Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
-
Upload
ronel-usita -
Category
Documents
-
view
216 -
download
0
Transcript of Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
1/29
Bone Plating in Patients with Type III Osteogenesis Imperfecta:Results and ComplicationsWilliam J Enright, MD andKenneth J Noonan, MD
Author informationCopyright and License information
This article has beencited byother articles in PMC.
Go to:
Abstract
The results of bone plating in four children (6 femurs, 2 tibias) with osteogenesis imperfecta type III were
analyzed. Average age at time of operation was 44 months. In three of the femurs, multiple platings were
performed for a total of 13 bone platings in the eight bones studied. Average time to revision following plating
was 27 months. Indications for revision included fracture (6), deformity (3), hardware failure (3), and
nonunion (1). Other complications included one case of compartment syndrome. All eight bones wereultimately revised to elongating intramedullary Bailey-Dubow rods. Bone plating in skeletally immature
patients with osteogenesis imperfecta does not provide better outcome than elongating rods. Complications
from bone plating leading to revision, such as refracture or hardware failure, are higher than in those children
managed with elongating rods, as previously reported in the literature.
Go to:
INTRODUCTION
Osteogenesis imperfecta (OI) is a group of inherited disorders caused by defective type I collagen synthesis.
Using the Sillence classification, one can determine the type of OI based on clinical, radiographic, and genetic
findings.13Patients with OI can suffer from frequent fractures and deformity of the long bones during
development, resulting in impaired ambulation. The goal of orthopedic surgery for OI is twofold: Reduce theincidence of fractures and correct long bone deformity. Contemporary surgical options for deformed bones in
OI include osteotomy and stabilization with non-elongating nails (Rush rods, flexible nails), elongating nails
(Bailey- Dubow, Frasier-Duval), and bone plating.14,7,8,10,14,15Elongating rods allow for growth of the bone,
thereby decreasing the number of repeat operations. The advantages of elongating rods over fixed
intramedullary rods include benefit to growing bones, lower incidence of re-fracture, and longer time to re-
operation.4,5,11,12There is also evidence that suggests that elongating rods used in the femur do not require
revision as often as those placed in the tibia.16
At our institution, we have utilized plate fixation for stabilization of osteotomies in young patients with severe
OI. Plate fixation was initially appealing in this group of patients given the age of the individuals and the
difficulty of placing expandable rods in small bones. In addition, the treating surgeon felt that these rods were
too large for the smallest children, thus resulting in stress shielding and bone atrophy. The purpose of thisstudy is to review our experience in this small but select group of patients.
Go to:
MATERIALS AND METHODS
This study is a retrospective review of all patients with osteogenesis type III treated with bone plating for
correction of deformity or treatment of fracture. All operations were performed by the same pediatric
http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Enright%2BWJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Enright%2BWJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Noonan%2BKJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Noonan%2BKJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Noonan%2BKJ%5bauth%5dhttp://void%280%29/http://void%280%29/http://void%280%29/http://void%280%29/http://void%280%29/http://void%280%29/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/citedby/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/citedby/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/citedby/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/14065693http://www.ncbi.nlm.nih.gov/pubmed/14065693http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R14http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R14http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R11http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R11http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R11http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R14http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pubmed/14065693http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/citedby/http://void%280%29/http://void%280%29/http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Noonan%2BKJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Enright%2BWJ%5bauth%5d -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
2/29
orthopedic surgeon between 1994 and 2001. Inclusion criteria for this study were a diagnosis of type III
osteogenesis imperfecta, history of bone plating, and recent clinical follow-up.
After review of the medical files of all patients treated for osteogenesis imperfecta at the University of
Wisconsin Hospital and Clinics, we were able to find four patients who had undergone at least one bone plating
as treatment for fracture or deformity. Clinical records and imaging studies were reviewed. We recorded the
indications for initial plating, types of plates and screws used, time to evidence of healing on radiograph, timeto revision, indications for revisions, hardware used in revision (plate or rod), number and location of fractures
following each plating, complications including hardware failure, and number of revisions for each bone.
Regarding the measurement of time to fracture and time to revision, the authors considered each plating
separately. There were cases of sequential platings of the same bone in patients where initial plating was
revised with further plating. Initial plating was considered as the start point for this study, and revision with
expandable rods was considered the end point.
Go to:
RESULTS
All four patients were diagnosed with osteogenesis type III using the Sillence classification.13There were three
males and one female, ranging in age from 14 to 82 months (44.7 months mean age) at the time of surgery.Ages ranged from five to eight years (7.7 years mean age) at last follow-up. The average time from initial plating
to final follow-up period was four years.
Thirteen bone platings were performed on eight bones. The eight bones included six femurs and two tibias.
Three of the femurs underwent multiple platings before being ultimately revised to Bailey-Dubow rods. Of
these three femurs, two were plated twice, and one femur was plated four times for a total of 13 platings. All
platings were separate operations. No two bones were plated at the same time. The indications for initial
plating of the eight bones included fracture and deformity. Of the six femurs, four were plated because of
fracture, and two were plated for correction of deformity. Of the two tibias, one was plated for correction of
deformity and the other because of fracture.
All eight bones ultimately required revision. Three of the femurs underwent further plating for revision, whilethe two tibias and three other femurs were revised to Bailey-Dubow rods. Indications for revision included
fracture (6), deformity (3), hardware failure (3), and nonunion (1). Rate of fracture following plating was 46%
(six fractures). Location of fracture was distal to the plate in two cases, under the plate in two cases, and
through the plate in two cases. In the two cases of fracture through the plate, fracture of bone with broken plate
was considered the reason for revision and also considered a complication (Figures 1andand2).2). The average
time to revision was 27 months (range 4 to 71 months). The average time from initial plating to final revision
with Bailey-Dubow rods was 42 months (range 9 to 89 months) for all bones.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2 -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
3/29
Figure 2
Radiograph showing screw pull-out. Note the proximal and distal cancellous screws have pulled out, allowingthe plate to displace from the bone and leading to hardware prominence.
The complication rate in these patients was 69.2% (9 plates). The most common complication following plating
was screw pull-out. Screw pull-out was seen following plating in five cases. One case involved multiple screws
and required revision for stabilization. Two fractures through the plate were seen, and these underwent
revision. Bending of two of the plates was observed. Of these nine complications, three instances of hardware
failure led to revision: Screw pull-out required revision in one case, and two fractures went through the plate as
mentioned above. Complications are listed inTable 1.
TABLE 1
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/table/T1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F2/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/figure/F1/ -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
4/29
There was one case of compartment syndrome following plating of a tibia, which required fasciotomy. There
was one case of nonunion in a femur. This nonunion was noted five months after the initial plating and was
revised with bone plating seven months after the initial operation. There were three instances of prominent
hardware, one of which was symptomatic.
Go to:
DISCUSSION
Bone plating is an option in the treatment of fracture and deformity in children with osteogenesis imperfecta.
Previous studies in the orthopedic literature report treatment of these patients with intramedullary rods, both
fixed and elongating. The benefits of elongating rods over fixed rods have been demonstrated in regard to
reduction in the number of operations performed and facilitation of growth.4,5,12There are no studies, however,
examining the results of bone plating in comparison to the results obtained with elongating intramedullary
rods.
The purpose of this study was to examine the results of bone plating in patients with osteogenesis imperfecta.
Average time to revision following plating was 27 months. This compares quite unfavorably with the five years
to revision following placement of Bailey-Dubow rods reported by Luhmann et al.9It compares more favorably
with the average time to revision of 2.5 years following placement of non-elongating rods reported by Marafioti
and Westin.10The most common indication for revision following plating was fracture (6), followed by
deformity (3) and hardware failure (3).
The complication rate of plating was 69.2%. This rate was slightly higher than the 63.5% complication rate
previously reported by Jerosch et al. and significantly higher than the 27% complication rate reported by
Marafioti and Westin in their treatment of patients with OI.6,10Jerosch et al. implanted Bailey-Dubow rods in
107 bones and Kirschner wires in eight bones.6In their study, the Kirschner wires were implemented because
of small bone diameter. The most common complication of Bailey-Dubow rods has been reported to be rod
migration.6,7The most common complication seen after plating was screw pull-out. This seems intuitive given
the quality of bone in patients with osteogenesis imperfecta. Not only does the bone quality not allow for
purchase of the screws, the bowing of bones may act to further any screw pull-out. Screw pull-out was not a
clinical problem in this series unless it was associated with increasing deformity or fracture.
The treatment plan for skeletally immature patients with osteogenesis imperfecta must include consideration ofgrowth. The advantage of the elongating rod is that it allows for longitudinal bone growth. The rod does cross
the physis, but the diameter of the rod is small enough not to affect growth.2Bone plating does not disturb the
physis in most cases, but it does not migrate with growth, thus leaving unsupported bone. Higher revision and
failure rates in the bone adjacent to the plate are also most likely due to the sharp disparity in construct rigidity
and osteopenic metaphyseal bone.
Considering the higher complication rates, shorter length of time to revision, and unknown effect on
longitudinal growth, bone plating does not compare favorably to elongating rods in patients with osteogenesis
imperfecta. We recommend elongating rods when considering treatment of deformity or fracture in patients
with osteogenesis imperfecta.
Go to:
Footnotes
Study conducted at University of Wisconsin Hospital and Clinics, Madison, WI
Go to:
References
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R9http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R9http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R6http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R9http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#R4http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1888596/#ui-ncbiinpagenav-2 -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
5/29
1. Bailey RW. Studies of longitudinal bone growth resulting in an extensible nail. Surg Forum.1963;14:455
458. [PubMed]
2. Bailey RW. Further clinical experience with the extensible nail. Clin Orthop. 1981;159:171176.[PubMed]
3. Bailey RW, Dubow HI. Evolution of. the concept of an extensible nail accommodating to normal longitudinal
bone growth: clinical considerations and implications. Clin Orthop. 1981;159:157170.[PubMed]
4. Gamble JG, Strudwick WJ, Rinsky LA, Bleck EE. Complications of intramedullary rods in osteogenesis
imperfecta: Bailey-Dubow rods versus nonelongating rods. J Pediatric Ortho.1988;8(6):645649.
5. Harrison WJ, Rankin KC. Osteogenesis imperfecta in Zimbabwe: a comparison between treatment with
intramedullary rods of fixed-length and self-expanding rods. J Royal College Surg Edinburgh.1998;43(5):328
332.
6. Jerosch J, Mazzotti I, Tomasevic M. Complications after treatment of patients with osteogenesis imperfecta
with a Bailey-Dubow rod. Archives Ortho & Trauma Surg. 1998;117(4-5):240245.
7. Lang-Stevenson AI, Sharrard WJ. Intramedullary rodding with Bailey-Dubow extensible rods in osteogenesis
imperfecta: an interim report of results and complications. J Bone Joint Surg Br. 1984;66-B(2):227232. [PubMed]
8. Li YH, Chow W, Leong JC. The Sofield-Millar operation in osteogenesis imperfecta: a modified technique. J
Bone Joint Surg Br. 2000;82-B(1):1116. [PubMed]
9. Luhmann SJ, Sheridan JJ, Capelli AM, Schoenecker PL. Management of lower extremity deformities in
osteogenesis imperfecta with extensible intramedullary rod technique: a 20-year experience. J Pediatric
Ortho. 1998;18(1):8894.
10. Marafioti RL, Westin GW. Elongating intramedullary rods in the treatment of osteogenesis imperfecta. J
Bone Joint Surg Am. 1977;59A(4):467472. [PubMed]
11. Mulpuri K, Joseph B. Intramedullary rodding in osteogenesis imperfecta. J Pediatric
Ortho.2000;20(2):267273.
12. Porat S, Heller E, Seidman DS, Meyer S. Functional results of operation in osteogenesis imperfecta:
elongating and nonelongating rods. J Pediatric Ortho. 1991;11(2):200203.
13. Sillence D. Osteogenesis imperfecta: an expanding panorama of variants. Clin Orthop. 1982;159:11
25. [PubMed]
14. Sofield HA, Millar EA. Fragmentation, realignment, and intramedullary rod fixation of deformities of the
long bones in children. J Bone Joint Surg. 1959;41A:1371.
15. Stockley I, Bell MJ, Sharrard WJ. The role of expanding intramedullary rods in osteogenesis imperfecta. J
Bone Joint Surg Br. 1989;71-B(3):422427. [PubMed]
16. Zionts LE, Ebramzadeh E, Stott NS. Complications in the use of the Bailey-Dubow extensible nail.Clin
Orthop. 1998;348:186195. [PubMed]
http://www.ncbi.nlm.nih.gov/pubmed/14065693http://www.ncbi.nlm.nih.gov/pubmed/14065693http://www.ncbi.nlm.nih.gov/pubmed/14065693http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pubmed/7285454http://www.ncbi.nlm.nih.gov/pubmed/7285454http://www.ncbi.nlm.nih.gov/pubmed/7285454http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pubmed/9553552http://www.ncbi.nlm.nih.gov/pubmed/2656718http://www.ncbi.nlm.nih.gov/pubmed/7285446http://www.ncbi.nlm.nih.gov/pubmed/863940http://www.ncbi.nlm.nih.gov/pubmed/10697308http://www.ncbi.nlm.nih.gov/pubmed/6368564http://www.ncbi.nlm.nih.gov/pubmed/7285454http://www.ncbi.nlm.nih.gov/pubmed/7285455http://www.ncbi.nlm.nih.gov/pubmed/14065693 -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
6/29
Management Of Femur Fractures With Self-Made Polymethylmethacrylate Plates, Stainless
Steel Plates, Intra-Medullar Pins And Interlocking Nails In Dogs
P. Mukherjee1, D. Ghosh1, S. Roy1 and S. Basu2
West Bengal University of Animal and Fishery Sciences,37, K. B. Sarani, Kolkata-700 037, India.
1. Department of Veterinary Surgery & Radiology.
2 Department of Veterinary Gynaecology and Obstetrics.
Corresponding author
Dr. Prasenjit Mukherjee
Senior Research Fellow
Department of Veterinary Surgery and Radiology
West Bengal University of Animal and Fishery Sciences,
Kolkata- 700 037, India.
SUMMARY
This is a retrospective study of 24 femur diaphyseal transverse fractures stabilized with intra-medullar pinning, steel bone plating,
fabricated polymethylmethacrylate (PMMA) plates and intra-medullar interlocking nailing (ILN). Four groups, each including 6
animals, were followed-up for 9 weeks in the perspective of postoperative complications and fracture healing. Routine physical
examinations assessed limb function, joint involvement and condition of the operative site. Serum calc ium and phosphorus showed
no significant change. Full limb function was obtained quicker using fabricated PMMA plates, followed, in the order, by ILN, steel
bone plating and intra-medullar pinning. Fabricated PMMA and steel bone plates showed earlier radiographic disappearance of
fracture lines and earlier formation of direct bridging callus. The use of fabricated PMMA plates showed promising results for the
management of the femur transverse fracture in dogs considering the advantages of lower cost, easy fabrication and actual
adaptation to the specific contour of the bone.
Key Words: Bone Plating, Canine, Femur Fracture, Intra-Medullar Interlocking Nailing, Intra-Medullar Pinning,
Polymethylmethacrylate Plate.
INTRODUCTION
Among the long bones, the incidence of femur fractures is highest (45.87%) (Gahold et al, 2002) mostly seen in diaphysis and
distal metaphysis (Roy et al, 2005). Internal fixation provides mechanical stability to a fractured bone, allowing weight bearing,
early use of the limb and rapid healing. The selection of internal fixation is based on mechanical, biologic and clinical parameters
associated with each patient and fracture, not just the fracture pattern itself (Aron et al, 1995). Intra-medullar pinning is most
widely used because provides axial alignment and resists bending forces but not the shear and rotational forces (Vasseur et al,
1984). Less surgical exposure and dissection is needed to place intra-medullar interlocking nails compared to placement of bone
plates. Therefore, the use of intra-medullar inter locking nail may result in preservation of more periosteal vascularity (Heitemeyer
et al, 1990), promoting biological osteosynthesis (Reems et al, 2003). Bone plating resists tension, compression, shearing and
rotational forces, and depending upon their placement resist bending forces. However, it is a more traumatic procedure (Stiffler,
2004), and demands extreme professional skills to achieve dynamic compression. The present study was carried out t o assess the
feasibility of using bone plates which contributes to dynamic compression but devoid of some complications like accurate proficiency
in contouring plate with bone interface, as well as easy affordability. To this purpose we adopted an extremely versatile
thermoplastic polymeric material, polymethylmethacrylate (PMMA), firstly introduced by Charnley (1960), used for decades as
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
7/29
"filler" material in total-hip insertion and recently for internal fracture-fixation plates, to more evenly distribute forces over the
plate-bone interface, thereby combating premature plate failure (Moursi et al, 2002).
MATERIAL AND METHODS
Aims
To evaluate the efficacy of fabricated polymethylmethacrylate (PMMA) plating as a method of internal fixation in canine diaphyseal
femur fractures and to compare it with ILN, intra-medullar pinning and steel plating in view of bone healing and complications.
Study design
The study was conducted on twenty four (24) clinical cases of femur diaphyseal transverse fractures in dogs between the age group
2-5 years of either sex. The cases were randomly divided in to four groups and treated with four internal fixation devices (Gr. A-
Intramedullary pinning; Gr. B- Bone Plating; Gr. C- Bone plating with fabricated PMMA plates and Gr. D- Intramedullary
Interlocking nailing) comprising six animals in each group. Each animal of different groups were subjected to physical (condition of
the operative site, assessment of full limb function, affection of joint as per the method described by Branden and Brinker, 1973)
(Table I) and radiological examinations (14 mAs; 50Kvp and 90 cm FFD) throughout the study period. The decision for adopting any
one of the internal fixation technique following the standard procedures (DeYoung and Probst, 1985; Conzemius and Swainson,
1999 and Raghunath and Singh, 2002) was randomly adopted.
Fabrication of polymethylmethacrylate (PMMA) bone plate
For fabrication of PMMA plates of appropriate thickness, two parts polymer of methylmethacrylate powder was mixed with one part
of liquid monomer methylmethacrylate . Different s izes of femur from canine cadaver of different body weights were taken as
negative cast. Then the PMMA was applied over the lateral side of the femur to achieve 6-8 mm thickness and kept t ill drying as a
cast. The plates then were removed and grounded with sand paper into desired shape and finish and drilled with 3.5 mm drill bit to
make six hole plates of different sizes (Fig. 1). Sterilization of fabricated plate was achieved by autoclaving. At the time of surgical
intervention, different plates were taken corresponding to the size and body weight similar to patient under the study.
Table: I. Clinical evaluation of functional limb usage
Grade Limb use
description
Definition
I Nonuse No functional use of the limb;
carries the limb most of the time.
II Slight use Some functional use; will set limb
down to stand or walk; carries limb
when running; does not bear weight
on limb.
III Limp Functional use of limb; partial
weight bearing.
IV Normal Full function for standing, walking,
running; full weight bearing.
Anaesthesia preoperative preparation and surgical procedure
The dogs were pre-anaesthetized with subcutaneous injection of atropine sulphate @ 0.04 mg/kg body weight 15 minutes before
the administration of injection xylazine hydrochloride @ 1 mg/kg body weight intramuscularly. After proper sedation, the dogs were
placed to the operation table and operation was performed with intraoperative administration of injection ketamine hydrochloride
@10 mg/ kg body weight and injection diazepam @ 0.5 mg/ kg body weight intravenously for maintenance of anaesthesia.
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
8/29
Preoperatively, operative site was aseptically prepared with routine application of antiseptic solution, scrubbing and painting.
Anesthesia was performed using atropine sulphate (0.04 mg/kg), xylazine hydrochloride (1 mg/kg), ketamine hydrochloride (10
mg/ kg) and diazepam (0.5 mg/ kg).
The decision for adopting any one of the internal fixation technique following the standard procedures (DeYoung and Probst, 1985;
Conzemius and Swainson, 1999 and Raghunath and Singh, 2002) was randomly adopted.
Postoperative careRobert-Jones bandage was applied in all the cases postoperatively for 3 days to alleviate movement and the soft tissue swelling.
Animals were intramuscularly administered with injection ceftriaxone @ 10 mg/ kg body weight for 7 days and injection meloxicam
@ 0.3 mg/kg body weight for 3 days. Post operative dressing was carried out on 3rd, 5th and 7th day and as and when required.
Removal of cutaneous sutures was done after complete healing of the wound in 10th postoperative day. The movements of the
animals were restricted over the post operative period for 7-10 days. Implants were kept in situ over the entire study period.
Statistical analysis
The data were analyzed statistically by general linear model with univariate data by Tukey HSD mult iple comparison test (Tukey,
1953) using SPSS 10.0 version for windows.
RESULTS
The anaesthetic regimen provided adequate anaesthesia. None of the animals showed untoward complication due to anesthesia and
operative procedures.
Physical examination
Postoperative physical examination showed marked soft tissue swelling mostly up to 1st week of operation and in some cases
extent of swelling persisted little bit more i.e. up to 2nd week in the animals of all four groups. The postoperative results of limb
function viz. range of motion of stifle joint and full functional limb usage have been shown in Table II and III. The clinical evaluation
of functional limb usage showed a remarkable difference amongst the study groups being earliest in Gr. C.
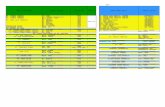
Table: II. Results of limb function and Range of Motion of the Stifle Joint (ROMSJ)
1st week 3rd week 5th week 7th week 9th week ROMSJ
Gr. A (n= 6) Grade- I: (n=6) Grade- II: (n=6) Grade- II: (n=4) III:
(n=2)
Grade- III: (n=6) Grade- III: (n=4)
IV: (n=2)
A5 week: (n=6
Gr. B (n= 6) Grade- I: (n=6)
Grade- II: (n=2)
III: (n=4)
Grade- II: (n=1) III:
(n=5)
Grade- II: (n=1)
IV: (n=5)
Grade- II: (n= 1)
IV: (n= 5)
A7 week: (n=
Gr. C (n= 6) Grade- I: (n=5)
II: (n=1)
Grade- II: (n=1)
III: (n= 5)
Grade- III: (n=4) IV:
(n=2)
Grade- IV: (n=6) Grade- IV: (n=6) N
Gr. D (n= 6) Grade- I: (n=6) Grade- II: (n=1)
III: (n=5)
Grade- II: (n=1) III:
(n=4) IV: (n=1)
Grade- II: (n=1)
IV: (n=5)
Grade- II: (n= 1)
IV: (n= 5)
A7 week: (n=
week: (n=2
A= ankylosis, N=normal, ROMSJ= range of motion of stifle join
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
9/29
Table: III. Mean S.E. of achievement of Grade IV (full functional) limb usage in days
Groups Days
Gr. A 63.00 0.00
Gr. B 49.00 0.00
Gr. C 44.33 2.95
Gr. D 46.20 2.80Radiographic findings
Radiographically, fabricated polymethylmethacrylate plated animals showed early disappearance of fracture line and formation of
direct bridging callus, whereas in intramedullary pinning, animals exhibited formation of excess external callus and more
remodeling time. In intramedullary interlocking nailing, though did not show appreciably noticeable excess external callus
formation, they took more remodeling time than steel bone plating and fabricated polymethylmethacrylate plating but lesser than
intramedullary pinning. The 9th week post operative diagram of femur fracture of dog managed with intramedullary pin showed no
radiographic signs of soft tissue swelling, pin migration or distortion. The radiodensity of the callus at the fracture side was uniform
to that of cortical bone, suggesting maturation and remodeling. The medullary cavity was noticed reestablished in proximal and
distal fragments of the fracture except at the site of union, which still represented the presence of dense callus packing the
medullary canal. The remodeling was yet to be completed though, process found to be in advance stage as evidenced by irregularly
arranged hypo dense callus at the periphery of the union site (Figure 2). The end stage radiograph at the 9th week of fractur eimmobilization in group -B, showed intact radiodense stainless steel plate and screws. The fracture gap was completely obliterated
and remodeled imparting uniformity in radiographic features to that of proximal and distal bone fragments. The thickness of cortex
at the union site was similar to that of normal in transcortical site (Figure 3). After the 9th week of fracture treatment with PMMA
plate the radiograph showed presence of plate and all screws in situ without any materialistic abnormalities. The medullary cavity
was established with uniformity of diameter throughout the length of bone. The remodeling was completed which was evidenced by
absence of extra callus in the exterior or interior of the cortex at the junctional zone (Figure 4). After 9 weeks of fracture
immobilization with ILN in the radiograph, fracture was found completely obliterated with organized callus. The nail and screws
were found intact without any distortion, bending or breakage. The medullary canal looked uniform in diameter even at the
junctional site to that of proximal and distal fragments (Figure 5).
DISCUSSION
Formation of pre-molded PMMA concave plate was very convenient without much difficulty due to its some inherent biomechanical
properties like noncorrosiveness and nonabsorption or degradation of the material within the system (Vcsei and Starlinger, 1982).
Marked soft tissue swelling during 1st postoperative week, irrespective of the groups, was due either to the preoperative trauma by
the bone fragments and severity of the soft tissue injury during surgery. In group C and B the more duration of perceptible soft
tissue swelling was due to more injury inflicted upon the tissue at the t ime of surgery. Moreover, more number of screw t ips which
crossed the transcortex might had also resulted more sustained trauma to the muscle mass in comparison to other two groups,
where either no screw or less numbers of screws were used. The early ambulation of the affected limbs in the animals treated with
PMMA plate in group C, followed by group D (ILN), B (steel plate) and A (intramedullary pinning) were also suggestive of quality of
healing in those group in a same order as, weight bearing is considered to be one of the most important gross observable
parameter for assessing the quality of fracture healing (Hutzschenreuter et al, 1969). The animals of group A treated with
intramedullary pinning showed nonuse of limb for a longer duration (table-II). might have resulted due to the painful swelling of the
operated limb which improved in course of time. The more duration of nonuse of the limb by the same animals might be due to
incomplete neutralization of the forces as the rotational forces never are neutralized as a result of which slight rotational instability
persisted in early phase of fracture healing. Similar to the animals of group A, the femur fracture of dogs immobilized with steel
bone plate in group B also showed nonuse of the affected limb during the 1st week of operation which might be due to the
inflammatory reaction of tissue at the site. The observation of grade-II and grade-III limb use on 3rd week as well as full functional
limb use on 7th week of fracture immobilization indicated the positive correlation of better fracture immobilization and fracture
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
10/29
healing with limb use. The use of bone plate for internal immobilization results to rigid fixation, resisting tension, compression,
shearing and rotational forces (Stiffler, 2004). The use of PMMA plate for internal fixation of fracture is comparatively a newer
concept with variable success (Kallmes and Jensen, 2003). The postoperative physical finding after using PMMA plates for
management of femur fracture in the present study should be graded as promising as, such treated dog showed early ambulation,
weight bearing and uneventful recovery which obviously might had resulted from optimum rigid fixation and qualitative fracture
healing. Femur fractures were treated with interlocking nail as internal fixation device also showed grade- I limb function in firstweek which suggested the similar grade of t issue trauma to other groups while the surgical intervention was undertaken for fixing
the internal fixation device. Subsequently, the dogs showed better grades of limb ambulation which reached to its best i.e. grade-
IV, earliest at 5th to 7th postoperative weeks. Intramedullary pinning in long bone in animals undoubtedly results to better f ixation
stability barring its incapability for resisting the rotational force which can be overcome by using the ILN (Dueland et al, 1999). The
addition of screws or bolts increases the ability of the pin to resist the rotational, shearing and compressive forces at the fracture
site. The early and full limb ambulation is one of the criteria on the basis of which apparently quality of callus formation and
fracture healing can be assessed, was satisfactorily observed in the animals of the Group D treated with ILN.
Intramedullary interlocking nailing does not require perfect anatomic fracture reduction of fracture for stability as such fracture with
intramedullary interlocking nail undergoes indirect bone healing as interfragmentary load sharing is not usually obtained (Stiffler,
2004). In the instant study, presence of moderate quantities of external bridging callus in group A and D, is indicative of secondary
bone healing with stability of fracture. As compression fixation was not attained by interlocking nailing as well as due to preventionof rotational stability of pin by screwing, the exuberant callus formation was not observed which has also been reported by many
workers (Wiss et al, 1986 and Brumback et al, 1988). Radiographically, the fracture fragments were found perfectly aligned,
retained without any remarkable anomalies in group B and C. The prefabricated concave plate, when used for immobilization of the
bone with convex surface, coupled perfectly covering almost 1/3rd of the circumference, which provided very good gr ipping when
fixed with cortical screws in the present study that might be attributed to the reasons for good alignment , retention of fracture
fragments in postoperative observation period. In group B, type of periosteal reaction and formation of callus are in conformity of
normal bore healing (Dambacher and Ruegsegger, 1994). At all stages of radiography in both the groups , the minimum external
callus formation was observed with quickest symptoms of remodeling. The quality and quantity of fracture callus formation mostly
depends on type and accuracy of fracture fixation; more the rigidity and stability in the fixation, minimum is callus formed (Beale,
2004). In the present study, due to rigid fixation, fracture healed by primary union, where direct osteon to osteon union of
fragments occured (Stiffler, 2004; Vasseur et al, 1984).
CONCLUSIONS
Based on the above findings it may be concluded that bone plating is considered to be best option than any other immobilization
devices but, self fabricated PMMA plate seems promising result in veterinary orthopedic surgery considering its cost, fabrication and
facilities for imparting the specific contour of the questioned bone to be repaired, which provide the efficacy of using dynamic
compression of fracture healing.
REFERENCES
Aron, D.N., Palmer, R.H. and Johnson, A.L., 1995. Biologic strategies and a balanced concept for repair of highly comminuted long
bone fractures. Comp. Contin. Educ. Pract. Vet., 17: 35-49.
Beale, B., 2004. Orthopedic Clinical Techniques Femur Fracture Repair. Clin. Tech. Small Anim. Pract., 19: 134-150.
Branden, T.D. and Brinker, W.D., 1973. Effect of certain internal fixation devices on functional limb usages in dogs. J. Am. Vet.
Med. Assoc., 162: 642-646.
Brumback, R.J., Uwagie-Ero, S., Lakatos, R.P., Poka, A., Bathon, G.H. and Burgess, A.R., 1988. Intramedullary nailing of femoral
shaft fractures. Part II: Fracture-healing with static interlocking fixation. J. Bone Joint Surg. Am., 70 (10):1453-62.
Charnley, J., 1960. Anchorage of the femoral head prosthesis to the shaft of the femur. J. Bone Joint Surg., 42: 28.
Conzemius, M. and Swainson, S., 1999. Fracture fixation with screws and bone plates. Vet. C lin. North Am. Small Anim. Pract., 29
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
11/29
(5): 1117-1133.
DeYoung, D.J. and Probst, C.W., 1985. Methods of fracture f ixation. In: Textbook of Small Animal Surgery, W.B. Saunders,
Philadelphia, Edn. 1, Slatter, D.H. p 1949-1988.
Dueland, R.T., Johnson, K.A., Roe, S.C., Engen, M.H. and Lesser, A.S., 1999. Interlocking nail treatment of diaphyseal long-bone
fractures in dogs. J. Am. Vet. Med. Assoc., 214 (1): 59-66.
Gahold, B.M., Dhakate, M.S., Patil, S.N., Gawande. P.S. and Kamble, M.V., 2002. Retrospective study of fractures in canines Areport of 109 cases. Indian J. Vet. Surg., 23 (2): 129.
Heitemeyer, U., Claes, L., Hierholzer, G. and Krber, M., 1990. Significance of postoperative stability of bony reparation of
comminuted fractures. Arch. Orthop. Trauma. Surg., 109 (3): 144-149.
Hutzschenreuter, R., Perren, S.M., Steinemann, S., Geret, V. and Klebl, M., 1969. Some effects of rigidity of internal fixation on the
healing pattern of osteotomies. Injury, 1: 77-81.
Kallmes, D.F. and Jensen, M.E., 2003. Percutaneous vertebroplasty. Radiology, 229:2736.
Moursi, A.M., Winnard, A.V., Winnard, P.L., Lannutti, J.J. and Seghi, R.R., 2002. Enhanced osteoblast response to a
polymethylmethacrylate-hydroxyapatite composite. Biomaterials, 23 (1): 133-144.
Raghunath, M. and Singh, S.S., 2002. Intramedullary interlocking nailing (ILN) for long bone fracture fixation in dogs using
indigenously designed equipment. Indian J. Vet. Surg., 23 (2): 89-91.
Reems, M.R., Beale, B.S. and Hulse, D.A., 2003. Use of a plate-rod construct and principles of biologic osteosynthesis for repair ofdiaphyseal fractures in dogs and cats: 47 cases (1994-2001). J. Am. Vet. Med. Assoc., 223: 330-335.
Roy, S., Samanta, G., Mukherjee, P., Ghosh, D. and De, D., 2005. Occurrence of fracture in dogs in and around Kolkata: A review
of 150 cases. In: XXIX Annual Congress of Indian Society for Veterinary Surgery and National Symposium. p 30.
Stiffler, K.S., 2004. Internal fixation. Clin. Tech. Small Anim. Pract., 19: 105-113.
Tukey, J.W., 1953. The problem of multiple comparisons. Dittoed Manuscript of 396 pages, Department of Statistics, Princeton
University.
Vasseur, P.B., Paul, H.A. and Crumley, L., 1984. Evaluation of fixation devices for prevention of rotation in transverse fractures of
the canine femoral shaft: An in vitro study. Am. J. Vet. Res., 45: 1504-1507.
Vcsei, V. and Starlinger, M., 1982. Gentamicin-PMMA bead chains in the treatment of posttraumatic osseous and tissue infections.
Arch. Orthop. Trauma Surg., 99 (4): 259-263.
Wiss, D.A., Fleming, C.H., Matta, J.M. and Clark, D., 1986. Comminuted and rotationally unstable fractures of the femur treated
with an interlocking nail. Clin. Orthop. Rel. Res., 212: 35-47.
Copyright Priory Lodge Eduation Limited 2008 -
First Published November 2008
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
12/29
Trends in the United States in the Treatment of Distal RadialFractures in the ElderlyKevin C. Chung, MD, MS,1Melissa J. Shauver, MPH,1 andJohn D. Birkmeyer, MD2
Author informationCopyright and License information
This article has beencited byother articles in PMC.
Go to:
Abstract
Background: Traditionally, distal radial fractures in the elderly have been treated nonoperatively with
casting. However, since the introduction of the volar locking plating system in 2000, there has been an interest
in the use of more aggressive treatment methods. The purpose of the present study was to assess changing
trends in the treatment of distal radial fractures in elderly patients in the United States.
Methods: We evaluated a 5% sample of Medicare data from 1996 to 1997 and a 20% sample from 1998 to
2005. Information on four treatment methods (closed treatment, percutaneous pin fixation, internal fixation,and external fixation) was extracted from the dataset. Other available data were diagnosis, physician specialty,
and patient age, sex, and race. We calculated frequencies and rates to compare the utilization of different
treatments over time.
Results: Over the ten-year time period examined, the rate of internal fixation of distal radial fractures in the
elderly increased fivefold, from 3% in 1996 to 16% in 2005. Closed treatment, however, remained the
predominant method (used for 82% of the fractures in 1996 and 70% in 2005). Fractures in patients with an
age of eighty-five years or more were significantly more likely to be treated in a closed fashion (p < 0.0001).
There was a large variation among physician specialties with regard to the fixation methods that were used.
Orthopaedic surgeons were significantly more likely to use closed treatment than hand surgeons were, whereas
hand surgeons were significantly more likely to use internal fixation than orthopaedic surgeons were.
Conclusions: Since 2000, although the majority of distal radial fractures are still treated nonoperatively,
there has been an increase in the use of internal fixation and a concurrent decrease in the rate of closed
treatment of distal radial fractures in the elderly in the United States.
Distal radial fracture is a public health concern, particularly among the elderly, who often experience fragility
fractures. Approximately 10% of sixty-five-year-old white women in the United States will sustain a distal radial
fracture during the remainder of their lifetime1. Traditionally, these fractures in the elderly have been treated
nonoperatively with use of casting alone2. The use of nonoperative treatment has been based on the perceived
low functional demands in the elderly population; however, it has been shown that casting alone for the
treatment of unstable osteoporotic distal radial fractures can result in collapse of the fracture fragments and the
development of a malunion3,4. Interestingly, despite the development of a malunion, many elderly patients
function relatively well, but the majority of studies showing acceptable function involved elderly patients who
were frail or had low functional demands5-9.
Recently, there has been an interest in more aggressive fracture fixation in the elderly in the hopes of speeding
the rate of recovery in order to preserve the ability of patients to live independently2,10-12. The introduction of
the volar locking plating system in 2000 has spurred this interest. A recent prospective study evaluating the
rate of functional improvement after treatment with the volar locking plating system demonstrated similar
rates of recovery between patients in two age groups (twenty to forty years and more than sixty years)13. The
volar locking plating system imparts sufficiently stable fixation to maintain good anatomic reduction, even in
the elderly14. This stability makes it easier for elderly patients to resume activities of daily living earlier than is
the case after treatment with use of the traditional, more conservative approaches that require a longer period
of immobilization14.
http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Chung%2BKC%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Chung%2BKC%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Shauver%2BMJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Shauver%2BMJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Shauver%2BMJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Birkmeyer%2BJD%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Birkmeyer%2BJD%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Birkmeyer%2BJD%5bauth%5dhttp://void%280%29/http://void%280%29/http://void%280%29/http://void%280%29/http://void%280%29/http://void%280%29/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/citedby/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/citedby/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/citedby/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pubmed/2818106http://www.ncbi.nlm.nih.gov/pubmed/2818106http://www.ncbi.nlm.nih.gov/pubmed/2818106http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pubmed/16951109http://www.ncbi.nlm.nih.gov/pubmed/1767640http://www.ncbi.nlm.nih.gov/pubmed/1767640http://www.ncbi.nlm.nih.gov/pubmed/1767640http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib5http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib5http://www.ncbi.nlm.nih.gov/pubmed/15664601http://www.ncbi.nlm.nih.gov/pubmed/15664601http://www.ncbi.nlm.nih.gov/pubmed/15664601http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib10http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib10http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib13http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib13http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib13http://www.ncbi.nlm.nih.gov/pubmed/15614440http://www.ncbi.nlm.nih.gov/pubmed/15614440http://www.ncbi.nlm.nih.gov/pubmed/15614440http://www.ncbi.nlm.nih.gov/pubmed/15614440http://www.ncbi.nlm.nih.gov/pubmed/15614440http://www.ncbi.nlm.nih.gov/pubmed/15614440http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib13http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib12http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib10http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pubmed/15664601http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib5http://www.ncbi.nlm.nih.gov/pubmed/1767640http://www.ncbi.nlm.nih.gov/pubmed/16951109http://www.ncbi.nlm.nih.gov/pubmed/15507821http://www.ncbi.nlm.nih.gov/pubmed/2818106http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/citedby/http://void%280%29/http://void%280%29/http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Birkmeyer%2BJD%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Shauver%2BMJ%5bauth%5dhttp://www.ncbi.nlm.nih.gov/sites/entrez?cmd=search&db=PubMed&term=%20Chung%2BKC%5bauth%5d -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
13/29
Despite their high prevalence, the epidemiology of distal radial fractures is not well-characterized and the
treatment of these fractures in the elderly population remains ill-defined. The specific purpose of the present
investigation was to study a random sample of United States Medicare claims from a ten-year period (1996 to
2005) in order (1) to examine the changing trend in the treatment of distal radial fractures in the Medicare
population and (2) to evaluate physician specialty experiences in the treatment of these fractures.
Go to:
Materials and Methods
For the present study, we used a 5% sample of claims data from 1996 and 1997 and a 20% sample of claims data
from 1998 to 2005 from the United States Centers for Medicare and Medicaid Services, obtained by means of a
formal request. We obtained this dataset from The Dartmouth Institute for Health Policy and Clinical Practice;
investigators at that institution have previously used this particular dataset to track practice variations for a
variety of diseases. The dataset has undergone extensive cleaning to allow ease of analysis and is most
relevant for studying distal radial fractures. The United States Centers for Medicare and Medicaid Services
draws the samples from the claims data for fee-for-service Medicare patients who are sixty-five to ninety-nine
years of age. Both samples were of Medicare Part B claims, which cover physicians' services and were randomly
selected on the basis of the last two digits of the Health Insurance Claim number15. From this sample, we first
extracted claims including an ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical
Modification) code indicating a closed distal radial fracture. Using this smaller group of claims, we then filtered
for claims with Current Procedural Terminology codes for closed treatment (with or without manipulation),
percutaneous pin fixation, external fixation (uniplane or multiplane), and open treatment (Table I). Because of
the coding terminology, we were unable to determine if fixation took place during open treatment. However, it
is rare that open treatment is pursued without internal fixation. For these reasons, we will refer to open
treatment as internal fixation throughout the present report.
TABLE IICD-9-CM and CPT Codes Used for Filtering Medicare Datasets*
Each claim contained the Current Procedural Terminology code of the procedure (treatment method)
performed, the year in which the claim was filed, the sex of the patient, the age group of the patient (sixty-five
to sixty-nine years, seventy to seventy-four years, seventy-five to seventy-nine years, eighty to eighty-four years,
and eighty-five years or more), and the racial category of the patient (white or nonwhite). In addition, each
claim contained the self-designated primary specialty of the treating physician. The United States Centers for
Medicare and Medicaid Services allows the physician to designate as many as three specialties in the order thathe or she chooses. For instance, a surgeon may identify himself or herself as an orthopaedic surgeon primarily
and as a hand surgeon secondarily. Alternatively, the same surgeon could identify himself or herself as a hand
surgeon primarily and as an orthopaedic surgeon secondarily. The dataset that we obtained contained only the
primary specialty designation. It is quite possible that an orthopaedic hand surgeon may identify himself or
herself as an orthopaedic surgeon primarily and as a hand surgeon secondarily.
Frequencies were calculated for 1996 to 1997 by multiplying the 5% sample by 20. Likewise, frequencies for
1998 to 2005 were calculated by multiplying the 20% sample by 5. This is a standard and often-used method to
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#ui-ncbiinpagenav-2http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib15http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib15http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib15http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/table/tbl1/http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#bib15http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2714808/#ui-ncbiinpagenav-2 -
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
14/29
determine overall frequencies from small samples16-18. The significance of differences between groups was
analyzed with use of the Student t test and odds ratios.
Source of Funding
The present study was supported in part by a grant from the American Foundation for Surgery of the Hand, the
National Institute of Arthritis and Musculoskeletal and Skin Diseases Exploratory/Developmental ResearchGrant Award (R21AG030526), a Clinical Trial Planning Grant (R34 AR055992-01), and a Midcareer
Investigator Award in Patient-Oriented Research (K24AR053120) to one of the authors (K.C.C.). Funds were
used to purchase the dataset and for salary support.
Go to:
Results
The 5% dataset (1996 to 1997) and the 20% dataset (1998 to 2005) represented an average of 81,008 Medicare
claims (range, 76,080 to 87,315 claims) for distal radial fracture treatment per year. The tabulation of this ten-
year dataset is presented inTable II. Closed treatment was the predominant method of distal radial fracture
fixation in these patients (Fig. 1). In 2005, 70% of the Medicare claims were for closed treatment. The rate of
percutaneous pin fixation, the second-most-frequently used method of treatment, remained flat before
decreasing slightly between 2004 and 2005. The rate of external fixation use was very low, with little change
occurring over the study period. There was an increasing trend in the use of internal fixation (from 3% to 16%),
which corresponded with a decrease in the use of closed treatment (from 82% to 70%).
TABLE IIEstimated Frequency and Percentage of Fractures Treated Each Year According to Physician Specialty*
Fig. 1Line graph illustrating the rate of each fixation method according to year.
There was very little variation in fixation method according to sex. Male patients were 1% more likely to be
managed with closed reduction, and female patients were 2% more likely to be managed with percutaneous
pinning. There was no difference between the sexes with regard to the use of internal or external fixation. Therewas also no notable difference in the utilization of fixation techniques according to racial group. White patients
were 1% more likely to be managed with percutaneous pinning, whereas nonwhite patients were 1% more likely
to be managed with both closed reduction and internal fixation. As with sex, there were no racial differences in
terms of the percentage of patients who received external fixation. As patients aged, the rate of nonoperative
treatment increased (Table III). Overall, the rate of closed reduction increased from 70.9% of all patients who
were sixty-five to sixty-nine years of age to 87.0% in patients who were more than eighty-five years of age (p
-
7/30/2019 Bone Plating in Patients With Type III Osteogenesis Imperfecta11 (Autosaved)
15/29
0.0001). Likewise, the rate of internal fixation decreased from 10.9% in the youngest age group to 1.0% in the
oldest age group.
TABLE IIIEstimated Frequency* and Percentage of Fractures by Age Groupand Fixation Method
There was a considerable difference among physician specialties with regard to the fixation methods used (Fig.
2). Orthopaedic surgeons were significantly more likely to use closed reduction than hand surgeons were;
specifically, closed reduction was used for 78.2% of fractures treated by orthopaedic surgeons, compared with
56.5% of fractures treated by hand surgeons (p < 0.0001). Similarly, hand surgeons were significantly more
likely to use internal fixation than orthopaedic surgeons were; specifically, internal fixation was used for 27.1%of fractures treated by hand surgeons, compared with 6.3% of fractures treated by orthopaedic surgeons (p








![ATC ppt [autosaved] [autosaved] [autosaved] [autosaved]](https://static.fdocuments.net/doc/165x107/558ca444d8b42a27548b465c/atc-ppt-autosaved-autosaved-autosaved-autosaved.jpg)
