Bone scan
-
Upload
sitanshubarik -
Category
Health & Medicine
-
view
2.054 -
download
0
Transcript of Bone scan

Bone Scintigraphy

Bone Scanning
• Bone scintigraphy is a diagnostic study used to evaluate the distribution of active bone formation in the body.
• Phosphate analogues can be labeled with 99mTc and are used for bone imaging because of their good localization in the skeleton and rapid clearance from soft tissues.

• It can be performed as:– a) Limited bone scintigraphy or spot views
(planar images of a selected portion of the skeleton)
– b) Whole-body bone scintigraphy (planar images of the entire skeleton in anterior and posterior views)
– c) SPECT (single photon emission computed tomography- image of a portion of the skeleton)
– d) Multiphase bone scintigraphy (immediate and delayed images to study blood flow)

• In oncology the standard technique of bone scintigraphy is considered to be the whole-body scan.
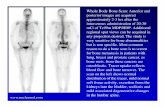
• Whole-body bone scintigraphy produces planar images of the skeleton, including anterior and posterior views of the axial skeleton.
• Anterior and/ or posterior views of the appendicular skeleton also are obtained.
• Additional views are obtained as needed.

• Limited bone scintigraphy or spot views are indicated only where a specific clinical problem detected on whole-body imaging needs to be clarified.
• SPECT has a higher diagnostic specificity than planar imaging and may be preferable when there is diagnostic uncertainty.
• Multiphase bone scintigraphy is more useful when trauma or musculoskeletal inflammation/infection is suspected and is not usually indicated in oncology.

• Multiphase bone scintigraphy usually includes blood flow images, immediate images, and delayed images.
• The blood flow images are a dynamic sequence of planar images of the area of greatest interest obtained as the tracer is injected.
• The immediate (blood pool or soft tissue phase) images include 1 or more static planar images of the areas of interest, obtained immediately after the flow portion of the study and completed within 10 min after injection of the tracer.

• Delayed images may be limited to the areas of interest or may include the whole body, may be planar or tomographic, and are usually acquired 2–5 hrs after injection.
• If necessary, additional delayed images may be obtained up to 24 h after tracer injection.

Clinical indicationsOncological indications• Primary tumours (e.g. Ewing’s sarcoma,
osteosarcoma)• Staging, evaluation of response to therapy and
follow up of primary bone tumors• Secondary tumours (metastases)
– Staging and follow-up of neoplastic diseases– Distribution of osteoblastic activity prior to
radiometabolic therapy

Indications for non-neoplastic diseases:• Bone scan changes occur whenever there is an
increase in blood flow to a lesion or there is an alteration in osteoblastic activity. For this reason, bone scan images also reveal abnormalities in non-neoplastic diseases such as:– Stress and/or occult fractures.– Trauma – accidental and nonaccidental.– Musculoskeletal inflammation and infection– Bone viability (grafts, infarcts, osteonecrosis).– Metabolic bone disease.– Arthritides

– Complications of hardware/prosthetic joint replacement, loose or infected joint prosthesis
– Pain of suspected musculoskeletal etiology.– Heterotopic ossification.– Complex regional pain syndrome (CRPS)– Spondylolysis– Abnormal radiographic, lab or clinical findings.– Distribution of osteoblastic activity prior to
radiopharmaceutical administration for palliation of bone pain.
– Other bone disease, such as Paget disease, Langerhans cell histiocytosis, or fibrous dysplasia.
– Congenital or developmental anomalies.

Contraindications
• Pt. recently had contrast media for a different study.
• Pt. Recently (24-48 hrs) had a TC99m-based nuclear scan

• patients should be well hydrated and instructed to drink 2 or more glasses of water between the time of injection and the time of delayed imaging.
• The patient should be asked to urinate immediately before delayed imaging and to drink plenty of fluids for at least 24 h after radiopharmaceutical administration.

• Technetium-99m medronate (methylene diphosphonate [MDP]),
• technetium-99m oxidronate (hydroxymethylene diphosphonate [HMDP]),
• or hydroxyethylene diphosphonate (HDP) is administered intravenously.

Precautions• Pregnancy (suspected or confirmed). In the
case of a diagnostic procedure in a patient who is known or suspected to be pregnant, a clinical decision is necessary to weigh the benefits against the possible harm of carrying out any procedure.
• Breast-feeding should be discontinued and milk expressed and discarded when possible for 24 h (and atleast for 4 h) post radiopharmaceutical administration).

Physiology• Phosphonates concentrate in the mineral phase
of bone: nearly two-thirds in hydroxyapatite crystals and one third in calcium phosphate.
• Two major factors control accumulation of phosphonates in bone, namely blood flow and extraction efficiency, which in turn depend on capillary permeability, acid-base balance, parathyroid hormone levels, etc.
• About 50% of the activity injected accumulates in the skeleton.

• Maximum bone accumulation is reached 1 h after injection and the level remains practically constant up to 72 h.
• The blood clearance of these radiopharmaceuticals is high. Three hours after injection only 3% of the administered activity remains in the bloodstream.
• The peak of activity through the kidneys is reached after approximately 20 min. Within 1 h, with normal renal function, more than 30% of the unbound complex has undergone glomerular filtration andwithin 6 h, 60%.

• The quantity of phosphonates eliminated via the intestines is insignificant.
• The biological half-life of phosphonates is 26 h.• In a normal bone scan all but the smallest bones
are recognisable. • On the anterior view it is possible to distinguish
the sternum.

• On the posterior view the bodies of individual vertebrae are seen, as well as pedicles and transverse and spinous processes in the lower dorsal and lumbar regions. In this projection the sacro-iliac joints usually have the highest uptake.
• In children the appearance of the bone scan is characterised by areas of uptake due to active growth in the epiphyseal regions.
• After fusion of the epiphyses these areas are no longer visible.

• When evaluating bone scan images, the following points should be taken into consideration:– The bone scan is very sensitive for localisation of
skeletal metastases or tumours, but the specificity is low. It must be interpreted in the light of all available information, especially patient history, physical examination, other test results and previous studies.
– Symmetry in the representation of right and left sides of the skeleton and homogeneity of tracer uptake within bone structures are important normal features. Particular attention should be paid to left–right asymmetries and/or heterogeneity of tracer uptake.

Bone abnormalities
• Both increases and decreases in tracer uptake have to be assessed; abnormalities can be either focal or diffuse.
• Increased (decreased) tracer activity in the bone, compared with that in normal bone, indicates increased (decreased) osteoblastic activity.

• Differential diagnosis can sometimes be based on the configuration of the abnormality or abnormalities and the location and number of abnormalities. Most patterns are non-specific.
• Focal decrease without adjacent increase in tracer uptake is less common than focally increased activity and is often caused by benign conditions (attenuation, artefact or absence of bone, e.g. due to surgical resection).

• Decreases in the intensity of tracer uptake and in the number of abnormalities compared with a previous study often indicate improvement or may occur secondary to focal therapy (e.g. radiation therapy).
• Increases in the intensity of tracer uptake and in the number of abnormalities compared with a previous study often indicate progression of disease but may reflect a flare response to therapy.

Soft tissue findings• Normal structures should be noted: kidneys and
bladder. Tracer uptake in the kidney can be focal or diffuse.
• Generalised increased soft tissue uptake compared with normal bone can be due to renal failure, dehydration or a shortened interval between injection and imaging.
• A generalised decreased soft tissue uptake compared with normal bone can be due to “superscan” or a prolonged interval between injection and imaging.

Normal Bone Scan• tracer uptake greatest in axial
skeleton• background activity of soft tissue• kidneys routinely visualized• skull can appear uneven
(variations in calvarial thickness)• sites of persistently increased
symmetric uptake, are acromial and coracoid processes of the scapulae, the medial ends of the clavicles, the junction of the body and manubrium of the sternum and the sacral alae

Normal Bone Scan• Hyperostosis Frontalis
• Dental Problems
Common Cold

Normal Bone Scan-Pediatrics· Growth Center
most intense: distal femur-proximal tibia-proximal humerus (which is also the order of relative occurence of osteosarcoma in children)
Costochondral junctions

Additional Views
Tail On Detector-TOD

SPECT

Metastatic Bone Disease
Prostate Cancer

• The presence of multiple, randomly distributed areas of increased uptake of varying size, shape, and intensity is highly suggestive of bone metastases
• Though encountered in other pathologic conditions, it is often possible to distinguish metastatic disease from other entities by analyzing the pattern of distribution of the abnormalities.
• Metastatic disease occasionally manifests as a solitary abnormality, usually in the spine like in degenerative d/s. SPECT is useful for differentiating these two

Metastatic Bone Disease ?• Multiple Fractures• Radiotracer
accumulation in both the vertebral body and pedicles usually indicates metastatic disease, whereas abnormalities that involve the vertebral body and facets but spare the pedicles are usually benign• Activity that is confined
to the vertebral body can be due to tumor, trauma, or infection



Metastatic Bone Disease

Flare Phenomenon
Usually occurs 3-6 months post chemotherapy

Flare phenomenon• seen in patients who are responding to treatment,
reflects healing of the bone lesions and has been described as the “flare” phenomenon.
• This phenomenon is usually observed within 3 months after initiation of treatment and is often associated radiographically with the sclerotic changes that indicate healing.
• Continued increase in the number and intensity of lesions beyond 6 months is usually indicative of disease progression


Superscan• When the metastatic process is
diffuse, virtually all of the radiotracer is concentrated in the skeleton, with little or no activity in the soft tissues or urinary tract. The resulting pattern, which is characterized by excellent bone detail, is frequently referred to as a superscan• A superscan may also be associated
with metabolic bone disease. Unlike in metastatic disease, however, the uptake in metabolic bone disease is more uniform in appearance and extends into the distal appendicular skeleton.

Hypertrophic Osteoarthropathy
• linear tracer uptake along the femurs, tibias, and distal upper extremitis (black arrows) • nonuniform, irregular
cortical uptake involving the long bones and giving rise to the “tramline sign”

Osteosarcoma

Ewing Sarcoma

Multiple Myeloma
• lytic bone lesions (bone formation is markedly suppressed or absent)
• unless associated fracture present bone scan often normal

Benign Bone Tumors
• Osteoid Osteoma (and osteoblastoma)• Enchondroma • Osteochondroma• Chondroblastoma

Osteoid Osteoma– “double density” sign

Enchondroma• typically only mildly increased uptake
unless secondary fractures occur

Osteochondroma• uptake on bone scan varies

Chondroblastoma• uptake on bone scan varies

Skeletal Trauma
• 95% visualized by day 3, maximum positivity by day 7 (age<65 y)
• advanced age, debilitation can cause delayed or non-visualization
• return to normal depends:– location and degree of damage– age of patient
• patients age<65y: 60-80% of non-displaced fx revert to normal in 1 year, 95% by 3 y)
• patients >65 year can remain positive



Stress Fractures
• radiograph can be negative• occurs in normal bone that undergoes abnormal
stress (insufficiency fractures occur with normal stress in bones that are weakened)
• most common sites are the femoral neck and tibia. • typical pattern is oval area of increased uptake with
long axis parallel to axis of bone


Shin Splints (Periostitis)
• exercise induced pain along medial or posteromedial aspect of tibia
• associated with increased tracer uptake• >1/3 of bone length • middle to distal tibia• usually bilateral (not necessarily symmetrical)• microperiosteal tears (via Sharpey’s fibers)• positive finding does not predict further injury

• Hyperperfusion and hyperemia are typically present in acute stress fracture.
• Unlike in stress fractures, angiograms and blood pool images are usually normal in shin splints. Delayed bone images reveal longitudinally oriented linear areas of increased uptake of varying intensity that involve one-third or more of the posterior tibial cortex


Bone Infarction/AVN • appearance depends on time course
– In the acute phase of vascular compromise, no radiotracer is delivered to the bone tissue. At scintigraphy, the affected part of the bone appears as a photopenic defect.
– After revascularization, exuberant osteoblastic repair manifests as intense radiotracer uptake.
–Subsequently, when repair is complete, radiotracer uptake may return to baseline levels
• less sensitive than MRI

Legg-Calve-Perthes
• early imaging photon deficient lesion
• increased activity with healing (for months)

Osteomyelitis
• increased tracer uptake – (except occasionally in children paradoxically
decreased secondary to increased pressure in marrow space)
• skeletal scintigram for whole body survey• MRI very sensitive, but limited as survey
tool• A combination of focal hyperperfusion,
focal hyperemia, and focally increased bone uptake is virtually diagnostic for osteomyelitis

Osteomyelitis vs Cellulitis• MRI of limited value in the diabetic foot• three phase bone scan for differentiation of
cellulitis vs OM• non specific-similar pattern in:
–neuropathic joint–gout– acute fractures–healing osteonecrosis–RSD

• The first (dynamic) phase reflects the relative amount of blood flow to the area of interest, whereas the second (blood pool) phase reflects the amount of activity that has extravasated into the tissues around the area of interest. The third (delayed [bone]) phase reflects the rate of bone turnover.
• The classic appearance of osteomyelitis on three-phase bone scans consists of focal hyperperfusion, focal hyperemia, and focally increased bone uptake


Plantar fascitis

Reflex Sympathetic Dystrophy (complex
regional pain syndrome)diffuse, uniformly increased uptake throughout the affectedregion

Prosthesis-Loosening vs Infection
• increased uptake normal after surgery–~1y w/ cemented, ~2-3y w/ non-cemented
• start w/ bone scan if negative no infection or loosening
• if positive and unclear whether loosening or infection consider Tc-HMPAO-WBC scan to differentiate Infection from loosening
l

loosening Infection

Bone Dysplasias
• Paget’s Disease– accelerated rate of bone turnover– excessive resorption and formation of bone– intensely increased activity throughout the
involvedbones– most common: pelvis
• Others – fibrous dysplasia– Osteognesis imperfecta– Osteopetrosis– Melorheostosis


Heterotopic ossification

Sources of error• – Patient movement• – Greater than necessary collimator-to-patient
distance• – Imaging too soon after injection, before the
radiopharmaceutical has been optimally cleared from soft tissues
• – Injection artefacts• – Radiopharmaceutical degradation• – Urine contamination or a urinary diversion
reservoir

• – Prosthetic implants, radiographic contrast materials or other attenuating artefacts which may obscure normal structures
• – Homogeneously increased bony activity (e.g. “super-scan”)
• – Restraint artefacts caused by soft-tissue compression
• – Prior administration of a higher energy radionuclide (131I, 67Ga, 111In) or of a 99mTc radiopharmaceutical which accumulates in an organ that could obscure or confound skeletal activity

• – Significant findings outside the area of interest may be missed if a limited study is performed
• – Changing bladder activity during SPET of the pelvic region
• – Purely lytic lesions• – Pubic lesions obscured by underlying
bladder activity• – Renal failure