– Identify patients in troubleIdentify patients in trouble
– Identify patients with increased mortalityIdentify patients with increased mortality
– Identify patients with increased probability of massive transfusionIdentify patients with increased probability of massive transfusion

The Lethal TriadThe Lethal TriadThe Lethal TriadThe Lethal Triad
AcidosisAcidosis HypothermiaHypothermia
CoagulopathyCoagulopathy
Death
Brohi, K, et al. J Trauma, 2003.

Damage Control ResuscitationDamage Control Resuscitation
Acidosis- Base Deficit > - 6Acidosis- Base Deficit > - 6
Coagulopathy – INR > 1.5Coagulopathy – INR > 1.5
Hypotension – Systolic B/P < 90Hypotension – Systolic B/P < 90
Hemoglobin - < 11Hemoglobin - < 11
Temperature - < 96. 5Temperature - < 96. 5
Pattern recognitionPattern recognitionWeak or absent radial pulse Weak or absent radial pulse Abnormal mental statusAbnormal mental statusSevere Traumatic InjurySevere Traumatic Injury

ChallengesChallenges
Requires robust Medical settingRequires robust Medical setting
Need system approach to deliver Need system approach to deliver casualties to most capable facilitiescasualties to most capable facilities
Isolated and far forward facilities can still Isolated and far forward facilities can still benefit from these principlesbenefit from these principles

AcidosisAcidosisAcidosisAcidosisBase deficit (BD) ≥ 6 identifies patients that Base deficit (BD) ≥ 6 identifies patients that
– require early transfusion,require early transfusion,– increased ICU days and increased ICU days and – risk for ARDS and MOFrisk for ARDS and MOF
BD of ≥ 6 is strongly associated with the need for BD of ≥ 6 is strongly associated with the need for MT and mortality in both civilian and military MT and mortality in both civilian and military trauma. trauma. Patients have an elevated BD Patients have an elevated BD beforebefore their blood their blood pressure drops to classic “hypotension” levels.pressure drops to classic “hypotension” levels.Acidosis contributes more to coagulopathy more Acidosis contributes more to coagulopathy more than hypothermia (not reversible)than hypothermia (not reversible)
Base deficit (BD) ≥ 6 identifies patients that Base deficit (BD) ≥ 6 identifies patients that – require early transfusion,require early transfusion,– increased ICU days and increased ICU days and – risk for ARDS and MOFrisk for ARDS and MOF
BD of ≥ 6 is strongly associated with the need for BD of ≥ 6 is strongly associated with the need for MT and mortality in both civilian and military MT and mortality in both civilian and military trauma. trauma. Patients have an elevated BD Patients have an elevated BD beforebefore their blood their blood pressure drops to classic “hypotension” levels.pressure drops to classic “hypotension” levels.Acidosis contributes more to coagulopathy more Acidosis contributes more to coagulopathy more than hypothermia (not reversible)than hypothermia (not reversible)

CoagulopathyCoagulopathy on Presentationon PresentationCoagulopathyCoagulopathy on Presentationon Presentation
An initial INR ≥ 1.5 reliably predicts those An initial INR ≥ 1.5 reliably predicts those military casualties who will require MT.military casualties who will require MT.
Pts who have a significant injury present with a Pts who have a significant injury present with a coagulopathy. coagulopathy.
Severity of injury and mortality is linearly Severity of injury and mortality is linearly associated with the degree of the initial associated with the degree of the initial coagulopathy. coagulopathy.
An initial INR ≥ 1.5 reliably predicts those An initial INR ≥ 1.5 reliably predicts those military casualties who will require MT.military casualties who will require MT.
Pts who have a significant injury present with a Pts who have a significant injury present with a coagulopathy. coagulopathy.
Severity of injury and mortality is linearly Severity of injury and mortality is linearly associated with the degree of the initial associated with the degree of the initial coagulopathy. coagulopathy.

CoagulopathyCoagulopathy and and TraumaTrauma
CoagulopathyCoagulopathy and and TraumaTrauma
Derangements in Derangements in coagulation occur rapidly coagulation occur rapidly after trauma after trauma
By the time of arrival at By the time of arrival at the ED, 28% (2,994 of the ED, 28% (2,994 of 10,790) of trauma 10,790) of trauma patients had a detectable patients had a detectable coagulopathy that was coagulopathy that was associated with poor associated with poor outcomeoutcome
Brohi Graph Here
(Brohi et al., 2003)

HypotensionHypotension HypotensionHypotension
A systolic blood pressure of 90 mm Hg or less is A systolic blood pressure of 90 mm Hg or less is indicative casualties that have lost over 40% of indicative casualties that have lost over 40% of their blood volumetheir blood volume
– ((~~2000 ml in an adult)2000 ml in an adult)
– They have impending cardiovascular collapse They have impending cardiovascular collapse and have significantly increased mortality.and have significantly increased mortality.
A systolic blood pressure of 90 mm Hg or less is A systolic blood pressure of 90 mm Hg or less is indicative casualties that have lost over 40% of indicative casualties that have lost over 40% of their blood volumetheir blood volume
– ((~~2000 ml in an adult)2000 ml in an adult)
– They have impending cardiovascular collapse They have impending cardiovascular collapse and have significantly increased mortality.and have significantly increased mortality.

HemoglobinHemoglobinHemoglobinHemoglobin
Otherwise young healthy soldiers with a Hgb of Otherwise young healthy soldiers with a Hgb of < 11 have only one reason for their anemia, < 11 have only one reason for their anemia, namely acute blood loss.namely acute blood loss.
Otherwise young healthy soldiers with a Hgb of Otherwise young healthy soldiers with a Hgb of < 11 have only one reason for their anemia, < 11 have only one reason for their anemia, namely acute blood loss.namely acute blood loss.

TemperatureTemperatureTemperatureTemperature
A temperature < 96°F or 35°C is A temperature < 96°F or 35°C is associated with an increase in mortality.associated with an increase in mortality.
Trauma patients that are hypothermic Trauma patients that are hypothermic are not perfusing their tissueare not perfusing their tissue
The coagulation cascade is an enzymatic The coagulation cascade is an enzymatic pathway that degrades with temperature pathway that degrades with temperature and ceases at 92 Fand ceases at 92 F
A temperature < 96°F or 35°C is A temperature < 96°F or 35°C is associated with an increase in mortality.associated with an increase in mortality.
Trauma patients that are hypothermic Trauma patients that are hypothermic are not perfusing their tissueare not perfusing their tissue
The coagulation cascade is an enzymatic The coagulation cascade is an enzymatic pathway that degrades with temperature pathway that degrades with temperature and ceases at 92 Fand ceases at 92 F

Diagnosis doneDiagnosis doneDiagnosis doneDiagnosis done
Diagnosis DoneDiagnosis Done– How to resuscitate these How to resuscitate these
casualties?casualties?
Diagnosis DoneDiagnosis Done– How to resuscitate these How to resuscitate these
casualties?casualties?
Damage Control ResuscitationDamage Control Resuscitation1.1. Hypotensive resuscitationHypotensive resuscitation
2.2. Hemostatic resuscitationHemostatic resuscitation

Hypotensive ResuscitationHypotensive Resuscitation
Time Honored technique developed by Military Time Honored technique developed by Military physicians during WWI and WWIIphysicians during WWI and WWII
Maximizing the resuscitation benefit to the Maximizing the resuscitation benefit to the mitochondria while minimizing rebleeding by mitochondria while minimizing rebleeding by avoiding “popping the clot”avoiding “popping the clot”
Supported by a significant body of scientific data. Supported by a significant body of scientific data. This approach preserves the resuscitation fluid This approach preserves the resuscitation fluid within the vascular systemwithin the vascular system
Logistically sound by preventing needless waste Logistically sound by preventing needless waste of blood and fluids. of blood and fluids.
Time Honored technique developed by Military Time Honored technique developed by Military physicians during WWI and WWIIphysicians during WWI and WWII
Maximizing the resuscitation benefit to the Maximizing the resuscitation benefit to the mitochondria while minimizing rebleeding by mitochondria while minimizing rebleeding by avoiding “popping the clot”avoiding “popping the clot”
Supported by a significant body of scientific data. Supported by a significant body of scientific data. This approach preserves the resuscitation fluid This approach preserves the resuscitation fluid within the vascular systemwithin the vascular system
Logistically sound by preventing needless waste Logistically sound by preventing needless waste of blood and fluids. of blood and fluids.

Hemostatic ResuscitationHemostatic Resuscitation
Damage control philosophy can be extended to Damage control philosophy can be extended to hemostatic resuscitationhemostatic resuscitation
restoring restoring normal coagulationnormal coagulation
minimizing crystalloidminimizing crystalloid
Traditional resuscitation strategies dilute the already deficient Traditional resuscitation strategies dilute the already deficient coagulation factors and increase multiple organ failurecoagulation factors and increase multiple organ failure
The aggressive hemostatic resuscitation should The aggressive hemostatic resuscitation should be combined with equally aggressive control of be combined with equally aggressive control of bleeding bleeding
Damage control philosophy can be extended to Damage control philosophy can be extended to hemostatic resuscitationhemostatic resuscitation
restoring restoring normal coagulationnormal coagulation
minimizing crystalloidminimizing crystalloid
Traditional resuscitation strategies dilute the already deficient Traditional resuscitation strategies dilute the already deficient coagulation factors and increase multiple organ failurecoagulation factors and increase multiple organ failure
The aggressive hemostatic resuscitation should The aggressive hemostatic resuscitation should be combined with equally aggressive control of be combined with equally aggressive control of bleeding bleeding

Standard Resuscitation ParadigmStandard Resuscitation ParadigmStandard Resuscitation ParadigmStandard Resuscitation Paradigm
Crystalloid 3:1 Ratio
Blood
FFP
Transient or no response
6-10 u PRBC
Crystalloid
Oh- By the way: show me the
data

Hemostatic ResuscitationHemostatic ResuscitationHemostatic ResuscitationHemostatic Resuscitation
1.1. Early Dx in EDEarly Dx in ED
2.2. 1:1 ratio (PRBC to FFP)1:1 ratio (PRBC to FFP)3.3. ED use of rFVIIaED use of rFVIIa
4.4. Call for FWB from the EDCall for FWB from the ED
5.5. Frequent cryo and plateletsFrequent cryo and platelets
6.6. Repeated doses of rFVIIa in OR and ICU Repeated doses of rFVIIa in OR and ICU as requiredas required
7.7. Minimal crystalloidMinimal crystalloid
1.1. Early Dx in EDEarly Dx in ED
2.2. 1:1 ratio (PRBC to FFP)1:1 ratio (PRBC to FFP)3.3. ED use of rFVIIaED use of rFVIIa
4.4. Call for FWB from the EDCall for FWB from the ED
5.5. Frequent cryo and plateletsFrequent cryo and platelets
6.6. Repeated doses of rFVIIa in OR and ICU Repeated doses of rFVIIa in OR and ICU as requiredas required
7.7. Minimal crystalloidMinimal crystalloid

Thawed PlasmaThawed PlasmaThawed PlasmaThawed PlasmaThawed plasma should be used as a primary Thawed plasma should be used as a primary resuscitative fluid. resuscitative fluid.
This product should be present upon arrival of the This product should be present upon arrival of the casualty in the ED casualty in the ED
This approach not only addresses the metabolic This approach not only addresses the metabolic abnormality of shock, but initiates reversal of the abnormality of shock, but initiates reversal of the coagulopathy present in the . coagulopathy present in the .
Thawed plasma should be used as a primary Thawed plasma should be used as a primary resuscitative fluid. resuscitative fluid.
This product should be present upon arrival of the This product should be present upon arrival of the casualty in the ED casualty in the ED
This approach not only addresses the metabolic This approach not only addresses the metabolic abnormality of shock, but initiates reversal of the abnormality of shock, but initiates reversal of the coagulopathy present in the . coagulopathy present in the .

Electrolytes (mmol/L) average unit of FFP ~ Electrolytes (mmol/L) average unit of FFP ~ 300cc300cc
NaNa 165 (48mmol/unit) 165 (48mmol/unit)
KK 3.3 (1.0mmol/unit)3.3 (1.0mmol/unit)
GlucoseGlucose 2020
CalciumCalcium 1.81.8
CitrateCitrate 2020
LactateLactate 33
pHpH 7.2-7.4 (LR 6.5, NS 5.0)7.2-7.4 (LR 6.5, NS 5.0)
PhosphatePhosphate 3.633.63
Plasma CompositionPlasma CompositionPlasma CompositionPlasma Composition

1:1 Ratio of PRBC to Plasma1:1 Ratio of PRBC to Plasma1:1 Ratio of PRBC to Plasma1:1 Ratio of PRBC to Plasma
Increased FFP transfusions within first Increased FFP transfusions within first 24 hrs of admission were independently 24 hrs of admission were independently associated with increased survival. associated with increased survival.
Median ratio of FFP: RBC was Median ratio of FFP: RBC was 1:1.71:1.7 in in survivors compared to survivors compared to 1:3 1:3 in non-in non-survivors (p<0.001). survivors (p<0.001).
Increased FFP transfusions within first Increased FFP transfusions within first 24 hrs of admission were independently 24 hrs of admission were independently associated with increased survival. associated with increased survival.
Median ratio of FFP: RBC was Median ratio of FFP: RBC was 1:1.71:1.7 in in survivors compared to survivors compared to 1:3 1:3 in non-in non-survivors (p<0.001). survivors (p<0.001).

Mortality PRBC:FFPMortality PRBC:FFPMortality PRBC:FFPMortality PRBC:FFP

Cause of Death
0
10
20
30
40
50
60
70
80
90
100
low medium high
Plasma ratio
Hemorrhage
Sepsis
Airway/Resp
CNS

Fresh Whole BloodFresh Whole BloodFresh Whole BloodFresh Whole BloodFresh whole blood (FWB) must be called for Fresh whole blood (FWB) must be called for early after ED arrival, takes 60 minutes early after ED arrival, takes 60 minutes – Injury Pattern recognitionInjury Pattern recognition
FWB is the optimal resuscitation fluid for FWB is the optimal resuscitation fluid for severely injured casualties. severely injured casualties.
FWB is the best fluid for hypotensive FWB is the best fluid for hypotensive resuscitation for hemorrhagic shock. resuscitation for hemorrhagic shock.

Component Therapy vs Fresh Whole Blood
PRBCPRBCHct 55%Hct 55%335 mL335 mL
PltPlt5.5x105.5x101010
50 mL50 mL
FFP80%
275 mL
So Component Therapy Gives You1U PRBC + 1U PLT + 1U FFP + 10 pk Cryo =
660 COLDCOLD mL•Hct 29%•Plt 87K•Coag activity 65%•750 mg fibrinogen
500 mL Warm500 mL Warm
Hct: 38-50%Hct: 38-50%
Plt: 150-400K Plt: 150-400K
Coags: 100%Coags: 100%
•Armand & Hess, Transfusion Med. Rev., 2003
1500 mg
Fibrinogen
1500 mg
Fibrinogen

Scoring System
SBP < 110
HR > 105
Hct < 32
pH < 7.25
0
10
20
30
40
50
60
70
80
90
0 1 2 3 4
Score
% P
roba
bilit
y of
Mas
sive
Tra
nsfu
sio
n
n=180
n=153
n=203
n=115
n=57

rFVIIarFVIIaIn military casualties requiring massive transfusion, early In military casualties requiring massive transfusion, early administration of rFVIIa decreased pRBC use by 23%administration of rFVIIa decreased pRBC use by 23%
rFVIIa increases the SBP at which arterial rebleeding occursrFVIIa increases the SBP at which arterial rebleeding occurs– suggesting the formation of a tighter, stronger fibrin plug suggesting the formation of a tighter, stronger fibrin plug
in the presence of high concentrations of rFVIIain the presence of high concentrations of rFVIIa
Seven prospective, randomized surgical trials have Seven prospective, randomized surgical trials have documented the safety of this drug.documented the safety of this drug.
The clinical goal is a subnormal PT or INR, ensuring that if The clinical goal is a subnormal PT or INR, ensuring that if bleeding is still occurring then surgical intervention is bleeding is still occurring then surgical intervention is required.required.
In military casualties requiring massive transfusion, early In military casualties requiring massive transfusion, early administration of rFVIIa decreased pRBC use by 23%administration of rFVIIa decreased pRBC use by 23%
rFVIIa increases the SBP at which arterial rebleeding occursrFVIIa increases the SBP at which arterial rebleeding occurs– suggesting the formation of a tighter, stronger fibrin plug suggesting the formation of a tighter, stronger fibrin plug
in the presence of high concentrations of rFVIIain the presence of high concentrations of rFVIIa
Seven prospective, randomized surgical trials have Seven prospective, randomized surgical trials have documented the safety of this drug.documented the safety of this drug.
The clinical goal is a subnormal PT or INR, ensuring that if The clinical goal is a subnormal PT or INR, ensuring that if bleeding is still occurring then surgical intervention is bleeding is still occurring then surgical intervention is required.required.

When comparing rFVIIa (+) to rFVIIa (-) patientsWhen comparing rFVIIa (+) to rFVIIa (-) patients– 24 hour mortality was 7/49 24 hour mortality was 7/49 (14%)(14%) and 26/75 and 26/75 (35%),(35%), (p=0.01) (p=0.01)
– 30 day mortality was 15/49 30 day mortality was 15/49 (31%)(31%) and 38/75 and 38/75 (51%),(51%), (p=.03). (p=.03).
SBP was higher in the rFVIIa (+) groupSBP was higher in the rFVIIa (+) group
The use of rFVIIa was associated with improved early and late The use of rFVIIa was associated with improved early and late survival after severe trauma and massive transfusion. survival after severe trauma and massive transfusion. rFVIIa was not associated with increased risk of thrombotic rFVIIa was not associated with increased risk of thrombotic events.events.
The Effect of Recombinant Activated Factor VII on Mortality in Combat-Related Casualties With Severe Trauma and Massive TransfusionPhilip C. Spinella, MD, Jeremy G. Perkins, MD, Daniel F. McLaughlin, MD, Sarah E. Niles, MD, MPH,Kurt W. Grathwohl, MD, Alec C. Beekley, MD, Jose Salinas, PhD, Sumeru Mehta, MD, Charles E. Wade, PhD,and John B. Holcomb, MD J of Trauma- Feb 2008

Retrospective Study of Combat CasualtiesRetrospective Study of Combat Casualties Who Who diddid and and did notdid not Receive rFVIIa Receive rFVIIa
Jan 2004 - Oct 2006 Jan 2004 - Oct 2006 n = 615n = 615
Retrospective Study of Combat CasualtiesRetrospective Study of Combat Casualties Who Who diddid and and did notdid not Receive rFVIIa Receive rFVIIa
Jan 2004 - Oct 2006 Jan 2004 - Oct 2006 n = 615n = 615
329 US casualties 329 US casualties did did notnot receive rFVIIa receive rFVIIa
ISS = 21 ISS = 21 ± 14± 14
Complications = 17%Complications = 17%– Thrombotic = 11%Thrombotic = 11%
ICU days = 6 ICU days = 6 ± 24± 24
Hospital days = 27 Hospital days = 27 ± 40± 40
PRBCs = 8 PRBCs = 8 ± 7± 7
Mortality = Mortality = 19% 19%
286 US Casualties 286 US Casualties did did receive rFVIIareceive rFVIIa
ISS = 24 ISS = 24 ± 13± 13**
Complications = 23%Complications = 23%**– Thrombotic = 14%Thrombotic = 14%
ICU days = 10 ICU days = 10 ± 15± 15**
Hospital days = 37 Hospital days = 37 ± 35± 35**
PRBCs = 18 PRBCs = 18 ± 22± 22**
Mortality = Mortality = 21%21%
* P < 0.05

SummarySummaryRecognize ShockRecognize Shock– Five Critical CriterionFive Critical Criterion– Identify the critical 10 %Identify the critical 10 %
Resuscitate ImmediatelyResuscitate Immediately– Devote attention to Hemostatic resuscitationDevote attention to Hemostatic resuscitation
Provide volume that also restores the hemostatic Provide volume that also restores the hemostatic cascadecascadeMinimize crystalloidMinimize crystalloidStop the bleedingStop the bleedingStay out of troubleStay out of trouble
Thawed or liquid plasmaThawed or liquid plasma– Whole BloodWhole Blood