Clinical conundrums in a case of upper quadrant dysfunction
-
Upload
lisa-roberts -
Category
Documents
-
view
214 -
download
1
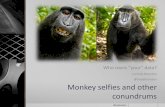
Transcript of Clinical conundrums in a case of upper quadrant dysfunction

lable at ScienceDirect
Manual Therapy 17 (2012) 192e195
Contents lists avai
Manual Therapy
journal homepage: www.elsevier .com/math
Case report
Clinical conundrums in a case of upper quadrant dysfunction
Lisa Roberts a,b,*
a Therapy Services Department, Southampton University Hospitals (NHS) Trust, Tremona Road, Southampton, Hampshire SO16 6YD, United Kingdomb Faculty of Health Sciences, University of Southampton, Highfield, Southampton, Hampshire SO17 1BJ, United Kingdom
a r t i c l e i n f o
Article history:Received 6 March 2011Received in revised form16 May 2011Accepted 17 May 2011
Keywords:NeurodynamicDouble crushScapho-trapezio-trapezoidal fusion
* Faculty of Health Sciences, Building 45, UniversitSouthampton, Hampshire SO17 1BJ, United Kingdomfax: þ44 (0) 23 8059 5301.
E-mail address: [email protected].
1356-689X/$ e see front matter � 2011 Elsevier Ltd.doi:10.1016/j.math.2011.05.009
a b s t r a c t
This case study charts the progress of a 60-year-old angling coach presenting with a complex upperquadrant dysfunction. Following a brief summary of the history and physical examination, the main focusof the paper explores the mechanical and physiological rationale for adopting a neurodynamic approachfor a proposed double crush condition. This case further highlights mismatches that arose between theclinical findings and traditional healing timescales, and the importance of considering pathomechanics ofthe whole quadrant in complex clinical circumstances.
� 2011 Elsevier Ltd. All rights reserved.
1. Introduction
In December 2009, the patient was referred to physiotherapyone year following a scapho-trapezio-trapezoidal (STT) joint fusionfor his longstanding wrist pain, secondary to degenerative arthritis.Post-operatively, he acquired an infection, which was treated withsix weeks of intravenous antibiotics, multiple immobilizing plastersand opioid analgesia (morphine). At six months, he was furtherdiagnosed with a ‘nasty carpal tunnel syndrome’ which was surgi-cally decompressed, resulting in worse pain and anaesthesiathroughout the hand and wrist. Five months later, the patientreported numbness and loss of dexterity in all fingers, whichsignificantly impacted upon his work as an angling coach.
2. Referral and investigations
A referral was made to physiotherapy for desensitisation andsensory re-education, noting a superficial radial nerve neuropraxia.Nerve conduction study findings revealed “Only very mild slowingacross the carpal tunnel.; although there is an un-recordablesuperficial radial nerve response.” In clinic letters, the orthopaedicsurgeon stated: “I am afraid that I cannot explain the profoundnumbness here in light of the nerve studies. The numbness does goacross all the fingers and not just that of the median nerve.”
y of Southampton, Highfield,. Tel.: þ44 (0) 23 8059 5311;
All rights reserved.
3. Examination findings
At his initial assessment, the patient reported being unable to tiehooks, cast lines and assist the children (and adults) he was coach-ing. He expressed frustration with his clumsiness, disappointmentand anger at his lack of progress, and described his arm as ‘useless.as if it didn’t belong’. He reported virtually constant numbness, withonly occasional paraesthesiae, unaffected by activity (Fig. 1).
The key findings from the physical examinationwere: flattening ofthe mid-thoracic kyphosis; increased tension in the upper fibres oftrapezius; restriction in all active thoracic and cervical movements(except cervical flexion) (Fig. 2); only 90� of right active shoulderabduction and flexion; discomfort on all shoulder girdle active move-ments; hypomobility of the first rib, cervicothoracic junction and onposteroanterior palpation of the thoracic spine down to the level of T6.
There was minimal limitation in active elbow flexion andextension and 25% loss of active radio-ulnar pronation on the rightside, limited by pain in the posterior upper arm.
In addition, neurological testing revealed weakness at all levelsfrom C5 to T1 and neurodynamic testing reproduced symptoms forthe median, ulnar and radial nerves on the right, and the medianand radial nerves on the left. Palpation (in neutral) revealed localtenderness and apparent tethering of the carpal tunnel scar. Insummary, this routine STT fusion had progressed to involve thewhole upper quadrant over the intervening twelve months.
4. Clinical conundrums
The patient considered he was far worse following surgery thanwith his original arthritis, and twelve months on, presented with

Fig. 1. Body chart at the initial consultation.
L. Roberts / Manual Therapy 17 (2012) 192e195 193
symptoms that did not fit traditional healing timescales. Forexample, neurapraxia represents the mildest of the three periph-eral nerve injuries proposed by Seddon in 1942, inwhich distortionof myelin occurs near the nodes of Ranvier, producing segmentalconduction block without Wallerian degeneration (Bradley et al.,2004a). Given that the loss of function is transient (until remyeli-nation occurs), this type of injury reportedly has an excellentprognosis for complete recovery and is rarely clinically evidentbeyond six weeks (Bradley et al., 2004b). Therefore, why was itapparent at twelve months? Second, the distribution of numbnessinvolving the whole limb did not match the nerve conductionfindings. Third, in addition to the non-dermatomal sensory find-ings, it was important to consider possible mechanisms for thebilateral signs implicating both median and radial nerves.
The stakes were high and no further medical interventions wereplanned. Furthermore, there was a mismatch in expected outcomebetween the surgeon (who expressed hope of some recovery overtime), and the patient (who expressed grave doubts about thefuture, given a year had already elapsed).
5. Clinical reasoning strategies
Developing a treatment plan required multiple clinicalreasoning strategies. Pattern recognition highlighted the impor-tance of starting centrally with the spine and including the first rib,which needs to bemobile to enable the clavicle to rotate posteriorly30� and the arm to elevate (Kapandji, 1982). Pattern recognitionalone however was insufficient, and using a hypothetico-deductiveapproach, it was hypothesized that hypomobility at the cervico-thoracic junction contributed to the neurodynamic symptoms.
Fig. 2. Initial active ranges of movement modified Maigne diagrams representing limitations3 dashes ¼ severe restriction. [The dashes are diagrammatic representations only and the
Therefore, the initial treatment plan was to mobilise the thoracicand cervical spines, to test this theory.
6. Treatment progression
Having considered safety checks for cervical arterial dysfunc-tion, and contra-indications to manual therapy, treatmentcommenced with posteroanterior glides and transverse mobi-lisations (to the left) to T2e6 spinous processes. Central techniqueswere chosen as the hypomobility was central and the neuro-dynamic symptoms were bilateral. Six sets of 10� grade III, oscil-latory, longitudinal mobilisations ( ) were performed to thecervical spine in neutral and four further sets in flexion (targetingthe cervicothoracic junction), and deep kneading techniques wereapplied to the trapezius muscle. Immediately post-treatment, thepatient reported paraesthesiae in his fingers rather than numbness,which was promising, given the symptom duration.
One week later, the patient reported significant progress, withincreased sensitivity in his fingertips, episodic tingling, onlyoccasional numbness, and increased grip precision. However,weakness was still apparent, as the patient reported droppinga mug of coffee. Further longitudinal cervicothoracic junctionmobilisations and neurodynamic techniques were introduced,involving cervical flexion in slumped-sitting, moving the neuraltissues through range. In addition, there was localised discomfortand resistance on gliding the right dorsal scapular nerve at T4-5region and this resolved with three sets of grade III� unilateralmobilisations at C4 and local gentle frictions in the upper thoracicregion, to further encourage neural gliding. Physiological mobi-lisations of the scapula (elevation and protraction) were per-formed and local friction massage applied to the carpal tunnel scarsite. After three treatments, the patient could abduct all his fingersas his strength was increasing. The patient was encouraged to:maintain the improvements gained through fist traction to targetthe cervicothoracic junction; undertake five active thoracicmovements (with exhalation) to each of the six movements, atleast twice a day; and undertake a slider exercise for the neuraltissues in slump sitting using cervical spine flexion �10, at leastthree times daily.
During the next four sessions, manual therapy techniquesincluded: a progression through cervical side flexion (Fig. 3)localising in a cephlad direction as necessary; longitudinal mobi-lisations to the first rib; and soft tissue techniques in the cervicaland thoracic regions.
Further friction massage was applied to the carpal tunnel scarsite and the home exercise programme (designed to mobiliseneural tissues) was progressed, including three sets of 30 shouldergirdle depressions, at least twice daily and a similar dosage of two-ended median nerve sliding techniques, (in the upper limb tensiontest position with median nerve bias) using reciprocal elbow
of active movements. One dash ¼mild restriction, 2 dashes ¼moderate restriction andir positions do not form graphic rating scales.]

Fig. 3. Mobilising the cervicothoracic junction.
L. Roberts / Manual Therapy 17 (2012) 192e195194
flexion/extension (with the wrists and fingers maintained inextension). Improvements were evident at every session in func-tion, upper limb strength; range of movement (Fig. 4); thenarmuscle bulk; and most importantly for the patient, the ability toresume fishing without tingling, paraesthesiae or numbness.
After seven treatments, the patient was overjoyed to fish ina competition for 6 hwith only slight, resultant local soreness in thehand and cervical spine.
At his final review (session 11), the patient reported climbinga tree to retrieve a child’s fishing tackle, describing his recovery as100%, and his arms ‘stronger than ever’. He relished his review withthe orthopaedic surgeon, who commented that treating the cervi-cothoracic junction had ‘dramatically improved the neurogenicsymptoms in his hand’.
7. Rationale for approach
The main approach used in this case study was neurodynamic,considering the relationship between the mechanical and physio-logical mechanisms within the nervous system.
Peripheral nerves are strong, largely comprised of connectivetissue, surrounded by a sheath and are connected through the
Fig. 4. Evidence o
body, from the cranial dura to the filum terminale. This designenables them to: slide and glide; return from an elongated toa shortened position; withstand compression, jolting, repetitiveforces and bending (Butler, 2000, p. 101). In a study of ten unfixedcadavers, with the shoulder maintained in 90� abduction, Zoechet al. (1991) demonstrated 100 mm excursion from themedian nerve bed in wrist flexion þ elbow flexion to wristextension þ elbow extension, with an average median nervelength of 517 mm. This represents a length difference of 19% and,in a complex activity like casting a fishing rod, as in this casereport, the patient’s median nerve must be able to respond to suchbiomechanics.
When mechanical stresses are applied to nerves, a complexchain of events occurs evoking physiological responses, such asalterations in intraneural blood flow, impulse traffic and axonaltransport (Shacklock, 1995). In this case study, it was not possible todetermine the precise aetiology of the symptoms, however varioushypotheses may be proposed from the literature:
Mechanical:
� Tight muscles through which the nerves must slide (Butler,2000, p. 99).
f progression.

L. Roberts / Manual Therapy 17 (2012) 192e195 195
� Some scarring, linking the nervous system to the surroundingtissues, creating foci of mechanical pressure (Butler, 2000,p. 99).
� An abnormal impulse generating site (Butler, 2000, p. 99) in theoverstretched, pinched and swollen system, resulting from theoriginal surgery and infection.
� If the peripheral nerve sheath was injured, it may have becomefibrotic and shrunk (Millesi et al., 1995).
� Possible connections between peripheral nerves, which aredescribed as common (Butler, 2000, p. 404).
� Irritation, compression or traction of the brachial plexuscompromising nerve function and possibly indicating a neuro-logical thoracic outlet syndrome (Watson et al., 2009).
� Reduced axoplasmic flow due to physical constriction of thenerve (Butler, 2000, p. 113).
Physiological:
� Axoplasmic flow may also have been reduced by ischaemia,eg. in the patient’s wrist, post-surgery: Axoplasm (the cyto-plasm of peripheral nerves) carries material, including ionchannels and neurotransmitters bound for the cell membrane(Butler, 2000, p. 112). There is also a retrograde transportsystem, flowing at speeds of 200 mm per day, carrying unusedanterograde and exogenous material, including neutrophicfactors (Butler, 2000, p. 112). Axoplasmic flow is vital formaintaining the axon’s physical health and will be compro-mised when neural mobility is restricted. The thixotrophicproperties of axoplasm further justify a neurodynamicapproach.
� When operating on carpal tunnels, Phalen (1972) noted thepresence of venous engorgement and peripheral vasodilation.He surmised that venous stasis would add further pressure,resulting in a pressure gradient between the artery and vein, sothat blood is forced into the tunnel, across blood-nervebarriers. Movement helps normalise this pressure gradientand disperse the ‘inflammatory soup’ collected in the connec-tive tissues of the median nerve (Butler, 2000, p. 405).
� ‘Double crush’: This concept was originally proposed by Uptonand McComas (1973), from a study of 115 patients with carpaltunnel syndrome or lesions of the ulnar nerve at the elbow.They identified electrophysiological and clinical evidence ofneural lesions at the neck in 81 out of 115 patients, hypothe-sizing that neural function is impaired because single axons,having been compressed in one region, become especiallysusceptible to damage at another site. Biologically, doublecrush symptoms may be due to receptor upregulation in thedorsal root ganglion and increased expression of the inflam-matory mediator (cytokine) IL-1, which promotes the secretionof nerve growth factor (a cytokine that serves the neutrophicrole of promoting nerve regeneration and survival of nervecells) in the dorsal root ganglia (Yamamoto et al., 1998).
Given the complex mechanical and physiological responses tosurgery (and infection), a double crushwas consideredmost likely toexplain the spread and coexisting symptoms. The key to rehabilita-tionwasmovement, since all healing tissues, especially those largelycomprising connective tissue, required appropriate movement toassist healing and restore mechanical abilities (Butler, 2000, p. 384).Therefore, the starting point was mobilising the hypomobile cervi-cothoracic junctionandfirst rib, to ensure theneural soft tissues couldmove more freely. Using neurogenic massage techniques across thecarpal tunnel scar, whilst not physically influencing the nerve, arejustified biologicallywhen there is swelling around thenerve, venousstasis and organising scar in the peripheral nerve connective tissue
sheath (Butler, 2000, p. 383). This needed to be done alongside anactive mobilisation programme, focussing on elongating and glidingneural tissues. The neurodynamic techniques aimed to mobilise thescar tissue and improve blood supply and physiological function,including axoplasmic flow (Zvulun, 1998). In summary, making thelink between the hand symptoms and the spine underpinned therationale for a neurodynamic approach. It was important to considerthe patient’s responses to neurodynamic testing were not solely duetomechanical effects on neural tissues, but also coexisting inputs andprocessing in the central nervous system (Butler, 2000, p. 358),compounded by psychosocial factors, especially the threats to hisidentity and livelihood as an angling coach.
This case highlights the possibility of gaining significantimprovements in symptoms beyond physiological healing time-scales and that the speed of change following manual therapytreatments can be significant e for example distinct changes infinger abductionwithin a 30-min treatment session, presumably asa consequence of improved neuromuscular firing, as suddenchanges were unlikely to be due to cumulative strengthening. It hasbeen suggested that elongation of muscular connective tissue maycontribute to the enhancement of motor function (Zvulun, 1998).
In conclusion, this case demonstrates the importance of history-taking, keeping an open mind and challenging when the evidencedoes not appear to ‘fit’. There were mismatches between healingtimescales and clinical presentation, with unexpected findings suchas bilateral involvement of the median and radial nerves, therebyproviding evidence that this could not be due to local patho-mechanics in the hand. A double crush phenomenon could explainhow a persistent proximal lesion would account for an apparentsurgical failure after adequate decompression of a median nerve atthe wrist (Upton and McComas, 1973). In future, when facingcomplex clinical conundrums, it is important for clinicians toconsider the pathomechanics of the whole quadrant.
Acknowledgements
This work was awarded the British Health Professionals inRheumatology Clinical Prize 2011. Thanks are expressed to: thepatient for his encouragement to write this case study; ArthritisResearch UK (who fund the author’s academic post); and to MartinKerridge-Weeks MSc MCSP MMACP for his helpful comments onthe manuscript.
References
Bradley WG, Daroff RB, Fenichel GM, Jankovic J. Neurology in clinical practice.Principles of diagnosis and management. 4th ed., vol. I. Philadelphia: Butter-worth-Heinemann; 2004a. p. 498.
Bradley WG, Daroff RB, Fenichel GM, Jankovic J. Neurology in clinical practice.Principles of diagnosis and management. 4th ed., vol. II. Philadelphia: Butter-worth-Heinemann; 2004b. p. 1181.
Butler DS. The sensitive nervous system. Adelaide: Noigroup Publications; 2000.Kapandji IA. The physiology of the joints. In: Upper limb, vol. 1. Edinburgh:
Churchill Livingstone; 1982. pp. 66e67.Millesi H, Zoch G, Riehsner R. Mechanical properties of peripheral nerves. Clinical
Orthopaedics and Related Research 1995;314:76e83.Shacklock M. Neurodynamics. Physiotherapy 1995;81(1):9e16.Phalen GS. The carpal-tunnel syndrome. Clinical evaluation of 598 hands. Clinical
Orthopaedics and Related Research 1972;83:29e40.Upton ARM, McComas AJ. The double crush in nerve-entrapment syndromes. The
Lancet; 1973 August 18:359e62.Watson LA, Pizzari T, Balster S. Thoracic outlet syndrome part 1: clinical manifes-
tations, differentiation and treatment pathways. Manual Therapy 2009;14:586e95.
Yamamoto S, Ochi N, Ryoke K, Yamaguchi H. Expression of cytokines in the dorsalroot ganglion cell body in an experimental model of entrapment neuropathy.Hand Surgery 1998;3(2):175e83.
Zoech G, Reihsner R, Beer R, Millesi H. Stress and strain in peripheral nerves. Neuro-orthopaedics 1991;10:73e82.
Zvulun I. Mobilizing the nervous system in cervical cord compression. ManualTherapy 1998;3(1):42e7.