BMI Chelsfield Park Hospital - Care Quality Commission
Transcript of BMI Chelsfield Park Hospital - Care Quality Commission
This report describes our judgement of the quality of care at this location. It is based on a combination of what wefound when we inspected and a review of all information available to CQC including information given to us frompatients, the public and other organisations
Ratings
Overall rating for this location Good –––
Are services safe? Requires improvement –––
Are services effective? Good –––
Are services caring? Good –––
Are services responsive? Good –––
Are services well-led? Good –––
BMIBMI ChelsfieldChelsfield PParkark HospitHospitalalQuality Report
Bucks Cross RoadChelsfieldOrpingtonKent
BR6 7RGTel:01689 877855Website:www.bmihealthcare.co.uk/hospitals/bmi-chelsfield-park-hospital
Date of inspection visit: 12 and 13 July 2016Date of publication: 06/12/2016
1 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Letter from the Chief Inspector of Hospitals
Chelsfield Park hospital is one of 59 hospitals and clinics provided by BMI Healthcare Limited. BMI Healthcare is the UK'slargest private hospital group and was formed in 1970. In 1993 after various changes, the group was renamed BMIHealthcare, and its new corporate group became General Healthcare Group (GHG). In 2006 GHG was acquired by aconsortium led jointly by Netcare Limited, a South African healthcare company.
We inspected the hospital as part of our independent hospital inspection programme. The inspection was conductedusing the CQC’s comprehensive inspection methodology. This was a routine planned inspection.
The hospital provides a range of medical, surgical and diagnostic services. The onsite facilities include two operatingtheatres (both with laminar airflow), 36 registered beds spread across two floors, a minor procedure theatre, sevenconsulting rooms and a minor procedure room.
The hospital offers physiotherapy treatment as both an inpatient and outpatient service in its own dedicatedphysiotherapy suite. The imaging department provides plain x-ray, ultrasound, and mobile MRI onsite four days a week,and full field digital mammography.
The dedicated assisted conception unit was not included in this inspection.
Services offered include general surgery, bariatrics, and cosmetic surgery. Diagnostic imaging and endoscopy providediagnostic services. In addition there is limited general medicine provision, oncology and physiotherapy. Patients areself-paying or use private medical insurance. Some services are available to NHS patients through the NHS choose andbook system or spot contracts.
The announced inspection took place between 12 and 13 July 2016, followed by a routine unannounced visit on 21 July2016.
This was a comprehensive planned inspection of all core services provided at the hospital: surgery, outpatient anddiagnostic imaging, both of which include services for children and young people. General medical services areprovided to patients using the same nursing staff, patient rooms and facilities as other patients. For this reason we havenot reported this separately but have included endoscopy and children and young peoples services within surgery.
Are services safe at this hospital
• Improvements were required to ensure a safe service was consistently provided. This included improving thecompletion of the World Health Organisation (WHO) ‘five steps to safer surgery’ checklist, and patient treatment andcare records.
• Infection prevention and control practice in theatres and on the wards was mostly good. The use of personalprotective equipment was not always used by consultants during procedures which may have posed as a risk ofexposure.
• Staff were provided with relevant safety training, including safeguarding vulnerable people. They wereknowledgeable about the hospital’s safeguarding policy and clear about their responsibilities to report concerns.Staff were supported by a designated safeguarding lead. However, the number of staff trained to safeguarding level 3did not meet the recommended guidance.
• Medicine optimisation was managed safely.• Staff were fully aware of the incident reporting process, and there was a formal system for reviewing and learning
such matters. The duty of candour was understood by staff with regards to incidents, which met the threshold ofinforming relevant individuals.
• Nursing staffing levels were organised to ensure the delivery of safe care. The service ensured a Resident MedicalOfficer (RMO) was on duty at all times.
Summary of findings
2 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Consultants with practising privileges took ultimate responsibility for treatment and care.• There were arrangements for communicating patient related information between shift changes, and at times when
the admitting consultant needed to be made aware of their respective patient’s condition.• A national early warning score was used to identify patients whose condition might deteriorate, and transfer
arrangements had been established for patients who required higher levels of treatment or care.
Are services effective at this hospital
• Staff provided care and treatment, which took account of nationally recognised evidence based guidance andprofessional standards. Audit of practices followed a defined programme and included medicine management, andurinary catheters. Action plans were completed and acted upon where audits achieved less than 100% compliance.
• Policies related to service provision at the location were shared with staff and then discussed at the Medical AdvisoryCommittee.
• Pain management and nutritional support was integral to the provision of effective patient care.• There were effective arrangements for reviewing and agreeing consultant practising privileges, and for removing
these when required information was not forthcoming. The revalidation of the consultants and registered nursingstaffs fitness to practise ensured services could be delivered effectively.
• There were nine unplanned returns to theatre during the reporting period April 2015 to March 2016. Unplannedreadmissions within 28 days of discharge for the same period was 18. There were five unplanned transfers ofinpatients to another hospital, which was better than other similar independent hospitals.
• NHS Patients participated in the patient reported outcome measures (PROMS) data collection if they had undergonesurgery for hip or knee replacement and inguinal hernia repair. Insufficient data was available for the period April2014 to March 2015 (reported February 2016) to calculate the average adjusted health gain score for either primaryknee or hip replacement.
• Staff had been provided with training in the Mental Capacity Act 2005 (MCA) and Deprivation of Liberty Safeguards(DoLS) as part of mandatory training. They understood their responsibilities, and were clear about the processes tofollow if they thought a patient lacked capacity to make decisions about their care. The Gillick test and the Fraserguidelines, which related to a child’s capacity to give independent consent to medical procedures, were understoodby relevant clinical staff.
• Patients were provided with information as part of the consent process; however, most patient notes reviewedshowed consent was obtained on the day of treatment.
Are services caring at this hospital
• The hospital participated in the ‘friends and family test’ (FFT). Between October 2015 and March 2016 the hospitalreported 100% of patients would recommend the hospital to their friends and families. The amount of patients whoresponded to the test was moderate (between 30% and 58%).
• The Patient Led Assessments of the Care Environment (PLACE) audit between February 2015 and June 2015 scorefor privacy, dignity and wellbeing was 92%, compared to an England average of 87% for independent acute hospitals.
• Staff recognised patients individuality and ensured they provided sufficient information and emotional support toenable a rapid recovery. Staff were respectful in their administrations, and treated patients and family members withkindness, courtesy and compassion.
Are services responsive at this hospital
• The executive team worked with clinical commissioning groups to determine the range of surgical and other servicesprovided to NHS patients within the surrounding population. Private provision of services reflected the agreed rangeof activities, based on the suitability of facilities, available support and risk criteria.
• An inclusion/acceptance criterion was applied by staff after assessing the patient’s needs. All patients are riskassessed for potential to require extended recovery care. The admitting consultant would make decisions regardingthe suitability of admitting patients with specific needs associated with dementia or learning disabilities.
Summary of findings
3 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• The Resident Medical Officer reviewed patients throughout the day and was available out of hours. Consultantsreviewed their own patients and were required to attend to their patients within a thirty minute journey time, shouldthe need arise. Transfer arrangements were set up in the event of a patient’s condition deteriorating.
• The hospital dealt with complaints and concerns responsively, and learning from such matters was used to improvethe quality of care.
Are services well led at this hospital
• Staff were aware of the expectations of executive team and understood what the vision and values were. They weresupported by an effective and responsive leadership at the executive level, as well as their respective departments.
• Staff enjoyed working at the hospital, and described an open culture and of feeling valued and supported. The recentchanges in management at the hospital were positively acknowledged.
• The Medical Advisory Committee worked with the executive team to ensure the monitoring of quality of services wasreviewed, and challenged where needed. They were responsible for reviewed practising privilege, including fit andproper person information, before agreeing acceptance to use the service.
• Governance arrangements ensured incidents, complaints, audit results and policy development were reviewed andlearning was shared appropriately. However, the risk register, which was a temporary document, was not sufficientlyrobust and lacked evidence of review dates for many of the identified risks.
• Staff were encouraged to continuously learn and improvement was fostered through training and developmentopportunities.
• The availability of capital helped the service to improve and develop services. Recent purchases included a bariatricoperating table, new theatre stack systems and endoscopes.
• As an approved service for Bariatric surgery, equipment was available to support the service, and a designated teamof specialty trained staff worked with the consultant to ensure patients received the required standards of treatmentand care.
• An enhanced recovery program provided a comprehensive rehabilitation program for orthopaedic patients, includingspecialised physiotherapy to achieve earlier mobilisation and discharge.
• The pharmacy manager had implemented a pharmaceutical care plan, and an antibiotic care plan had also beenintroduced to improve practices.
• The service was working toward obtaining accreditation for the endoscopy services with an external body.
Our key findings were as follows:
• The service was led by a dedicated local executive team, supported by loyal staff, who were professional in theirduties and responsibilities.
• The areas in which patients received treatment and care were noted to be clean and well organised. Infectionprevention and control measures were followed by the majority of staff.
• Staffing levels, skills and experience contributed to high standards of care and good patient experiences.• Patients’ needs including effective pain management and nutrition were optimised.
• The standards of leadership and governance arrangements contributed to the effectiveness and responsiveness ofthe services.
• There were sufficient and appropriately skilled staff available to support the safe delivery of patient care.• The nutritional and hydration needs of patients were assessed and catered for.
However, there were areas of where the provider needs to make improvements.
Importantly, the provider should:
• Improve compliance with the World Health Organisation (WHO) ‘five steps to safer surgery’ procedures.
Summary of findings
4 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Improve consultant compliance with the use of personal protective equipment during invasive procedures, in linewith NICE guidelines and BMI policy.
• Improve the completion of patient records to enable the availability of a fully detailed record.• Consider how professional guidelines can be applied to support the safeguarding training further.• Improve the use of the risk register with the incorporation of review dates for all identified risks.• Consider having leaflets available in other languages as well as in English.
Professor Sir Mike RichardsChief Inspector of Hospitals
Summary of findings
5 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Our judgements about each of the main services
Service Rating Summary of each main service
Surgery
Good –––
We rated surgical services as requires improvement forsafe and good for effective, caring, responsive andwell-led.Implementation of the World Health Organisation(WHO) 5 steps to safer surgery checklist was notconsistently completed.Infection prevention and control practices were notalways consistently adhered to.Patient records were not always completed withrequired information.Whilst there were appropriate staffing levels and theskills of staff enabled them to support the delivery ofcare, the level of safeguarding training did not meetbest practice guidelines.Surgical services provided good care and treatment topatients, and had a compassionate and patientcentered approach.Patients received information about their treatmentand were involved in decisions about their care, andtreatment plans. We observed staff maintain patients’respect and dignity at all times.Medical and nursing staff carried out effective riskassessments from pre-assessment through todischarge.Staff followed evidence based care and treatment, andmonitored and reviewed patient outcomes. The staffworked effectively across different disciplines and hadgood links with staff at other BMI hospitals and localNHS services.There was effective and responsive leadership at theexecutive level, and staff commented favourably onthe hospital manager and other senior leadersGovernance arrangements ensured incidents,complaints, audit results and policy developmentwere reviewed and learning was shared appropriately.
Outpatientsanddiagnosticimaging
Good –––
Overall, we rated the outpatients department,diagnostic imaging and oncology services as good.However, we rated safety as requires improvement,and there was insufficient evidence to rate theeffectiveness of services.
Summary of findings
6 BMI Chelsfield Park Hospital Quality Report 06/12/2016
The outpatients, physiotherapy, and diagnosticimaging departments provided a broad range ofservices for both privately funded and NHS fundedpatients. The patients we spoke with werecomplimentary about the care, treatment, and servicethey had received in both departments.Patients we spoke with told us they were treated withdignity and respect. All patient feedback on theinspection was positive. They described the service as‘very good’ and ‘professional’, and described theprocess of making an appointment as easy.The oncology department provided treatment forcancer patients by means of chemotherapy,monoclonal antibodies therapy, and supportivetherapies. The service was provided by Chemotherapyspecialist trained nurses.Staff were competent and worked to nationalguidelines, ensuring patients received the best careand treatment.The culture within both departments was patientfocused, open, and honest. The staff we spoke to feltvalued and worked well together. Staff followedpolicies and procedures to manage risks and madesure they protected patients from the risk of harm.There were short waiting times for appointments.Private patients were seen within one week, and NHSpatients were usually seen within four weeks ofreferral. We found patients could get appointmentswith their chosen consultant and most clinics startedon time.The departments, including oncology, were visiblyclean, well equipped and we observed staff usingpersonal protective equipment (PPE) appropriately.However;Some staff involved in the direct care of children andyoung people had not received the required level ofsafeguarding training. Non clinical staff had not beentrained to identify patients who may become unwellwhilst awaiting their appointment.Nursing staff receiving patient calls to the out of hour’soncology service did not always include anassessment of the patient’s temperature. This is animportant indicator for sepsis diagnosis.Oncology patient notes did not always contain asummary of the multidisciplinary team (MDT) held atthe consultants NHS trust. As a result, staff did nothave up to date information on the patient.
Summary of findings
7 BMI Chelsfield Park Hospital Quality Report 06/12/2016
It was not always clear if equipment used foroutpatient care had been cleaned.
Summary of findings
8 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Contents
PageSummary of this inspectionBackground to BMI Chelsfield Park Hospital 11
Our inspection team 11
Why we carried out this inspection 11
How we carried out this inspection 11
Information about BMI Chelsfield Park Hospital 12
The five questions we ask about services and what we found 13
Detailed findings from this inspectionOverview of ratings 17
Outstanding practice 55
Areas for improvement 55
Summary of findings
9 BMI Chelsfield Park Hospital Quality Report 06/12/2016
BMI Chelsfield Park Hospital
Services we looked atSurgery including endoscopy and services for children and young people; Outpatients & diagnostic imaging, andOncology.
Good –––
10 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Background to BMI Chelsfield Park Hospital
The hospital was opened in 1987, and benefited from a3.5 million pound refurbishment programme during2014/15.
The hospital provides a range of services including;general surgery, bariatric surgery (for weight loss),cosmetic surgery, diagnostic imaging, endoscopy, generalmedicine, oncology and physiotherapy. Patients areself-paying or use private medical insurance. Someservices are available to NHS patients through the NHSchoose and book system, and spot contracts. BMIChelsfield Park has 36 registered beds with all roomsoffering en-suite facilities, television and telephone. Thehospital has two operating theatres (both with laminarairflow), a minor procedure theatre, seven consultingrooms and a minor procedure room.
The following services are outsourced:
• Agency clinical staff
• Catering services
• Instrument decontamination
• Pathology service
• Resident Medical Officer (RMO)
• Blood transfusion
• Laundry services
• Histo-Pathology
• Histology
• Radiation and Laser protection
• Magnetic Resonance Imaging (MRI)
Neither the dedicated assisted conception unit nor any ofthe outsourced service providers were included in thisinspection.
We inspected the hospital as part of our plannedinspection programme. This was a comprehensiveinspection and we looked at two core services providedby the hospital: surgery to include endoscopy andservices for children and young people. Outpatient anddiagnostic imaging to include oncology andphysiotherapy.
The registered manager is the hospital manager and hasbeen in post at Chelsfield Park Hospital for one year atthe time of the inspection; however, they have worked forBMI Healthcare for 26 years.
Our inspection team
Our inspection team was led by Stella Franklin, a CQChospital inspection manager.
The team of seven included three CQC inspectors, aconsultant surgeon, a head of nursing for children andneonates and a senior theatre nurse.
Why we carried out this inspection
We carried out this inspection as part of our annualprogramme.
How we carried out this inspection
To get to the heart of patients’ experiences of care, wealways ask the following five questions of every serviceand provider:
Is it safe?
Is it effective?
Summaryofthisinspection
Summary of this inspection
11 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Is it caring?
Is it responsive to people’s needs?
Is it well-led?
Before visiting, we reviewed a range of information weheld about the hospital, and additional informationrequested from the hospital. We carried out anannounced inspection visit between 12 and 13 July 2016,
and a routine unannounced inspection on 21 July 2016.We spoke with 19 members of staff, including managers,consultants, medical staff, registered nurses, health careassistants, operating department assistants, allied healthprofessionals and administrative staff. We spoke withpatients and relatives, and observed care and treatment.We also reviewed patients’ records
Information about BMI Chelsfield Park Hospital
The hospital provides a range of services to patients atany age, though most commonly patients are aged 16years and over. Between April 2015 and March 2016, 5% ofthe hospital’s overall activity was care and treatmentdelivered to children between the ages of three and 15years old. Of this activity, 1% was delivered to youngpeople aged 16 or 17 years old. The total activity in thesame reporting period for children under the age of threeyears old was also 1%. Adult patients aged 18 -74 yearsrepresented 81%, and those over 75 years represented12% of overall hospital activity respectively during thesame time frame.
There were 5,009 inpatient and day case episodes of carerecorded at the hospital during the period April 2015 andMarch 2016; of those 18% were NHS funded, and 82%funded by other means. NHS funded patients accountedfor 45%, and 24% of patients funded by other meansstayed overnight.
During the same period there were 29,005 outpatienttotal attendances; 11% were NHS funded and 89% werefunded by other means.
Hospital activity during the year April 2015 to March 2016included:
• 3,600 day-case patients;
• 4,595 visits to theatre;
• 9,901 outpatients (first attendees) (NHS 1,089, other8,812);
• 19,104 outpatients (follow up appointments) (1,963NHS, 17,141 other)
Within the two main theatres between April 2015 andMarch 2016; the five most common proceduresperformed were:
• 342 Laparoscopy and therapeutic procedureincluding laser, diathermy.
• 280 Phako-emulsification of lens with implant.
• 161 Hysteroscopy including biopsy, dilation,curettage and polypectomy.
• 143 Multiple arthroscopic operations on knees,including meniscectomy.
• 123 Laparoscopic repair of inguinal hernia.
The most common medical procedures were:
• 247 Diagnostic colonoscopy, including forcepsbiopsy
• 186 Diagnostic oesophago-gastro-duodenoscopy(OGD), including forceps biopsy, biopsy urease testand dye spray
• 159 image guided injection(s) into joint(s)
• 155 Diagnostic endoscopic examination of bladder(including any biopsy)
The controlled drugs accountable officer was the hospitalmanager.
Summaryofthisinspection
Summary of this inspection
12 BMI Chelsfield Park Hospital Quality Report 06/12/2016
The five questions we ask about services and what we found
We always ask the following five questions of services.
Are services safe?• Improvements were required to ensure a safe service was
consistently provided. This included improving the completionof the World Health Organisation (WHO) ‘five steps to safersurgery’ checklist, and patient treatment and care records.
• Infection prevention and control practice in theatres and on thewards was mostly good. The use of personal protectiveequipment was not always used by consultants duringprocedures which may have posed as a risk of exposure.
• Staff were provided with relevant safety training, includingsafeguarding vulnerable people. They were knowledgeableabout the hospital’s safeguarding policy and clear about theirresponsibilities to report concerns. Staff were supported by adesignated safeguarding lead. However, the number of stafftrained to safeguarding level 3 did not meet the recommendedguidance.
• Medicine optimisation was managed safely.• Staff were fully aware of the incident reporting process, and
there was a formal system for reviewing and learning suchmatters. The duty of candour was understood by staff withregards to incidents, which met the threshold of informingrelevant individuals.
• Nursing staffing levels were organised to ensure the delivery ofsafe care. The service ensured a Resident Medical Officer (RMO)was on duty at all times.
• Consultants with practising privileges took ultimateresponsibility for treatment and care.
• There were arrangements for communicating patient relatedinformation between shift changes, and at times when theadmitting consultant needed to be made aware of theirrespective patient’s condition. A national early warning scorewas used to identify patients whose condition mightdeteriorate, and transfer arrangements had been establishedfor patients who required higher levels of treatment or care.
Requires improvement –––
Are services effective?• Staff provided care and treatment, which took account of
nationally recognised evidence based guidance andprofessional standards. Audit of practices followed a definedprogramme and included medicine management, and urinarycatheters. Action plans were completed and acted upon whereaudits achieved less than 100% compliance.
Good –––
Summaryofthisinspection
Summary of this inspection
13 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Policies related to service provision at the location were sharedwith the Medical Advisory Committee and signed off, beforedisseminating across the staff groups.
• Pain management and nutritional support was integral to theprovision of effective patient.
• There were effective arrangements for reviewing and agreeingconsultant practising privileges, and for removing these whenrequired information was not forthcoming. The revalidation ofthe consultants and registered nursing staffs fitness to practiseensured services could be delivered effectively.
• There were nine unplanned returns to theatre during thereporting period April 2015 to March 2016. Unplannedreadmissions within 28 days of discharge for the same periodwas 18. There were five unplanned transfers of inpatients toanother hospital, which was better than other similarindependent hospitals.
• NHS Patients participated in the patient reported outcomemeasures (PROMS) data collection if they had undergonesurgery for hip or knee replacement and inguinal hernia repair.Insufficient data was available for the period April 2014 toMarch 2015 (reported February 2016) to calculate the averageadjusted health gain score for either primary knee or hipreplacement.
• Staff had been provided with training in the Mental Capacity Act2005 (MCA) and Deprivation of Liberty Safeguards (DoLS) as partof mandatory training. They understood their responsibilities,and were clear about the processes to follow if they thought apatient lacked capacity to make decisions about their care. TheGillick test and the Fraser guidelines, which related to a child’scapacity to give independent consent to medical procedures,were understood by relevant clinical staff.
• Patients were provided with information as part of the consentprocess; however, most patient notes reviewed showedconsent was obtained on the day of treatment.
Are services caring?• The hospital participated in the ‘friends and family test’ (FFT).
Between October 2015 and March 2016 the hospital reported100% of patients would recommend the hospital to theirfriends and families. The amount of patients who responded tothe test was moderate (between 30% and 58%).
• The Patient Led Assessments of the Care Environment (PLACE)between February 2015 and June 2015 privacy, dignity andwellbeing scored 92% compared to an England average of 87%for independent acute hospitals.
Good –––
Summaryofthisinspection
Summary of this inspection
14 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Staff recognised patients individuality and ensured theyprovided sufficient information and emotional support toenable a rapid recovery. Staff were respectful in theiradministrations, and treated patients and family members withkindness, courtesy and compassion.
Are services responsive?• The executive team worked with clinical commissioning groups
to determine the range of surgical and other services providedto NHS patients within the surrounding population. Privateprovision of services reflected the agreed range of activities,based on the suitability of facilities, available support and riskcriteria.
• An inclusion/acceptance criterion was applied by staff afterassessing the patient’s needs. High risk patients and thoserequiring complex surgery were not accepted. The admittingconsultant would make decisions regarding the suitability ofadmitting patients with specific needs associated withdementia or learning disabilities.
• The Resident Medical Officer reviewed patients throughout theday and was available out of hours. Consultants reviewed theirown patients and were required to attend to their patientswithin a thirty minute time frame, should the need arise.Transfer arrangements were set up in the event of a patient’scondition deteriorating.
• The hospital dealt with complaints and concerns responsively,and learning from such matters was used to improve thequality of care.
Good –––
Are services well-led?• Staff were aware of the expectations of executive team and
understood what the vision and values were. They weresupported by an effective and responsive leadership at theexecutive level, as well as their respective departments.
• Staff enjoyed working at the hospital, and described an openculture and of feeling valued and supported. The recentchanges in management at the hospital were positivelyacknowledged.
• The Medical Advisory Committee worked with the executiveteam to ensure the monitoring of quality of services wasreviewed, and challenged where needed. They wereresponsible for reviewed practising privilege, including fit andproper person information, before agreeing acceptance to usethe service.
Good –––
Summaryofthisinspection
Summary of this inspection
15 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Governance arrangements ensured incidents, complaints, auditresults and policy development were reviewed and learningwas shared appropriately. However, the risk register was notsufficiently robust and lacked evidence of review dates formany of the identified risks.
• Staff were encouraged to continuously learn and improvementwas fostered through training and development opportunities.
• The availability of capital helped the service to improve anddevelop services. Recent purchases included a bariatricoperating table, new theatre stacker and endoscopes.
• As an approved service for Bariatric surgery, equipment wasavailable to support the service, and a designated team ofspecialty trained staff worked with the consultant to ensurepatients received the required standards of treatment and care.
• An enhanced recovery program provided a comprehensiverehabilitation program for orthopaedic patients, includingspecialised physiotherapy to achieve earlier mobilisation anddischarge.
• The pharmacy manager had implemented a pharmaceuticalcare plan, and an antibiotic care plan had also been introducedto improve practices.
• The service was working toward obtaining accreditation for theendoscopy services with an external body.
Summaryofthisinspection
Summary of this inspection
16 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Overview of ratings
Our ratings for this location are:
Safe Effective Caring Responsive Well-led Overall
Surgery Requiresimprovement Good Good Good Good Good
Outpatients anddiagnostic imaging
Requiresimprovement N/A Good Good Good Good
Overall Requiresimprovement Good Good Good Good Good
Notes
Detailed findings from this inspection
17 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Safe Requires improvement –––
Effective Good –––
Caring Good –––
Responsive Good –––
Well-led Good –––
Information about the serviceBMI Chelsfield Park provides elective surgery to patientswho pay for themselves, are insured or are NHS fundedpatients. Between April 2015 and March 2016, there were4,595 visits to theatre.
Surgical operations included general surgery,ophthalmology, ear, nose and throat (ENT), orthopaedicincluding spinal surgery, urology, vascular surgery,neurosurgery, bariatric service and chronic painprocedures.
The hospital has two operating theatres, both of whichhave laminar airflow ventilation systems (a system ofcirculating filtered air to reduce the risk of airbornecontamination). The hospital has 36 beds spread over twofloors. There are no critical care facilities. In an emergency,the hospital transfers these patients to nearby NHShospitals.
The on-site bariatric facility was recognised as a centre ofexcellence in 2013 and 2015. The service has also recentlybeen re-accredited with the International FederationSurgically Obese award (IFSO). The department has twodedicated extended recovery beds for all level one post-oppatients. Gastric bypass surgery is not performed at thishospital as it does not have the required level two (highdependency) facilities. Gastric bypass surgery is performedat another BMI hospital, and any outpatient appointmentsare conducted at the Chelsfield Park Hospital.
Between April 2015 and March 2016 there were 3,600 daycase and 1,409 inpatient treatments. The NHS fundedapproximately 18% of those treatments.
There were 247 diagnostic colonoscopies, 186 diagnosticoesophago-gastro-duodenoscopies, 159 image-guided
injections into joints and 155 diagnostic endoscopicexaminations of the bladder amongst others during thereporting period. The hospital does not performendoscopic examinations on children and young personsunder sixteen years.
The most commonly performed surgical operations were:
• Laparoscopy and therapeutic procedure including laserand diathermy.
• Phako-emulsification of lens with implant –unilateral;• Hysteroscopy including biopsy, dilation, curettage and
polypectomy;• Multiple arthroscopic op on knee including
meniscectomy;• Laparoscopic repair of inguinal hernia – unilateral• Arthroscopic meniscectomy• Laparoscopic cholecystectomy• Total prosthesis replacement knee joint, with/without
cement
Surgeons carried out the majority of procedures onweekdays, with theatre one also open on weekends andtheatre two also open on Saturday (weekend openingaccording to planned activity).
The hospital carries out surgical treatments for childrenand young people over the age of three years. In the periodApril 2015 to March 2016 there were 209 day casetreatments for children and young people. Children areadmitted to the ward as day case patients and have theirown private room.
The inspection included a review of all the areas wherepatients receive care and treatment. We visited thepre-assessment clinic, the surgical ward, anaestheticrooms, theatres and recovery area. We spoke with sixpatients and reviewed seven patient records. During the
Surgery
Surgery
Good –––
18 BMI Chelsfield Park Hospital Quality Report 06/12/2016
inspection we spoke with 11 members of staff, includingmanagers, medical staff, and registered nurses, health careassistants, operating department assistants, allied healthprofessionals, and administrative staff. Before, during andafter our inspection we reviewed the hospital’sperformance and quality information.
Summary of findingsWe rated surgical services as requires improvement forsafe and good for effective, caring, responsive andwell-led.
• The World Health Organisation (WHO) ‘five steps tosafer surgery’ checklist was not always fullyimplemented.
• During our inspection we looked at a selection ofpatient notes and found there were a number ofsections not completed, for example; incompletepatient details, pre-op checklist incomplete,incomplete anaesthetic record, no pre-op verificationlist completed.
• The number of staff trained to safeguarding level 3did not meet the recommended guidance.
• Consultants did not always follow best practiceguidelines with regard to infection prevention andcontrol.
• Most areas of the service we visited were visiblyclean, with the exception of the sterile room withinthe theatre complex, and there were systems tosupport the safe delivery of care and treatment.
We also found;
• Surgical services provided good care and treatmentto patients. Nursing and medical staff were caring,compassionate and patient centred in theirapproach. Patients felt they received enoughinformation about their treatment and were involvedin decisions about their care. We observed staffmaintain patients’ respect and dignity at all times.Patients reported being happy with their care anddescribed the staff as lovely.
• Medical and nursing staff carried out effective riskassessments from pre-assessment through todischarge. They planned treatment, recovery anddischarge in line with patients’ specific needs.
• Staff followed evidence based care and treatment,and monitored and reviewed patient outcomes. TheStaff worked effectively across different disciplinesand had good links with staff at other BMI hospitalsand local NHS services.
Surgery
Surgery
Good –––
19 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• There was effective and responsive leadership at theexecutive level, and staff commented favourably onthe hospital manager and other senior leaders
• Governance arrangements ensured that incidents,complaints, audit results and policy developmentwere reviewed and learning was sharedappropriately.
Are surgery services safe?
Requires improvement –––
We rated safety as requires improvement. This wasbecause:
• The World Health Organisation (WHO) ‘five steps to safersurgery’ checklist was not always fully implemented,namely ‘time out’ and ‘sign out’
• The number of staff trained to safeguarding level 3 didnot meet the recommended guidance.
• Patient treatment and care records were not alwaysproperly completed.
• We observed the available personal protectiveequipment (gloves) was not used in the anaestheticroom during the insertion of a cannula.
However;
• There were no hospital acquired infections betweenApril 2015 and March 2016.
• Staff understood their responsibilities to raise concernsand report incidents, and there was evidence learningoccurred as a result.
• Most clinical areas were visibly clean and all wereappropriately equipped to provide safe care andtreatment.
• Infection prevention and control practice in theatresand on the wards was good. Infection prevention andcontrol link staff in all departments provided advice andguidance for staff.
• Staff were knowledgeable about the hospital’ssafeguarding policy and clear about theirresponsibilities to report concerns.
• Nursing staffing levels were sufficient to provide safecare. Hospital managers responded quickly to addressany staff shortages.
• A resident medical officer was on duty at all times, andconsultants took responsibility for overseeing thetreatment of patients admitted under their care.
• Staff were provided with safety training.• Staff routinely assessed and monitored risks to patients.
They used the national early warning score to identifypatients whose condition might deteriorate. There wereappropriate transfer arrangements to transfer patientsto a local NHS hospital if required.
Surgery
Surgery
Good –––
20 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Incidents• A robust process was used to consider serious incidents
and never events. A never event is defined as: ‘a serious,largely preventable patient safety incident that shouldnot occur if the available preventative measures havebeen implemented by healthcare providers. Althougheach Never Event type has the potential to cause seriouspotential harm or death, harm is not required to haveoccurred for an incident to be categorized as a NeverEvent’.
• We reviewed the root cause analysis (RCA) investigationreport provided to us for a wrong site regionalanaesthetic block. This event occurred in November2015 and was deemed to be a never event under theNHS England never events list 2015/16.
• The RCA was sufficiently detailed, covering contributoryfactors, chronology, root cause, recommendations andlessons learnt. We saw details regarding the supportprovided for the patient and staff, and the duty ofcandour to be open and honest had been adhered to,although there is no record of a written apology beinggiven to the patient. A detailed action planaccompanied the RCA and lessons learnt hadsubsequently been communicated to staff formally inmeetings, which were minuted.
• The Serious Injury incident, which occurred in January2016, concerned an elderly patient who received a newlens from a batch which had been the subject of a fieldsafety notice on 31 December 2015, and as such shouldnot have been used. The RCA was again sufficientlydetailed, with a comprehensive action plan. The duty ofcandour was adhered to.
• Staff had access to information related to duty ofcandour. This was in the form of the corporate ‘BeingOpen and Duty of Candour Policy’. The policy indicatedtraining on duty of candour was incorporated into riskmanagement training, and staff also had access toe-learning through the National Reporting and LearningService, (NRLS).
• During the reporting period there were 392 clinicalincidents; 90% of those occurred in surgery or inpatientsand 10% in other services. 316 of those were recordedas causing no patient harm, 78 as low and 19 asmoderate and one as severe. When analysed over thereporting period as per 100 bed days the rate of clinicalincidents was over 14% higher than the data we held forother independent hospitals (12 records).
• The Quarterly Clinical Report, 1 January to 31 March2016 was reviewed and we noted Mortality andMorbidity figures were reported on. There had been noin-patient mortalities or deaths within 30 days ofsurgery.
Duty of Candour• From November 2014, NHS providers were required to
comply with the duty of candour, Regulation 20 of theHealth and Social Care Act 2008 (Regulated Activities)Regulations 2014. The duty of candour is a regulatoryduty, that relates to openness and transparency, andrequires providers of health and social care services tonotify patients (or other relevant persons) of certain‘notifiable safety incidents’ and provide reasonablesupport to that person.
• Staff we interviewed were fully aware of the duty ofcandour regulation (to be honest and open) therebyensuring patients received a timely apology andsupport.
• Both RCA’s for the notified incidents provided evidenceof the duty of candour being properly implemented bystaff.
Safety thermometer or equivalent (how does theservice monitor safety and use results)• The NHS Safety Thermometer is a tool for measuring,
monitoring, and analysing patient harms and 'harmfree' care on one day each month. The hospital auditedand monitored avoidable harms caused to patients. Onthe first floor ward we observed a safety thermometerdisplaying venous thromboembolism (VTE)assessments, number of patient pressure sores (0),Meticillin Resistant Staphylococcus Aureus (MRSA) andClostridium difficile (C. diff) swab results, both zero.
• Staff routinely assessed patients for VTE and thescreening rate was 100% for the whole of the reportingperiod from April 2015 to March 2016.
Cleanliness, infection control and hygiene• During the period April 2015 to March 2016 there was no
incidence of meticillin Resistant Staphylococcus Aureus(MRSA), meticillin Sensitive Staphylococcus Aureus(MSSA), Clostridium difficile (C. diff) or Escherichia coli(E-coli) reported.
• The environment in which treatment and care wasdelivered was found to be subject to high levels ofcleaning by suitably trained staff.
Surgery
Surgery
Good –––
21 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• The operating theatres had been subject to a deepclean on 8 and 30 April 2016.
• Our observations of the wards indicated areas wereclean, tidy and well organised.
• In the patient-led assessment of the care environment(PLACE) audit in 2015, the hospital scored 98% forcleanliness, equal to the national average forindependent hospitals.
• Within the theatre area was a sterile store room whichcontained a number of very dusty trolleys and out ofdate equipment. We escalated this to the theatremanager who swiftly organised cleaning and checkingof the trolleys and equipment.
• Staff who spoke with us described the arrangements forcleaning areas, including the process for deep cleaningpatient rooms in the event that a patient subject toisolation precautions had vacated.
• Cleaning equipment in use reflected the recommendednational colour codes, which helped to minimise risks ofcross contamination.
• Guidance for the frequency, methods of cleaning andproducts to be used were available to staff.
• Staff with direct cleaning duties confirmed they hadbeen subject to supervisory training as part of theirinduction, which ensured they understood therequirements of the role.
• Minutes from health and safety meetings reviewed by usindicated incidents related to waste management andcleanliness were discussed.
• Throughout the hospital we observed there was a highlevel of provision to personal protective equipment(PPE), and staff were seen to use it. Items available tostaff included gloves and plastic aprons. However, ananaesthetist was observed in the anaesthetic roominserting a peripheral cannula into a patient withoutwearing gloves, which is contrary to NICE guidance.
• The disposal of used sharps items was generally doneso safely. It was noted a used giving set with bloodcontaminant was protruding from a sharps box in thesluice room of ward two.
• Testing of water on-site for Legionella bacteria wascarried out twice weekly on the wards by housekeeping,and yearly hospital wide checks are undertaken by anexternal specialist company.
• Commodes checked by us were found to be clean.• The director of clinical services was the designated
director for infection prevention and control (DIPC).
• The DIPC was supported by a lead for infectionprevention and control (IPC), and there were designatedlink staff representatives from each clinical area andhousekeeping.
• The IPC lead was undertaking an associated degree tosupport their role.
• The ward link nurse had 10 hours a week designated forIPC activity, including audits and data management.
• Monthly link meetings had commenced in October 2015for IPC, and minutes reviewed by us confirmed a rangeof matters were discussed. For example, audit findings,new policies, sharps awareness, waste management,and training, as well as patient satisfaction feedback.Where actions were required, these were identified witha responsible owner assigned. Subsequent meetingminutes indicated updates on actions were discussed.
• Care setting rapid improvement tools were used tomonitor various IPC elements. We reviewed a number ofreports and noted for example, the first floor wardresults for May 2016 achieved an overall score just below93%. In physiotherapy they scored 70%. The scores forimaging in July 2016 were 100%.
• Various care bundles were expected to be monitored aspart of patient safety, including IPC. Monitoring includedthe insertion of peripheral cannula and ongoingassessment of these, as well as urinary catheters.
• The first floor ward scored 80% in June 2016 audit forthe peripheral cannula care bundle. We noted the sameaudit undertaken in theatres in May 2016 identified only50% compliance for the hand hygiene component of theperipheral cannulation care bundle. An action planaccompanied the report and this was followed up inJune 2016, with a result achieved of 100%.
• Results from IPC audits carried out in theatres and onthe wards were reviewed by us. For example, handhygiene outcomes for theatres in April 2016 showed100% of observed staff were bare below elbows and90% of staff were observed to follow hand hygienepractices. In May 2016 theatre staff scored 80%, for beingbare below elbows, and 90% for hand hygiene.
• The incident reporting system was used to reportpost-operative infections; blisters associated withwound dressings, and positive wound swab culturesassociated with a Surgical Site Infection occurring within30 days or a year for total hip or total knee replacements
Surgery
Surgery
Good –––
22 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• We asked for information about the post-operativeinfection rates, which were noted to be higher thanexpected. The information provided indicated these hadbeen fully reviewed, and no trends had been identifiedto suggest practice related concerns.
• Staff had access to up to date electronic and hard copyIPC policies and procedures, a sample of which wereviewed.
• Mattress audits were undertaken at regular intervals.Where mattresses were deemed to have lost theirimpermeable protection, they were escalated to the IPClead for action. Action taken included destruction andreplacement.
Environment and equipment• Clinical hand basins were not provided in patient rooms.
This did not comply with Health and Building Notice(HBN) 009 (2013). There were clinical hand basinshowever in the two bariatric extended recovery rooms.
• The flooring in some patient rooms was not compliantwith HBN (2013), 0010 part a, as it was carpet and not asheet system type of flooring. The management wereaware and a phased replacement was planned over thecoming year.
• The wards and theatres had mobile resuscitationtrolleys for use if a patient had a cardiac arrest. Recordsshowed staff checked the trolleys daily in line withprofessional guidance to ensure equipment wasavailable and in date. The paediatric resuscitationtrolley was checked on days when paediatric patientswere scheduled and placed in the location where thosepatients would be.
• The theatres had paediatric recovery areas but we weretold the staff did not like to draw the curtains leading toconcerns about privacy and dignity. There was also theconcern the children may be visible to other patientsand/or see and hear things which may disturb them.
• In the patient-led assessment of the care environment(PLACE) audit in 2015, scored 97% against the nationalaverage of 92% for condition, appearance andmaintenance.
• The risk register identified an environmental red ratedrisk within surgery, which concerned the scrub sinks inanaesthetic rooms one and two, which did not have theright taps, and overflows. It has been identifiedadditional funds would be required to correct the scrubsinks. The hospital action plan had scheduledcompletion of this task for September 2016.
• Although generally clean and tidy the theatres andanaesthetic rooms appeared dated and in need ofmaintenance. There were defects to paint on the wallsand scuffs to paintwork. Some wall edging in the scrubsroom was coming away from the wall.
• All decontamination of surgical instruments andendoscopy equipment was carried out off-site.
• Equipment within the hospital was asset tagged andbasic maintenance was carried out by the on-siteengineers. There were two specialised companiescontracted to provide routine checking of equipmentand more in depth maintenance and repair.
• There was an annual validation of the theatres by anexternal contractor. The laminar flow filters werechanged every quarter and the chlorination systemevery six months.
Medicines• On the ward and in theatre, medicines including
controlled drugs, and intravenous fluids were storedsecurely in locked cupboards and inside locked rooms.The lead nurse on duty kept the keys for the controlleddrugs on her person. Staff on the ward kept medicinetrolleys locked and secured when not in use.Pharmacists held BMI private prescription pads securely.
• Staff monitored fridge and room temperatures and tookappropriate action when temperatures were outside therecommended range to store medicines safely.
• Pharmacy and nursing staff monitored and managedstock levels of medicines and controlled drugsappropriately. Staff completed the controlled drugsregisters in line with current national guidance and thehospital policy.
• Out-of-hours the RMO together with a nurse and aporter could gain access to stock items from thepharmacy.
• There were piped medical gases in the theatres andpiped oxygen in each patient room. Portable oxygen wasalso available for patient transfer between ward andtheatre if required.
Records• The hospital used patient records in paper format in the
form of standardised pre-formed booklets. Theseprovided a clear colour coded pathway for staff to followfrom pre-operative assessment to discharge and postcare contact, although these records were not alwaysproperly completed.
Surgery
Surgery
Good –––
23 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• We reviewed seven patient records and found therewere areas not properly completed in three of themsuch as incomplete patient details, incomplete pre-opchecklist and anaesthetic records, and incompletepre-op verification list. Two of the records had just a fewincomplete items but the third record had over 17 areasnot completed.
• A post-operative care 48 hour follow-up telephone callwas part of the inpatient care pathway document.However, we found the calls relating to paediatricpatients were completed but not documented on therecords we reviewed.
• We observed the records store on the second floor wasalways kept locked unless occupied.
• GP patient referrals under the ‘choose and book’scheme were emailed to the admin suite andsubsequently triaged by clinical staff.
• The records of patients not seen for a year were keptsecurely off-site, with protocols in place to ensure theirtimely retrieval if required. The records are scannedwithin 10 days and are accessible via an online systemto key staff.
• There was a BMI audit programme supported by anaudit calendar, which included medical and nursingrecords. The hospital patient health record audit inJanuary, February and March 2016 were 98%, 89% and92% respectively.
Safeguarding• The director of clinical services was the overall lead for
safeguarding adults and children (level 3 trained).Thelead paediatric nurse was the safeguarding lead forchildren (level 4/5 trained) and attends the BromleyLondon safeguarding children’s board (LSCB) four timesa year.
• Figures provided by the hospital stated there were threestaff trained to level 3 and 22 trained to level 2. Theremainder of the staff were trained to level one.
• NHS England provides guidance on the required level ofsafeguarding training. The number of staff trained tolevel 3 did not meet the recommended guidance.
• A paediatric nurse accompanied each child patient whowas undergoing surgery as far as the anaesthetic room,and then attended the recovery area with the child’sparents after the procedure.
• The director of clinical services confirmed the hospitalwas putting measures in place to ensure all clinical staffwere trained to at least safeguarding level 2.
• The director of clinical services confirmed the paediatricconsultants were trained to safeguarding level 3.
• Up to date policies on safeguarding for both adults andchildren were available to all staff on the hospital’sintranet.
Mandatory training• A role-specific mandatory training plan was
automatically assigned to each staff member in the BMIe-learn system. Staff completed most trainingelectronically but this was supplemented by practicaltraining where appropriate.
• At the time of our inspection 90.7% of staff were fullycompliant with mandatory training, which included;adult basic life support, infection prevention and controlamongst many others.
• Individual training records were kept and staff couldaccess this information online.
Assessing and responding to patient risk• Theatre staff used the ‘five steps to safer surgery’ WHO
checklist; this is a nationally recognised system ofchecks before, during and after surgery, designed toprevent avoidable harm and mistakes during surgicalprocedures. However, its use was described asperfunctory by our specialist advisor. On one observedoccasion Step 3 ‘time out’ was not completed prior tosurgery but it was later seen to be documented ashaving been done. A senior theatre practitioner told usthere was no standardisation of practice as clinicianscame from different trusts, and used the WHO checklistin different ways. However staff regularly auditedcompletion of the checklist and results for January,February and March 2016 showed 100% compliance asreflected in the hospital’s quarterly clinical report. Theaudit results did not correspond with our observationsbut may be explained by the completion of a checklistafter the event as witnessed by our inspector.
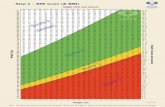
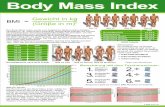
• Patients completed a health questionnaire, whichnursing staff reviewed at pre-assessment to assess thesuitability of patients for surgery at the hospital. Staffconfirmed if the pre-assessment raised concerns theywould escalate the issue to the surgeon or anaesthetistby telephone or email for further assessment. Patientshad to meet certain criteria before the hospital acceptedthem for surgery. For example, the hospital did notaccept NHS patients with a body mass index (BMI)greater than 40 as part of the exclusion criteria withinthe contract.
Surgery
Surgery
Good –––
24 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• We observed a pre-admission consultation in which athorough medical history was taken from the patient.The procedure to be done was fully explained alongwith expected outcomes, aftercare and the importanceof post-op mobility. The patient had bloods and swabstaken in privacy behind a curtain. He was given a safetyleaflet as he left.
• Procedures to monitor patients for any deterioration intheir health were used by staff. The hospital used thenational early warning system (NEWS) after surgery torecord patient observations, and a standard scoringsystem was used across all patient pathways. Staffinitiated the NEWS scoring in recovery and continued iton the ward. Staff we spoke to knew how to escalateconcerns if a patient’s observations deviated fromexpected ranges.
• A paediatric early warning system (PEWS) was used forchildren and young people; although it was noted thePEWS scores were not consistently added up. The leadnurse audited PEWS and informed staff of any poorcompletion.
• Staff had access to detailed guidance, including therequired action to take in the event of a patient,including children deteriorating and requiring transferout of the hospital. The Emergency Transfer of Patientpolicy provided an outline of responsibilities ofconsultants and senior clinical team members.
• An Escalation and Transfer of Patient standard operatingprocedure provided further guidance and instruction tostaff for the transfer of patients needing a higher level ofcare. Such transfer decisions were made subject to theoutcomes of the patient vital signs as recorded on theNEWS. The arrangements for transfer were set up with alocal NHS trust location and the relevant ambulanceservice details and contact numbers were provided.
• The aforementioned policy indicated all registerednurses and health care assistants (HCA) working on theward were required to complete training in Acute IllnessManagement (AIMs) every three years.
• The resident medical officer (RMO) confirmed indiscussion with us the nursing staff would alert them toany concerns about the patients. Assessment andimmediate action would take place and they wouldmake the patients admitting consultant aware. Whilstthe RMO did not know the actual procedure or whichhospital transfer agreement was set up with, they saiddecisions about transfer would be made in conjunctionwith the consultant.
Nursing staffing• The hospital used the BMI Patient Dependency and
Nurse Planning Tool to plan the skill mix of staff fourweeks in advance, with continuous review on a dailybasis. Theatres were currently only planning rosters twoweeks in advance.
• We were told the recruitment of permanent theatre staffwas challenging. The theatre staff establishment wasfifteen whole time equivalent (WTE). This wassupplemented with long term bank staff familiar withBMI practices.
• Paediatric patients were planned admissions to ensurethe required specially trained staff were available.Patients under the age of 12 required two paediatricspecialist nurses.
• We observed a morning ward handover. There wereseven members of staff in attendance and they tooknotes against the handover sheet. Patient names, roomnumber and preferred names to be called were given forall patients. Good details on each patient were givenincluding pain, mobility and allergies. Details of the dayadmissions and tasks were spoken about before thehandover concluded.
• The ‘dashboard’ displayed on the ward showed therequired staff and the actual staff on duty as beingequal.
• We found the induction programme for theatre agencystaff, which had been reviewed and updated by theinterim theatre manager, very comprehensive. Forcontracted staff, depending on the individual, theinduction took place over a three month period. All ofthe staff were consulted and contributed to theprogramme. In the recovery area we also witnessedexcellent support by a recovery practitioner for anItalian nurse who had just obtained her registration pin.
Medical staffing• Consultants with admitting rights were responsible for
overseeing the treatment and care of their patients.They were not based in the hospital but were expectedto review their patients and be available to respond tonursing or medical staff questions or concerns.
• The hospital had an RMO, who was provided through anagency under a corporate agreed contract. The RMOworked on two weekly rotations, covering the service24/7, with sleep-in facilities provided.
Surgery
Surgery
Good –––
25 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• All children were looked after by consultant medicalstaff, whose practising privileges included paediatrics.The consultant in charge was accessible via thetelephone and based within 10 miles of the hospitalaccording to their practising privileges.
• An anaesthetist with paediatric practising privileges wasalso available during the day and on call at other times.
• Verbal handover between outgoing and incoming RMOwas said to cover in-patients and any particularrequirements.
• The RMO confirmed they had been working at thehospital for two months. Their shifts commenced at8am, when they reviewed patients and undertookinterventions, such as blood samples for testing. Theyhad a break of one hour at lunchtime and thencommenced an afternoon shift from 1pm to 6pm. Anevening review of patients according to need took placebefore retiring for the night. Nursing staff were able tocontact the RMO during the night if needed, but theyhad not experienced frequent disturbance. They addedthe experience of the nursing staff affected the amountof disturbance, sighting agency staff as not alwayshaving the same level of experience.
• Staff reported variation in the RMOs, with regard tolanguage skills and understanding of the medicinesused.
• In line with the consultant practising privilegesrequirements the admitting consultants wereresponsible for the patients care management for theduration of their stay. For surgical patients theanaesthetists were also responsible for the patientsprior, during and after surgery. They were expected to becontactable twenty four hours a day, seven days a weekif required, or to arrange cover if they were not available.
Major incident awareness and training• The hospital staff had access to two separate policies to
support the delivery of service. The Business ContinuityPolicy provided strategic and operational informationfor preparedness and response to adverse situations orevents. Roles and responsibilities were defined, alongwith risk assessments and planning arrangements. TheBusiness Continuity Plan defined location relatedinformation, and identified the locations quality and risklead as the nominated person for this area.
Are surgery services effective?
Good –––
We rated effective as good. This was because:
• Staff provided care and treatment that took account ofnationally recognised evidence based guidance andstandards.
• Patients reported staff managed their pain effectivelyand they had access to a variety of methods for painrelief.
• Patients were advised about pre-surgery fasting timesand the hospital aimed to ensure they were kept to aminimum to help prevent dehydration andpost-operative complications.
• There were formal systems for managing and facilitatingthe revalidation of both the consultants and registerednursing staff.
• The hospital held daily ‘10@10’ staff meetings whereinformation from all departments was shared andcascaded to the remaining staff in their respectivedepartments.
However,
• The majority of patient notes reviewed showed consenton the day of treatment, and we were not clear fromrecords if patients had been given sufficient informationto enable them to reflect on the surgical procedurebeforehand.
Evidence-based care and treatment• Staff provided care to people based on national
guidance, such as the National Institute for CareExcellence (NICE) guidelines. We saw evidence ofdiscussion of updated NICE guidelines and drug alertsand recalls in clinical governance meetings.
• There was a hospital program of audits undertaken,which included audits such as theatre medicinemanagement (85% compliance), ward medicinemanagement (96% compliance), urinary catheterinsertion 10 patient sample (100%) compliance. We sawaction plans with dated completion requirements forthose audits with less than 100% compliance.
• Patients over 50 years of age, those undergoing aprocedure requiring a longer than one day hospital stayand those under 50 having a major procedure will allhave a pre-assessment. Patients not meeting thesecriteria may not have a face to face pre-assessment.
Surgery
Surgery
Good –––
26 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Paediatric patients were triaged booked intooutpatients for an initial consultation. Those requiringsurgery were then pre-assessed by one of the paediatricspecialist nurses.
• There were different care pathways for staff to followdependent on the type of clinical procedure, such as theAdult Inpatient Day Case pathway and the Endoscopypathway. They were all documented and evidencebased. Paediatric care pathways were used forpaediatric patients.
• The hospital followed NICE guidelines for preventingand treating surgical site infections (SSIs) using the SSIbundle. There were five SSIs in the reporting period April2015 to March 2016. A review of these did not suggestany evidence to indicate poor hygiene or infectioncontrol practices were a contributory factor to SSIs.
• The hospital was moving towards accreditation by theJoint Advisory Group on gastrointestinal endoscopy(JAG). This is a quality improvement and serviceaccreditation programme for gastrointestinalendoscopy.
Pain relief• Nurses discussed post-operative pain relief with
patients at pre-assessment, and gave them informationleaflets about pain control and anaesthesia. Thisincluded information about different types of pain reliefand pain scoring. We also observed anaestheticconsultants discussing post-operative pain relief withpatients.
• Pain scores were recorded in recovery and the patientswere not discharged from recovery until theanaesthetist had controlled the pain. Nursing staffcompleted the day care pathway which included painassessment and score recording. We spoke to patientswho were happy with their pain control measures.
• Pharmacy staff conducted a daily ward round andreviewed all new patients’ medicine care plans. Theyalso discussed pain control and informed patientsabout take home medications.
• A pain assessment tool featuring smiley faces was usedfor paediatric patients.
Nutrition and hydration• Staff advised patients about fasting times prior to
surgery at pre-assessment and in their booking letter.The hospital aimed to ensure fasting times were as shortas possible before surgery to prevent dehydration andreduce the risk of post-operative nausea and vomiting.
• Intravenous fluids were given as required andmonitored as part of the day adult day case pathway.
• The Malnutrition Screening Tool (MUST) was used aspart of the adult risk assessment documentation.Patients had access to a dietitian if required.
• The hospital offered light snacks and drinks for day carepatients before discharge home.
Patient outcomes• There were nine unplanned returns to theatre in the
year to March 2016. This was a rate of 0.2 per 100 theatrevisits. In the year to March 2016 there were 18unplanned readmissions within 28 days of discharge.This was not high when compared with otherindependent hospitals.
• The rate of unplanned transfers of inpatients to anotherhospital was better than other similar independenthospitals. There were five cases during the samereporting period. These were reviewed and did notindicate any underlying themes.
• NHS Patients participated in the patient reportedoutcome measures (PROMS) data collection if they hadundergone surgery for hip or knee replacement andinguinal hernia repair. PROMS measures the quality ofcare and health gain received from the patient’sperspective. There was insufficient data available for theperiod April 2014 to March 2015 (reported February2016) to calculate the average adjusted health gainscore for either primary knee or hip replacement.
Competent staff• Staff confirmed they received an annual performance
review in October, regardless of start date. They told usthey also had a half year review. Appraisals wererecorded electronically.
• We were told by the interim theatre manager all theatrestaff had appraisals completed between December 2015and January 2016.
• The resident medical officer (RMO) was providedthrough a contractual arrangement with an externalbody. The agency was required to provide evidence oftheir training, competencies and professional records.
• Consultants who worked in the NHS were required tosubmit evidence of their appraisal. For consultants whohad retired from the NHS, we were told their appraisalwas undertaken by the medical director or someoneappropriate. This was managed at head office.
Surgery
Surgery
Good –––
27 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• We saw there was a database for recording whenconsultant appraisals and other essential evidence wasdue to expire, had been received or was overdue.
• Information related to appraisals was submitted to theregional manager as part of the monitoring of requiredstandards.
• The service was actively supporting nurses to achievetheir revalidation and a number of nurses had alreadydone so. A formal database identified when revalidationwas due, and the director of nursing and clinical servicessupported the process.
• Revalidation was part of consultant fitness to practiceand agreeing practising privileges of consultants. Wesaw there was a formal system for managing both theseelements. Documentation was provided for consultantsand held in their personnel files. A designated memberof staff had responsibility for chasing records when due,unless provided by the individual.
• The Medical Advisory Committee (MAC), reviewed newapplicants, and those who were removed as a result ofthe required information not being provided.
• The paediatric lead nurse attends the BMI children’ssteering committee three times a year.
Multidisciplinary working• The hospital held daily ‘10@10’ staff meetings where
information from all departments was shared andcascaded to the remaining staff in their respectivedepartments.
• We observed a theatre briefing involving seven staff, aconsultant surgeon, an anaesthetist and nursing staff.Staff introduced themselves, and were given the chanceto raise any concerns or issues. The consultant led thebriefing, which covered the day’s list, and each patientwas discussed.
• Physiotherapy staff supported effective recovery andrehabilitation, including an appointment atpre-assessment for patients having orthopaedic surgery,and follow up at outpatient clinics. They visited theward daily including weekends. They also had a goodrelationship with the local respite centre. Physiotherapystaff did not attend any MDT meetings but took part inthe ward handovers.
• There were monthly ward meetings during whichinformation from the clinical governance meetings wasshared. Staff signed to indicate they had read theminutes of the meetings, which were also available onthe hospital's shared drive.
• The hospital had a service level agreement (SLA) with alocal trust and a private ambulance service for thetransfer of deteriorating patients from Chelsfield Park.There was also the option of using the standard 999system, depending on the circumstances.
Seven-day services• Nursing staff were available on the ward seven days a
week.• The normal operating hours for theatre one Monday to
Friday were 7am and 9pm Monday to Friday, Saturday8am until 4pm and 8am until 2pm on Sunday. Theatretwo began an hour later during the week and wasclosed on Sunday. Weekend operating was onlyaccording to planned activity. Theatre three’s normaloperating hours were 7am to 11am on Monday,Wednesday and Friday. An on call surgery team wasavailable outside normal working hours.
• Consultants provided 24 hour on call cover for theirpatients or organised cover by a consultant colleague ifthey were not available. Those with patients on theward conducted daily ward rounds.
• A resident medical officer (RMO) was available on site 24hours a day, seven days a week.
• Physiotherapists were available during the working day,evenings and at weekends.
• Pharmacy services were available 8.30am until 4pmMonday to Friday. They provided a service 8.30am -1pmon a Saturday. Basic packs of some take homemedicines were available on the ward in a designatedcupboard. If needed a nurse, the RMO and a portercould access pharmacy for stock items out of hours.
Access to information• The hospital kept records on site for a year after
admission, after which they were sent to an offsitestorage facility. Staff could access paper records storedoffsite within 24 hours. Key staff also had access toscanned records within 10 days of the records beingsent off-site.
• Staff were able to access hospital policies andprocedures via the intranet as well as contact details forconsultants and other staff.
• There was a general information folder within thetheatre area available for all staff to communicate.
Surgery
Surgery
Good –––
28 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Consent, Mental Capacity Act and Deprivation ofLiberty Safeguards• From the majority of the patient notes reviewed we
noted consent for the surgical procedure had beenobtained on the day of the operation, although it waslikely there would have been a verbal discussion withthe consultant earlier in the process. Patient’s consentshould ideally be secured in advance, so they haveplenty of time to obtain information about theprocedure and ask questions. The Royal College ofSurgeons offers the following guidance in its booklet‘Consent – Supported Decision-making 2016’, “Patientsshould be given enough time to make an informeddecision regarding their treatment, wherever this ispossible and not adverse to their health”.
• Patients received information prior to their endoscopyprocedure. This allowed patients to read theinformation and, if understood, give informed consentwhen they came for their procedure. Consent formsappropriately detailed the risks and benefits to theprocedures, and were signed.
• Staff assessed patients’ mental capacity to makedecisions about their care and treatment atpre-assessment. Staff were clear about the processes tofollow if they thought a patient lacked capacity to makedecisions about their care.
• The hospital provided training in the Mental CapacityAct 2005 (MCA) and Deprivation of Liberty Safeguards(DoLS) as part of mandatory training. DoLS are toprotect the rights of people, by ensuring any restrictionsto their freedom and liberty have been fully consideredand authorised by the local authority.
• Staff were aware of the Gillick test and the Fraserguidelines, which relate to a child’s capacity to giveindependent consent to medical procedures. Therewere specific consent forms for children but during ourinspection the paediatric patients were young childrenand consent had been obtained from their parents orguardians.
Are surgery services caring?
Good –––
We rated caring as good. This was because:
• We observed staff treated patients with kindness andcompassion during our visit. Staff maintained patients’dignity and respect at all times.
• Feedback from patients about their care and treatmentwas consistently positive.
• Patients told us they had sufficient information abouttheir treatment, including costs, and were involved inmaking decisions about their care.
• Staff provided good emotional support to patients andtheir relatives. They went out of their way to ensure theirindividual needs were met.
Compassionate care• We observed compassionate and caring interactions
from all staff. Patients were positive about the care andtreatment they received. They described staff as friendly,helpful, caring, considerate, kind and respectful.Patients said, “Staff are lovely, as expected” and“Excellent, all the staff are lovely, in the ward andtheatre. The “anaesthetist’s a charmer”.
• Feedback from parents of paediatric patients was alsopositive. One parent said she especially liked that thenurse who had taken care of her son previously asked totake over from the assigned nurse on the most recentvisit.
• We observed staff referring to patients by their recordedpreferred name. Patients were seen to be treated withdignity and their privacy respected. This view wasconfirmed by the patient’s themselves.
• Both the hospital manager and the director of clinicalservices made time to ‘walk the hospital’ speaking tostaff and patients.
• The hospital participated in the ‘friends and family test’(FFT). During the reporting period October 2015 toMarch 2016 the hospital reported 100% of patientswould recommend the hospital to their friends andfamilies. The amount of patients who responded to thetest was moderate (between 30% and 58%).
• In the Patient Led Assessments of the Care Environment(PLACE) between February 2015 and June 2015, resultsfor privacy, dignity and wellbeing scored 92% comparedto an England average of 87% for independent acutehospitals.
Surgery
Surgery
Good –––
29 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Understanding and involvement of patients andthose close to them• Patients, and their relatives, where appropriate, were
fully involved in the discussion of treatment and care.They were encouraged to actively participate in theprogramme of recovery, and were enabled to do so byhaving open visiting.
• We observed a full and detailed handover from recoverypractitioner to the ward nurse. The patient declaredthey were happy with all of the treatment received.
• The parents of paediatric patients (children and youngpeople) could accompany their child into theanaesthetic room and then were called to recoverywhen the patient awakes.
• The costs of treatment were discussed fully withpatients, including what was covered within the costincluding tests, investigations and follow up visits,should they be required.
• Information related to different payment methods wasavailable on the hospital web site, as well as via thehospital.
Emotional support• There was open visiting on the wards to allow patients
to have emotional support from family and friends.• Staff recognised and responded to patient’s emotional
needs, including the specific needs of children andyoung people in ways that were respectful, kind andreassuring
• As part of the discharge pathway patients could bereferred to aftercare, rehabilitation support groups andcounselling.
Are surgery services responsive?
Good –––
We rated responsive as good. This was because:
• The provider and clinical commissioning groupsdetermined the range of surgical and other servicesprovided.
• The provider planned and delivered services in a waywhich met the needs of the local population. Theservice reflected the importance of flexibility and choice.
• Staff assessed patient’s needs, and the hospital wasable to take the needs of different people into accountwhen planning and delivering services.
• The hospital dealt with complaints and concernspromptly, and there was evidence the hospital usedlearning from complaints to improve the quality of care.
However,
• There was an issue with gynaecological patient flow,reflected in the higher than average day case toinpatient conversions.
Service planning and delivery to meet the needs oflocal people• The hospital developed NHS services in conjunction
with the local clinical commissioning groups (CCGs). TheCCG checked the hospital provided NHS patients withservices in line with agreed quality criteria at quarterlycontract meetings.
• The hospital pre-planned all admissions to allow staff toassess patients’ needs prior to surgery or medical care.They accepted patients for treatments with low risks ofcomplication, and whose post-operative or medical careneeds were met through ward-based nursing.
• Children could visit the ward and meet staff in advance ifthey wished.
• There were no facilities for emergency admissions andcommissioners and the local NHS trust understood this.
• The paediatric lead manages the surgical list to ensurethere are no more than three tonsillectomies per day tomitigate the risk from postoperative haemorrhage.
Access and flow• There were 3194 surgical procedures carried out during
the period April 2015 to March 2016. The hospitalreported it cancelled 15 procedures during that time fornon-clinical reasons; of those 14 patients were offeredanother appointment within 28 days of the cancelledappointment.
• The hospital met the target of 92% of all admitted NHSsurgical patients beginning treatment within 18 weeksof referral to treatment (RTT) during the reportingperiod, apart from May and July 2015 when it fell to88%.
• In the reporting period, 1168 of the surgical procedureswere gynaecological in nature. During the inspectionpre-planning it was noted the overnight stays for NHSfunded patients was 45.4% compared to 24.4% for otherfunded patients, yet NHS patients only accounted for18% of the total number of patients. This was raisedduring the inspection and we were told part of thereason was many of the gynaecological procedures
Surgery
Surgery
Good –––
30 BMI Chelsfield Park Hospital Quality Report 06/12/2016
were carried out during the afternoon or later as thesurgeons completed their NHS hospital work in themornings. Certain post-surgery milestones needed to becompleted before the patient could be discharged,which would often mean for patient safety they wouldstay overnight.
• The hospital’s quarterly clinical report for the quarterending March 2016 reported a total of 52 day case toinpatient conversions, of which 35 were gynaecologypatients. The director of clinical services confirmed noadditional cost was passed on to the NHS in thosecircumstances.
• The two main theatres were open each weekday andtheatre one opened on Saturday and Sunday, andtheatre two opened on Saturday, both according toplanned activity.
• The paediatric surgical list started at 7.30am to enablerecovery during normal working hours and dischargehome the same day.
Meeting people’s individual needs• We heard nursing staff discuss discharge plans at
pre-assessment to ensure the post-surgical patientneeds were properly in place before surgery. This meantstaff were assured when offering surgical admissionsthere would be no unnecessary delays in discharge dueto obtaining specialist equipment or organising a carepackage.
• Patients could access wheelchairs available in the mainreception area. There was a lift available for use by lessmobile patients to enable easy access to the first andsecond floors.
• The physiotherapy department aimed to giveappointments within 48 hours. Each patient was seenfor a pre-operation assessment and current and postoperation needs were discussed.
• Physiotherapy was involved with the enhanced recoveryprogramme, which aimed to enable orthopaedicpatients to be discharged three days after major jointreplacement. They saw the patient twice a day, had agood relationship with the consultant’s and wouldescalate if the patient required longer recovery time.
• There was a variety of menu options available forinpatients and the chef catered for the needs of patientswith special diets, and children’s meal choices.
• All patients we spoke to felt staff had given themsufficient information about their procedure, and wereable to discuss it with their consultant and nursing staff.
Staff gave patients information about their procedure atpre-assessment. This included procedure specificinformation leaflets and a patient information bookletabout their stay. Staff discussed their care in detail andexplained what to expect post-operatively includinglength of stay, and involved patients in their plans fordischarge. Ward staff gave patients a discharge packwith specific post-operative instructions and a copy ofthe discharge letter sent to their GP and district nurse ifrequired.
• The parents/guardians of children undergoing surgicalprocedures were able to accompany them to theatresand recovery areas.
• There was a recent decrease in hospital patientsatisfaction survey scores with meal provision, due to achange in the catering provision. The hospital is awareof the situation and is working with COMPASS, the newprovider, to return the survey scores to theirpre-out-sourced levels.
• In the Patient Led Assessments of the Care Environment(PLACE) for the period February to June 2015 thehospital scored 93% for food, equal to the Englandaverage for Independent Acute hospitals and 96%compared to 94% for ward food.
• The children and young people’s feedback formintroduced by the lead nurse resulted in 27 formsreceived at the time of our inspection. The complaintswere about slow wi-fi, requests for more food choices,more television channels and better ventilation/airconditioning. The children liked the staff, the rooms, thespeed of care and the doctors and nurses.
Learning from complaints and concerns• A formal electronic system was used to collect
complaints information. Each complaint was assigned areference number and a tracker was kept up to datethroughout the subsequent management.
• We reviewed in full five complaints, selected by theinspector. From our review we found there was a robustsystem for managing complaints, which includedacknowledgement, investigation, interim holding lettersand a final response. The latter included details of anyinvestigation and actions taken. Letters contained aformal apology.
• Complaints information was presented to the MedicalAdvisory Committee (MAC) as part of the hospitalmanagement report. We saw for example in the Minutes
Surgery
Surgery
Good –––
31 BMI Chelsfield Park Hospital Quality Report 06/12/2016
of the January 2016 MAC meeting, 24 complaints hadbeen received; the majority (14) were non-clinical inorigin, six of which related to financial or consultantissues.
• Information about complaints discussed in the April2016 MAC indicated 20 complaints had been received,half of which were clinical in origin. Three of these wereattributed to nurse/ HCA or consultant.
• Learning from complaints or concerns wascommunicated to staff through meetings with heads ofdepartments (HODs). Minutes reviewed by us confirmedthis, for example the theatre team minutes (April 2016)reflected feedback was given on the wrong site blockand incorrect lens incidents.
Are surgery services well-led?
Good –––
We rated well led as good. This was because:
• There was effective and responsive leadership at thelocal executive level, and staff commented favourablyon the hospital manager and other senior leaders
• Staff across the service enjoyed working at the hospital.They described an open culture, felt supported andpositive about the recent changes in management atthe hospital.
• Governance arrangements ensured that incidents,complaints, audit results and policy development werereviewed and learning was shared appropriately.
However,
• The risk register lacked review dates for many of theidentified risks.
Vision and strategy for this service• The local strategy underpinned the broader
organisational vision, which was to provide the bestpatient experience, best outcomes and the most costeffective. The local vision had been communicated tostaff
• During our inspection staff told us they were aware andfully engaged with the hospital plan. Information wasshared with staff through the ‘10@10’ gatherings, staffmeetings where information was cascaded anddiscussed and the intranet.
• Operational priorities had been identified for thefinancial year, and included closing the loop onincidents, focus on patient satisfaction related todischarge procedures and food services. Peoplepriorities centred on recruitment, appraisals,revalidation of nurses, internal staff development, andincluded management development.
• In terms of business growth and maximising efficiencies,the executive team had identified priorities whichincluded; the enhanced recovery programme, stockmanagement and capacity, specialty focus, NHS and GPworking and engagement, ambulatory care anddevelopment of outpatients.
Governance, risk management and qualitymeasurement• The hospital had its own governance structure, which
reported into the regional committee. We found therewere ‘Terms of Reference’, which underpinned thepurpose and functions of respective committees.Departments reported through their respectivemeetings into the head of departments,(HODs), andthey in turn, along with the Hospital Clinical GovernanceCommittee, and Hospital Health and Safety Committeereported to the Executive Team. The latter reported intothe Medical Advisory Committee, (MAC).
• Business Development, Operational Performance, andPeople and Performance reported directly to the localExecutive Team.
• The frequency of meetings varied, with weekly localExecutive Team meetings, monthly HODs and RegionalCommittee meetings. All others were indicated as takingplace bi-monthly on documented information providedto us. However, we had conflicting verbal informationabout the frequency of the MAC meetings, the chair ofwhich confirmed took place every two months. Thehospital manager indicated they currently took placequarterly, and minutes reviewed confirmed this. Wenoted in the minutes dated 26 April 2016 the MACagreed to move to bi-monthly meetings.
• The MAC membership was made up of the hospitalmanager, director of clinical services, surgeon,physician, and anaesthetist representatives. There was aconsultant paediatrician who represented children andyoung people on the MAC. This was confirmed by theMAC chair.
• With the exception of MAC meetings, minutes ofmeetings reviewed by us contained standard agenda
Surgery
Surgery
Good –––
32 BMI Chelsfield Park Hospital Quality Report 06/12/2016
items, such as, hospital activity, finance, legislation andcorporate policies, significant events and complaints,and updates to the risk register. Actions had beenidentified with ownership, date for delivery, and thestatus.
• The MAC chair met with the hospital manager prior tothe formal meeting, where they reviewed the agendaand items for discussion. Meeting minutes indicatedpracticing privileges were reviewed, as well as removalsand suspensions. The management report was sharedwith attendees, followed by any other business.Resulting actions were summarised.
• Data from quality reports and dashboards providedoversight in relation to safety, effectiveness andperformance in general.
• Monthly Clinical Governance meetings were attended bymanagers from each area, as well as consultantrepresentative. We reviewed several sets of minutesfrom such meetings and noted there was a detailedagenda, which addressed a wide range of subjects,relevant to governance, safety and quality.
• There were procedures for ensuring only consultantswith approved practising privileges worked at thehospital. We reviewed five randomly selected consultantfiles and saw evidence of checks on fitness to practice,professional indemnity and registration. Appraisals andre-validation was monitored and requested wherere-newal was required. MAC minutes confirmeddiscussion of the removal of individuals where they hadnot provided the required information.
• There was an open culture of staff being able to identifyand raise risks.
• A copy of the risk register was provided to us, along withan archived version. We noted risks were categorisedusing a traffic light system, red down to green. Therewere eight red rated risks out of 44, and the rest wereamber. We did not identify any green rated risks. Thedate each risk was entered onto the register was stated,along with existing controls, if further action wasrequired, the committee with responsibility and keylead. Review dates had not been entered for 32 of therisks. Because of this it was difficult to know whatprogress had or was being made.
• Some risks had been on the register since 2009, andincluded risks associated with slips, trips and falls, andrelated to manual handling. In the further action
section, the commentary indicates further riskassessments to be completed. There were no dates forreview and we did not know if the required action hadbeen taken.
• We noted a risk related to the driveway external to thehospital had been put on the risk register in July 2014.Despite there not being a review date, we observed thedriveway had been resurfaced.
• In our discussion with the quality and risk lead, we weretold the risk register would be changing to a new systemas from December 2016.
• We were told risks were discussed in health and safetymeetings, and we saw examples of minutes accordingly.In addition, we saw evidence of some risks discussed inthe minutes of clinical governance committee meetings.The identified top five risks formed part of the quarterlypresentation and discussion at the MAC meetings.
Leadership of service• There was effective and responsive leadership at the
local executive level, and staff commented favourablyon the hospital manager and other senior leaders. Anumber of staff told us the hospital manager and thedirector of clinical services had made a big difference forthe better at the hospital. The executive team were veryvisible and staff said they were approachable. The sizeof the hospital helped staff to know one another andcontributed to a feeling of ‘family’. Staff told us there wasa high level of comradery.
• There were heads of department (HOD), who werereported to work well together. They providedleadership and support to staff, as well as to theexecutive team. HOD met monthly and reviewed a rangeof subject areas, ensuring they were able to cascadeinformation to their teams.
• A ‘10@10’ meeting took place daily, where a staffrepresentative from each area had the opportunity toupdate the hospital manager and colleagues withrespect to their department. We attended one of theseand witnessed the communication of information, suchas activity, equipment matters, staffing and cover forholidays.
• Clinical department managers had various leadershipresponsibilities. For example, the pharmacy manageroversaw medicines optimisation. They also chaired the
Surgery
Surgery
Good –––
33 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Drug and Therapeutic Committee, and were a memberof the Clinical Governance Committee. This enabledeffective oversight and engagement with staff at alllevels.
• Pharmacy leadership was proactive and ensured safety,improvements to the service, and patient experienceswere at the heart of the departments’ objectives.
• In the absence of departmental leaders, deputy staffhad been given the designated responsibility for leadingtheir teams, and we heard very positive and passionateinformation related to the physiotherapy services. Inparticular, the way the service worked and areas offocus aimed at optimising patient outcomes. Less seniorstaff commented favourably on their line managers anddeputies in the majority of areas. Theatre staff gave verypositive feedback about the new interim theatremanager saying that morale and standards hadimproved and staff were much happier. However, stafffelt the ward manager on the first floor could be difficultto approach and had little respect for paediatricservices.
• We were told the recruitment process included checkson key skills, and interviewers would include someonewith relevant expertise to ensure a fair and consistentapproach.
• Performance which was not consistent with the valuesand expected behaviours was line manged, with actionplans and time scales. Regional Human Resources wereavailable to support where needed, and an on-linesystem was accessible for HOD, where they could betalked through the process if needed.
Culture within the service• Staff felt confident to recommend the hospital as a safe
place, with caring staff. One staff member told us theirrelative had had treatment in the hospital and it stoodout as having caring staff.
• Our observations and discussion with staff indicated aculture of openness, a willingness to report concerns,incidents or errors, and to learn from the subsequentinvestigations.
• An equal opportunities approach was applied torecruitment and selection. Information provided to usshowed the workforce, was in the main (76%) whiteBritish, 16% were of Asian ethnicity, 3.5% Black African,0.80%, Black Caribbean, and 0.80%, Chinese. Otherethnic groups accounted for 2%, and 0.40% were mixedWhite. The remaining were not stated.
• Although a small number of ward nurses and healthcareassistants reported not receiving information aboutincident outcomes, we found detailed evidence whichshowed information was shared through meetings. Wealso saw a folder kept by the first floor ward managercontaining meeting outcomes. Staff were required tosign they had read them. Minutes of meetings were alsoavailable on the hospital intranet.
• The requirements related to duty of candour were metthrough the processes for investigating incidents, andreviewing and responding to complaints. All the staff weinterviewed were able to properly articulate how theduty of candour was to be implemented. Staff were ableto tell us how important it was to be open and honestwith people and to apologise when things went wrong.
Public engagement• Patient-led assessments of the care environment
(PLACE) feedback from the hospitals NHS patients ratesthe hospital higher or equal to the independent hospitalEngland average in every area except for organisationalfood.
• Patients are encouraged to complete feedback formseither in paper format or on-line. The latest publishedresults (Jan – Dec 2015) show 99% of patients rated thequality of care was very good or excellent. All of theother measures were over 90% with the exception ofcatering which was just below at 89.4%.
• A child friendly pain score assessment has beenintroduced using smiley faces. A children and youngpeople’s feedback form has also been introduced.
Staff engagement• The hospital manager told us they ensured they walked
the floor and spoke with staff, asking about thechallenges they had. They also met with the heads ofdepartment (HOD) team and received corporatefeedback with regard to performance.
• Open forums enabled staff to bring matters to theattention of managers, although staff reported it wasdependent on the manager.
• Staff reported having diverse roles, and of having equalopportunities. One administrative staff member told usthey were able to make the role “their own.”Non-national staff were said to be welcomed in thehospital and supported to progress as they so wished.
Surgery
Surgery
Good –––
34 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Exit interviews were arranged either face to face or viaan on-line method. Feedback from recent leavers in thetheatre department had related to the managementand leadership style of the former manager there.
Innovation, improvement and sustainability• The hospital manager told us continuous learning and
improvement was engendered through access totraining and development opportunities. The ethos wasof encouraging studies, and auditing what it looks likefor patients.
• The availability of capital helped the service to improveand develop services. The hospital manager confirmedthey had money to use as they saw fit, for example, thepurchase of bariatric operating table, new theatrestacker and scopes. Other requests over and above thiswould be considered on a risk basis.
• The hospital had been approved for Bariatric surgery,although this was limited to procedures which wouldnot require high dependency care. Equipment tosupport this service was in place, and a designatedteam of specialty trained staff worked with theconsultant to ensure patients received the requiredstandards of treatment and care.
• The enhanced recovery program provided acomprehensive rehabilitation program for orthopaedicpatients, including specialised physiotherapy to achieveearlier mobilisation and discharge.
• The pharmacy manager had been proactive in ensuringmeasures to minimise adverse events and optimisemedicines management were implemented. Thisincluded having a pharmaceutical care plan, modifiedfollowing incident reviews. An antibiotic care plan hadalso been introduced to improve practices.
• JAG Accreditation is the formal recognition anendoscopy service has demonstrated it has thecompetence to deliver against the measures in theendoscopy GRS Standards. The JAG Accreditation
Scheme is a patient centred and workforce focusedscheme based on the principle of independentassessment against recognised standards. The schemewas developed for all endoscopy services and providersacross the UK in the NHS and Independent Sector. Thehospital was not currently JAG accredited but wasworking towards it. They have reported capitalexpenditure investment remains a priority in this area toachieve accreditation. All decontamination ofendoscopy equipment had recently been outsourcedand was carried out off-site.
• The hospital was using new capsule endoscopytechnology to replace more invasive techniques.Capsule endoscopy is a camera housed within a large‘pill’ that is swallowed and takes pictures of a patient’sdigestive system.
• Work had been concluded with regard to identifying andchanging previously admitted patients to day care. Forexample, women having a colposcopy were admitted toan in-patient bed, as were patients having hernias andlaparoscopies. These patients had their procedures asday cases, when previously they had been admitted to abed.
• The hospital was now working towards ambulatorycare, although the MAC had raised concern about onecategory of patient, who they felt this would not beappropriate for.
• The recent upgrade of the OPD had meant there wasnow provision of a minor procedures room, fordermatology procedures.
• The service was continuing to work with external ClinicalCommissioning Groups, GP and Clinical Service Users toensure best experience for the patients. Discussion withrepresentatives of CCG indicated they received a serviceto the expected level and there were no concernsidentified.
Surgery
Surgery
Good –––
35 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Safe Requires improvement –––
Effective
Caring Good –––
Responsive Good –––
Well-led Good –––
Information about the serviceThe outpatient (OPD) and diagnostic imaging (DI)department are located on the ground floor of the hospital.There are seven consulting rooms and a minor operationsroom. There are a variety of OPD clinics every weekincluding gynaecology, cardiology, gastroenterology,paediatrics, dermatology, neurology, and orthopaedics.The main hospital reception is located within the OPD andreceives patients for the OPD as well as those visiting otherareas of the hospital.
Between April 2015 and March 2016, the OPD had 29005attendances. Of these 11% were NHS funded and 89% werefunded by alternative means. Adults between the ages of18 and 74 years of age accounted for 81% of activity, with27,643 OPD visits, and 4,089 (12%) over the age of 74.
During the same period there were 2037 children andyoung people seen in the OPD, represented by 406 (1%)aged nought to two years of age, 1,567 (5%) aged three to15 years of age, and 309 (1%) 16 and 17 years old.
The diagnostic imaging department is located at the farend of the outpatient department. It provides X-Ray,fluoroscopy, ultrasound, mammography (breast screening)and magnetic resonance imaging (MRI) scans. Diagnosticimaging is important in the diagnosis and treatment oftrauma and disease and diagnostic radiographers andradiologists produce and interpret images of the body.Diagnostic Imaging has a separate waiting area.
There is a dedicated Physiotherapy department treatmentfor outpatients as well as access to an off-site hydrotherapypool, providing extensive pre and post-operativetreatments and rehabilitation,
There are separate clinical managers for the OPD,diagnostic imaging, and physiotherapy.
We inspected the outpatient services and diagnosticimaging department on the 12 and 13 July 2016. We spoketo six patients and one family member. We also spoke toeight members of staff including consultants working in theOPD, the department managers, nurses, radiographers, andhealth care assistants.
The oncology department provided treatment for patientsas day cases and so we have included our inspection of thisservice within outpatients. We spoke with the twomembers of staff and two patients.
Before the inspection, we reviewed information provided tous by the hospital. We spoke to clinical commissioners andreviewed external stakeholder information where provided.We observed processes, the environment, care, and theculture, and looked at records during our inspection.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
36 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Summary of findingsOverall, we rated the outpatients department,diagnostic imaging, which included oncology, andphysiotherapy services as good. However, we ratedsafety as requires improvement, and there wasinsufficient evidence to rate the effectiveness ofservices.
• The outpatients, physiotherapy, and diagnosticimaging departments provided a broad range ofservices for both privately funded and NHS fundedpatients. The patients we spoke with werecomplimentary about the care, treatment, andservice they had received in both departments.Patients we spoke with told us they were treated withdignity and respect. All patient feedback on theinspection was positive. They described the serviceas ‘very good’ and ‘professional’, and described theprocess of making an appointment as easy.
• The oncology department provided treatment forcancer patients by means of chemotherapy,monoclonal antibodies therapy, and supportivetherapies. The service was provided byChemotherapy specialist trained nurses.
• Staff were competent and worked to nationalguidelines, ensuring patients received the best careand treatment.
• The culture within both departments was patientfocused, open, and honest. The staff we spoke to feltvalued and worked well together. Staff followedpolicies and procedures to manage risks and madesure they protected patients from the risk of harm.
• There were short waiting times for appointments.Private patients were seen within one week, and NHSpatients were usually seen within four weeks ofreferral. We found patients could get appointmentswith their chosen consultant and most clinics startedon time.
• The departments, including oncology, were visiblyclean, well equipped and we observed staff usingpersonal protective equipment (PPE) appropriately.
However;
• Some staff involved in the direct care of children andyoung people had not received the required level ofsafeguarding training. Non clinical staff had not beentrained to identify patients who may become unwellwhilst awaiting their appointment.
• Nursing staff receiving patient calls to the out ofhour’s oncology service did not include anassessment of the patient’s temperature. This is animportant indicator for sepsis diagnosis.
• Oncology patient notes did not always contain asummary of the multidisciplinary team (MDT) held atthe consultants NHS trust. As a result, staff did nothave up to date information on the patient.
• Information about obtaining leaflets in alternativelanguages was not available, and information toadvise patients how to raise a concern or complaintwas not obviously displayed in public areas.
• The pre-appointment arrangements for seeingpatients who had specific needs related to learningdisabilities or a cognitive impairment were notsufficiently clear.
• Information regarding costs and fees was notsufficiently clear, resulting in patients complainingwhen they received their bill.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
37 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Are outpatients and diagnostic imagingservices safe?
Requires improvement –––
We rated the services as requires improvement for safetybecause:
• Although a suitably trained safeguarding nurse waspresent during the treatment or care of children in theoutpatient department, other staff involved in thetreatment and care of children had not all been trainedto the best practice guidance level for safeguarding.
• We found two handwashing sinks in the diagnosticimaging department to be non-compliant with infectionprevention control guidelines. The sinks were recordedon the hospital’s risk register to be replaced.
• Out of hour’s oncology patient calls did not alwaysinclude assessing and reporting of their temperature,which is an important indicator for sepsis diagnosis.Further, oncology patient notes did not always contain asummary of the multidisciplinary team (MDT) held atthe consultants NHS trust, which meant staff did nothave up to date information.
However;
• Patients received harm-free care and treatment in theoutpatients, physiotherapy, and diagnostic imagingdepartment.
• Staff reported incidents appropriately. Incidents wereinvestigated, and lessons were learned and then sharedacross the hospital.
• Staff had received safety related mandatory training.They knew the procedure for reporting safeguardingconcerns.
• There were enough clinical and medical staff within theboth departments to ensure patients received safe careand treatment.
• The environment in which patients received treatmentand care were visibly clean and safely organised.
• Equipment was well maintained and there was enoughequipment to ensure patients safely received thetreatment they needed.
Incidents• Staff had access to information related to duty of
candour. This was in the form of the corporate ‘Being
Open and Duty of Candour Policy’. The policy indicatedtraining on duty of candour was incorporated into riskmanagement training, and staff also had access toe-learning through the National Reporting and LearningService, (NRLS). The duty of candour is a regulatory dutythat relates to openness and transparency and requiresproviders of health and social care services to notifypatients (or other relevant persons) of ‘certain notifiablesafety incidents’ and provide reasonable support to thatperson.
• Between April 2015 and March 2016 there were 22clinical incidents and 15 non-clinical incidents. Theywere rated as low or no harm incidents. This is lowerthan the average of other departments in similarhospitals.
• Staff knew how to report incidents and felt confident indoing so. The quality and risk lead entered these formsonto the hospital’s electronic system.
• All of the staff we spoke to understood ‘duty of candour’and were able to describe its principles related toadverse events or serious incidents.
• Staff received regular feedback on incidents at monthlyteam meetings. Feedback included incidents from theirdepartment, from the wider hospital and from otherhospitals in the group. Staff described the departmentas having a learning culture around incidents.
• There had been no reported incidents to the CareQuality Commission under the Ionising Radiation(Medical Exposure) Regulations 2000 (IRMER) Regulation4(5). The regulation is intended to protect patients fromunintended, excessive, or incorrect medical exposure toradiation.
• A clinical incident occurred within oncology inNovember 2015. The patient began to deteriorate andwas eventually transferred to a local NHS hospital. Theroot cause analysis (RCA) we reviewed was sufficientlydetailed and identified the main causes of the incidentas poor communication of test results. The patient’sfamily complained and this was appropriately handled.In accordance with the duty of candour, a final letterwas sent with an apology, an explanation, and details ofthe investigation and actions taken.
Cleanliness, infection control and hygiene• The director of clinical services was the designated
director for infection prevention and control (DIPC).
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
38 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• The DIPC was supported by a lead for infectionprevention and control (IPC), and there were designatedlink staff representatives from each clinical outpatientarea and housekeeping.
• The IPC lead nurse was embarking on academic andprofessional studies to support their role.
• All staff had access to infection prevention and controlguidance, which reflected best practice guidelines andlocal standards.
• We observed the clinical and public areas visited werevisibly clean and tidy, and were safely organised.
• Domestic staff had responsibility for cleaning clinicrooms daily and had guidelines with respect to therequired standards. Colour coded cleaning equipmentwas provided for the various tasks, and areas of thehospital, which reflected national guidance. We sawcompleted checklists indicating areas had beencleaned.
• The hospital's Patient-Led Assessments of the CareEnvironment (PLACE) scores were the same as theEngland average for cleanliness, at 98%.
• Staff told us each nurse and healthcare assistant hadresponsibility for an allocated clinical room. Theycompleted a weekly cleanliness audit and ensured eachclinical room was stocked with the correct equipment.We were shown audits, which indicated the monitoringof the required standards.
• We checked six consulting rooms and found all thecurtains were visibly clean and had labels with the datewhen they were last changed.
• Staff had access to guidance for cleaning equipmentused by patients. We found ‘I am clean labels’ werebeing used across the department to indicate whenequipment had been cleaned and was safe to use.
• There were hand washing facilities and hand geldispensers in every consulting room. We did find thesinks in rooms one and two in diagnostic imaging werenon-compliant, as they did not have elbow operatedtaps. These were on the hospitals’ risk register. This hadbeen incorporated into the budget for the next financialyear and would be undertaken early in the financial yearcommencing Oct 2016.
• The risk register identified two environmental red ratedrisks, one of which related to carpets in oncology, andthe potential for contamination if medicines were
spilled. At the time of our inspection we found thecarpet had been replaced with hard flooring, which metIPC standards, in that the floor could be easily cleanedand maintained.
• Care setting rapid improvement tools were used tomonitor various IPC elements. We reviewed a number ofreports and noted for example, in physiotherapy theyscored 70%. The scores for imaging in July 2016 were100%.
• A hand hygiene observational audit conducted in May2016 indicated 80% of the staff observed were barebelow the elbows and met hand hygienedecontamination standards. The staff we observedduring our inspection were all bare below the elbows
• Staff complied with infection control and preventionpolicies, using supplied personal protective equipment(PPE), such as gloves and aprons. They followed bestpractice guidance with respect to waste disposal.
• Clinical and domestic waste, as well as ‘sharps’ weredisposed of in the correct manner. There were separatewaste and sharps bins in all of the clinical rooms. Sharpsbins were found to be less than half full and dated.
• All staff in the OPD and diagnostics department hadcompleted their mandatory training on infectionprevention and control.
Environment and equipment• Adult and children’s resuscitation equipment was
available in tamper proof trolleys. The trolleys andequipment on the top of the trolley was checked daily.Diagnostic imaging shared the resuscitation equipmentwith the outpatients department but the equipmentwas not stored near the midway point of the two areas.This meant staff in diagnostic imaging had further totravel to access the resuscitation equipment in anemergency than was necessary.
• Staff told us they had all necessary equipment toprovide safe and effective treatment.
• Specific specialised items of equipment, such as thebariatric hoist was demonstrated and practiced inmanual handling training. The manual handling trainingwas facilitated by an experienced on sitephysiotherapist.
• The minor operations room had the necessaryequipment to provide safe and effective treatment. Itshared the resuscitation trolley with the main OPD.
• Radiology staff had access to appropriate protectiveclothing to prevent any harmful exposure to radiation.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
39 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Signage was actively used to alert the public and staffwhen radiation was in use.
• We were told the hospital outsourced services inrelation to Radiation and Laser protection from a localNHS Foundation Trust. The services they providedincluded overseeing safety in the diagnostic imagingdepartment, and compliance with regulations. Staff toldus these individuals were always available for advice.
• We found the viewing room in the diagnostic imagingdepartment was not fit for purpose. Staff told us the airconditioning unit had been broken for 18 months.Frequent high temperatures in the room caused a risk tothe equipment’s performance in the viewing room andmade the working environment unbearable at times.This was on the hospital’s risk register but noreplacement had been approved. Whilst not in a clinicalarea, the carpet in the viewing room looked old anddirty despite being recently cleaned. The manager hadasked for a replacement but was still waiting for aresponse.
• In the OPD, staff felt the space for administrative dutieswas limited. In diagnostic imaging, there was a lack ofadequate desk provision for staff to work safely.
Medicines• There was safe management and storage of medicines
in locked cupboards in the outpatient and diagnosticimaging department. Medication refrigeratorstemperatures were checked daily and were withincorrect limits. Ambient temperatures of rooms wheremedicines were stored were checked and recorded.These measures ensured the medicine’s potency. Nocontrolled drugs were kept in the department.
• The diagnostic imaging department kept flammablemedicines in a lockable fireproof cabinet.
• Emergency drugs were kept on the resuscitation trolleyand were checked daily.
• Diagnostic imaging had a separate emergencyanaphylaxis drug kit. Anaphylaxis is a life threateningallergic reaction that requires immediate treatment.
• Prescription pads for each clinic room were kept in alocked drawer by the nurse in charge and were auditedat the end of every clinic. This ensured that noprescriptions went missing. Doctors wrote prescriptionsat the time of the patient’s consultation.
• The oncology department had their own secure storageand drug fridge, which was properly monitored and
audited. Chemotherapy drugs were ordered from theon-site pharmacy after obtaining the patient’s bloodtest results. Any take home drugs were also provided onthe day.
• Oncology medicines requiring cold storage were kept inoncology in a locked fridge. Records showed nursingstaff checked the temperature each day to ensuremedicines were stored at a safe temperature. Nursingstaff were aware of actions to take if the fridgetemperatures were not within an acceptable range.
• In the event of chemotherapy not being used for apatient because of their health status, it was disposed ofby pharmacy and no charge was applied to the patientwhether insurance or self-funded.
• Chemotherapy spillage kits were available in theOncology department and staff used designated purplebins for chemotherapy waste.
• The on-site pharmacy was in the process of developingan e-prescribing system for chemotherapy drugs, whichthey believed would lead to even better safety bystandardising the way the different trust oncologistsprescribed.
Records• Records for NHS patients were stored securely in the
medical records department. The notes were availablefor clinics and then taken back to medical records.
• All staff had separate logins for accessing any patientidentifiable information. This was mandatoryrequirement by BMI healthcare.
• Staff told us records for patients were always availablefor clinics. Information provided to us prior to theinspection was there had not been any times whenpatient notes were not available for their consultation ortreatment for the period January to March 2016.
• Individual consultants retained private patient’s noteswith copies held in medical records. Consultants wererequired to adhere to information governance policies.
• Physiotherapy notes of the patients using the off-sitehydrotherapy pool were transported in a lockable box,which was fire and water proof. The notes were taken ina private car with the physiotherapy staff to the poolwhere the box was unlocked. The notes remained theresponsibility of the physiotherapy staff for the durationof the session before the box was relocked and returnedto the hospital for filing.
• We were provided with information in advance of theinspection indicating ‘Choose & Book’ NHS notes were
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
40 BMI Chelsfield Park Hospital Quality Report 06/12/2016
delivered to the department the day prior to a clinicappointment and were returned the following day.Notes for follow up appointments after surgery wereavailable on request from onsite medical records.
• All imaging, histology, and blood results were availableelectronically. Consultants could be provided withpaper copies if they required.
• Diagnostic imaging used a picture archiving andcommunication system (PACS) which meant imagescould be viewed on any computer connected to theintranet in all BMI hospitals and via a remote accessfacility. This meant the radiologists could report quicklyin case of an emergency. PACS is a nationally recognisedsystem used to report and store patient imagessecurely.
• Clinic letters were kept on site for three months, andthen scanned for electronic storage. This meant therewas a good system enabling retrieval of informationshould this be required at a later date.
• We were shown audits within oncology to track theeffectiveness of out-of- hour’s patient calls, and wenoted the patient’s reported temperature was notalways recorded. This was an important indicator forsepsis diagnosis.
• Multidisciplinary team (MDT) meetings for oncologypatients did not take place at the hospital as theconsultants tended to discuss treatment plans at theirmain NHS hospitals. A summary of the MDT meetingwas not always written in the clinic review recordtemplate, meaning nursing staff did not have up to dateinformation. We were told the hospital was currentlyworking with the consultants and surgeons to establisha more robust mechanism for this.
Safeguarding• The director of clinical services was the overall lead for
safeguarding adults and children (level 3 trained).Thelead paediatric nurse was the safeguarding lead forchildren (level 4/5 trained) and attended the BromleyLondon safeguarding children’s board (LSCB) four timesa year.
• The hospital safeguarding lead was available shouldstaff need advice or guidance, and staff knew who thesafeguarding leads were for adults and children. Theyknew their responsibilities regarding safeguarding andknew how to escalate concerns.
• Up to date policies on safeguarding for both adults andchildren were available to all staff on the hospital’s
intranet. These reflected the ‘safeguarding children andyoung people: roles and competences for health carestaff Intercollegiate Document, 2014'. Level 3 trainingwas required of clinical staff, including diagnostic staffand physiotherapists working with children, youngpeople and/or their parents/carers and who couldpotentially contribute to assessing, planning,intervening and evaluating the needs of a child or youngperson and parenting capacity where there aresafeguarding/child protection concerns.
• Figures provided by the hospital stated there were threestaff trained to level 3 and 22 trained to level 2. Theremainder of the staff were trained to level one.
• NHS England provides guidance on the required level ofsafeguarding training. The number of staff trained tolevel 3 did not meet the recommended guidance.
• We were told staff received level one adult and childrensafeguarding training as part of their mandatorytraining, at induction and two yearly intervals thereafter.Department managers had to undertake level twotraining. A programme to train all nurses to level twowas due to be implemented. Staff told us that levelthree trained staff were on duty caring for children whenthey attended the hospital.
• During the inspection we did see a child in clinic whohad received an X-Ray and had bloods taken for testing.None of the staff who saw this child had level threesafeguarding, which did not reflect the intercollegiateguidance.
• The department’s clinical manager told us there hadbeen no safeguarding issues in the 18 months they hadbeen in post.
• Staff knew about what action to take if they suspected apatient may be or at risk of abuse. One nurse told usthey had arranged an unplanned overnight stay for apatient who they felt was unable to follow preprocedure instructions.
• The hospital had an up to date chaperoning policy. Staffwere available for any patient requiring chaperoning.Records of chaperoning were kept in a log, and includedin patient’s notes.
• Staff told us they felt confident challenging anyconcerning practices or behaviours.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
41 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Mandatory training• We were told a role-specific mandatory training plan
was automatically assigned to each staff member in theBMI e-learn system. Staff completed most trainingelectronically but this was supplemented by practicaltraining where appropriate.
• Mandatory safety training was required to be completedby all staff. This included for example health and safety,manual handling, PREVENT (Protecting people at risk ofradicalisation), infection prevention and control andequality and diversity.
• The outpatient’s clinical manager showed us that all thestaff in the department were up to date with theirmandatory training. In diagnostic imaging, twomembers of staff were newly employed and were yetto completed their mandatory training, and 95% of theoncology staff had completed their training. Informationprovided to us indicated 100% of physiotherapy staffhad received their mandatory safety training.
• Training was automatically monitored online and eachmember of staff had a password protected trainingaccount. Staff received automated reminders when amodule was due for completion and the managerregularly reviewed the staffs’ compliance withmandatory training.
• Training could be delivered through e-learning andface-to-face sessions. Staff reported that they were givensufficient time and support to complete their training.
• It was mandatory for staff working with children to haveeither paediatric Basic Life Support (BLS) or ImmediateLife Support (PILS), and this had been provided to 100%staff. Three staff had undertaken Advanced PaediatricLife Support.
Assessing and responding to patient risk• Staff had access to detailed guidance, including the
required action to take in the event of a patient,including children deteriorating and requiring transferout of the hospital. The Emergency Transfer of Patientpolicy provided an outline of responsibilities ofconsultants and senior clinical team members.
• When patients arrived in the reception area, receptionstaff greeted them. The department manager told us ifthe staff on reception had concerns that a patient was atrisk, they would immediately alert a nurse who would
assess the patient. Further, reception staff had receivedtraining in basic life support and were aware of theprocedures to follow when alerting staff to concernsabout the wellness of patients.
• Nursing staff told us if a patient was identified as havingany health related risks then they would move thepatient from the main reception area and a trained staffmember would remain with the patient.
• Staff told us they did not routinely take patient’s baseline observations, as patients didn't usually require this.However, they would record the patients observations ifrequested to do so, or if they assessed the patientas unwell. They would then report this to the consultantimmediately.
• Staff in diagnostic imaging confirmed they would notcarry out a scan on a female patient of childbearing ageunless the patient had signed a declaration confirmingtheir pregnancy status. This was not subject to any auditat the time of our visit.
• The imaging department used an adapted safetychecklist, as outlined in the World Health Organisation(WHO) Surgical Safety Checklist and the Safe Surgeryinitiative. The imaging department had carried out anaudit on WHO check list compliance.
• In consulting rooms, the WHO checklist wasincorporated within the patient pathway. Thesepathways had been used since the minor treatmentroom was first used. Audit forms part of the monthlymedical records audit going forward.
• The hospital had a trained emergency ‘Crash’ team, allof whom carried a bleep to respond to emergencies inthe department. Alarm activation was via the telephoneor from a button in each clinic room.
• There were two standard operating procedures (SOPs),one for cardiac arrest in imaging and the other forcardiac arrest for MRI.
• We observed all clinic rooms and toilets had emergencyalarm button and pull cords.
• The department had regular practice scenarios onresponding to emergencies, staged by an outsidecompany. Staff received no warning ahead of thesescenarios, in order to make them as realistic as possible.Consulting rooms held the last scenario on 23 May 2016,and this was a paediatric scenario.
• If a patient required urgent transfer to an NHSEmergency Department then they would use the 999system to call an ambulance and alert the receivinghospital.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
42 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Nursing staffing• There were sufficient nursing staff to meet the needs of
patients attending the department. Staff told us they feltstaffing levels were adequate for the number of clinicsrunning in the department.
• The department was fully staffed with both qualifiednurses and healthcare assistants. There were 3.57 wholetime equivalent (WTE) registered nurses, and 2.37 WTEhealthcare assistants. There were always a minimum oftwo qualified nurses on duty. Healthcare assistants(HCAs) assisted in clinics. The manager told us theycovered vacancies with their pool of 11 permanent andbank staff and never have to use agency staff. No bankor agency staff nurses or healthcare assistants wereused in outpatient departments in the reporting period(Apr 15 to Mar 16).
• Senior staff nurse completed staffing rotas four weeks inadvance and there was a mix of early and late shifts, inresponse to planned clinics.
• The department had a trained paediatric nurse forpaediatric clinics, trained to level three for Children’sSafeguarding, and we saw the rotas to confirm thisarrangement.
Medical staffing• There were procedures for ensuring only consultants
with approved practising privileges worked at thehospital. We reviewed five randomly selected consultantfiles and saw evidence of checks on fitness to practise,professional indemnity, and registration.
• Every clinic was run by a consultant who saw eachpatient on their specific list.
• We reviewed records, which showed the namedconsultant for each clinic had been available. Staff wereable to tell us of an incident when a consultant wasunable to attend their clinic due to sickness and staffwere able to get another suitably qualified consultant tocover at short notice.
• The manager kept an audit of clinics that started lateand would fill in an incident report if they did not startwithin 30 minutes of their scheduled time. We sawrecords, which showed the clinics in the majority ofinstances started on time.
• We spoke to patients who all said they had been able toget an appointment with their chosen consultant.
• The resident medical officers (RMO) were supplied by athird party, and as such information about the RMO,including their CVs and training records were provided
by the agency. The Director of Clinical Services and aConsultant Anaesthetist who was a member of theMedical Advisory Committee (MAC) reviewed the CV’sfrom the agency and individual applicants forassurances that training had been undertaken. It wasthe agencies responsibility to ensure all RMOs hadcompleted their mandatory training; however, thelocation checked the agency documentation to ensurethey were fully up to date. We were told a full corporate /hospital induction for all new RMO’s was undertaken atthe start of their contract at site.
Major incident awareness and training• The hospital staff had access to two separate policies to
support the delivery of service. The Business ContinuityPolicy provided strategic and operational informationfor preparedness and response to adverse situations orevents. Roles and responsibilities were defined, alongwith risk assessments and planning arrangements. TheBusiness Continuity Plan defined location relatedinformation, and identified the locations quality and risklead as the nominated person for this area.
• A copy of the Business Continuity Plan was available inthe main reception. It included Action cards, whichexplained roles in the event of a wide variety ofincidents and scenarios, but was not specific toindividual staff or departments.
• We looked at records to show that back-up generatorswere serviced and tested regularly.
• Staff knew what to do in the event of a fire or emergencyevacuation. Each department had a fire warden. Anevacuation drill in association with the local Fire andRescue Service had recently been conducted.
• Radiation incidents, should they occur were expected tobe reported and managed in accordance with safetyprocedures.
Are outpatients and diagnostic imagingservices effective?
We do not currently rate the effectiveness of the outpatientand diagnostic service.
• The outpatients and diagnostic imaging departmentwere providing effective treatment for patients. Patientsreceived diagnostic imaging results promptly.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
43 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Treatment was always consultant led and used evidencebased best practice from the World Health Organisation(WHO), the National Institute for Health and CareExcellence, and the Royal Colleges.
• All staff had an appraisal in the past year, and thehospital supported them through the Nursing andMidwifery Council’s (NMC) revalidation process.
• Systems were set up for revalidation of medical staff andfor the effective management of doctors’ practisingprivileges.
• Staff knew their responsibilities in relation to consentand the Mental Capacity Act (2005).
Evidence-based care and treatment• Clinical staff knew of and used of the relevant NICE
guidelines for their department along with relevantRoyal College guidelines. These guidelines could beaccessed easily through the intranet, such as guidancearound consent, resuscitation and clinical procedures.
• Both departments undertook numerous clinical andnon-clinical audits. These included infection preventionand control, cleaning, hand hygiene, medicinesmanagement, waiting times, revenue, image quality,WHO surgical checklist (a system of checks for ensuringsafe management of surgical procedures), and X-Rayaudits. Results of these audits were fed back to bothstaff and senior management. We saw that where areasneeded to improve action plans were agreed, and thesewere followed up at subsequent audit.
• A recent audit of clinic start times in OPD resulted in twoconsultants being referred to the hospital manager, witha view to making improvements.
• The radiation protection supervisor (RPS) annuallyreviewed the diagnostic reference levels and these werequality assured on a daily/weekly/monthly basis. Allreference levels were established at the beginning of theyear by the radiation protection advisor, the RPS andhead of department. Documented evidence of qualityassurance and reference levels were maintained.
• The service had one BV Libre image intensifier and acorporate policy/ionisation radiation policy, as well as alocal standard operating procedure for the handling ofthe image intensifier.
• An audit of the use of markers (a point of reference or ameasure to aid interpretation) in images produced indiagnostic imaging resulted in the purchase of newmetal markers and all images were subsequently to beapproved by the imaging manager.
• All standard operating procedures (SOP) withindiagnostics were within review dates. A new SOP forminor treatment room in use, ratified at ClinicalGovernance meeting. Any new SOP’s, local or corporatewere cascaded to staff and a signature sheet kept.
• Staff working in the minor operations room used anadapted WHO surgical checklist, which met nationalguidelines. We saw examples of these having beencompleted in records reviewed.
Pain relief• Staff told us that external requests to the outpatients
department for pain relief were infrequent. They told usthey would contact the patient’s consultant or referthem to their GP if necessary. The Resident MedicalOfficer (RMO) was also available in the event of a patientrequiring a review of their pain management.
• Consultants discussed pain management within theconsultation process for patients who were going to bebooked in for a surgical procedure.
Nutrition and Hydration• Staff advised patients about fasting times prior to
surgery at their pre-assessment and provided additionalinformation in their booking letter.
• During oncology treatment nutritional needs were metwith the provision of hot/cold beverages as well assnacks and light meals.
• There was access to water and other drinks could beprovided if required.
Patient outcomes• Staff told us diagnostic test results were available
promptly. Most tests were available electronically andcould be viewed on terminals in each consultationroom. The diagnostic imaging manager told us reportswould be completed within a few minutes when aradiologist was on duty. This meant that in most casesthe patient’s results were available during theconsultation.
• When radiologists were unavailable, they had a 48-hourstandard for completing reports. If a report was requiredurgently then they had a rota of on call radiologists thatcould either attend the hospital or report remotely.
• The hospital did not participate in imaging accreditationschemes or improving quality in physiological servicesscheme. The Imaging Services Accreditation Scheme(ISAS) is a patient-focused assessment and
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
44 BMI Chelsfield Park Hospital Quality Report 06/12/2016
accreditation programme designed to help diagnosticimaging services ensure their patients consistentlyreceive high quality services, delivered by competentstaff in safe environments.
• Patient outcomes in physiotherapy were monitored byrecognised outcome measures such as range ofmovement, pain scores and the quality of life measuresin order to establish the effectiveness of treatment.
• The standard national tool used throughout thephysiotherapy arm of the company was the EQ5D. Thisis a key measure chosen by the Department of Health inEngland in the current patient reported outcomesmeasures (PROM's) programme. It has been used since2009 to evaluate and benchmark various electivesurgical pathways, such as total knee replacement, totalhip replacement. We were told the outcome data wascomparable to the NHS.
Competent staff• Nursing staff could operate across all the speciality
areas allowing them to cover any adult clinic. There wasa paediatric nurse for children’s clinics. There were tworadiographers who had additional training inmammography.
• An outside company supplied the mobile MagneticResonance Imaging (MRI) scanner. The diagnosticimaging department did not staff the scanner, butmanaged the scanner’s appointments.
• There was a radiation protection supervisor on site, whowas also a senior radiographer. They had a certificate ofcompetence and had attended the required training.
• All staff had received an appraisal in the past 12 monthsexcept newly employed staff. Appraisals were reflectionon the previous year’s performance against setobjectives, new objectives for the year ahead and anytraining requirements staff felt would benefit theirdevelopment.
• New members of staff had completed both a hospitaland department induction programme, to give anoverview of the policies and procedures. They hadsupernumerary time and reported feeling supported intheir new roles by all members of staff. New members ofstaff were required to complete mandatory training.
• We were told the RMO agency was asked to provideevidence of their training. With regard to resuscitation,
although the RMOs undertake this training with theiragency prior to arrival at the location, the RMO wasincluded in all resuscitation scenarios to ensure theywere familiar with the team and equipment available.
• The department was aware of the importance of theNMC’s revalidation of nursing staff and the staff reportedfeeling supported in the process. Revalidation ensuresthat nurses are practising safely.
• Many staff had worked in the hospital for a long timeand described a good working relationship with theconsultants. They felt confident in helping patientsclarify points about their treatment with theconsultants. Newer staff said they had felt welcomed byboth the medical and nursing staff.
• Paediatric nurses within the hospital supported childrenattending for x-ray and the corporate Children andYoung People’s policy was available to reference andadhere to.
• Revalidation was part of consultant fitness to practiseand agreeing practising privileges of consultants. Wesaw there was a formal system for managing both theseelements. Documentation was provided for consultantsand held in their personnel files. A designated memberof staff had responsibility for chasing records when due,unless provided by the individual. The Medical AdvisoryCommittee (MAC), reviewed new applicants, and thosewho were removed as a result of the requiredinformation not being provided.
• Medical Advisory Committee minutes confirmeddiscussion of the removal of individuals where they hadnot provided the required information.
• The reporting radiologist reported on the patientprocedure and a copy went to the referring clinician.Imaging staff did not send patient discharge letters.
• Clinicians were responsible for management of theirpatients’ discharges and updates and had timeallocated to write reports if necessary.
• The consultant was responsible for OPD letters. Copieswere available in the patient record.
Multidisciplinary working• There were no specific multidisciplinary meeting.
However, staff told us they were able to call on theexpertise from other departments in the hospital ifrequired. They described a good working relationshipwith other departments, such as oncology and surgery.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
45 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• We were unable to observe any minor operations duringour visit, but both the consultants and nursing staffdescribed a good working relationship.
• The diagnostic imaging manager described an excellentworking relationship with the external company thatprovided the MRI. The radiologists reported on MRIscans.
• There was a one-stop breast clinic, supported byspecialist breast care nurses and imaging.
• Physiotherapy staff supported effective recovery andrehabilitation, including an appointment atpre-assessment for patients having orthopaedic surgery,and follow up at outpatient clinics.
Access to information• Staff had access to corporate and location specific
policies and guidance.• Patient notes and relevant information was accessible.
Medical notes included all information pertaining totheir assessment and treatment plans included detailsof treatment and care. Copies of all externalcommunications, including GP letters were also storedin the patient’s notes.
• Staff also had access to contact details for consultants,the RMO and senior managers.
• The results of diagnostic tests were available on thehospitals intranet system. Staff could only accessinformation via a secure log in.
• Diagnostic imaging used a picture archiving andcommunication system (PACS) which meant imagescould be viewed on any computer connected to theintranet in all BMI hospitals and via a remote accessfacility.
• There was no evidence of records being unavailable atconsultations in the department.
• Clinic information was shared with patients’ GPs in letterformat. These were produced by the clinician followingthe appointment and copies sent to GPs and patients.
Consent, Mental Capacity Act and Deprivation ofLiberty Safeguards• Staff we spoke with knew about consent procedures
and discussed any issues with others involved in thepatient’s care and with the patient’s family. The MentalCapacity Act 2005 (MCA) contains the law that applies toanyone who lacks the mental capacity needed to maketheir own decisions about their medical treatment.
• The consent policy and Children’s and Young person’spolicy defined how a child could show they were GillickFraser competent.
• Staff told us patients were not routinely consented forinpatient procedure while in the outpatientsdepartment.
• We saw evidence that procedures undertaken in theminor operations room were consented appropriately.
• Patients told us they had been asked for their consentbefore a procedure.
• Mandatory training included the MCA. Staff knew how toobtain consent from patients with limited capacity. Onestaff member was able to tell us how they referred atpatient living with dementia needs back to theconsultant as there were concerns about their capacity.They told us they were subsequently praised by themanager.
• Nursing staff were aware of Deprivation of LibertySafeguards, but could not recall an incident in theoutpatient department when they had needed to beused.
• A patient’s cognitive and perceptual ability wasassessed by oncology staff. Consent forms forchemotherapy treatment in oncology were fullycompleted and signed.
Are outpatients and diagnostic imagingservices caring?
Good –––
We rated the services as good for caring because:
• Patients told us and we observed staff treating themwith compassion, dignity, and respect.
• All patients were very positive about their experience inthe department, and the staff ensured the patientsreceived a positive experience as far as they were able.
• Patients and their families felt involved in decisionaround their treatment, and feedback from patientresponse postcards indicated high levels of satisfactionwith outpatient services.
• Information was provided by consultants and clinicalstaff in order to ensure choices and decisions could bemade about investigations, treatment and care.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
46 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Compassionate care• We observed staff treated patients and their
accompanying relative or companion with care, dignity,and respect. Staff welcomed the patients into the OPDand explained the process for new patients. Staff offeredpatients complimentary refreshments and directedthem to the waiting area.
• We observed staff introducing themselves by name andaddressing the patients in a respectful and dignifiedmanner.
• Patients who wished to have a chaperone weresupported by staff during their visit to outpatientdepartments. Information about chaperones wasprovided in hospital literature and could be arranged inadvance or on arrival.
• All of the patients we spoke to said they had a verypositive experience, most describing it as ‘very good’.They said the staff were very polite, caring, andprofessional.
• All consultations were conducted in private clinic roomswith the doors closed, with clear signs on the doorindicating the name of the consultant and whether theroom was in use. We saw no evidence of staff havingclinical discussions either with or without patients inpublic areas.
• The diagnostic imaging manager had installed a newcurtain in the ultrasound room that shielded theexamination bed from the door to protect patient’sdignity.
• The oncology patients we spoke with were bothreceiving chemotherapy treatments. Both were verycomplimentary about the staff and the facilities.
• Patient satisfaction information was collected through adashboard. We reviewed the March 2016 dashboard,which showed results for the previous three months,and included feedback from inpatients and day cases.For outpatient services the percentage of satisfactionranged from 92% for physiotherapy, 97% for diagnosticimaging.
• Outpatient Friends and Family postcard results forFebruary 2016 indicated 95% of the 35 respondents whowere NHS patients recommended the service. Of the 274insured or self-pay patients 98% recommended theservice.
• There were numerous positive comments indicating theprovision of a compassionate service and namingindividual staff, such as: ‘All staff were very helpful and
friendly. Clear explanations from the doctors, who wasexceptionally patient and kind’, ‘Kind and caring staff,very professional’, and ‘Such a friendly, helpfuldepartment. Radiographers so helpful’.
Understanding and involvement of patients andthose close to them• Patients we spoke to said they felt they were involved in
their care. They told us the consultants had explaineddiffering treatment options clearly, and what they couldexpect from their treatment. They told us when aconsultant prescribed medication they explained anypossible side effects.
• Patients said their families or friends were welcomed atconsultations. One patient described thecompassionate way her consultant had listened to theconcerns of her husband during her appointment, andtook the time to answer all of his questions.
• We reviewed feedback made by patients in theoutpatient Friends and Family postcards for February2016. Comments included; ‘I was treated fairly. I feltlistened to and made comfortable, even though I was aNHS patient’; Staff were polite and very friendly -consultant gave very helpful advice, and ‘Everyone wasso kind and attentive and explained everything’.
• Imaging costs were discussed with patients upon arrival.Patients were given an “Outpatient ChargeArrangement" leaflet upon arrival. Staff were also able toprovide a price in advance of their appointment. Allimaging staff were able to refer to the imagingdepartment charge master.
• Where physiotherapy patients enquired through thenational enquiry booking centre, they were informed ofthe self-pay rates when making the appointment.
• Should a patient speak to an administrator in thephysiotherapy department they were informed of thetariff when they booked their appointment.
• As staff did not know what the private cover was foreach individual or the BMI agreed price with theirinsurance companies, they ensured the patients had alltheir details to hand to be able to authorise theirtreatment. If not, they were made aware they may beliable to receive an invoice for any insurance shortfall.This was confirmed on the registration form the patientsigned. If consumables were offered or sold, it wasmade clear to the patient they may not be covered forby their insurer and they may incur the cost.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
47 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Consulting room prices were available on the computersystem for reference. Information was given to allpatients explaining that tests / procedures may haveadditional cost implications. Costs were discussed atpoint of booking. Additionally, patients were given an“Outpatient Charge Arrangement" leaflet upon arrival,before their consultation.
• Consultation fees were separate to treatment costs andwere invoiced separately by the consultant. We notedthere was detailed information on the fees and costsattached to services, including fixed price packages,spreading the cost with a hospital card, as well asdifferent methods for paying.
• The hospital website also provided a range of patientinformation for national and overseas patients, andthose using the services via the NHS.
Emotional support• Cancer patients and their families have urgent needs for
information and support especially in the early stages ofthe cancer journey. To meet those needs the oncologyteam aimed to provide continuity and co-ordinatedcare. This included emotional and psychologicalsupport. Staff liaised with other healthcare professionalsincluding GPs and palliative care teams.
• Staff told us that upsetting or unexpected news wouldbe delivered sensitively and in appropriate privatesurroundings. They said they would try to arrange afriend or family member to accompany the patient.
• A comment made on patient feedback in respect totheir consultation was: ‘Very open and forthrightconsultation’.
• The outpatient department did not have a dedicatedservice to refer patients, if they required additionalemotional support. There were clinical nurse specialistswho would see patients as required to offer support.Staff told us they would try to give patients informationon groups and charities that may be able to offersupport or refer them back to their GP.
• Patients told us consultants spoke to them sensitivelybut they ensured the patient understood theinformation.
• Patients were able to telephone the ward or the out ofhour’s oncology staff after discharge for further help andadvice about any concerns or questions on their returnhome.
Are outpatients and diagnostic imagingservices responsive?
Good –––
We rated responsive as good because:
• Patients did not experience long wait times to see theirchosen consultant, and clinics ran mostly as planned.The OPD met the 18-week Referral to Treatment targetfor NHS patients of 92% for the year April 2015-March2016.
• The departments were fully accessible and wereorganised to facilitate a responsive service. There wasflexibility in appointments, and in general patient’schoices were taken into account when makingappointments.
• The outpatient departments had a range of services,which were fully established to meet the specific needsof patients, including children, young people andadults.
• Patients were happy with their experience in outpatientsand diagnostic imaging.
• There was a process for receiving, responding to andinvestigating complaints, and staff learnt frominformation arising from these.
However;
• Information informing patient about raising a concernor complaint was not readily available, and patientswere not made aware is they could obtain literature inother languages.
Service planning and delivery to meet the needs oflocal people• Staff told us that clinics were run on fixed days and
patients were usually seen within one week of referral.• Monthly clinical waiting times were audited, which
indicated 10 clinics were reviewed each month. Where aclinics showed delays it was re-audited the followingmonth. We reviewed the audit results for May and June2016. The results for June 2016 showed expected andactual start and finish times, the number of patientsseen and number of minutes late by. Across the 10clinics six clinics were late, one by five minutes, two by10 and fifteen minutes respectively, and one by twentyminutes.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
48 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• The manager told us that if a clinic had to be cancelledat short notice, patients would be contacted at theearliest opportunity. They would be offered of analternative consultant to see, or the next availableappointment with their chosen doctor.
• During our inspection, we observed a relaxedatmosphere in the outpatient area. The waiting areaswere not overcrowded and clinics were running on time.
• Most consultants scheduled their patients for thefollowing week’s clinic for minor procedures. However,in some circumstances treatment was required soonerand therefore, if requested by the consultant, thepatient had the procedure is completed at that visit.
• There was a range of opening times for outpatientservices, which allowed greater accessibility. Theoutpatients department was open from 8am to 9pmMonday to Friday and from 8am to 4pm on Saturday.
• The diagnostic imaging department was open from 8amto 8pm Monday to Friday and from 8am to 1pm onSaturday.
• The MRI unit was available four days per week from 8amto 5pm.
• The oncology services were open from 8.30am to 5pmMonday to Friday but if “longer treatments were bookedin, the department flexed to accommodate these. Thedepartment was covered by on call outside of thestandard opening hours.
• Outpatient physiotherapy was available Monday,Tuesday and Wednesday 8am to 8.30pm, and Thursdays8am to 8pm. On Fridays the service was available 8amto 5pm, and Saturday between 8am and 11am.
• Physiotherapy services were provided to patients fromage four years and above. This included pre-operativeassessments, a ‘Joint School’ for orthopaedic patients,and group work. An external hydrotherapy pool was inuse via physiotherapy, and this was open on Mondaysand Thursdays between 5pm and 8pm.
Access and flow• Access to appointments for clinics was satisfactory. All
the patients we spoke to told us they were happy withthe length of time they had waited to be seen followingreferral and had been offered times convenient to them.
• NHS ‘choose and book’ patients were seen within the18-week referral to treatment time target for NHSpatients. We saw evidence the hospital was consistentlyabove the 92% target for the year April 2015 – March2016.
• The physiotherapy department provided access tochildren aged four and over, and they were seen formusculoskeletal problems only. The department did notsee neurological problems or complex presentations,which was made clear when they received any referrals.
• Children could be seen in the majority of clinics byconsultants who regularly treated children in their NHSpractice. These clinics were supported by paediatricnurses. Paediatricians were also supported bypaediatric nurses.
• We examined records from NHS patients, and theseshowed that waiting times for an outpatientappointment was between two and four weeks. Privatepatients waited between one and two weeks, but thiswas not audited by the hospital.
• Orthopaedic outpatient activity was the most usedservice, accounting for 16% of throughput, followed bygynaecology, at 11.8%, and surgery 13.5%. Paediatrics,including surgery accounted for 2.5% of OPD activity.
• Paediatric patients were initially booked intooutpatients via the GP for an initial consultation. Atconsultation they were seen by a consultant andpaediatric nurse. If the child required surgery, they wereinvited to come back to be pre assessed by the preassessment paediatric nurse, who covered the pathwayof the patient journey.
• Children’s clinics were grouped together and thespecialist paediatric nurse would be on duty to overseethese clinics.
• All staff reported clinics generally started on time andran on schedule. The manager monitors late startingclinics and completes an incident form for any startingmore than 30 minutes late. Any consultants who wereconsistently late would be reported to seniormanagement.
• The patients we spoke to said they were seen either at,or very close to their appointment time.
• Did not attend (DNA) patients under the Choose & Bookscheme were logged and reviewed by an externalcompany. For Private patients, although they wererecorded on an electronic system if they DNA, this wasnot audited.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
49 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• In physiotherapy, DNAs were recorded on the patientpaper records and also on the electronic bookingsystems. If the patient DNA and no response or contactwas made, this would track a DNA on the referral trackerused for all patients when the patient was discharged.
• There were very few private patient DNA’s, and thesewere followed up with a telephone call.
Meeting people’s individual needs• There were parking spaces for those with mobility issues
and for patients in a wheelchair. Staff told us they oftenhelped patients out of vehicles and into the departmentand would provide a wheelchair if required.
• Outpatient services were planned, delivered, andco-ordinated to accommodate patients with complexneeds. This included patients living with dementia,learning difficulties or physical disabilities.
• Outpatient areas were on one level on the ground floor.The outpatient area was accessible to all patients.Patients had access to wheelchairs, which wereavailable in the main reception.
• Chairs at different heights were available in the waitingrooms. There were sufficient numbers of chairs in thewaiting area to suit individual needs.
• The oncology rooms were located at the end of thecorridor, which contributed to privacy and consisted ofthe main treatment room with two chemotherapychairs, secure drug storage and staff office space. Therewas also a private room opposite the treatment roomavailable for patients having longer treatments or thosewishing greater privacy.
• A member of the oncology staff was in attendanceduring the patient’s initial consultation, allowing forintroduction to be made early. After consented tochemotherapy a pre-treatment appointment was made,which included pre-chemotherapy bloods, ECG andMRSA screening as well as discussions about thetherapy, side effects and any concerns they may have.Vein assessment and arrangements for Picc lines orPortacaths was also be initiated. Literature wasprovided, along with a tour of the unit, and 24 hourcontact numbers were shared.
• Oncology treatments were usually administered onweekdays, with most being on Tuesdays, Wednesdaysand Thursdays. Flexibility allowed the patient to lead asnormal a life as possible around their treatment.Reflexology is available from the physiotherapy team.
• Staff told us that patient referral identified thosepatients who needed extra support at theirappointment, and this was flagged with clinic staff sothey could organise this.
• We found changing facilities in the diagnostic imagingdepartment had curtains providing privacy. Patientswho wished to change behind a locked door had to useone of the imaging rooms. There was appropriateclothing to change into, including dressing gowns. Therewere no lockers provided, patients had to carry theirclothes in supplied plastic bags, with them into theimaging rooms, which guaranteed the safety of theirpersonal items
• We saw there was a range of information leafletsavailable to patients in the waiting area on wide varietyof topics. The BMI group had produced most of theseand others had been produced by professionalorganisations. We did not see any of these available inalternative languages.
• The hospital did not provide in house interpretingservices, but staff knew where to find information inorder to obtain an interpreter. Staff told us they werenormally made aware of whether English was not apatient’s first language in the patient’s referral letter, andwould plan accordingly. Language line was used toarrange either face to face or telephone interpretation.
• Staff told us if they identified a patient as having needsassociated with dementia or learning difficulties, thenthey would ensure the patients’ needs were met. Forexample, organising a suitable waiting area. They told usthat in the past they had arranged for patients to wait inunused clinic rooms if appropriate. Staff attendedpatients with complex needs at all times whennecessary.
• Staff were trained in chaperoning and had access to apolicy to support this. All chaperones were recordedusing the BMI recommended chaperone form, whichwas also evidenced by recording on the Imaging referralform. This was then scanned onto the patient numberon the CRIS system. A chaperone audit was in progressin diagnostics.
• In the physiotherapy department there were wallposters to encourage patients to request a chaperone ifdesired. Patient information posters were visible both inthe outpatient reception area and in all consultingrooms. Chaperones documentation was undertaken asper the chaperone policy in the chaperone register,although the register was not currently audited.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
50 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• A dedicated children’s nurse ran the children’s clinics.While there was no specific children’s waiting area, theydid have some appropriate toys and books for thechildren to play with while waiting. There was a range ofstickers and certificates they could give to children forbeing well behaved and brave.
• Diagnostic imaging rooms used wide tables toaccommodate bariatric patients. Bariatrics is the branchof medicine that deals with the causes, prevention, andtreatment of obesity. They employed techniquesenabling bariatric patients to have an X-Ray withoutlying down if required. The MRI scanner used by thehospital could accommodate bariatric patients.
• Oncology patients were given 24 hour contact numbersof a member of the oncology team for any questions orconcerns they may have had.
• The patient-led assessment of the care environment,(PLACE) was above the England average for privacy anddignity, scoring 92%, against a score of 87%.
Learning from complaints and concerns• We observed there was no information on how to
complain available in the public areas. The hospital hadpublished a leaflet entitled; 'We’d Like To Hear FromYou', which did contain correct information on thecomplaints procedure. This leaflet was available in arack with other leaflets in the waiting area, but itscontent was not obvious.
• The hospital had a complaints policy, which provided aframework within which complaints were to beresponded to.
• The Quality and Risk Lead with the Hospital Managerwere responsible for co-ordinating and managing thecomplaints procedure. The Quality & Risk Lead acted asthe lead investigator.
• The complaint investigation file was reviewed, alongwith the response to the patient by the HospitalManager, who then approved the complaint responseletters.
• Complaint could be raised by telephone, in person, inwriting or made verbally. We found from our review ofthe complaints process, a letter of acknowledgementwas sent out within two working days of receipt of acomplaint letter. Full response was sent within 20working days or if the investigation required furthertime, an update letter went out to the patient.
• For serious complaints, a holding letter was sent at leastevery 20 working days until final response.
• The director of clinical services was responsible forensuring a comprehensive investigation wasundertaken on clinical aspects of complaints and forensuring the recommendations made from complaintswere shared and acted upon.
• We saw from information reviewed complaints werediscussed at head of department meetings, the MedicalAdvisory Committee, at clinical governance meetings,and departmental meetings. We saw for example in theMinutes of the January 2016 MAC meeting 24complaints had been received, the majority(14) werenon-clinical in origin, six of each related to financial orconsultant issues. The department manager told usmost complaints were about fees, such as notappreciating the cost of tests.
• Staff who spoke with us in OPD knew the process shoulda patient want to complain, and told us they would tryto resolve any informal complaints immediately. Theytold us they could refer the patient to the departmentmanager if required.
• The department manager told us if the complaint couldnot be resolved, they would launch a formalinvestigation. The department manager would beresponsible for any subsequent investigation, under thedirection of the hospital manager.
• Staff confirmed they received feedback from complaintsat the monthly team meeting. The manager requiredstaff to sign that they had read and understood theinformation and feedback given to them in theirmonthly team meetings. This included staff who couldnot attend the meeting.
Are outpatients and diagnostic imagingservices well-led?
Good –––
We rated well led as good because:
• A formalised daily meeting provided opportunities forstaff to update colleagues with respect to theirdepartment, and to be informed of other service relateddevelopments.
• Staff felt well supported by their line manager andsenior managers. Staff told us, senior managers werevisible, engaging, and approachable, and there was anopen culture for raising matters and shared learning.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
51 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• The outpatient services engaged with staff and patients.They gave them the opportunity to provide feedbackabout their experiences of the services.
• Staff told us they felt care and treatment was patientfocused, and they enjoyed working in the outpatientand diagnostic imaging departments. All felt part of awider team.
• There was a well-defined governance structure aimed atimproving patient services.
• The managers of the OPD and diagnostic imaging wereenthusiastic and proud of their departments.
• E-prescribing was being introduced for chemotherapydrugs which would enhance patient safety.
However;
• Some staff did not have a full awareness of the hospitalsstrategic priorities.
• Information about patient feedback on the servicesprovided was not visibly displayed.
Vision and strategy for this this core service• The local hospital strategy underpinned the broader
organisational vision, which was to provide the bestpatient experience, best outcomes and the most costeffective.
• The local vision had been shared with staff, althoughsome staff were not fully aware of the specific aspectsrelated to the outpatients.
• Operational priorities had been identified for thefinancial year, and included closing the loop onincidents, focus on patient satisfaction related todischarge procedures and food services. Peoplepriorities centred on recruitment, appraisals,revalidation of nurses, internal staff development, andincluded management development. In terms ofbusiness growth and maximising efficiencies, thelocations executive team had identified priorities, whichincluded; stock management and capacity, NHS and GPworking and engagement, and the development ofoutpatients.
• All staff we spoke to told us they thought that theirrespective department was patient rather than profitfocused.
• The manager told staff of plans for the hospital in theirmonthly meetings, for example the recent upgrade ofthe outpatients, and plans for e-prescribingchemotherapy.
Governance, risk management and qualitymeasurement for this core service• The hospital had its own governance structure, which
reported into the regional committee. We found therewere ‘Terms of Reference’, which underpinned thepurpose and functions of respective committees.Departments reported through their respectivemeetings into the Head of Departments (HODs), andthey in turn, along with the Hospital Clinical GovernanceCommittee, and Hospital Health and Safety Committeereported to the Executive Team. The latter reported intothe Medical Advisory Committee, (MAC)
• Business Development, Operational Performance, andPeople and Performance reported directly to theExecutive Team.
• The frequency of meetings varied, with weekly ExecutiveTeam meetings, monthly HODs and RegionalCommittee meetings. All others were indicated as takingplace bi-monthly on documented information providedto us. The hospital manager indicated the MAC currentlytook place quarterly, and minutes reviewed confirmedthis. We noted in the minutes dated 26 April 2016 theMAC agreed to move to bi-monthly meetings.
• The MAC membership was made up of the executivedirector, director of clinical services, surgeon, physician,and anaesthetist representatives. This was confirmed bythe MAC chair.
• With the exception of MAC meetings, minutes ofmeetings reviewed by us contained standard agendaitems, such as, hospital activity, finance, legislation andcorporate policies, significant events and complaints,and updates to the risk register. Actions had beenidentified with ownership, date for delivery, and thestatus.
• There were procedures for ensuring only consultantswith approved practicing privileges worked at thehospital. We reviewed five randomly selected consultantfiles and saw evidence of checks on fitness to practice,professional indemnity and registration. Appraisals andre-validation was monitored and requested whererenewal was required.
• The MAC chair met with the hospital manager prior tothe formal meeting, where they reviewed the agendaand items for discussion. Meeting minutes indicatedpracticing privileges were reviewed, as well as removalsand suspensions. The management report was sharedwith attendees, followed by any other business.Resulting actions were summarised.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
52 BMI Chelsfield Park Hospital Quality Report 06/12/2016
• Data from quality reports and dashboards providedoversight in relation to safety, effectiveness, andperformance in general.
• Monthly Clinical Governance meetings were attended bymanagers from each area, as well as consultantrepresentative. We reviewed several sets of minutesfrom such meetings and noted there was a detailedagenda, which addressed a wide range of subjects,relevant to governance, safety and quality.
• The hospital had a risk register and managers updatedthis accordingly. Managers in both the outpatient anddiagnostic imaging department were aware of theirdepartment’s risks, and these were correctly recordedon the hospitals risk register.
• Information provided to us indicated the lead paediatricnurse sat on the Clinical Governance Committee andrepresented children and young people services. Thelead nurse also represented the paediatric committees,which incorporated resuscitation meetings and theyattended the corporate safeguarding and best practicegroup for paediatrics.
• Children’s services were audited through Quality Healthand patient feedback.
• A Radiation Protection Advisor from a local HospitalNHS Foundation Trust oversaw the management ofpotential risks in diagnostics. A laser protection audithad been undertaken and an action plan was generatedto meet this.
• The managers knew they were responsible forperformance of their departments and receivedfeedback from Clinical Governance and Heads ofDepartment meetings and at individual performancereviews.
• The department managers attended a daily ‘10@10’meeting where a staff representative from each area hadthe opportunity to update the hospital manager andcolleagues with respect to their department. Weattended one of these, and witnessed thecommunication of information, such as activity,equipment matters, staffing and cover for holidays.
Leadership / culture of service• There was effective and responsive leadership at the
location executive level, and staff commentedfavourably on the hospital manager and other seniorleaders. The executive team were very visible and staff
said they were approachable. The size of the hospitalhelped staff to know one another and contributed to afeeling of ‘family’. Staff told us there was a high level ofcomradery.
• There were heads of department (HOD), who werereported to work well together. They providedleadership and support to staff, as well as to theexecutive team. HOD met monthly and reviewed a rangeof subject areas, ensuring they were able to cascadeinformation to their teams.
• We observed a good level of visibility and engagementof the departments senior teams, Staff we spoke withunderstood the departmental structure and knew whotheir line manager was. They reported feeling able todiscuss issues with their line manager, and told us howthey felt they could contribute to the running of thedepartment.
• Staff told us the senior management were extremelyvisible and approachable. Staff were confident in theability of senior management. All reported that eitherthe hospital manager or the director of clinical serviceswould visit the department daily and engage with staff,and managers of both departments were described asenthusiastic.
• We observed and it was confirmed by staff that thehospital was patient focused and staff arrangementsand resources enabled them to provide a high level ofcare for patients. All staff who spoke with us felt therewas an open culture in the department, and feltengaged as a part of a close team.
• We found the morning operations meeting, attended bythe hospital’s senior management team and heads ofdepartment, provided opportunities to discussoperational issues, incidents and other issues ofrelevance to the hospital each day leading to a healthyreporting culture.
• Our observations and discussions with staff confirmedwith us an open culture where they felt confident toshare ideas and to highlight any concerns, incidents, orerrors and learn from the subsequent investigations.
• The requirements related to duty of candour were metthrough the processes for investigating incidents, andreviewing and responding to complaints. Staff were ableto tell us how important it was to be open and honestwith people when things went wrong. One staff member
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
53 BMI Chelsfield Park Hospital Quality Report 06/12/2016
told us that she had telephoned a patient to inform andapologise after she realised that she had performed thewrong blood test. She was able to arrange for her to beseen again at the patient’s convenience.
• An equal opportunities approach was applied torecruitment and selection. Information provided to usshowed the workforce, was in the main (76%) whiteBritish, 16% were of Asian ethnicity, 3.5% Black African,0.80%, Black Caribbean, and 0.80%, Chinese. Otherethnic groups accounted for 2%, and 0.40% were mixedWhite. The remaining were not stated.
• We found there was positive and active management ofstaffing. For example, sickness rates for nurses workingin outpatient departments in the reporting period (Apr15 to Mar 16) were not high when compared to theyearly average of other independent acute hospitals,except for January 2016, when the rate of sickness wasabove the average. Sickness rates for outpatient healthcare assistants in the reporting period (Apr 15 to Mar 16)were not high when compared to the yearly average ofother independent acute hospitals, except in April 2015,January, and March 2016, when sickness rates wereabove the average.
• There were no vacancies for nurses or health careassistants. Many staff had been working in thedepartment for a long time. There had been a 1.3% staffturnover for outpatient nurses in the reporting period(April 2015 to March 2016). This rate was low whencompared to other independent acute hospitals. Therehad not been any staff turnover for outpatient healthcare assistants. These figures suggested staff werehappy working at the hospital, as was reported by staff.
• Most staff were aware the hospital had a whistleblowingpolicy. The manager was aware that she could whistleblow directly to the Care Quality Commission.
Public and staff engagement• Patients attending the outpatient department had the
opportunity to provide feedback through cardsavailable in reception. In order to increase the numberof responses, the staff had started giving these cards toall new patients during their appointment. We saw 64completed cards and the overwhelming majority werepositive.
• To the question ‘How likely are you to recommend ourservice to friends and family if they needed similar careand treatment’ for NHS patients, 100% of patientsresponded that they would recommend the service.
• Feedback cards were analysed and a report publishedby an independent company. The report was discussedwith staff every month at their team meetings, which didincluded individualised feedback for positivecomments. Negative feedback was given anonymously.
• We could find no evidence of the results of the patientsurvey on display in public areas in the department.Patients visiting the department were unaware of howwell the department performed.
• The hospital provided placements for nursing studentsfrom a local university, as well as work experience forschool children.
• We were told about a number of staff engagementactivities, which included for example; monthly charity“Give it Up”, ‘fairy cakes’ on Friday, Easter and Christmascompetitions, Inspirational ‘Quote of the week’, a freebirthday lunch. Staff were also named and receivedreward recognition letters.
• The hospital manager told us they ensured they walkedthe floor and spoke with staff, asking about thechallenge they had. They also met with the HOD teamand received corporate feedback with regard toperformance.
Innovation, improvement and sustainability• The recent upgrade of the OPD had meant there was
now provision of a minor procedures room, fordermatology procedures. This had a positive impact onthe patient journey, for example dermatology patientscould have minor procedures carried out without theneed for a new appointment or admission to a bed.
• The service was continuing to work with external ClinicalCommissioning Groups, GP and Clinical Service Users toensure best experience for the patients. Discussion withrepresentatives of CCG indicated they received a serviceto the expected level and there were no concernsidentified.
• Staff were proud of the impact of the recentrefurbishment programme, aimed at improving theoutpatient environment.
• The department had introduced a new moreuser-friendly diagnostic heart monitor. Plans for e -prescribing for Oncology patients were in progress.
• BMI Healthcare was shortlisted as a finalist in the ITinnovator of the year category of the 2016 HealthInvestor awards for this system, which was beingintroduced throughout the group.
Outpatientsanddiagnosticimaging
Outpatients and diagnosticimaging
Good –––
54 BMI Chelsfield Park Hospital Quality Report 06/12/2016
Outstanding practice
The arrangements to engage with staff wereacknowledged as a very positive and proactive approachto effective team work, and for respecting and valuingstaff.
Areas for improvement
Action the provider SHOULD take to improve
• Improve compliance with the World HealthOrganisation (WHO) ‘five steps to safer surgery’procedures.
• Improve consultant compliance with the use ofpersonal protective equipment during invasiveprocedures, in line with NICE guidelines and BMIpolicy.
• Improve the completion of patient records to enablethe availability of a fully detailed record.
• Consider how professional guidelines can be appliedto support the safeguarding training further.
• Improve the use of the risk register with theincorporation of review dates for all identified risks.
• Consider having leaflets available in other languagesas well as in English.
• Staff involved in the treatment and care of childrenand young people should have the required level ofsafeguarding training.
• Where oncology patients call the advice line, nursingstaff should include an assessment and recording ofpatient temperature in the record.
• Provide a means of ensuring the summary of oncologypatient MDT meeting are available in patient records.
• Review the accessibility of the resuscitation trolley fordiagnostic staff.
• Undertake regular auditing with regard to thecompletion of pregnancy status declarations
• Review its position with regard to participate inimaging accreditation schemes or improving quality inphysiological services scheme.
• Make it possible to obtain patient information leafletsin alternative languages.
• Make sure information to advise patients how to raisea concern or complaint more obvious in public areas.
• Review how information is communicated with regardto fees, so that patients do not find themselvescomplaining when they received their bill.
• Review the administrative facilities in the ODP anddiagnostics.
• Consider how staff may be better informed of thehospitals strategic priorities.
Outstandingpracticeandareasforimprovement
Outstanding practice and areasfor improvement
55 BMI Chelsfield Park Hospital Quality Report 06/12/2016