鶏肉からのサルモネラ属菌、大腸菌、 腸球菌の分離と薬剤耐性状 … · 鶏肉からのサルモネラ属菌、大腸菌、 腸球菌の分離と薬剤耐性状況(2)
中枢神经系统感染ccftp.scu.edu.cn/Download/20180905192435734.pdf病因 Mycobacteria...
Transcript of 中枢神经系统感染ccftp.scu.edu.cn/Download/20180905192435734.pdf病因 Mycobacteria...
概论 (1)
• Among the most common neurologic disorders (最常见)
• Most is amenable to treatment(可治)
• also,have a very high potential for causing catastrophic destruction of the CNS(后遗症)
Recognize early(早期发现)
概论 (2)
• Bacterial infection(细菌)Purulent Meningitis (Bacterial Meningitis)
• Tuberculous infection(结核)Tuberculous Meningitis
• viral infection(病毒)viral Meningitis (viral encephalitis )
• Mycobacteria(真菌) toxoplasma(弓形虫) spirochete(螺旋体)ameba(阿米巴) etc
概论 --- Purulent Meningitis (PM)
• PM is an infection caused by bacteria ,in which the membranes covering the CNS is mainly invovled(脑膜受累)
• PM occurs most frequently in winter & spring(冬春).
• PM is most commonly found in young children.(幼儿常见)
75% of cases occur in the age of <2yr (age 6 to 12 months)
• One of the most potentially serious infections, associated with high mortality (about 10%) and high neurologic sequelae (常见严重感染之一)
概论---Tuberculous Meningitis (TBM)
• TBM is an infection caused by the tuberculosis bacteria, in which the membranes covering the CNS is mainly invovled(脑膜受累)
• TBM is a type of severe TB, always be a part of systemic disseminated tuberculosis(全身感染的一部分), often occurs within 1 year of initial infection, especially in the first 3 to 6 months of infection. (感染1年内)
• TBM occurs in all age groups.(各年龄组)The younger the children, the more readily to develop TBM. (越小越易)60% in Children aged within 3 years(60%<3岁) .
• TBM is the most serious complication of tuberculosis in children and is usually fatal without treatment. Death rate: 15-30%(严重的儿童结核)
概论 --- viral encephalitis(VE)
• VE is an infection caused by virus ,in which the brain parenchyma is mainly invovled(脑实质受累)
• VE occurs most frequently in summer & autumn(夏秋). 70% of cases occur in Jun to Nov(6-11月).
• VE病情轻重及预后差异较大
病因
Mycobacteria Tubercolusis
结核杆菌
Meningitis Diplococcus *脑膜炎双球菌
Streptococcus Pneumoniae *肺炎链球菌
Haemophilus Influenza *流感嗜血杆菌
E. coli / 大肠杆菌
Group B Haemolytic Streptococcus B组溶血性链球菌
Staphylococcus Aureus 金黄色葡萄球菌
Enterovirus肠道病毒
Herpes simplex单纯疱疹病毒
Arbovirus虫媒病毒
(Epidemic type B encephalitisvirus
乙脑病毒)
Adenovirus腺病毒
Cytomegalovirus巨细胞包涵体病毒
etc
TBM PM VE
Major risk factors for meningitis易感因素
• Immature immunologic function免疫功能低下
• Immature blood-brain-barrier血脑屏障不完善 (BBB)
• Impaired blood-brain-barrier 脑脊膜膨出、颅脑手术、颅底骨折等
感染途径 Routes of infection to the meningites
• Blood-borne infection 血源性(major form)Bacteria Blood Meningites
B.B.B.eg: Respiratory tract infections (上感) / pneumonia(肺炎) , Skin lesion(皮肤损伤), Enteritis(肠炎)
• Infection of Adjacent tissue邻近感染扩散eg: Nose infection(鼻部感染), Ear infection(耳部感染)
• Injury of the skull 异常通道直接入侵
• 沿神经进入
病理 (2)
● 感染扩散至脑室内膜 脑室膜炎Ventriculitis
● 脑积水 hydrocephalus
脓液阻塞、粘粘及纤维化 Magendie’s foramen(正中孔、Luschka’s foramen(侧孔) 、 Sylvian aqueduct 阻塞
非交通性 Noncommunicating hydrocephalus
大脑表面或基底部蛛网膜粘连、萎缩 CSF回吸收障碍 交通性Communicating hydrocephalus
● 血管通透性增加、桥静脉栓塞性静脉炎 硬膜下积液 (积脓) subdural effusions
● 颅压增高、炎症的侵犯等 各种神经功 能障碍
临床表现
* Common manifestations全身症状
* CNS manifestationsCNS 症状
* Complications and sequelae manifestations并发症及后遗症症状
全身症状
TBM: toxic symptoms of tuberculous infection(结核感染中毒症状)
PM:acute infectious toxic symptoms(急性感染中毒症状)
VM: URI or injury of other organ symptoms(上感或其它脏器损伤症状)
CNS 症状
• meningeal irritation 脑膜刺激征nuchal rigidity(颈强直), kernig sign(克氏征), brudzinski sign(布氏征)
• increased intracranial pressure 颅压增高表现
headache, vomiting, herniation(脑疝)
• 脑实质损伤表现
Seizure(抽搐)
Alteration of mental status and consciousness(意识改变): irritability(激惹), lethargy(昏睡), stupor obtundation(迟钝), coma(昏迷)
local injury of parenchyma(局部脑实质损伤) etc
并发症及后遗症症状(自学)
• Subdural effusion (硬膜下积液)
• Ventriculitis(室管膜炎)
• Hydrocephalus(脑积水)
• Deafness(聋), blindness(盲), paralysis(瘫痪), epilepsy(癫痫), mental retardation(精神发育迟滞)etc
婴幼儿不典型表现
1. 体征不典型:Atypical miningeal irritation:Meninges irritation signs rarely occur (脑膜刺激征少见)
Intracranial hypertension: Frontal fontanelle projection (前囟隆起) and widening of cranial sutures in infant (颅缝增宽)
2. 症状表现不典型:
Febrile or low temperature(发热或体温不升) Lethargy(嗜睡) Irritable(易激
惹) Idly staring into space(目光呆滞) Vomiting(呕吐) Jaundice(黄疸)Cyanosis(发绀) Shock(休克) Irregular breath(呼吸不规则) Convulsion(惊厥) Coma(昏迷) etc.
结核典型三期
Stage 1: Prodrome(前驱期),约1~2周 ,早期主要症状:Mental status changes(性格行为改变);Focal neurologic signs are absentnonspecific symptom:Fever,fatigue(疲劳),malaise(不适),myalgia(肌
痛),drowsiness(思睡),headache, vomiting
Stage 2: Meningeal Irritation Stage(脑膜刺激期),约1~2周,中期appearance of definite neurologic signs(神经症状明显) : Meningeal Irritation Intracranial hypertension(颅内高压)
Cranial nerve abnormalities颅神经受累:面神经(其次是动眼神经、外展神经 )
signs More serious TB toxic symptoms(结核毒性症状)
Stage 3: Coma (昏迷期):约1~3周,晚期progressive abnormalities of vital signs, and eventual die from cerebral hernia (症状加重直至
脑疝)
Unresponsiveness/无反应,Opisthotonos/角弓反张 ,Decerebrate rigidity去大脑强直,Papilledema/视神经乳头水肿,Frequent convulsion(频繁惊厥)
实验室检查
• Blood (血): count, culture,etc• CSF(脑脊液):
Red and white blood cell count; protein concentration, glucose concentration;culture;serologic, immunologic, PCR detection(生化、常规、培养等)
• Brain biopsy(脑活检)(rarely)
CSF(脑脊液)
• CSF(脑脊液): 适应症与禁忌症
In the absence of focal neurologic deficits or signs of increased intracranial pressure, CSF should be obtained immediately from any patient in whom serious CNS infection is suspected.(一旦怀疑,立即腰穿)
.when papilledema or focal motor signs are present, a lumbar puncture may be delayed until a neruoimaging procedure has been done to exclude brain abscess or other space-occupying lesion (如有高颅压或局灶体征,先行影像检查)
高颅压:
ü视乳头水肿
ü高血压性心动过缓
ü瞳孔不等大
ü呼吸不规则
• 颅内出血
• 意识改变
• 新发癫痫
诊断--- 第一步
• Meningitis, Yes or Not?(是?否?)
任何发热,伴惊厥、意识障碍、颅压高或脑膜刺激征,而原因不明者,均应考虑此病,脑脊液检查是确诊的主要依据:
压力;白细胞数
诊断--- 第二步
• Meningitis, Which type? (哪种类型?)Purulent or Tuberculous or viral?
(1) 脑脊液检查是鉴别的主要手段:病原学证据非病原学证据:细胞数及分类,蛋白,糖,氯化物
as a general rule: CSF that contains a high proportion of polymorphonuclear leukocytes, a high protein concentration,
and a low glucose concentration strongly suggests bacterial infection.(高的多核细胞数及蛋白,低糖:提示细菌)
CSF containing predominantly lymphocytes, a high protein concentration, and a low glucose concentration strongly suggests infection with mycobacterial, fungi, uncommon bacterial .(淋巴分类为主,高蛋白,低糖:提示分支杆菌、真菌、不典型细菌)
CSF that contains a high proportion of lymphocytes, normal or only sligtly elevated protein concentration, and a normal glucose concentrations most suggestive of viral infection.(淋巴分类为主,正常或轻微增加的蛋白,糖正常:提示病毒)
(2)其它辅助证据
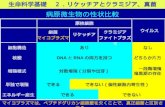
几种主要颅内疾病的脑脊液改变
脑脊液 压 力
(mmH2O) 外 观
白细胞数
(个/106)
Pandy试 验
蛋 白
(g/L)糖
(mmol/L) 其它改变
正 常 <180<1.76Kpa
清 <10 - 0.2 ~0.4 2.8~4.5 氯化物 110~120mmol/L
化脓性
脑膜炎
高 米汤样
数百~数万,多核为主
++ ~+++
明显增高 明显减少 涂片、培养可发现致病菌。氯化物可降低。
结核性脑膜炎
高或较高 毛玻璃
数十~数百,淋巴为主
+ ~+++
明显增高(通常1克以上)
减 少 薄膜涂片、培养可发现结核菌。氯化物可降低
病毒性脑、脑膜炎
正常或较高
清、或不太清
正常~数百,淋巴为主
±~++ 正常或稍增加
正常 特异性抗体增高,可分离出病毒
隐球菌性脑膜炎
高 不太清
数十~数百,淋巴为主
+ ~+++
增多 (通常1克以上)
减 少 墨汁涂片、真菌培养可发现真菌。氯化物可降低。
感染中毒性脑病
正常或稍高
清 正 常 — 或+ 正常或稍高
正 常
Treatment 治疗
• General Therapy 一般治疗
• Etiology Therapy 病因治疗
• Symptom Therapy 对症治疗
• Complications Therapy并发症治疗 (自学)
• Rehabilitation Therapy 康复治疗(后期) (自学)
病因治疗
• Therapy principles治疗原则:
early treatment早期, enough dose足量, enough course足疗程
• 化脑:抗生素治疗
• 结脑:抗结核治疗
• 病脑:抗病毒治疗
病因治疗 ---PM
• 抗生素治疗的疗程
流感嗜血杆菌脑膜炎和肺炎链球菌脑膜炎治疗不少于2~3周
大肠杆菌和金黄色葡萄球菌脑膜炎疗程应达3~4周以上
脑膜炎双球菌7-10天
如出现并发症或耐药,要酌情更换抗生素和延长疗程
症状消失,热退1周以上,脑脊液完全恢复正常
病因治疗 ---TBM
• 强化治疗阶段:3HRZS(E)or 4HRZS(E)INH(异烟肼)15-25mg/kg、 RFP (利福平)10-15mg/kg(<450mg/d)PZA (吡嗪酰胺)20-30 mg/kg(<750mg/d) 、SM (链霉素) 15-20 mg/kg(<750mg/d) 开始1~2周内,INH半量静脉使用,半量口服,病情好转全量口服
• 巩固治疗阶段:继用INH和RFP(EMB)INH:总1~2年 RFP:总9~12个月总疗程不少于12月,or CSF正常后继续6月
• DOTS方案 : 3HRZS/6HR 早期患者的短程方案
对症治疗--激素
• 能够控制炎症,减少渗出,降低颅内压,减少粘连,利
于脑脊液循环
• 结脑: 泼尼松,每日1~2mg/kg(小于30~45mg/d)1个月后减量,疗程8~12周
• 化脑:静注地塞米松,每日0.2~0.6mg/kg,共3~5天
• 病脑:视病情而定
预后相关因素
• treatment is begun治疗开始时间
• The stage of disease at which 治疗是否正确
• The age of the patient发病年龄
• 感染病原
• 并发症有无 …
常见神经后遗症
• developing retardation / 发育迟缓
• cranial nerve palsies / 颅神经瘫痪
• hydrocephalus / 脑积水
• optic atrophy / 视神经萎缩
• deafness / 耳聋
• palsies / 瘫痪
• coma / 昏迷
• convulsion / 惊厥,抽搐
• pituitary disturbances / 垂体功能紊乱