Circulatory disorders of liver
-
Upload
saurav-singh -
Category
Health & Medicine
-
view
276 -
download
3
Transcript of Circulatory disorders of liver

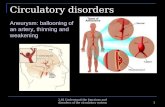
CIRCULATORY DISORDERS OF LIVER
DR.SAURAV SINGH

GENERAL CONSIDERATION
Liver has enormous flow of blood , & has dual blood supply Portal Vein : provides 60-70% of hepatic blood
flow Hepatic artery : supplies 30-40%
Portal vein & hepatic artery enter the liver through the hilum (porta hepatis)
Within the liver the branches of the portal veins, hepatic arteries & bile ducts travel in parallel in portal tracts

MECHANISMS

IMPAIRED BLOOD INFLOW Hepatic Artery Compromise
Liver infarcts are rare because of its dual blood supply
However, thrombosis / compression of an intrahepatic branch of hepatic artery can occur due to
Embolism Neoplasia Polyarteritis Nodosa or Sepsis
This results in localised infarct which can be anemic & pale tan / hemorrhagic
Retrograde arterial flow through accessory vessel when coupled with the portal venous supply is usually sufficient to sustain the liver parenchyma
Exception : In a transplanted liver, when the hepatic artery is thrombosed , it leads to infarction of the major ducts of biliary tree & finally loss of the organ


PORTAL VEIN THROMBOSIS
ACQUIRED DISEASE OF LARGE PORTAL VEINS
Thrombosis of the portal vein is associated with the presence of a hypercoagulable state, vascular injury,or stasis.
Associated hypercoagulable state includes Pregnancy O.C.P’s Prothrombin mutation Protein C/S deficiency Myeloproliferative disorders etc.

Inflammation of the portal vein can be induced by infection chemical injury initiated by pancreatitis accidental or surgical trauma
Stasis is a cause of portal vein thrombosis in Cirrhosis primary or secondary neoplasm retroperitoneal fibrosis.


Portal vein obstruction with tumor and or thrombus occurs in 23-70% of patients with hepatocellular carcinoma and in 5-8% of patients with metastatic tumor in liver.
Thrombosis in the presence of cirrhosis or hepatic neoplasm may precipitate hepatic decompensation,variceal bleeding or ascites.

ACQUIRED DISEASE OF SMALL PORTAL VEINS
Patients with portal hypertension due to obliteration of small portal veins may also have evidence of systemic microvascular disease as seen in Rheumatoid artheritis Myeloproliferative disease S.L.E Polyarteritis Nodosa etc.
Obliteration of small portal veins occur early in the course of primary biliary cirrhosis, primary sclerosing cholangitis Sarcoidosis

According to the concept of ‘menage a foie’ : “Development of injury to one portal structure because of inflammation primarily directed at a neighbouring portal tract structure”
This explains that a local portal venous obliteration may be secondary to arteritis or to ductal inflammation.( eg : Primary biliary cirrhosis & primary sclerosing cholangitis)
Portal vein obliteration may also be caused by Granulomas in sarcoidosis , Mineral oil granulomas Exposure to Throtrast.


Emboli or local thrombosis are important in Schistosomiasis Normal ageing C.C.F
Increased A.L.P, is seen in patients with Temporal/ rheumatoid arteritis Nodular regenerative hyperplasia Idiopathic portal hypertension Sarcoidosis
NOTE : The reason for above (raised ALP ) is : Ducts may also be injured by inflammation primarily involving the arteries & other portal tract structures

SCHISTOSOMIASIS
It is the most common cause of portal hypertension in this world.
Eggs deposited in the rectal veins float into the small portal veins where a transient eosionophilic infiltrate is followed by a granulomatous reaction.
The veins are obliterated with fibrous tissue and PAS positive egg cuticle is seen in surgical wedge biopsies.
Secondary proximal thrombosis causes dense fibrosis of the main perihilar portal tracts,so called Symmer’s pipe-stem fibrosis.


PATHOLOGY OF PORTAL VEIN DISEASE
After thrombosis, followed by organisation , large veins may have subtle white intimal plaques/ mural calcification
When recanalisation is less complete, the lumen may be obliterated or contain complex webs
Portal veins > 200 µm in diameter have eccentric intimal fibrous thickening which may be layered suggesting recurrent thrombosis
Veins < 200 µm in diameter dissapear as the wall becomes incorporated into fibrous scar while large veins may have residual wall best seen with elastic trichome/ Movat stain


PATHOLOGY OF PORTAL VEIN DISEASE(CONTD.)
Some portal veins remain patent & becomes dilated if the supplying portal veins are patent because the elevated portal pressure is transmitted to the the small vein
Now, this dilated vein often expand outside the portal tract stroma into the adjacent parenchyma giving an ‘ectopic’ appearance
Acute thrombosis of small portal vein results in a pseudo infarct( of Zahn)



HEPATIC VEIN THROMBOSIS: BUDD-CHIARI SYNDROME.
• Budd chiari syndrome is a clinicopathologic
syndrome variously defined as hepatic vein thrombosis,noncardiac venous outflow obstruction or venous outflow obstruction of any cause or site.
• Classical findings are :• Hepatomegaly• Ascites• Abdominal pain• Varying degrees of hepatic dysfunction

Hepatic vein thrombosis is associated with
primary myeloproliferative disorders, inherited disorders of coagulation, antiphospholipid syndrome, paroxysmal nocturnal hemoglobinuria and intra-
abdominal cancers.

AETIOLOGY OF BUDD-CHIARI SYNDROME
75% of patients in U.S, U.K and France with Budd-Chiari syndrome have a recognized pre disposing factor belonging to Virchow’s triad
The most common is hypercoagulable state specially Myeloproliferative disease such as : polycythemia vera etc.


PATHOLOGY OF BUDD-CHIARI SYNDROME The acute lesions after hepatic vein thrombosis are
dilatations of veins & sinusoids & variable degree of necrosis
Sinusoids are congested & R.B.C’s infilterate the space of disse
As the disease advances, the sinusoids become collagenized & dilated & hepatocytes become atrophic & are lost
The small hepatic vein dissappear as they get incorporated into septa which eventually link hepatic vein to establish a cirrhosis with relative sparing of portal triads so called “reversed lobulation cirrhosis or veno-centric cirrhosis”


MORPHOLOGY
The liver is swollen and red-purple and has a tense capsule.
Microscopically the affected hepatic parenchyma reveals severe centrilobular congestion and necrosis.
The major veins may contain totally occlusive fresh thrombi, subtotal occlusion, or in chronic cases, organized adherent thrombi.

BUDD-CHIARI SYNDROME-TREATMENT
o Address underlying cause; high mortality without treatment
o Acute interventions: o Surgical creation of portal-systemic shunt (portal
vein to systemic circulation), which allows reverse flow through portal vein, but hepatic artery inflow preserved to prevent infarction.
o Angiographic thrombectomy and/or dilation of hepatic vein.

PASSIVE CONGESTION.
Right sided cardiac decompensation leads passive congestion of liver.
The liver is slightly enlarged,tense and cyanotic, with round edges.
Microscopically there is congestion of centrilobular sinusoids.

CENTRILOBULAR NECROSIS
Left-sided cardiac failure or shock may lead to heaptic hypoperfusion and hypoxia, causing ischemic coagulative necrosis of hepatocytes in the central region of the lobule (centrilobular necrosis).
The combination of hypoperfusion and retrograde congestion acts synegistically to cause centrilobular hemorrhagic necrosis.
Central lobular congestion, producing “nutmeg” liver.
Microscopy there is sharp demarcation of viable periportal and necrotic pericentral hepatocytes, with suffusion of blood through the centrilobular region.

NUTMEG LIVER

VENO-OCCLUSIVE DISEASE
Veno occlusive disease is characterized by fibrous occlusion of small hepatic veins less then 1mm in diameter with secondary parenchymal congestion.
Originally described in Jamaican drinkers of pyrolizidine alkaloid-containing bush tea.
The disease usually affects young children but adults are also susceptible.
The onset may be acute or insidious.

Patients usually present in the 3 weeks after therapy with weight gain Thrombocytopenia Jaundice hepatic failure increased serum aminotransferases and alkaline
transferases and alkaline phosphtase.

CLINICAL FEATURE
o Disease is characterized by o rapid onset of abdominal pain,o hepatomegaly o ascites usually without jaundice,splenomegaly or
fever

The pathogenesis of the lesions is believed to be a primary injury to the endothelial cells of sinusoids and small venules.
The mechanism of endothelial injury after cytotoxic drugs may involve depletion of cellular glutathione.

MORPHOLOGY
Characterised by obliteration of hepatic vein radicle by varying amounts of sub endothelial swelling & finally reticulated collagen
In acute disease there is striking centrilobular congestion with hepatocellular necrosis & accumulation of hemosiderin laden macrophages
As the disease progresses obliteration of lumen of venule is easily identified with special stain for connective tissue

SINUSOIDAL OBSTRUCTION SYNDROME OR VENO-OCCLUSIVE DISEASE


DIFFERENTIAL DIAGNOSIS
Constrictive pericarditis Congestive cardiac failure Hepatic vein thrombosis

SINUSOIDS
Sinusoids are lined by modified endothelial cells containing fenestrations 50-300 nm in diameter which allow passage of lipoproteins and other large molecules but provide a barrier to blood cells.
Sinusoidal endothelial cells have numerous bristle-coated pits,pinocytotic vacuoles.

Sinusoidal endothelial cells differ from venous and arterial endothelial cells in expressing variety of markers including CD32 and CD16,aminopeptidase N,CD32,CD4 and CD54.
Sinusoidal endothelial expression of CD34 and CD31 is an indicator of angiogenesis, seen focally in cirrhosis, focal nodular hyperplasia, and dysplastic nodules.

SINUSOIDAL DILATION
Sinusoidal dilation occurs when there is increased pressure in the hepatic veins, atrophy of hepatocytes or disruption of the sinusoidal reticulin fibres.
It often shows a zonal distribution: centrolobular,periportal or irregular.

Centrolobular sinusoidal dilation is most common with prominent involvement of the perivenous region extending to the midzonal region .
It is observed in some drug induced lesions in rheumatoid arthritis,and in malignant or granulomatous diseases.

Periportal dilation affects the periportal sinusoids, eventually extending more centripetally.
Long term contraceptive use is a cause, as is preeclampsia and eclampsia in association with sinusoidal fibrin thrombi and periportal ischemic hepatocellular necrosis.

PELIOSIS HEPATIS
Peliosis hepatitis is primary diffuse dilation of sinusoids.
It occurs in any condition in which efflux of hepatic blood is impeded.
The liver contains blood filled cystic spaces, either unlined or lined with sinusoidal endothelial cells.

Peliosis hepatis is associated with many diseases including cancer,tuberculosis,AIDS,or post transplantation immunodeficiency.
Macroscopic lesions are usually induced by anabolic, estrogenic or adrenocortical steroids.
Microscopic lesions occur in patients receiving thiopurines for renal transplantation,liver transplantation or various malignancies.

Peliotic lesions found in AIDS and other immunosuppressed patients are caused by bacterial organisms (Bartonella species)
Patients often have peliosis of spleen and lymph nodes and cutaneous angiomatous lesions.

PELIOSIS HEPATITIS:PATHOLOGY
H&E: blood-filled spaces, incompletely lined by endothelial cells


REFERENCES
Robbins – 8th Edition Rosai & Ackerman – Surgical Pathology – 9th
Edition Mac Sween’s – Pathology of Liver