3.7 Orbital Cavity and Contents (Dimagiba) - Panda
description
Transcript of 3.7 Orbital Cavity and Contents (Dimagiba) - Panda
-
ORBITAL CAVITY
Dra. Dimagiba
ORBIT
paired of bony cavities that contains the eyes,
associated muscles, blood vessels, nerves, fat and most
of the lacrimal apparatus
protected anteriorly by two thin, movable folds called
EYELIDS
pyramidal cavity with its base in front and its apex
behind
thin tissue of skin, muscles, fibrous tissue and
mucous membrane
UPPER EYELID covers 1-2 mm of the limbus of the
cornea; larger and more mobile than lower
LOWER EYELID covers below limbus of the cornea
* they meet at the lateral and medial canthal angle
At the medial side of the eyelids, there are important
tissues:
o Caruncle (fleshy material)
o Plica semilunaris (reddish fold of material;
lateral to the caruncle)
LAYERS OF THE EYELID
1. Skin
2. Muscles
Orbicularis oculi (CN VII)
o concentric
o 2 parts: orbital portion & palpebral portion
(preseptal/pretarsal)
Eyelid retractors
o Levator palpebrae superioris (CN III)
o Superior tarsal muscle (sympathetic)
o Inferior rectus muscle (CN III)
o Inferior tarsal muscle (sympathetic)
Muscle O I N A
Orbicularis oculi
Orbital medial margin of
orbit
anterior surface of
medial canthal ligament
periorbit of superior
and inferior orbital
margin into the lateral palpebral ligament
CN VII
Forceful blinking of
the eye
Palpebral
Involuntary blinking of the eyes
Preseptal post lacrimal crest
medial
palpebral ligament
Fascia investing the orbital margin of zygomatic
bone
CN VII
Pretarsal aponeurosis of levator palpebrae superioris
muscle
Post lacrimal crest, medial cardinal ligament
that inserts into
lacrimal crest
CN VII
Levator palpebrae superioris
Lesser wing of sphenoid
Anterior tendon:
Skin of the upper eyelid
Posterior tendon: Anterior
surface and upper
border of superior
tarsal plate
CN III Responsible for the
opening of the eyes
3. Fibrous tissue
Orbital septum
Tarsal plate fibrous membrane of the eyelid which
gives tone to the eyelid
EYELIDS
For the Asians, the lateral angle is 2mm higher than the
medial angle. For the Chinese (Ching, Chua, Chun ),
their lateral angle is >2mm higher.
*Orbicularis oculi originates from the medial canthal ligament
and inserts around the orbit.
*Levator palpebrae superioris originates from the apex and
has 2 tendons:
Anterior tendon inserts to the skin of the eyelid
Posterior tendon inserts to the tarsal plate
EYELASHES stop abruptly at the medial angle because of
the presence of lacrimal papilla (where the tears pass).
Inside the lacrimal papilla is the structure called lacrimal
punctum.
1 PANDA (Section 1A)
-
4. Mucous Membrane
Palpebral conjunctiva
GLANDS
1. Gland of Zeis (sebaceous
gland)
found at the end of
each hair follicle
2. Gland of Moll (ciliary gland)
modified sweat
gland
3. Tarsal gland (Meibomian
gland)
its opening is found
in the tarsal plate
long modified
sebaceous gland
oily secretion to lid
margin
FUNCTION: prevents evaporation of the tear film / dryness of
the eye
ORBITAL SEPTUM
membranous sheet which forms the fibrous
framework of the eyelids
Medial canthal ligament
Lateral canthal ligament
Tarsus divides the contents of the orbit and eyelids;
without this, (+) flappy lids
Levator aponeurosis where the levator palpebrae
superioris inserts
HORDEOLUM
aka STYE
due to infection of the Gland of
Zeis
painful pimple-like with pus
course acute
treatment: oral and topical
antibiotic
CHALAZION (+) granuloma in the tarsal plate
due to obstruction of the
Meibomian gland
upon palpation, non-tender but
hard
treatment: warm compress;
incision
PTOSIS
drooping of the eyelids
depends on the etiology (e.g. weakness of the levator
palpebrae superioris; myasthenia gravis both eyes
have ptosis)
how to assess? Normally, the upper eyelids should
cover 1-2mm of the cornea. In patients with ptosis, the
upper eyelids cover 4mm of the cornea.
management: surgery depending on the etiology; sling
(tensor fascia latae is used)
DERMATOCHALASIS
seen in individuals as they age
management: removal of the excess fats (for cosmetic
reason)
Dermatochalasis
2 PANDA (Section 1A)
-
thin translucent membrane that lines the innermost
layer of the eyelids
its epithelium is continuous with that of the cornea
forms a potential space (conjunctival sac) which is
open at the palpebral fissure
Parts
Bulbar Conjunctiva covers the sclera
Palpebral Conjunctiva covers the eyelids
Fornix transition between the bulbar conjuctiva and
palpebral conjunctiva
Subtarsal sulcus groove beneath the eyelid which
runs close to and parallel with the margin of the lid
TENONS CAPSULE
fiber elastic membrane that envelopes the optic nerve
going to the ciliary body
located below the conjunctiva
it is where the eyeball moves
has 2 portions
1. SECRETORY lacrimal gland which rests on the
anterolateral surface of the orbital roof
2. COLLECTING - lacrimal duct and lacrimal
punctum which are seen on the medial aspect
LACRIMAL SYSTEM
(Flow of Tears)
Lacrimal Gland
Excretory Lacrimal Ducts
Lacrimal Canaliculus
Lacrimal Sac
Nasolacrimal Duct
Inferior Nasal Meatus
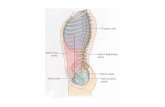
Orbital Margin base
Superior Frontal bone
Supraorbital notch
CONJUNCTIVA
The sulcus tends to trap small foreign particles introduced
into the conjunctival sac and is thus clinically important.
PTERYDIUM
mass that develops on the conjunctiva or cornea
management: removal of the mass and tenons
capsule (if tenons capsule is not removed, it can
recur)
LACRIMAL APPARATUS
ORBITAL BONES
3 PANDA (Section 1A)
-
Lateral Zygomatic bone
Zygomatic process of frontal bone
Inferior Zygomatic bone
Maxilla
Medial Process of maxilla
Frontal bone
Orbital Walls
Roof Frontal bone
Lesser wing of sphenoid bone
Lateral Zygomatic portion of frontal bone
Orbital portion of zygomatic bone
Greater wing of sphenoid
Medial Maxilla
Lacrimal
Ethmoid
Floor Palatine
Maxillary
Zygomatic
supraorbital notch or foramen
zygomatic foramina
infraorbital foramen
nasolacrimal canal
ethmoidal foramina
superior orbital fissure
inferior orbital fissure
optic canal
zygomaticotemporal foramen (to temporal fossa)
zygomaticofacial foramen (to cheek)
1. Supraorbital Notch or Foramen
supraorbital neurovascular bundle
supraorbital branch of frontal nerve (supraorbital
nerve) exits at the supraorbital notch in company with
the supraorbital artery
2. Infraorbital Foramen
orbital portion of the maxilla
infraorbital groove canal foramen
infraorbital neurovascular bundle (V2)
3. Nasolacrimal Canal
located anteriorly on the medial wall
separated from both the sinus and the nasal cavity by
a thin laminae of bone
lacrimal sac fossa to inferior meatus
transmits nasolacrimal duct (connects the lacrimal
punctum to the nose)
4. Inferior Orbital Fissure
located posteriorly between the maxilla and greater
wing of sphenoid
communicates with pterygopalatine fossa
maxillary nerve and zygomatic branch of
trigeminal nerve
IOV (inferior ophthalmic vein)
Sympathetic nerves
5. Ethmoidal Foramina
located on medial wall in ethmoid bone
anterior ethmoidal foramen br. nasociliary nerve
posterior ethmoidal foramen
6. Superior Orbital fissure
between the greater and lesser wing of sphenoid
transmits the following:
o oculomotor nerve (III)
o trochlear nerve (IV)
o trigeminal nerve (V)
lacrimal nerve
frontal nerve
nasociliary nerve
o abducent nerve (VI)
o SOV (superior ophthalmic vein)
the central portion is divided by the ANNULUS OF
ZINN (aka common tendinous ring; it is where the
extraocular muscles of the eyes originate except
superior oblique and inferior oblique muscles)
Superior Orbital Fissure
Inside the Annulus of Zinn Outside the Annulus of Zinn
Oculomotor nerve
(superior and inferior division)
Trochlear nerve
Abducens nerve Trigeminal nerve frontal and
lacrimal branches
Nasociliary nerve Ophthalmic veins
LATERAL WALL
thickest; has lower incidence of fracture
only entry point during removal of the tumors o Lateral orbitotomy - used for the removal
of orbital tumors and for orbital decompression.
MEDIAL WALL
Thinnest; not easily fractured because of the air sinuses
FLOOR
most commonly fractured because of its weak support
ORBITAL FLOOR FRACTURE
Manifestations:
patient cannot move his/her eyes because of the
impingement of inferior oblique and inferior rectus
muscles
diplopia
APERTURE / NOTCHES
4 PANDA (Section 1A)
-
7. Optic Canal
lesser wing of sphenoid
transmits optic nerve, ophthalmic artery and
central retinal vein
communicates with the middle cranial fossa
8. Zygomaticotemporal Foramen
transmits zygomaticotemporal nerve
9. Zygomaticofacial Foramen
transmits zygomaticofacial nerve
Muscles Origin Insertion
Recti Muscles Common tendinous ring Sclera
Superior
Oblique
Body of sphenoid Sclera; line of pull
of tendon passes
medial to vertical
axis
Inferior
Oblique
Floor of the orbit, lateral
to the opening of
nasolacrimal canal
Sclera behind
coronal equator
*Inferior oblique only extraocular muscle that do not originate
in the apex
Action of the Extraocular Muscles
EOM Primary Secondary Tertiary
Medial Rectus Adducts
Lateral Rectus Abducts
Sup. Rectus Elevates Adducts Intorts
Inf. Rectus Depresses Adducts Extorts
Sup. Oblique Depresses Abducts Intorts
Inf. Oblique Elevates Abducts Extorts
1. Optic Nerve
middle cranial fossa thru optic canal
pierces the sclera posteriorly
2. Trigeminal Nerve (CN V)
consists of a small motor component and a larger
sensory component
motor fibers - supply the masseter, temporalis,
internal pterygoid muscles, tensor tympani, tensor veli
palatini, omohyoid, and the anterior belly of the
digastrics muscle.
Three Main Divisions
a. Ophthalmic division
major sensory input from the eyelids and orbit
branches:
o frontal
o lacrimal
o nasociliary
b. Maxillary division
contributes a small component from the lower lid
branches:
o infraorbital
o zygomatic
MUSCLES OF THE ORBIT NERVES OF THE ORBIT
STRABISMUS
deviation in the eyes
medial strabismus / lateral strabismus
management: surgery of the EOM
GLAUCOMA
a medical condition wherein there is increased
intraocular pressure causing impingement of the
optic nerve
due to the impingement, there will be cupping of the
optic disc and nasalization of central retinal artery
common manifestations are:
o tunnel vision
o headache (one side of the head)
o blindness is irreversible
PAPILLEDEMA due to increased intracranial pressure bulging of
the lamina cribrosa (area of the sclera that is
pierced by the nerve fibers of the optic nerve) (+)
blurred disc border
manifestation: headache (both sides)
5 PANDA (Section 1A)
-
c. Mandibular division
3. Oculomotor Nerve (CN III)
carries somatic motor fibers to medial, superior and
inferior rectus muscles; inferior oblique muscle
and levator palpebrae superioris muscle
carries parasympathetic fibers to intrinsic muscles of
the eye and sensory neurons from proprioceptive
receptors in EOMs it innervates
within the main nerve trunk, pupillomotor fibers
maintain a superomedial position lesions located in
the cavernous sinus result in partial 3rd
nerve palsies
with sparing of pupillary function
4. Trochlear Nerve (CN IV)
innervate the contralateral superior oblique muscle
has a long intracranial course
part of its orbital extent lies adjacent to the bony wall,
thus, it is predisposed to injury from blunt head
trauma
5. Abducens Nerve (CN VI)
innervate the lateral rectus muscle
it is the last of the motor nerves to appear in
embryogenesis
first seen in 8th week stage of development
failure to develop may result in aberrant innervations
of the lateral rectus muscle by oculomotor nerve
(Duanes syndrome)
small, irregular, measuring 2mm horizontally by 1mm
vertically
postganglionic fibers pass from the ciliary ganglion
into 4 to 6 short posterior ciliary nerves
95% to 97% innervate the ciliary muscle
3% to 5% destined for the pupillary sphincter muscle
of the iris
lies about 10mm anterior to the superior orbital fissure
and 7mm anterior to the annulus of Zinn
BLOOD SUPPLY
In the adult, the vascular supply to the orbit derives
primarily from the INTERNAL CAROTID ARTERY.
OPHTHALMIC ARTERY carries the major blood
supply to the orbit in 96% of individuals.
In about 3%, the MIDDLE MENINGEAL ARTERY
shares equally through an enlarged accessory
ophthalmic (recurrent meningeal) branch.
In 1% of individuals, the MIDDLE MENINGEAL
ARTERY is the only source of arterial blood to the
orbit.
The order of branching along the arterial tree varies
considerably.
VENOUS DRAINAGE
Superior Ophthalmic Vein drains to cavernous sinus
Inferior Ophthalmic Vein drains to pterygoid plexus
Primary function to return to the vascular
compartment large protein molecules and excess fluid
extravasated into tissues from the blood
2 Divisions
1. Superficial system drains the skin and orbicularis
oculi muscle
2. Deep system drains the tarsus and the conjunctiva
Lymph Nodes Structures drained
Preauricular Nodes lateral 2/3 of the upper lid
lateral 1/3 of the lower lid
lateral half of the conjunctiva
Submandibular Nodes medial 1/3 of the upper eyelid
medial 2/3 of the lower eyelid
medial half of the conjunctiva
A. Coats of the Eyeball
Coats Parts
FIBROUS TUNIC Sclera
Cornea
VASCULAR TUNIC Iris
Ciliary body
Choroid
NERVOUS COAT
RETINA
Pigmented Layer
Neural Layer
1. FIBROUS COAT
SCLERA
dense connective tissue
white of the eye
anterior surface covered with tenons capsule and
episclera
CILIARY GANGLION
BLOOD SUPPLY & VENOUS DRAINAGE
OF THE ORBIT
Ophthalmic Artery
supplying branches to: (1) muscular arteries, (2)
central retinal artery, (3) ciliary artery
anastomosing with branches of external carotid
artery
LYMPHATIC SYSTEM
EYEBALL
6 PANDA (Section 1A)
-
2 openings:
o Anterior scleral foramen corneoscleral limbus
o Post scleral foramen (3mm medial to posterior
pole) optic nerve, CRV (exits the eye), CRA
(enters the eye), lamina cribrosa
ciliary arteries and nerves and their associated veins
(venae vorticosae)
Layers:
o Episclera: outermost, moderately dense,
vascularized connective tissue that merges with
scleral stroma
o Scleral stroma: types I and III collagen fibers
o Lamina fusca: innermost layer; composed of fine
collagen fibers derived from the sclera; connects
sclera and uveal tract
Blood supply: anterior ciliary arteries
Innervation:
o Anterior: 2 long ciliary nerves (nasociliary nerve
NV 1)
o Posterior: short ciliary nerves
CORNEA
anterior transparent 1/6th of the globe
corneoscleral limbus
main refracting surface of the eye
contacts posteriorly with aqueous humor
2. VASCULAR PIGMENTED COAT (UVEA)
CHOROID
composed of an outer pigmented layer and inner
highly vascular layer
located between the sclera on its outer side and
retinal pigmented epithelium on its inner side
gives nutrient to the eye
CILIARY BODY
continuous posteriorly with the choroid and anteriorly
it lies behind the peripheral margin of the iris
Uveal portion: ciliary muscle
Epithelial portion: secretes the posterior aqueous
humor
Ciliary Ring: posterior part of the body, surface has
shallow grooves (ciliary stria)
Ciliary Process: radially arranged in folds; connected
to suspensory ligament of the lens
Ciliary Muscle: meredianal and circular fibers of
smooth muscles connected to the zonular ligaments
which are important for the lens
IRIS
thin, contractile, pigmented diaphragm with a central
aperture called PUPIL
divides the space between the lens and cornea into
anterior and posterior chamber
Muscles Description Innervation Action
Sphincter
pupillae
Circular
(around the
margin of
pupil)
Parasympathetic
from CN III to
short ciliary
nerve
Constricts
(bright light,
accommodation)
Dilator
pupillae
Radial (lies
close to
posterior
surface)
Sympathetic to
long ciliary
nerve
Dilates
(low intensity
light, fright)
3. NERVOUS COAT (RETINA)
consists of an outer pigmented layer and inner
nervous layer
ORA SERRATA wavy ring; anterior edge of the
retina
MACULA LUTEA - highest visual acuity; oval,
yellowish area at the center of the posterior part of the
retina
penetrating trauma to sclera brownish material
from the sclera (choroid)
In glaucoma, there is blockage in the drainage of the
aqueous humor fluid haziness of the cornea (in acute
attack).
7 PANDA (Section 1A)
-
FOVEA CENTRALIS central depression within the
macula lutea
OPTIC DISC blind spot (absence of rods and
cones); where the optic nerve leaves the retina and it
is pierced by the central artery of the retina
During opthalmoscopy, you can see the following parts of the
retina:
Ora serrata
Macula lutea
Fovea centralis
Optic disc yellow orange in color; normal = distinct
disc border, normal cup:disc ratio
Central Retinal Artery/Vein
B. Contents of the Eyeball
1. AQUEOUS HUMOR
clear fluid that fills the anterior and posterior chamber
of the eye
functions:
o to support the wall of the eyeball by exerting
internal pressure and thus maintaining its
optical shape
o Nourishes the cornea and lens
o Removes the products of metabolism
Ciliary Body Posterior chamber between the iris & lens
Pupil Anterior chamber Trabecular meshwork Canal of
Schlemm Episcleral veins
2. LENS
transparent, biconvex structure enclosed in a
transparent capsule
situated behind the iris and in front of the vitreous
body
SUSPENSORY LIGAMENT: attaches the lens to the
ciliary processes of the ciliary body
part of the accommodation thickening of the lens
3. VITREOUS BODY transparent gel
produced by the ciliary body
fills the eyeball behind the lens
90% - water; others collagen, protein, etc.
If a light is shone into one eye, the pupils of both eyes
normally constrict. The constriction of the pupil on which the
light is shone is called the direct light reflex. The constriction
of the opposite pupil, even though no light fell on that eye, is
called the consensual light reflex.
CENTRAL SEROUS RETINOPATHY
fluid accumulation in the macula lutea that causes
visual impairment
individuals at risk are males who drinks alcohol,
smokes and age of 30-40
resolve by itself (3-6 months)
can be managed by laser
CATARACT opacity of the lens
ENOPHTHALMOS depressed eyeballs secondary to fracture
and surgery
EXOPHTHALMOS bulging of the eyeballs; common to
hyperthyroid patients
REFRACTIVE ERRORS
MYOPIA
near sightedness
parallel light rays come to focus in front of the retina
when eye is at rest
management: biconvex lens
HYPEROPIA
far sightedness
light rays from distant objects come to a focus in the
back of retina when eye is at rest
management: biconcave lens
PRESBYOPIA
reduced focusing power of the lens
loss of accommodation with age
management: bifocal lens
PUPILLARY REFLEXES
8 PANDA (Section 1A)