Child with pallor & jaundice (hemolytic anemia)
-
Upload
safia-sky -
Category
Health & Medicine
-
view
443 -
download
1
description
Transcript of Child with pallor & jaundice (hemolytic anemia)

اشرح لي صدري و { ر لي رب يس
اني أمري واحلل عقدة من ل س
}يفقهوا قولي
حيـــــــــــــم حمن الر بســــــــــــــم هللا الر

Child with pallor and jaundiceby 5th year medical students_ Tripoli university
group 6
(Haemolytic anaemia)

CONTENTS
• Introduction
• Sickle cell anemia
• Autoimmune (AIHA)
• Thalassemia

Jaundice is yellowish discoloration of skin and mucous membranes due to ↑ in
blood bilirubin
Pallor is is a pale color of the skin which can be caused by illness, emotional shock or
stress, or anemia,,, and is the result of a reduced amount of oxyheamoglobin in skin or mucous membranes
Anemia is HB level below the normal rage according To age
Neonate <14g/dl1_12 months <10g/dl1-12 year<11g/dl
Anaemia results from the following mechanisms:
1_reduced red cell production - either due to ineffective erythropoiesis (e.g. iron deficiency, the commonest cause of anaemia) or due to red cell aplasia
2_blood loss3-increased red cell destruction (haemolysis)

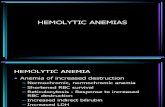
What is hemolytic anemia?
It is ↓ red cell life span due to ↑ red cell destruction in the circulation (intravascular) or in liver & spleen (extravascular)
note: BM can ↑ production about 8 fold , so symptoms & signs of hemolytic anemia appear when the BM no longer able to compensate for the premature destruction of RBCs(exeeding BM capacity for compensating)


Haemolytic anaemia
Red cell mem
disord.
ImmuneHaemoglobinopathiesRed cell enzyme
disord.
Hereditary
Spherocytosis
G6PDH
Def.
Thalassaemia
AIHA
Sickle cell
anemia

Hereditary spherocytosis: A genetic disorder of the red blood cell membrane
clinically characterized by anemia, jaundice (yellowing) and splenomegalyM.O.IIt is AD disease .
Defect or Deficiency of Beta Spectrin or Ankyrin Loss of membrane surface areabecomes more spherical Destruction in Spleen
Clinical picture*jaundice - usually develops during childhood but may be intermittent; may
cause severe haemolytic jaundice in the first few days of life
*anaemia - presents in childhood with mild anaemia (haemoglobin 9-11g/dl),
but the haemoglobin level may fall with an intercurrent infection; many children have 'compensated' haemolysis with a normal haemoglobin
* splenomegaly - depends on the rate of haemolysis;
* gallstones - due to increased bilirubin excretion

InvestigationCBCBlood filmOsmotic fragility test

• Treatment• oral folic acid as they have a raised folic acid
requirement secondary to their increased red blood cell production. .
• Splenectomy is beneficial but is only indicated for poor growth or troublesome symptoms of anaemia (e.g. severe tiredness)

Autoimmune Hemolytic Anemia:
(AIHA) Autoimmune disease involving auto-antibodies directed toward RBC surface antigens leading to accelerated destrution (hemolysis).

Etiology:
1. Idiopathic (most common cause).
2. Autoimmune disease: (SLE,RA).
3. Neoplastic: e.g lymphoma, myeloma
4. Drugs: methyldopa,penicillin
5. Infection: mycoplasma, EBV

Clinical picture:
_ Anemia + jaundice.
_ hand, foot and cyanosis (cold type).
_splenomegaly (warm type).

Two main types:
%
Site
Antibody
Active temperature
Treatment
Warm AIHA
80% of cases
Extravascular hemolysis
IgG
37 degree
Steroids & splenectomy.
Cold AIHA
20% of cases
Intravascular hemolysis
IgM
4 degree
Warming & plasmapheresis.

Investigation:
_CBC: normocytic normochromic or macrocytic hyperchromic.
_Blood film: spherocytosis, schistocytes.
_Direct antiglobuline test(Coombs’ test) : +ve


treatment:
_Treat underlying causes.
_Corticosteroids: response may take 3 weeks
_Splenectomy.
_Immunosuppressive therapy.
_Blood transfusion.

ThalassemiaGenetic disorders of Hb synthesis with ↓ produc.of either α or ß
polypeptide chains of Hb molecules (α-thalass. or ß- thalass.)
M.O.I : AR
ß -thalass. Carrier Carrier
Diseased
Onset : ≥ 6 months “ complete switch from fetal
Hb α2δ2 to adult Hb α2ß2 “


HistoryOnset of anemia > 6 months
Symptoms of anemia
FTT
History of frequent blood transfusion
not improve with iron supplement “ if minor”
positive FH

C\P & Complic.
Thalassaemic face
Causes of mortality: high output HF from sever Anm. or iron overload

Investigation
MCH↓ &CBC : ↑Retics. \ ↓MCV
Bld film\ target cells (T) ,
Poikilocytes (p) , microcytes (M)
Hb electrophoresis :↑↑Hb F
US “gall stone”
Imaging :

Pathological fractureSC compression

Management1-Monthly bld transfusion (aim : Hb >10g\dl , reduce growth failure ,
prevent bone deformation)
2-Iron chelation therapy (each unit of transfused RBCs contain 200mg
elemental iron)
3-Folic acid (hyperactive BM)
4-Splenectomy (if hyperactive \ after vaccination).
5-Cholecystectomy (for bilirubin stone)
*gene therapy “deliver globin gene into cells by viral vector”
*Emerging therapy “induce F-Hb by butyrates”
*BM transplant : (young , HLA match, no organ dysfunction.)

What is the Difference ß- thalass.minor & IDA?
NOTE :(both are microcytic hypochromic) Iron def. anemiaß-Thalassemia minor
Reticulocytes↓Reticulocytes↑
No abnormal cells , ↓ RDWTarget cells in bld film, normal RDW
Serum ferritin↓Serum ferritin↑
IRBC↑IRBC↓
normal HbHb A2 By electrophoresis↑

1 α-gene
Normally we have 4 α- globin genes
All α-gene2 α-gene 3 α-gene
Silent
carrier
α-thalass.
traitHHD
Hb-H
α-thalas. major
”Hb barts
hydrops
fetalis”
α- thalassaemia
Asymptomatic

REFERENCES Illustrated textbook of pediatrics
www.Medscape.com
www.pubMed.com
www.Sehha.com