Bone Marrow Interpretation
-
Upload
himanshu-bansal -
Category
Documents
-
view
713 -
download
9
Transcript of Bone Marrow Interpretation

1
Interpretation of Bone marrow aspiration and biopsy
Bone marrow is the site where blood cells develop from totipotential haematopoietic
stem cells. It consists of red marrow (haematopoetic tissue ) & yellow marrow (fat ) in
a meshwork of vascular sinuses and highly branched fibroblasts .
Production of blood cells commences in the yolk sac of embryo ,followed by liver
& to some extent spleen from 2 months of gestation till birth and bone marrow after
7 months which forms the only important site after birth .
Bone marrow is found in practically all bones at birth ,but in adults it is confined to
the central skeleton ( vertebrae, sternum, ribs, skull, sacrum, pelvis ) and proximal
ends of long bones (femur, tibia ,humerus).
Bone marrow aspiration is the removal by suction of the marrow .
It is a simple and safe procedure.
Individual cell morphology is well preserved
But arrangement of cells in marrow & relationship between one cell & another
is disrupted.
So this is an important tool for cell morphology but not for architecture
Bone marrow biopsy or needle core biopsy, is the removal of a small piece of intact
bone marrow
Considered better than aspiration for evaluation of cell distribution and
relationship between different cell types.
An important procedure when disease process is focal in nature
Bone marrow evaluation is not a baseline test, but rather a confirmatory test
used to rule in or rule out specific hypotheses based on routine hematological
investigations.

2
Indications of bone marrow examination
Investigation of unexplained cytopenias
o Unexplained leukopenia (neutropenia).
o Unexplained thrombocytopenia.
o Bicytopenia or pancytopenia.
Anemias esp. Megaloblastic anaemia
Investigation of atypical cells in the peripheral blood
o Immature hematopoietic cells (blasts) in the blood
o Atypical RBC (e.g., basophilic stippling, multiple Howell-Jolly
bodies), WBC, or platelet morphology.
Persistent, unexplained marked increases in RBC, WBC, or platelet numbers
in the peripheral blood.
Evaluation of infectious diseases such as leishmaniasis or histoplasmosis.
Investigation of hematological neoplasia
o Differentiation, diagnosis, and staging of leukemias and lymphomas.
o Diagnosis and staging of other neoplasias e.g. metastatic carcinoma.
Fever of unknown origin.
Immunophenotyping
Note :Bone marrow examination is not mandatory for diagnosis of leukaemias
but is performed for subtyping , baseline blast cell percentage and cytogenetic
analysis.
Same is true for diagnosis of iron deficiency anaemia where simple biochemical
tests along with peripheral blood findings are sufficient for diagnosis.

3
Specific indications of bone marrow biopsy
Dry tap
Suspected aplastic anaemia
Metastatic deposits
Myelofibrosis
Hairy cell leukaemia
Inflammatory conditions like Granulomatous inflammation
Lymphoma infiltration ( Hodgkins & Non hodgkins lymphoma)
To see pattern of involvement in Chronic lymphocytic leukaemia
Preferred sites for bone marrow aspiration & biopsy
Posterior superior iliac spine (both aspiration and biopsy)
Sternum (aspiration only in adults)
Anterior iliac spine (both aspiration and biopsy)
Tibial tuberosity (aspiration in children <one year age)
Procedure ( from posterior superior iliac spine [PSIS] )
1. Position patient in lateral decubitus
position
2. Prepare and sterilize the site with
iodine solution
3. Anesthetize skin and bone with 2%
lidocaine
4. Insert bone marrow aspiration needle
5. Syringe for aspirating bone marrow
while aspiration needle is in place with
trochar withdrawn
6. Aspirate is put on slide
7. Aspirate smear is made using another slide.
8. Biopsy is performed using the same skin
puncture but a different site (on same PSIS) than aspiration .
9. Feel the give of the needle as it enters the cortex
10. Withdraw the trochar from the needle
11. After another centimeter push, rotate the needle to cut the end of the
specimen
12. Withdraw the needle with the specimen inside the needle
13. Push the biopsy specimen from the marrow end to the hub end with the
trochar
14. Place the biopsy specimen in fixative (such as zenker’s)
for decalcification and processing .

4
Bone marrow aspiration & biopsy needles
Kilma aspiration needle
Salah aspiration needle
Jamshidi biopsy needle
Bone marrow aspiration film
Stained with Wright stain or Wright-Giemsa stain, Prussian blue stains.
In addition, special stains may be used that aid in the classification of
malignant white blood cells.
Satisfactory films: when marrow particles and free marrow cells can be seen
Differential counts should be made in the cellular trails
The bone marrow biopsy material is sectioned onto glass slides and stained with
hematoxylin-eosin stain .
Bone marrow aspiration smear Bone marrow biopsy section

5
Bone marrow evaluation includes the examination of :
1) Bone marrow aspirate;
2) Bone marrow core biopsy
3) Peripheral blood.
When a high-quality bone marrow aspirate is obtained, and depending on the reasons
for doing the bone marrow examination, sometimes an aspirate (without a core) is
sufficient for evaluation.
Peripheral blood (i.e., a CBC) ALWAYS is needed for accurate interpretation of
bone marrow
Bone marrow interpretation : The protocol
Review patient history and laboratory data .
Examine peripheral blood smear
Examine bone marrow aspirate
-Examine at least two films
-Low magnification (10X) examination - cellularity,
megakaryocytes , infiltrates
-High magnification (100X) examination- Examine each cell line
,fine cytological details, differential count in cell trails
Examine bone marrow biopsy
-Examine slides at minimum three levels
-Low power examination: evaluate cellularity , megakaryocytes
, focal /diffuse nature of the lesion
-High power examination : evaluate each cell line , detail of
focal lesion
Evaluate flow cytometry , immunohistochemical stains etc.
Assign final diagnosis.
A) Patient information
Patient identification a. Name b. Identification number c. Age d. Gender
Referring physician
Date of procedure
Clinical information
o Relevant history and physical findings

6
Constitutional symptoms- fever, fatigue,night sweats,weight loss
H/o autoimmune disorder,
Immune status i.e HIV
H/o bleeding from any site
Current medication –e.g aspirin
Prior diagnosis-documented malignancy
Prior therapeutic regimens
Any transplantation
Prior surgery- splenectomy,gasterectomy
Physicalfindings-pallor,icterus,ecchymosis,any
lymphadenopathy,hepatomegaly or splenomegaly
Relevant laboratory data
o ESR
o Biochemical investigations
o radiographic data & imaging studies
B) Peripheral blood film examination
Peripheral blood sample should be obtained on the same day as marrow collection.
This is essential because rapid changes can occur in peripheral blood counts and
accurate interpretation of cells in the marrow require knowledge of CBC results.
Hemoglobin
TLC
DLC
Platelet count
Microscopic description of RBCs ,WBCs & Platelets:
number
size
shape
Peripheral smear interpretation
C) Reporting of a bone marrow aspirate
1) Specification of site : Posterior Superior Iliac Spine or Sternum.
2) Overall sample quality/Adequacy of specimen i.e whether fragments present or
not seen as glistening particles caused by fat in the particles
3) Low power examination : Choose several of the best spread fragments which
contain easily visible marrow particles
i) Particle cellularity (hypocellular, normocellular, hypercellular).Cellularity
is assessed in relation to the amount of adipose tissue in the particles and can
be estimated as a percentage . A rough estimate is made as follows :
Amount of haematopoietic tissue / amount of adipose tissue X 100.
Because the amount of active marrow decreases with age, interpretation of
cellularity must take into account the patient's age.

7
Cellularity averages 79%( haematopoietic tissue) at ages 0-9 yrs.
50% (haematopoietic tissue)at ages 30-69yrs.
29% (haematopoietic tissue) at ages 70-79yrs
Normocellular marrow
Hypocellular marrow :
causes Aplastic anaemia
Inherited bone marrow failure syndromes
Chemicals like Benzene
Drugs like carbamazapine
viruses,
ionizing radiation
Autoimmune disorders
Paroxysmal nocturnal hemoglobinuria

8
Hypercellular marrow
Causes
myeloproliferative disorders,
myelodysplasia or other
ineffective hematopoiesis,
leukemias,
lymphoma infiltration
megaloblastic anemia, sidero
blastic anemia,
compensatory hyperplasia after
cell destruction
Scanning under low power reveals a heterogenous population of cells composed
of erythroid cells, cells of myeloid series, lymphoid cells, plasma cells etc.

9
ii) Megakaryocytes. These are the largest cells randomly distributed throughout the
bone marrow . These are assessed for :
a) Number (adequate/ inadequate): These make about 0.5% of total cells in the
marrow . Roughly at least five megakaryocytes should be present per fragment
b) Maturation (mature forms should exceed immature forms in normal marrow):
normal maturation of megakaryocyte includes following stages
o Megakaryoblast : 6-24 micrometer in diameter with large minimally
indented nucleus having fine chromatin , multiple nucleoli and scant
basophilic cytoplasm. Comprise 20% of megakaryocyte lineage cells
in marrow.
o Promagakaryocyte : larger than megakaryoblast lobulated nucleus
,with comparatively coarser chromatin and more abundant and less
basophilic cytoplasm than megakaryoblast .Comprise 25% of marrow
megakaryocytes.
o Mature magakaryocytes measures 50-150 microns in size with
abundant pink cytoplasm containing numerous purple-red or pink
granules; nucleus has 8, 16 or 32 overlapping lobes ; no nucleolus.
Megakaryocytes producing platelets may have demarcated granular
clumps of platelets streaming from the margin
c) Morphology: normal morphology is described above
mature megakaryocyte

10
Abnormalities in number
Megakaryocytic hyperplasia
i) Reactive,in chronic inflammatory disorders
ii) Idiopathic thrombocytopenic purpura (ITP)
iii) Myeloproliferative diorders
iv) Essential thrombocythemia
Megakaryocyte depression
i) Aplastic anaemia
ii) Drugs
iii) Viral induced
Abnormalities in maturation
Presence of young forms in Idiopathic thrombocytopenic purpura
Abnormalities in morphology
i. Dysplastic megakaryocytes seen as hypolobulated
micromegakaryocyte or nonlobulated nuclei in
megakaryocytes of all sizes and multiple ,widely separated
nuclei- In myelodysplastic syndromes(MDS)
ii. Hyperlobated nuclei – in Essential Thrombocythemia.
iii. Atypical megakaryocytes –enlarged with abnormal chromatin
clumping associated with balloon shaped lobulation of nuclei as
well as frequent naked megakaryocytic nuclei seen in Chronic
idiopathic myelofibrosis .
iii) Search for abnormal cells i.e. Clumps of cells foreign to the bone marrow
Granulomas
Metastatic deposits
Macrophages
Sea blue histiocytes in storage disorders
Necrosis: leukemias and lymphomas, chemotherapy, AIDS
Gelatinous transformation :anorexia, alcohol, AIDS
Gelatinous transformation Gaucher cells (sea blue histiocytes)

11
4) High power examination : The part of the smear spread best is examined at high
magnification
A minimum of 500 nucleated cells should be evaluated under oil immersion.
Differential using categories : erythroid, myeloid ,lymphoid and plasma cells
is generally adequate
Only intact cells are evaluated; bare nuclei should be excluded
Counting is performed where cells are not overlapping, clustered or
artifactually distorted
i) The myeloid:erythroid (M:E) ratio
Myeloid series : Neutrophil ,Eosinophil, Basophil precursors and mature forms are
collectively reffered to as myeloid cells
a. Erythroid hyperplasia(M:E,1:1 or less)
-DNA synthesis defects(B12 ,folate deficiency, drugs like methotrexate)
-Hemoglobin synthesis disorders(Thalassemias & congenital sideroblastic anemia)
-Hemolytic anemias i.e hemogobinopathies,RBC membrane disorder or enzyme
deficiencies) or acquired (immune hemolytic anemia,PNH)
-After massive haemorrhage
-Polycythemia
Erythroid hyperplasia
b. Erythroid hypoplasia : Absence/suppression of red cell precursor
Pure red cell aplasia

12
Congenital : Diamond blackfann syndrome
Acquired:Parvovirus B19 infection , Secondary to Thymoma etc.
c. Myeloid hyperplasia
Myeloproliferative disorders
Myelodysplastic syndromes.
Acute leukemia
Infections
Myeloid hyperplasia
d. Myeloid hypoplasia
Drug induced- cytotoxic drugs
Chemicals like benzene etc.
Virus induced
ii) Erythroid cell line. Evaluated for numbers, maturation, morphology.
Erythroid cells in bone marrow are the erythroblasts in different
stages of maturation seen as proerythroblasts, basophilic erythroblasts ,
polychromatic erythroblasts and orthochromatic erythroblasts.
Number : The mean percentage of erythroid series in bone marrow is about 25%
Cell composition of erythroid series with normal range
Proerythroblasts 0.1-1.1%
Basophilic erythroblasts 0.4-2.4%
Polychromatic erythroblasts 2-30%
Orthochromatic erythroblasts 2-10%
Erythroid hyperplasia and hypoplasia can occur in a variety of conditions as discussed
in previous section on M:E ratio.
Maturation and morphology
Red cells are produced by proliferation and differentiation of erythroblasts in the
marrow . During the course of differentiation, the size of erythroblasts progressively
decreases and the character of nucleus and cytoplasm changes as depicted in the
diagram below

13
1.Proerythroblast 2.Basophilic erythroblast 3.Polychromatic erythroblast
4.Orthochromatic erythroblast 5.Reticulocytes 6.Red blood cells
Proerythroblast : These are the least mature of the morphologically
identifiable cells of erythroid series measuring 14-20 micrometer in
diameter , have round to oval nucleus with fine chromatin ,multiple nucleoli, and
basophilic cytoplasm.
Basophilic erythroblast : It is a round cell measuring 12-16 micrometer in
diameter (smaller than han proerythro blast) with coarser and more basophilic
nuclear chromatin and more basophilic cytoplasm than proerythroblast.
Polychromatic erythroblast : It is a round cell 12-14 micrometer in diameter
having coarse nuclear chromatin seen in deeply basophilic clumps and
polychromatic cytoplasm because of acidophilic haemoglobin (starts appearing at this
stage) and basophilic ribonucleic acid. The prolifertive activity of nucleus ceases after
this stage.
Orthochromatic erythroblast : These measure 8-12 micrometer in diameter
with a small pyknotic nucleus giving a homogenous blue-black appearance and
predominantly acidophilic cytoplasm.
Reticulocytes are formed from Orthochromatic erythroblasts after extrusion of
nucleus from latter .These than enter the blood and mature into red blood cells .
Abnormalities in maturation and morphology
1) Megaloblastic maturation : Seen in megaloblastic anaemia .The changes
occur at all stages of maturation and are best appreciated in late precursors
.
1 4
2
5
2
6
2 2
3
2

14
The cells are larger than the normal counterparts with an increase in both
cytoplasm and nuclear size .The nuclear chromatin is arranged in fine reticular
fashion to give a stippled appearance (sieve like).This stippled appearance is
still well marked in polychromatic erythroblasts and sometimes also in
orthochromatic erythroblasts
-Nuclear cytoplasmic asynchrony : the maturation of nucleus lags behind
cytoplasmic maturation
2) Dyserythropoiesis : seen in myelodysplastic syndromes ( primary and therapy
related MDS )-seen as Nuclear alterations including budding, internuclear
bridging ,karyorrhexis, binucleation , multinucleation and megaloblastoid
change ( chromatin pattern as megaloblast but normal in size)
Cytoplasmic features including ring sideroblasts ,vacuolization and periodic
acid schiffpositivity-
Bone marrow smear exhibiting 1) nuclear budding and 2) multinucleation in
erythroid series of cells
3) Micronormoblastic maturation: Smaller than normal with scant cytoplasm
having ragged borders .Cytoplasmic maturation lags behind nuclear
maturation so that nucleus often appears pyknotic despite the fact that
cytoplasm is still polychromatic ( see normal maturation and morphology of
erythroblasts) -seen in Iron deficiency anaemia
4) Maturation arrest : Characterized by an increase in the proportion of more
primitive cells – seen in Megaloblastic anaemia , where promegaloblasts and
basophil megaloblasts may constitute > 50% of erythroblasts .
iii. Myeloid cell line. Neutrophil ,Eosinophil, Basophil precursors
and mature forms are collectively reffered to as myeloid cells . These are
evaluated for numbers, maturation and morphology.
Number : The mean percentage of myeloid series in marrow is about 55% .
Neutrophil series constitute approximately 90-95 % of the total myeloid series and
eosinophils make virtually all of the remainder.
Neutrophil series %
– Myeloblasts 0-3
– Promyelocytes 0.5-5
1 2

15
– Myelocytes 5-23
– Metamyelocytes 7-27
– Polymorphs 4-28
Eosinophil series 0.3-4
Basophil series 0-0.5
Myeloid hyperplasia and hypoplasia can occur in a variety of conditions as discussed
in previous section on M:E ratio.
Maturation and morphology : Mature granulocytes are produced by the
proliferation and maturation of precursors from the earliest recognizable stage , the
myeloblast, through the promyelocyte, myelocyte, metamyelocyte and stab form stage
,until the mature segmented stage is reached. .Development of the three cell lines of
myeloid series follows a similar pattern except that the distinction between colour of
granules becomes obvious at the myelocyte stage.
The myeloblast : measures 15-20 micrometer , with round to oval
nucleus having fine nuclear chromatin , prominent nucleoli and moderate amount of
basophilic cytoplasm .No granules are seen .
The Promyelocyte :features are similar to those of myeloblast except for
the development of some cytoplasmic granules , coarser chromatin and prominent
nucleoli.
The myelocyte : It is slightly smaller than promyelocyte having
prominent cytoplasmic granules( may be neutrophilic, eosinophilic or basophilic) and
less basophilic cytoplasm with comparatively low nuclear cytoplasmic ratio , coarser
chromatin than promyelocyte and no nucleoli. This stage is the most mature
proliferating cell in the myeloid lineage . Subsequently steps in the maturation process
occur in non-proliferating cells
The metamyelocyte : features are similar to those of myelocyte except
that nucleus is indented (kidney shaped) ,granules more prominent, cytoplasm less
basophilic and chromatin more coarse.

16
The band or stab form stage . :characterized by indented nucleus
with degree of indentation more than 50% of the nucleus diameter and cytoplasm
colour identical to that of a mature segmented neutrophil .
Segmented granulocyte : measures 12-14 micrometer in diameter having
lobulated nucleus with lobes of clumped chromatin linked by a thin chromatin strand .
Mature neutrophil has 2-4 lobes of nucleus .It measures 12-14
micrometer in diameter and pink cytoplasm with fine granules
Mature eosinophil has bilobed nucleus ,measure 12-17micrometer in
diameter with cytoplasm packed with distinctive spherical eosinophilc granules
Mature basophil has nuclear lobes that tend to fold on each other
resembling a closed lotus flower .It measures about 16 micrometer in diameter with
distinctive large ,variably sized dark blue or purple granules in the cytoplasm
obscuring the nucleus .
1. The myeloblast 2. The Promyelocyte 3. The myelocyte
4. The metamyelocyte 5. The band or stab form 6. Segmented granulocyte
Abnormalities in maturation and morphology
Maturation arrest- shift to left till promyelocyte stage ,blasts still within
normal limits seen in Myelodysplastic syndrome(MDS) ,severe infections
,AIDS
1 2
4 3 5 6
Basophil series
Neutrophil series
Eosinophil series

17
Increase in myeloid blasts : in acute myeloid leukaemias
The blast cells are lage with nucleus having fine chromatin prominent nucleoli and
moderate cytoplasm with som e cells exhibiting granules and auer rods
.
Morphology Giant metamyelocytes and stab forms seen as large cells with nucleus
having irregular outline in megaloblastic anemia
Dysplasia in myeloid series : seen as hypogranulation, nuclear hyper and
hyposegmentation , marked left shift in maturation-MDS
A hypogranular, hyposegmentedneutrophil(pseudo-Pelger-Huët anomaly).Note the severe thrombocytopenia.
A giant myeloid precursor.
Erythroid and myeloid precursors.Many of the myeloid cells arehypogranulated. Some of the lateerythroid precursors are mildly enlarged.
Ring sideroblastsand increasediron incorporation in both erythroidprecursors and mature RBCs.
A hypogranular, hyposegmentedneutrophil(pseudo-Pelger-Huët anomaly).Note the severe thrombocytopenia.
A giant myeloid precursor.
Erythroid and myeloid precursors.Many of the myeloid cells arehypogranulated. Some of the lateerythroid precursors are mildly enlarged.
Ring sideroblastsand increasediron incorporation in both erythroidprecursors and mature RBCs.
Bone marrow aspirate showing hypogranulated neutrophils with left shift seen as
increased number of myelocyte and metamyelocytes
iv. Maturation index.
The proportions of proliferating ( proerythroblast+ Basophil+ polychromatic
erythroblast for Erythroid series and myeloblast + promyelocyte+ myelocyte
in myeloid series ) vs nonproliferating cells ( orthochromatic erythroblasts in
erythroid series and metamyelocyte+band form+ mature forms in myeloid
series) can be estimated or counted for calculation of an erythroid maturation
index, myeloid maturation index, and overall ( adding the two) maturation
index.
Maturation indices are useful for semi-quantifying left or right shifts in
hematopoietic cell maturation.

18
v Lymphocytes: Normal range : 5-24% of total cells in marrow . In children
may constitute up to 50% of all nucleated cells. Lymphocytes pass through a series of
changes in the course of development from lymphoblasts.
Lymphoblasts are slightly smaller than the myeloblasts except that the ratio of the
diameter of nucleus to that of the cell tends to be greater and the number of nucleoli
per nucleus are fewer than in the myeloblast .
Small lymphocyte:These are small cells with a thin rim of cytoplasm , occasionally
containing fine azurophilic granules. Uniform nuclei 9-12 micrometer in diameter
which is roughly the size of a red blood cell.
Large lymphocyte measuring 12-16 micrometer in diameter with round nucleus
and clumped chromatin with more abundant pale blue cytoplasm containing
azurophilic granules.
Evaluated for number and maturation.
Number :Increased lymphocytes can be seen in
Older individuals
Chronic inflammatory & autoimmune diseases
Lymphproliferative disorders involving marrow
Maturation Presence of lymphoblasts : seen in leukaemias .
VI Plasma cells
The plasma cells are seen as round to oval cells with 2 -3 times the size of
small lymphocytes ,one or more eccentrically placed nuclei ,clumped
chromatin in the form of cart wheel and a perinuclear clear zone
These make 0-3.5% of total cells in the marrow.
Evaluated for number , immature forms , inclusion .
Number- normal or increased :
Increased in : Reactive plasmacytosis
Lymphoblasts : seen as cells having altered
nucleocytoplasmic ratio , with fine nuclear
chromatin ,inconspicuous nucleoli and scant
amount of cytoplasm

19
Neoplastic –Multiple myeloma .
Immature forms (plasma blasts) seen as pleomorphic
frequently multinucleate cells having dispersed nuclear
chromatin, prominent nucleoli and high nucleocytoplasmic
ratio. Seen in Multiple myeloma.
Inclusions :seen because of condensed or crystallized cytoplasmic Ig
producing a variety of morphologically distinctive findings e.g
- Cherry red refractive round bodies -Russell bodies,
- Vermillion staining glycogen rich Ig - Flame Cells,
- Multiple pale bluish white ,grape like accumulation-Mott Cells,
- Overstuffed fibrils –Gaucher like cells, thesaurocytes.
Plasmablasts in multiple myeloma Mott cells
vii. Monocytes and macrophages
These are the phagocytic cells involved in host defence against infection.
These develop from monoblasts through promonocytes.
- Monoblasts are the least mature of the morphologically recognizable
members of the monocyte-macrophage series. These are similar in appearance
to myeloblasts
- Promonocytes: similar in size to the promyelocyte ,but has a more irregularly
shaped and often deeply cleft nucleus containing nucleoli with cytoplasm
containing granules which are more basophilic than in mature monocyte.
Monocytes: Normal range : 0-0.6% of total cells in marrow
These are similar to the circulating leucocytes measuring 15 -18 micrometer
in diameter and have large curved often horseshoe shaped (wrung towel) with
bluish cytoplasm containing fine reddish granules
Increased in
Reactive monocytosis
Acute monocytic leukaemia
Chronic myelomonocytic leukaemia
Macrophages: Normal range: 0-2% of total cells in marrow

20
These range from 15-80 micrometer having one or more oval nuclei and
abundant cytoplasm with an irregular cytoplasmic outline containing granules
and sometimes vacuoles which may contain phagocytosed material.
Increased production o when there is an increased need for phagocytes.
Infectious process
During chemotherapy
o Haemophagocytic syndromes
o Storage disorders
o Malignant histiocytosis
Cytochemical stains:
Cytochemistry is the technique used to identify diagnostically useful enzymes or other
substances in the cytoplasm of the haematopoietic cells .It is particularly useful to
characterize the blasts cells in acute leukaemias as myeloid ,to identify monocytic and
granulocytic components in AML .
Various cytochemical stains used and the cells attained by them are listed below
Leishmania Donovani infection:
seen as T shaped or double dot
Leishmania donovani (LD) bodies
present both intracellularly (within
the macrophages) and
extracellularly
• Haemophagocytosis : RBCs
are seen engulfed by
activated macrophages. Cells
appear as stuffed

21
Uses
Myeloperoxidase stain :gives brown granular staining and used to differentiate
between myeloid (+) and lymphoblastic (-) leukaemias .
Sudan black : The reaction product is black and granular with reactivity similar in
to myeloperoxidase and is used to differentiate between myeloid (+) and
lymphoblastic (-) leukaemias .
Chloracetate estrase : The reaction product is bright red with positivity in
granulocytic cells and mast cells .The activity appears as the myeloblasts mature to
promyelocytes and myelocytes which stain strongly . It is therefore useful as a marker
of cytoplasmic maturation in granulocytic leukaemias with heavy cytoplasmic
staining in acute promyelocytis leukaemia.
α naphthyl butyrate esterase : The reaction product is brown and granular and
is used to identify the monocytic population in AML M4 and M5
β naphthyl butyrate esterase : gives diffuse red/brown staining and is used to
identify the monocytic population in AML M4 and M5 .Less specific than α naphthyl
butyrate esterase .

22
Acid phosphatase: Its reaction product is red and is used in diagnosis of T cell
acute leukaemias and hairy cell leukaemia.
Periodic acid schiff:The reaction product is magenta in colour. Two types of
pattern are seen i.e. granular and diffuse positivity in granulocytic precursors &
block positivity in lymphoblasts in acute lumphoblastic leukaemia
Toulidine blue: The reaction is granular and bright red/purple in colour .It is used
to highlight mast cells and basophils.
5. Hemosiderin. Iron is essential for haemoglobin synthesis and is present in bone
marrow as haemosiderin , which is the main storage form of iron in
reticuloendothelial cells . .
Bone marrow iron stores : The iron stores (hemosiderin) can be assessed by using
the Prussian (perl’s) blue stain .It is best performed on bone marrow aspirate
smears.For grading of iron stores intracellular iron( present in macrophages with a
small amount in erythroblasts) is evaluated as extracellular iron can be an artifact .
The iron stores in bone marrow may be assessed as normal , decreased or increased
and grading from 1+ to 6+ (as given below) is used .

23
Bluish iron in Bone Marrow Aspirate smear (perl’s Prussian blue stain)
Grades 1+ to 3+ are considered normal with decreased iron stores when < 1+
and increased iron stores when > 3+ .
Increased bone marrow iron
Anaemia of chronic disorder
Sideroblastic anaemias etc
Decreased bone marrow iron
Iron defeciency anaemia
The Prussian blue stain can also be used to identify sideroblasts which
constitute 30-50% of erythroblasts in a normal marrow .These have small , few( 2-
5), fine, scattered prussian blue positive granules in the cytoplasm . Another type
of sideroblasts i.e. Ring sideroblasts seen as numerous and large granules
,frequently forming a complete or partial ring around nucleus can also be found in
the marrow in conditions with disturbed haem synthesis
Ring sideroblasts are seen in
Sideroblastic anaemia
Lead intoxication
Megaloblastic anaemia
Drug reaction : Chloramphenicol, Isoniazid etc.
Bone marrow biopsy interpretation
BMB is mandatory when aspirate is not obtained ("dry aspirate" or "dry tap"),the causes for
which are listed below .
Aplastic anaemia
Bone marrow failure syndromes
Marrow fibrosis
Marrow infiltration disorders(including metastatic deposits,lymphoma
involvement )
Hairy cell leukaemia
Granulomatous disorders
Pyrexia of unknown origin
Bone Marrow Biopsy has some advantages over aspirate as listed below :
Examination of a greater volume of tissue with preserved architecture,
Assessment of cellularity

24
Detection of compact and/or fibrotic lesions,
Detection of metastatic deposits
Identification of granulomas
Application of immunohistochemistry (IHC).
Analysis of the BM biopsy : Bone marrow biopsy should be examined at
minimum three levels .A systematic approach is needed which includes:
-Low power examination: evaluate for cellularity , megakaryocytes ,any focal
lesions
-High power examination : evaluate for details of each cell line and detail of the
focal lesion
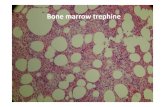
i) Size / adequacy of the biopsy
A bone marrow trephine biopsy specimen must be of adequate size to permit
reliable interpretation of cellularity and to give a reasonable probability of
detecting focal lesions.
It should contain three or four intertrabecular spaces and be at least 0.5cm in
length . The current recommendation for adequate biopsy being 1.6cm-2.0cm
Trephine biopsies composed of cortical bone and a small amount of
subcortical bone marrow are inadequate and may give a false impression of
hypocellularity
a) Cellularity is assessed by roughly estimating the percentage of section
occupied by the haematopoietic tissue in relation to the adipose tissue and this
can vary with age.
Different patterns of cellularity in a young adult are as below :
Hypocellular Normocellular Hypercellular
The variations of cellularity with age have already being discussed in section on bone
marrow aspiration
b) Megakaryocytes : these are the largest cells in marrow and are evaluated for
distribution, number and morphology .
Distribution
- Normally the megakarycytes are perisinusoidal in central parts of
marrow and are seen either singly or in clusters of ≤3 cells .
- Abnormal distribution can be seen in

25
-Myelodysplastic syndrome where the megakaryocytes are seen
paratrabecular in location.
-Large clusters of megakaryocytes seen in myeloprolferative disorders
and following chemotherapy.
Number : the causes of increased and decreased megakaryocyte number have
already been discussed in section on bone marrow aspiration.
Morphology :
- Size : Large megakaryocytes in Essential thrombocythemia
o Small megakaryocytes in Chronic melogenous leukaemia
- Dysplasia : seen as anisocytosis, abnormal nucleocytoplasmic ratio ,
hyperlobulation and/or hypolubulated nuclei in Myelodysplastic
syndromes and Chronic idiopathic myelofibrosis.
High power examination
For details of haemopoietic cell lines: ( distribution, maturation and morphology)
Normal distribution
Erythropoietic islands: perisinusoidal in central parts of marrow
Myeloid cells : Precursors are mainly partrabecular in 2-3 rows .As the cells
mature these lie in central parts of marrow cavity
Other cells : show no particular pattern
a) Erythroid cells : present as clusters of erythroid cells in different stages of maturation seen around sinusoids .These cells are arranged closely adhered to each other and have round nuclei with condensed chromatin in late erythroblasts (can be confused with lymphoid cells which show coarse clumping of chromatin).These cells are evaluated for distribution ,number, maturation and morphology.

26
Distribution: Erythroid cells present in paratrabecular location in myelodysplastic syndrome
Number: The causes of increase and decrease in erythroid cell number
in marrow have already been discussed in section on bone marrow
aspiration.
Maturation and morphology :
-In regenerating marrow the islands of erythroid cells are composed of
cells in same stage of maturation i.e. clusters of immature elements
seen -Dyserythropoiesis : as seen on bone marrow aspirates ( already discussed
before )
b) Myeloid cells : In a normal marrow precursors of myeloid cells are mainly partrabecular in 2-3 rows and as the cells mature these lie in central parts of marrow cavity.
o Distribution abnormal in Myelodysplastic syndrome : Abnormal localisation of Immature
Precursors(ALIP) : 3 or > foci of small aggregates of myeloblasts ,promyelocytes localised in central portion of marrow away from vascular structures and endosteal surface of bone trabecula .
Myeloproliferative disorder (CML) : Paratrabecular cuff of immature neutrophils increased to 5-10 cells thick.
o Morphology : dysplastic changes as already discussed before under bone marrow aspirate examination.
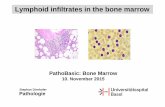
c) Lymphoid cells : these show no particular pattern of distribution and are seen scattered in between the other haematopoietic elements .
Increase in lymphoid cells : can be seen as a part of reactive process or a neoplastic proliferation .
Arrangement of lymphoid cells : Reactive process may show interstitial arrangement or a nodular
pattern . Interstitial is described as lymphoid cells interspersed between the normal haematopoietic cells with increase in number of lymphoid cells .The confirmation of nonneoplastic nature of lesion is done on immunohistochemistry Nodules of reactive lymphoid cells are small with well defined margins and composed of polymorphous population of lymphoid cells depicting different stages of maturation .
Neoplastic proliferation oon the other hand shows three types of pattern:
Interstitial
Nodular
Diffuse
Interstitial : Presence of individual neoplastic cells interspersed between the haematopoietic
cells without distortion of bone marrow architecture.

27
Nodular pattern : seen as large nodules with ill defined margins often extending around fat
cells and composed of homogenous population of lymphoid cells .
Diffuse pattern: replacement of normal marrow( distorting archtitecture of marrow ) by
diffuse sheets of neoplastic lymphoid cells .
d) Abnormal cells: which are identified as:
- Blasts of different cell lineage
- Lymphoma infiltration by marrow
- Myeloma cells
- Metastatic deposits
Note: For details of individual cell types kindly refer to standard text books.
Biopsy showing sheets of blasts –acute leukaemia
Biopsy of hairy cell leukaemia with honey comb or fried egg appearance

28
Biopsy of Multiple myeloma with shets of plasma cells
Granulomas (arrows) in bone marrow
Oxalate crystals with gaint cell raction in patient with oxalosis
Metastatic deposits : seen as clusters and glandular arrangement of hyperchromatic &
pleomorphic cells
Amyloidosis: showing extracellular homogenous eosinophilic material

29
Storage disorder : Gaucher cells with abundant tissue paper cytoplasm
Quantification of BM reticulin
Reticulin is an early form of collagen( connective tissue) which is always present in small
amount in normal bone marrow i.e. mainly perivascular and periendosteal in location.
Reticulin can be stained using silver impregnation technique or Massons trichrome stain
(stains collagen).The silver impregnation technique is routinely used in many laboratories
and it stains reticulin black .
Reticulin deposition can be graded as follows
The majority of normal subjects have grade of 0-1.While grading reticulin the perivascular
and periendosteal areas should be disregarded as
these may give a false high grade .
Normal reticulin Increased reticulin
Causes of Increased reticulin Idiopathic myelofibrosis
Secondary myelofibrosis
o Myeloproliferative disoreders
o Hodgkin’s disease
o Hairy cell leukaemia

30
o SLE
o AIDS
Bone marrow artifacts Various artifacts in bone marrow aspirate and biopsies need to be recognized so that
they are not misinterpreted. These artifacts can be introduced during the procedure or
while processing in the laboratory.
Bone marrow aspirate artifacts :
1. Procedure : - Inadequate particles: because of poor technique
- Abnormal spreading: cell crushing and distortion because of excess
pressure applied.
- Clotted specimen
2. Processing: - Inadequate drying of the film: the nuclear contents are seen leaking
into the cytoplasm and cellular outline is indistinct.
- Poor fixation: because of water uptake into methanol used for fixation
.It causes refractile inclusions in the red cells and poor definition of
cellular details.
- Delayed fixation and staining which gives strong blue tint to the film
3. Extraneous material : like crystals of glove powder which stains blue
with May Grunwald Giemsa stain and red with Periodic acid Schiff stain .
Crush artifact because of abnormal spreading Artifact because of inadequate drying of film
Bone marrow biopsy artifacts
1. Procedure : - Too short biopsy sampling - Mainly subcortical bone in biopsy sample when needle introduced at
wrong angle : falsely hypocellular specimen - Use of blunt needle leads of crumbling of bone to amorphous material - Torsion artifact elongated nuclei produced by twisting of the needle - Aspiration artifact : when aspiration performed immediately before a
biopsy causes haemorrhage, disruption of tissue - Biopsy done from a previous biopsy site: shows fat necrosis and
granulation tissue .

31
2. Processing : - Poor fixation : glassy nuclei with detailed structure cannot be recognized - Shrinkage artifact : a clear space seen around the erythroblasts and megakaryocytes - Poor stainig : excessive decalcification
3. Extraneous material
Special tests on bone marrow
Immunophenotyping
Detection of antigens on the cells by using monoclonal antibodies .
Techniques utilized :
Flow cytometry: when the cells bearing the antigen are identified by means of monoclonal
antibodies labeled with a flourochrome .Peripheral blood sample ( when significant number
of abnormal cells are present) and bone marrow samples are used.
Immunohistochemistry or immunocytochemistry : when the cells bearing the antigen are
identified by means of monoclonal antibodies applied to fixed cells or tissue sections on
glass slides .Peripheral blood sample ( when significant number of abnormal cells are
present) , bone marrow samples or a washed mononuclear cells isolated from blood or
bone marrow are used.
Used in
- Diagnosis and classification of haematological neoplasms - For detection of minimal residual disease.
Cytogenetics:

32
Refers to study of chromosomes and their abnormalities.
Chromosomal abnormalities are a common finding in haematological neoplasms so much so
that some neoplasms are defined more precisely by the percentage of specific chromosomal
abnormalities like acute myeloid leukaemias with recurrent genetic abnormalities
Used for :
1. Confirmation of diagnosis e.g. by demonstration of t (15;17) in M3 variant of AML
2. Also certain chromosomal abnormalities offer prognostic information e.g. in acute myeloid leukaemias presence of t(8;21) ,t(15;17) or inv (16) are indicative of better prognosis.
3. Confirmation of neoplastic processe 4. Monitoring the treatment like in Chronic myelogenous leukaemia by estimation
of Philadelphia positive [ t (9: 22) ]metaphases . Performed on cell suspensions obtained from peripheral blood or bone marrow .
Suggested further reading:
DC Thachuk ,JV Hirschmann, Approach to the microscopic evaluation of blood & Bone marrow In : Wintrobe’s atlas of clinical Haematology , Eds . DC Thachuk ,JV Hirschmann, Lippincott Williams & Wilkins,2007; p 275-327
I Bates .Bone marrow biopsy . In : JV Dacie & SM Lewis .Practical Haematology, 9th edition , Eds .SM Lewis , BJ Bains, I Bates, Churchill Livingstone ,London , 2001: 101-114.
LP Sherrie .Examination of blood & bone marrow In : Wintrobe’s clinical Haematology ,vol 1, 11th edition , Eds .JPGreeer, GM Rodgers, J Foerster et al , Lippincott Williams & Wilkins, 2004; p 3-26.