Biliary Imaging. Radiographic examination of the biliary system involves studying the manufacture,...
-
Upload
clinton-banks -
Category
Documents
-
view
223 -
download
4
Transcript of Biliary Imaging. Radiographic examination of the biliary system involves studying the manufacture,...
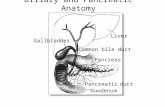
Radiographic examination of the biliary system involves studying the manufacture, transport, and storage of bile. Bile is manufactured by the liver, transported by various ducts, and stored in the gallbladder.
The liver is the largest solid organ in the human body and weighs 3 or 4 pounds (1.5 kg), or 1/36 of the total body weight in an average adult. It occupies most of the right upper quadrant
The distal end of the gallbladder extends slightly below the anterior, inferior margin of the liver. The rest of the gallbladder lies along the inferior and posterior surface of the liver
The liver is partially divided into two major lobes and two minor lobes. As viewed from the front in only the two major lobes can be seen. A much larger right lobe is separated from the smaller left lobe by the falciform ligament
The liver is a complex organ that is absolutely essential to life. The liver performs more than 100 different functions, but the one function most applicable to radiographic study is the production of large amounts of bile. It secretes from 800 to 1000 ml, or about 1 quart, of bile per day.
The major function of bile is to aid in the digestion of fats by emulsifying or breaking down fat globules and the absorption of fat following its digestion. Bile also contains cholesterol, which is made soluble in the bile by the bile salts
Bile is formed in small lobules of the liver and travels by small ducts to the right or left hepatic duct. The right and left hepatic ducts join to continue as the common hepatic duct. Bile is carried to the gallbladder via the cystic duct for temporary storage, or it may be secreted directly into the duodenum by way of the common bile duct, which is joined by the pancreatic duct.
Bile is concentrated within the gallbladder as a result of hydrolysis (removal of water). In the abnormal situation, if too much water is absorbed or if the cholesterol becomes too concentrated, gallstones (choleliths) may form in the gallbladder.
The gallbladder normally contracts when foods such as fats or fatty acids are in the duodenum. These foods stimulate the duodenal mucosa to secrete the hormone cholecystokinin (CCK). Increased levels of CCK in the blood cause the gallbladder to contract and the terminal opening of the common bile duct to relax.
The common bile duct descends behind the superior portion of the duodenum and the head of the pancreas to enter the second or descending portion of the duodenum.
In the past, contrast medium was ingested orally for a cholecystogram; thus this procedure was termed an oral cholecystogram, abbreviated OCG. Sonography has replaced these OCG exams once performed in imaging departments. In addition, production of oral contrast media for the OCG has been discontinued
Sonography of the gallbladder provides a noninvasive means of studying the gallbladder and the biliary ducts
Sonography offers four advantages over conventional OCG imaging
• No ionizing radiation
• Detection of small calculi
• No contrast medium
• Less patient preparation
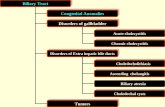
CholePrefix denoting relationship to bileCystoPrefix denoting sac or bladderCholangiogram Radiographic examination of the biliary ductsCholecystocholangiogram Study of both the gallbladder and the biliary ductsCholeliths Gallstones Cholelithiasis Condition of having gallstonesCholecystitis Inflammation of the gallbladderCholecystectomy Surgical removal of the gallbladder
Choledocholithiasis is the presence of stones in the biliary ducts. Biliary stones may form in the biliary ducts or migrate from the gallbladder. Often, these stones produce a blockage in the ducts. Symptoms include pain, tenderness in the right upper quadrant, jaundice, and sometimes pancreatitis.Cholelithiasis is the condition of having abnormal calcifications or stones in the gallbladder. Increased levels of bilirubin, calcium, or cholesterol may lead to the formation of gallstones. Female and obese patients are at a higher risk for developing gallstones. Ninety percent of all gallbladder and duct disorders are due to cholelithiasis. Symptoms of cholelithiasis include right upper quadrant pain usually after a meal, nausea, and possibly vomiting. Patients with complete blockage of the biliary ducts may develop jaundice.
Choledocholithiasis (stones in biliary ducts)
SonographyEndoscopic retrograde cholangiopancreatogram (ERCP)Operative cholangiography
Enlargement or narrowing of the biliary ducts due to presence of stones
Cholelithiasis (stones in gallbladder)
SonographyCholescintigraphy (radionuclide studies)†
Both radiolucent and radiopaque densities seen in the region of the gallbladder; “shadowing” effect with sonography; failure to accumulate radionuclide within gallbladder†
Acute cholecystitis
SonographyCholescintigraphy (radionuclide studies)†
Thickened wall of gallbladder with sonography; failure to accumulate radionuclide within gallbladder†
Chronic cholecystitis
Sonography
Calcified plaques or calcification of the wall of the gallbladder
Neoplasms SonographyComputed tomography
Mass seen within gallbladder, liver, and/or biliary ducts; extensive calcification of gallbladder wall
Biliary stenosis
Operative cholangiogramEndoscopic retrograde cholangiopancreatogram (ERCP)
Elongation, tapered, and narrowing of common bile duct
Postoperative (T-Tube or Delayed) Cholangiography
PURPOSEPostoperative, also termed T-tube, or delayed cholangiography usually is performed in the radiology department following a cholecystectomy. The surgeon may be concerned about residual stones in the biliary ducts that went undetected during surgery. If these concerns exist, the surgeon will place a special T-tube catheter into the common bile duct during the cholecystectomy. The catheter extends to the outside of the body and is clamped off
PATHOLOGIC INDICATIONS
• Residual calculi
• Strictures:
CONTRAINDICATIONSPrimary contraindications for T-tube cholangiography include hypersensitivity to iodinated contrast medium, acute infection of the biliary system, and elevated creatinine and/or BUN levels
PATIENT PREPARATIONPatient preparation for the T-tube cholangiography will vary based on department protocol. The procedure should be clearly explained to the patient and a careful clinical history taken. The patient should be placed in a hospital gown and should be NPO at least 8 hours prior to the procedure.MAJOR EQUIPMENTFluoroscopy is required during injection of contrast medium. Postradiographic images may be taken following the fluoro procedure.ACCESSORY EQUIPMENTSyringes of various sizes, syringe adapters, iodinated, water-soluble contrast medium (possibly a diluted concentration to prevent obscuring of small calculi), emesis basis, gloves, and sterile drapes are needed.
SUMMARY OF POSTOPERATIVE (T-TUBE) CHOLANGIOGRAPHY PROCEDUREThe following steps are taken in the performance of a postoperative cholangiogram: 1.Prepare the fluoroscopic suite.2.Set up the examination tray.3.Select and prepare the contrast medium. Determine whether the patient is hypersensitive to iodinated contrast media.4.Take the appropriate scout images to verify position and technique.5.Provide lead aprons for those persons who remain in the room during the procedure.6.Monitor the patient during the procedure.7.Change fluoro spot film-screen cassettes as needed.8.Produce conventional radiographs as requested. The RPO position is often performed to project biliary ducts away from the spine.
After duct drainage and under fluoroscopic control, the iodinated contrast medium is injected fractionally, and fluoro spot images are taken. It is important not to introduce any air bubbles while injecting contrast media because these bubbles may be confused for radiolucent stones.If residual stones are detected, the radiologist may elect to remove them
Endoscopic Retrograde Cholangiopancreatography (ERCP)
PURPOSEAnother procedure that is performed more frequently for examination of the biliary and main pancreatic ducts is endoscopic retrograde cholangiopancreatography, or simply ERCP
PATHOLOGIC INDICATIONS
• Residual calculi
• Strictures:
CONTRAINDICATIONSPrimary contraindications for ERCP include hypersensitivity to iodinated contrast medium, acute infection of the biliary system, possible pseudocyst of the pancreas, and/or elevated creatinine and/or BUN levels.
The ERCP can be a diagnostic or a therapeutic procedure. Therapeutically, ERCP can be performed to relieve certain pathologic conditions through the removal of choleliths or small lesions, or for other purposes, such as to repair a stenosis (narrowing or blockage of a duct or canal) of the hepatopancreatic sphincter or associated ducts.For diagnostic purposes, in general, the ERCP procedure includes the endoscopic insertion of the catheter or injection cannula into the common bile duct or main pancreatic duct under fluoroscopic control, followed by retrograde injection (backward or reverse direction) of contrast medium into the biliary ducts. The procedure usually is performed by a gastroenterologist who is assisted by a team that comprises the technologist, one or more nurses, and perhaps a radiologist
CONTRAINDICATIONSPrimary contraindications for ERCP include hypersensitivity to iodinated contrast medium, acute infection of the biliary system, possible pseudocyst of the pancreas, and/or elevated creatinine and/or BUN levels.
PATIENT PREPARATIONPatient preparation for ERCP will vary based on departmental protocol. The procedure should be clearly explained to the patient, and a careful clinical history taken. The patient should be placed in a hospital gown and should be NPO at least 8 hours prior to the procedure
SUMMARY OF ERCP PROCEDUREERCP typically involves the following steps: 1.Prepare the fluoroscopic suite.2.Set up the examination tray.3.Select and prepare the contrast medium. Determine whether the patient is hypersensitive to iodinated contrast media.4.Take the appropriate scout images to verify position and technique.5.Assist the gastroenterologist with fluoroscopy for placement of the catheter or injection cannula.6.Monitor the patient during the procedure.7.Change fluoroscopy spot films as needed, if a film-screen system is being used.8.Produce conventional radiographic images as requested. Oblique projections may be requested to project the biliary ducts away from the spine.
PRECAUTIONS1. Because the patient's throat is anesthetized during the procedure, the patient should remain NPO for at least 1 hour (or more) after the procedure. This will prevent aspiration of food or liquid into the lungs. 2. Review the clinical history of the patient to determine whether the patient has pancreatitis or, specifically, a pseudocyst of the pancreas. Injecting contrast media into a pseudocyst may lead to rupture. 3. Ensure that all persons in the fluoroscopy room wear protective aprons.
Percutaneous Biliary DrainagePercutaneous biliary drainage (PBD) can be used for many reasons, such as internal or external drainage, stone removal, dilation of obstructed bile duct, and biopsy. The most common use of PBD is as a palliative procedure for unresectable malignant disease. Less popular uses include the treatment of biliary obstruction, suppurative cholangitis, postoperative or posttraumatic biliary leakage, and stone removal.Patients who undergo PBD may have infected bile. To avoid the spread of infection, antibiotics should be administered at least 1 hour before the procedure.
Catheter drainageCatheter drainage through the Seldinger over-the-wire technique may be used for inserting the catheter. An example of this is the Van Sonnenberg sump drain–type catheter illustrated in If a sump pump type of arrangement is used, a double-lumen type of catheter is required, by which room air can flow into the abscess region while the suction is being applied. This simultaneous drainage and venting prevents suction, which causes the abscess material to cling to the walls of the catheter, thereby blocking the drainage holes. The “pigtail” type of design at the end of the catheter shown in aids in retention or accidental withdrawal