201108 Obstetrics 5
description
Transcript of 201108 Obstetrics 5

810 l AUGUST JOGC AOÛT 2011
Risk Factors for Postpartum Hemorrhage: Can We Explain the Recent Temporal Increase?Michael S. Kramer, MD,1,2 Mourad Dahhou, MSc,1 Danielle Vallerand,3
Robert Liston, MD,4,5,6 K.S. Joseph, MD, PhD4,5,6
1Department of Pediatrics, Faculty of Medicine, McGill University, Montreal QC2Department of Epidemiology, Biostatistics and Occupational Health, Faculty of Medicine, McGill University, Montreal QC3Department of Obstetrics and Gynecology, Faculty of Medicine, McGill University, Montreal QC4Department of Obstetrics and Gynaecology, University of British Columbia, Vancouver BC5School of Population and Public Health, University of British Columbia, Vancouver BC 6Children and Women’s Health Centre of British Columbia, Vancouver BC
OBSTETRICS
Key Words: Postpartum hemorrhage, maternal morbidity, labour induction, Caesarean Competing Interests: None declared .Received on February 8, 2011
Accepted on March 15, 2011
J Obstet Gynaecol Can 2011;33(8):810–819
Abstract
Objective: To assess risk factors for postpartum hemorrhage (PPH) and the extent to which changes in those risk factors may explain the rising incidence of PPH recently reported from industrialized countries .
Methods: We carried out a hospital-based cohort study of 103 726 consecutive deliveries from January 1, 1978, to January 31, 2007, from the computerized medical records of a tertiary-care university maternity hospital in Montreal . We examined adjusted odds ratios for any PPH (estimated blood loss > 500 mL for vaginal deliveries, > 1000 mL for Caesarean sections), severe PPH (estimated blood loss ≥ 1500 mL), and PPH accompanied by blood transfusion and/or hysterectomy .
Results: Major independent risk factors for PPH included primiparity, prior Caesarean section, placenta previa or low-lying placenta, marginal umbilical cord insertion in the placenta, transverse lie, labour induction and augmentation, uterine or cervical trauma at delivery, gestational age < 32 weeks, and birth weight ≥ 4500 g . An overall increase in rate of PPH over the study period (OR 1 .029; 95% CI 1 .024 to 1 .034 per year) disappeared (OR 0 .995; 95% CI 0 .988 to 1 .001 per year) after inclusion of maternal age, parity, prior Caesarean section, labour induction and augmentation, placenta previa or low-lying placenta, and abnormal placenta, with most of the reduction attributable to rises in previous Caesarean section and labour augmentation .
Conclusion: Labour induction, augmentation of labour, and prior Caesarean section are significantly associated with the risk of PPH, and their increase over the study period largely explains the observed rise in PPH .
Résumé
Objectif : Évaluer les facteurs de risque d’hémorragie postpartum (HPP) et la mesure dans laquelle les changements qu’ont connus ces facteurs de risque peuvent expliquer la hausse de l’incidence d’HPP récemment constatée au sein des pays industrialisés .
Méthodes : Nous avons mené une étude de cohorte en milieu hospitalier ayant porté sur 103 726 accouchements consécutifs (du 1er janvier 1978 au 31 janvier 2007) à partir des dossiers médicaux informatisés d’un hôpital de maternité universitaire de soins tertiaires de Montréal . Nous avons examiné les rapports de cotes corrigés en ce qui concerne toute HPP (perte sanguine estimée > 500 ml dans les cas d’accouchement vaginal, > 1 000 ml dans les cas de césarienne), l’HPP grave (perte sanguine estimée ≥ 1 500 ml) et l’HPP s’accompagnant d’une transfusion sanguine et/ou d’une hystérectomie .
Résultats : Parmi les principaux facteurs de risque indépendants d’HPP, on trouvait la primiparité, le fait d’avoir déjà subi une césarienne, le placenta praevia ou le placenta en présentation basse, une insertion marginale du cordon ombilical dans le placenta, une présentation transversale, le déclenchement et l’accélération du travail, un traumatisme utérin ou cervical au moment de l’accouchement, un âge gestationnel < 32 semaines et un poids de naissance ≥ 4 500 g . Une hausse globale du taux d’HPP au cours de la période d’étude (RC, 1,029; IC à 95 %, 1,024 – 1,034 par année) s’est estompée (RC, 0,995; IC à 95 %, 0,988 – 1,001 par année) à la suite de l’inclusion de l’âge maternel, de la parité, du fait d’avoir déjà subi une césarienne, du déclenchement et de l’accélération du travail, du placenta praevia ou du placenta en présentation basse et du placenta anormal, cette rectification à la baisse étant en grande partie attribuable à des hausses des taux de césarienne préalable et d’accélération du travail .
Conclusion : Les taux de déclenchement du travail, d’accélération du travail et de césarienne préalable sont significativement associés au risque d’HPP et leur hausse au cours de la période d’étude explique en grande partie la hausse constatée en ce qui concerne le taux d’HPP .

AUGUST JOGC AOÛT 2011 l 811
Risk Factors for Postpartum Hemorrhage: Can We Explain the Recent Temporal Increase?
INTRODuCTION
Postpartum hemorrhage (PPH) is a major cause of maternal mortality and severe morbidity, particularly
in low-income countries.1,2 Recently, however, several industrialized countries, including Australia, Canada, the United Kingdom, and the United States, have reported an increasing incidence of PPH.3–6
It is well recognized that appropriate obstetric management (in particular, active management of the third stage of labour) and access to blood transfusion and, if necessary, hysterectomy, can prevent mortality and severe morbidity once PPH occurs.7 Less is known, however, about individual-level risk factors for the occurrence of PPH.8 Perhaps more importantly, the reasons for the recent increase in its occurrence are unknown. An international PPH collaborative group met and published a summary of the recent evidence, as well as recommendations for future surveillance and research.9 Reasons speculated for the temporal increase include the rises in maternal obesity,10,11 previous Caesarean section,5,12,13 multiple pregnancy,5,8,12,14 and differences in the management of labour (including induction and augmentation of labour and epidural anaesthesia).8,9,15 Evidence supporting these possible explanations is extremely limited, however.5,6 We took advantage of a clinically rich hospital database comprising deliveries over three decades to examine a number of these hypothesized risk factors and their relationship to the occurrence and severity of PPH, as well as to assess whether changes in the prevalence of these risk factors could explain the observed temporal changes.
METHODS
We carried out a hospital-based, historical cohort study based on consecutive deliveries recorded in a perinatal record system, the McGill Obstetrics and Neonatal Database. This is a computerized archive that contains maternal anthropometric data, detailed clinical and sociodemographic information, obstetric history, and pregnancy and neonatal outcomes for all births at Montreal’s Royal Victoria Hospital since 1978. Maternal and infant medical records are the raw data source for the McGill Obstetrics and Neonatal Database and contain the antenatal record and a range of neonatal and obstetric forms that are completed during the birth hospitalization. These data are routinely verified for accuracy and completeness prior to computer entry.The study sample was restricted to singleton deliveries that occurred between January 1, 1978, and January 31, 2007. Until March 2001, PPH was coded as “yes” or “no,” on the basis of the delivering obstetrician’s estimate of blood loss during and after delivery: > 500 mL for vaginal deliveries
and > 1000 mL for Caesarean section. A new version of the McGill Obstetrics and Neonatal Database was initiated in April 2001 and contains additional variables not previously included in the database, including a quantitative estimate of postpartum blood loss. Based on that estimate, we used the same definition as previously for any PPH, but we also defined severe postpartum hemorrhage as a postpartum blood loss ≥ 1500 mL. Because of the subjectivity and variability inherent in estimating blood loss, we also analyzed cases of PPH in which the delivering woman received a blood transfusion and/or underwent hysterectomy during her hospital stay.
Potential risk factors under study included maternal age, parity, marital/cohabitation status, smoking during pregnancy, history of infertility, previous history of spontaneous abortion, previous Caesarean section, other uterine surgery, uterine fibroids, pre-pregnancy BMI, pre-pregnancy hypertension, pregnancy-induced hypertension (including preeclampsia), pre-pregnancy or gestational diabetes or impaired glucose tolerance, fetal presentation, abnormal placentation, amniotic fluid volume, induction of labour, augmented labour, cervical or vaginal trauma, delivery, placenta previa or low-lying placenta (considered together), tocolysis, and infant birth weight and gestational age.
Descriptive statistics for the potential risk factors in the overall sample of deliveries over the study period were analyzed, as were bivariate relationships between these potential risk factors and both any PPH and severe PPH. Multiple logistic regression analysis was used to assess the independent associations between each of the risk factors and the occurrence of any PPH and (for 2002 to 2007) of severe PPH. To ensure that clustering of outcomes in women with two or more deliveries at the study hospital during the study period did not influence the results, we also carried out a sensitivity analysis in which we randomly selected one delivery for such women and repeated the multiple logistic regression analysis.
Temporal trends were assessed graphically and by analyzing the association between year of delivery and the occurrence of any PPH. These trends were examined only for any PPH, since data for severe PPH are available for only the last five years of the study period. Data for 2007 were excluded from the trend analysis, since only January deliveries had been recorded in the database for that year. Potential risk factors were also examined for temporal trends, using similar methods. Those risk factors and covariates that varied over time were then analyzed sequentially to examine their impact on the overall temporal trend in the occurrence of PPH. All statistical analyses were performed with SAS version 9.1 (SAS Institute, Cary NC).

812 l AUGUST JOGC AOÛT 2011
OBSTETRICS
Table 1. Description of study cohort (n = 103 726)Variable %Maternal age, years
< 20 2 .320 to 34 80 .1≥ 35 17 .6
Parity0 47 .11 35 .42 to 4 16 .7≥ 5 0 .8
Civil statusMarried (legal or common-law) 83 .5Single, living alone 14 .7Separated, divorced, widowed 1 .8
Maternal education, years (n = 81 849)< 11 12 .211 to 12 26 .013 to 15 26 .3≥ 16 35 .5
Height, cm (n = 60 317)< 160 29 .2160 to 170 61 .0> 170 9 .7
Pre-pregnancy BMI, kg/m2 (n = 52 387)< 18 .5 9 .418 .5 to < 25 68 .225 to < 30 15 .5≥ 30 6 .9
Smoking in pregnancy 16 .6Prior spontaneous abortion 18 .4History of infertility (n = 52 431) 3 .3Prior Caesarean section 10 .8History of uterine surgery 0 .4Fibroids 1 .9Pre-pregnancy hypertension 1 .3Pregnancy-induced hypertension/preeclampsia 7 .4Pre-pregnancy or gestational diabetes, or impaired glucose tolerance
5 .4
Amniotic fluid volumeNormal 93 .2Polyhydramnios 1 .7Oligohydramnios 5 .0
Placenta previa or low-lying placenta 0 .8Gross placental pathology
Normal 87 .9Infarction 0 .9Marginal cord insertion 4 .4Circumvallate placenta 0 .7Chorangioma 2 .7Other abnormality 3 .4
continued
Table 1. continuedVariable %
Fetal presentation
Cephalic 94 .9
Breech 4 .2
Transverse 0 .4
Compound 0 .3
Oblique 0 .1
Other 0 .1
Induced labour 23 .2
Labour augmentation 30 .4
Duration of labour >12 hours (n = 94 115) 24 .6
Tocolytic therapy 6 .6
Labour anaesthesia
None 12 .7
Spinal 3 .0
Epidural 12 .4
Combined spinal/epidural 1 .1
Other 70 .8
Labour analgesia
None 97 .6
Narcotic 2 .2
Other 0 .2
Delivery mode
Spontaneous vaginal 64 .9
Forceps or vacuum 13 .8
Caesarean section 21 .3
Trauma at delivery
None 63 .9
Uterine 0 .2
Cervical 0 .3
Other (vaginal, perineal) 35 .6
Gestational age, weeks
< 32 1 .9
32 to 36 7 .0
≥ 37 91 .1
Birth weight, g
< 2500 6 .3
2500 to 3999 82 .8
4000 to 4499 9 .5
≥ 4500 1 .5

AUGUST JOGC AOÛT 2011 l 813
Risk Factors for Postpartum Hemorrhage: Can We Explain the Recent Temporal Increase?
RESuLTS
A total of 103 726 deliveries occurred at the study hospital during the study period, among which 2346 (2.3%) had a recorded PPH and 157 (0.15%) had a PPH accompanied by a blood transfusion and/or hysterectomy. Of the 20 445 deliveries since April 2001, 39 (0.19%) had severe PPH (estimated blood loss ≥ 1500 mL).
The study sample is summarized in Table 1 according to the risk factors and covariates under study. The bivariate (crude) relationship between each of the potential risk factors and covariates and the occurrence of any PPH and severe PPH is shown in Table 2. PPH was significantly associated with older maternal age, unmarried status, nulliparity or multiparity, maternal overweight/obesity, noncephalic presentation (other than breech), abnormal placenta, history of infertility, uterine surgery, prior Caesarean section, pre-pregnancy hypertension, pregnancy-induced hypertension, diabetes or impaired glucose tolerance, polyhydramnios, placenta previa or low-lying placenta, uterine or cervical trauma at delivery, Caesarean section in the index birth, labour induction, labour augmentation, tocolytic therapy, preterm birth, and both low and high birth weight. Neither anaesthesia nor analgesia type was associated with the risk of PPH, and smoking was significantly (albeit very modestly) inversely related to the risk of PPH. A graded increase in risk of any PPH was observed with increasing maternal pre-pregnancy BMI, although data on the latter variable were available for only half the overall study sample. Most of the factors associated with the risk of any PPH were also associated with severe PPH, although the much smaller sample size and low rate of occurrence (< 10% of the rate for total PPH) resulted in higher P values for severe PPH.
The results of the multiple logistic regression analysis for PPH and severe PPH are shown in Table 3. Pre-pregnancy and pregnancy-induced hypertension, transverse or compound presentation, abnormal placenta, prior Caesarean section, preterm birth, high birth weight, nulliparity, multiparity, uterine or cervical trauma during delivery, and placenta previa or low-lying placenta remained significantly associated with the risk of PPH. Of note, labour induction, augmentation of labour, and tocolytic therapy remained significantly associated with the risk of PPH. Both Caesarean section and operative vaginal delivery (forceps or vacuum) in the index birth were also significantly associated with PPH risk. The largest odds ratios were associated with transverse lie, previous Caesarean section, early preterm birth, and uterine and cervical trauma during delivery. Odds ratios for severe PPH were highest for older maternal age, the extremes of parity, pre-pregnancy hypertension, fibroids,
prior Caesarean section, prior uterine surgery, transverse lie, early preterm birth, placenta previa and low-lying placenta, and Caesarean section for the index birth. The results shown in Table 3 do not include maternal pre-pregnancy BMI or history of infertility, because a logistic model that included those variables in addition to those shown in this Table showed no significant association between PPH and either of these variables, and the sample size was severely reduced (n = 19 929) because of the large proportion of subjects with missing values for those variables (Tables 1 and 2). Logistic regression analysis for PPH accompanied by blood transfusion and/or hysterectomy yielded similar results to those for severe PPH, except for higher adjusted ORs for trauma at delivery: 6.5 (95% CI 2.2 to 1.3) for uterine trauma and 20.0 (95% CI 6.0 to 66.5) for cervical trauma.
The sensitivity analysis (inclusion of only one randomly selected birth for mothers with two or more births recorded in the database during the study period) yielded very similar results to those presented above for the entire sample of births. The sample size was reduced from 103 726 to 69 121 in the sensitivity analysis, and thus confidence intervals around the point estimates were wider. Statistically significant risk factors in the multiple logistic regression analysis included primiparity (aOR 1.4; 95% CI 1.2 to 1.7), parity 2 to 4 (aOR 1.3; 95% CI 1.1 to 1.6), prior Caesarean section (aOR 1.3; 95% CI 1.04 to 1.6), pregnancy-induced hypertension (aOR 1.4; 95% CI 1.2 to 1.7), transverse lie (aOR 3.1; 95% CI 1.9 to 5.2), marginal cord insertion (aOR 1.4; 95% CI 1.1 to 1.7), other abnormal placentation (aOR 1.8; 95% CI 1.4 to 2.2), birth weight 4000 to 4499 g (aOR 1.6; 95% CI 1.5 to 2.1), birth weight ≥ 4500 g (aOR 2.6; 95% CI 1.9 to 3.5), gestational age < 32 weeks (aOR 2.9; 95% CI 1.7 to 4.7), induced labour (aOR 1.2; 95% CI 1.1 to 1.4), uterine (aOR 4.6; 95% CI 2.6 to 8.1) or cervical (aOR 3.1; 95% CI 1.4 to 6.7) trauma at delivery, placenta previa or low-lying placenta (aOR 3.6; 95% CI 2.6 to 5.0), forceps or vacuum delivery (aOR 1.6; 95% CI 1.3 to 1.9), and Caesarean section for the index birth (aOR 1.3; 95% CI 1.1 to 1.6). Risk factors that were no longer significant in the sensitivity analysis were augmentation of labour (aOR 1.1; 95% CI 1.0 to 1.3) and tocolytic therapy (aOR 1.2; 95% CI 1.0 to 1.6).
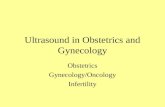
The yearly rate (proportion of all deliveries) of PPH from 1978 to 2006 is shown in the Figure. The rate rose, albeit irregularly, from 1978 to 1994, declined from 1994 to 1997, and then remained stable until 2006. The rates of several of the risk factors significantly associated with PPH also rose during the study period, including induction of labour, augmentation of labour, previous Caesarean

814 l AUGUST JOGC AOÛT 2011
OBSTETRICS
Table 2. Variations in rates (%) of PPH and severe PPH by risk factors and covariates
VariablePPH
(n = 103 726)Severe PPH (n = 20 445)
Maternal age, years *** ***
< 20 1 .7 0 .37
20 to 34 2 .2 0 .10
≥ 35 2 .7 0 .41
Parity ***
0 2 .6 0 .18
1 1 .8 0 .15
2 to 4 2 .3 0 .32
≥ 5 3 .1 0 .43
Civil status **
Married (legal or common-law) 2 .2 0 .17
Single, living alone 2 .5 0 .29
Separated, divorced, widowed 3 .0 0 .30
Maternal education, years (n = 81 849)
< 11 2 .4 0 .31
11 to 12 2 .5 0 .19
13 to 15 2 .6 0 .20
≥ 16 2 .5 0 .14
Height, cm
< 160 2 .1 0 .20
160 to 170 2 .2 0 .19
> 170 2 .3 0 .08
Pre-pregnancy BMI, kg/m2 (n = 52 387)
***
< 18 .5 1 .7 0 .00
18 .5 to < 25 2 .1 0 .27
25 to < 30 2 .8 0 .06
≥ 30 3 .0 0 .09
Smoking in pregnancy *
Yes 2 .0 0 .31
No 2 .3 0 .18
Prior spontaneous abortion *
Yes 3 .0 0 .29
No 2 .7 0 .15
History of infertility (n = 52 431) ***
Yes 4 .8 0 .24
No 2 .6 0 .19
Prior Caesarean section ** ***
Yes 3 .0 0 .56
No 2 .5 0 .14
History of uterine surgery ** ***
Yes 4 .2 2 .01
No 2 .3 0 .18
continued
Table 2. continued
VariablePPH
(n = 103 726)Severe PPH (n = 20 445)
Fibroids **
Yes 2 .8 0 .68
No 2 .3 0 .17
Pre-pregnancy hypertension *** ***
Yes 4 .1 1 .14
No 2 .2 0 .18
Pregnancy-induced hypertension/preeclampsia
***
Yes 3 .5 0 .11
No 2 .2 0 .19
Pre-pregnancy or gestational diabetes, or impaired glucose tolerance
***
Yes 3 .2 0 .20
No 2 .2 0 .19
Amniotic fluid volume ***
Normal 2 .2 0 .19
Polyhydramnios 3 .6 0 .31
Oligohydramnios 2 .2 0 .15
Placenta previa or low-lying placenta
*** ***
Yes 9 .3 3 .81
No 2 .2 0 .15
Gross placental pathology *** *
Normal 2 .1 0 .16
Infarction 3 .3 0 .75
Marginal cord insertion 3 .7 0 .24
Circumvallate placenta 3 .4 0 .23
Chorangioma 2 .5 0 .26
Other abnormality 4 .1 0 .73
Fetal presentation *** ***
Cephalic 2 .2 0 .17
Breech 1 .7 0 .42
Transverse 10 .2 3 .75
Compound 4 .7 0 .00
Oblique 3 .8 0 .00
Other 1 .7 0 .00
Induced labour ***
Yes 2 .6 0 .10
No 2 .1 0 .23
Labour augmentation
Yes 2 .8 0 .11
No 2 .5 0 .23
Duration of labour, hours ***
≤ 12 2 .1 0 .20
> 12 2 .8 0 .15
continued

AUGUST JOGC AOÛT 2011 l 815
Risk Factors for Postpartum Hemorrhage: Can We Explain the Recent Temporal Increase?
Table 2. continued
VariablePPH
(n = 103 726)Severe PPH (n = 20 445)
Tocolytic therapy **
Yes 2 .8 0 .24
No 2 .2 0 .19
Labour anaesthesia ***
None 2 .5 0 .39
Spinal 2 .5 0 .62
Epidural 2 .1 0 .05
Combined spinal/epidural 2 .1 0 .23
Other 2 .2 0 .00
Labour analgesia
None 2 .3 0 .20
Narcotic 2 .1 0 .00
Other 1 .7 0 .00
Delivery mode *** ***
Spontaneous vaginal 2 .0 0 .05
Forceps or vacuum 2 .4 0 .08
Caesarean section 3 .0 0 .61
Trauma at delivery *** **
None 2 .4 0 .26
Uterine 9 .6 1 .08
Cervical 4 .7 0 .00
Other (vaginal, perineal) 2 .4 0 .04
Gestational age, weeks *** ***
< 32 3 .9 1 .04
32 to 36 2 .5 0 .36
≥ 37 2 .2 0 .16
Birth weight, g *** **
< 2500 2 .4 0 .59
2500 to 3999 2 .1 0 .16
4000 to 4499 3 .7 0 .26
≥ 4500 4 .2 0 .00* P < 0 .05
** P < 0 .01
*** P < 0 .001
section, placenta previa or low-lying placenta, abnormal placentation, older maternal age, and parity ≥ 5.
Over the entire study period, we estimated the average yearly effect (OR; 95% CI) estimated from univariable logistic regression analysis as 1.029 (1.024 to 1.034). We then sequentially entered the following additional variables that were significantly positively associated with PPH in the logistic regression analysis and that showed graphical evidence of a temporal increase during the study period: maternal age, parity, prior Caesarean section, labour induction, augmentation of labour, placenta previa or low-
lying placenta, and abnormal placenta. As shown in Table 4, the OR for the yearly term diminished at each step, and after all of these seven risk factors were entered into the model, it became non-significant (OR 0.995; 95% CI 0.988 to 1.001). This suggests that in the absence of temporal trends in these seven risk factors, no overall rise in PPH incidence would have been observed over the study period. The largest decreases in the yearly effect were observed with prior Caesarean section and labour augmentation, suggesting that temporal increases in the rates of these two obstetric interventions were responsible for most of the crude rise in PPH.
When we restricted the trend analysis to the period of observed increase in PPH incidence (see Figure), i.e., from 1978 to 1994, the yearly crude OR was 1.152 (95% CI 1.138 to 1.167), but the inclusion of the above-mentioned risk factors reduced the yearly effect to 1.108 (95% CI 1.089 to 1.128). In other words, the temporal trend in these seven risk factors explained only 0.044/0.152 (29%) of the observed yearly increase from 1978 to 1994. When we examined the temporal decline in PPH incidence observed from 1994 to 1997, the yearly decrease (crude OR 0.741; 95% CI 0.678 to 0.810) was unaffected by changes in the seven risk factors (aOR 0.737; 95% CI 0.674 to 0.807).
A crude rise in severe PPH incidence was observed over the short interval (2001 to 2006) in which this variable was classifiable in the database (crude yearly OR 1.145; 95% CI 0.940 to 1.395), but the low overall rate of occurrence (0.19% of deliveries) led to a highly imprecise and non-significant estimate. Similarly, the low rate of occurrence of PPH accompanied by blood transfusion and/or hysterectomy (0.15%) showed no significant increase over the entire study period (crude yearly OR 1.009; 95% CI 0.990 to 1.029).
DISCuSSION
We studied a large number of potential risk factors for postpartum hemorrhage, including many that are not available in population-based birth registries or databases of hospital discharges. These potentially important risk factors include placenta previa, abnormal gross placental pathology, fetal presentation, duration of labour, uterine and cervical trauma at delivery, and uterine fibroids. We confirmed previously reported associations with prior Caesarean section, labour induction and augmentation, and fetal macrosomia.8,15 In addition, we observed increased risks associated with transverse lie, marginal umbilical cord insertion in the placenta, placenta previa or low-

816 l AUGUST JOGC AOÛT 2011
OBSTETRICS
Table 3. Results of multiple logistic regression analyses
VariablePPH
aOR (95% CI)Severe PPH
aOR (95% CI)
Maternal age, years
< 20 0 .8 (0 .5 to 1 .2) 4 .7 (0 .5 to 42 .2)
20 to 34 1 .0 (reference) 1 .0 (reference)
≥ 35 1 .0 (0 .9 to 1 .2) 2 .9 (1 .3 to 6 .6)
Parity
0 1 .5 (1 .4 to 1 .7) 2 .4 (0 .7 to 8 .2)
1 1 .0 (reference) 1 .0 (reference)
2 to 4 1 .3 (1 .1 to 1 .5) 1 .9 (0 .7 to 5 .0)
≥ 5 1 .4 (0 .9 to 2 .2) 4 .5 (0 .5 to 40 .3)
Civil status
Married (legal or common-law) 1 .0 (reference) 1 .0 (reference)
Single, living alone 1 .0 (0 .8 to 1 .1) 2 .1 (0 .9 to 4 .8)
Separated, divorced, widowed 1 .2 (0 .9 to 1 .7) 1 .5 (0 .2 to 12 .1)
Smoking in pregnancy 1 .0 (0 .9 to 1 .1) 1 .7 (0 .6 to 5 .0)
Prior spontaneous abortion 1 .1 (1 .0 to 1 .2) 1 .3 (0 .6 to 2 .7)
Prior Caesarean section 1 .4 (1 .2 to 1 .6) 3 .1 (1 .0 to 10 .1)
History of uterine surgery 1 .3 (0 .8 to 2 .3) 4 .6 (1 .2 to 17 .7)
Fibroids 0 .8 (0 .6 to 1 .1) 4 .0 (1 .4 to 11 .4)
Pre-pregnancy hypertension 1 .3 (0 .9 to 1 .8) 4 .8 (1 .2 to 19 .5)
Pregnancy-induced hypertension/preeclampsia
1 .4 (1 .2 to 1 .6) 0 .2 (0 .02 to 1 .7)
Pre-pregnancy or gestational diabetes, or impaired glucose tolerance
1 .1 (0 .9 to 1 .3) 0 .3 (0 .1 to 1 .4)
Amniotic fluid volume
Normal 1 .0 (reference) 1 .0 (reference)
Polyhydramnios 1 .3 (1 .0 to 1 .7) 1 .2 (0 .2 to 5 .9)
Oligohydramnios 0 .8 (0 .7 to 1 .1) 0 .2 (0 .02 to 1 .3)
Placenta previa or low-lying placenta 3 .5 (2 .7 to 4 .5) 17 .1 (6 .2 to 46 .7)
Gross placental pathology
Normal 1 .0 (reference) 1 .0 (reference)
Infarction 1 .2 (0 .8 to 1 .8) 3 .9 (0 .4 to 34 .0)
Marginal cord insertion 1 .5 (1 .2 to 1 .8) 1 .6 (0 .5 to 5 .0)
Circumvallate placenta 1 .5 (1 .0 to 2 .3) 2 .0 (0 .3 to 16 .1)
Chorangioma 0 .9 (0 .7 to 1 .2) 1 .1 (0 .1 to 8 .4)
Other abnormality 1 .5 (1 .3 to 1 .9) 2 .8 (0 .8 to 9 .0)
Fetal presentation
Cephalic 1 .0 (reference) reference
Breech 0 .7 (0 .5 to 0 .9) reference
Transverse 3 .4 (2 .3 to 5 .1) 7 .3 (1 .8 to 30 .0)*
Compound 1 .9 (1 .03 to 3 .3) reference
Oblique 1 .2 (0 .4 to 4 .0) reference
Other 0 .6 (0 .1 to 2 .5) reference
Induced labour 1 .2 (1 .1 to 1 .4) 0 .8 (0 .2 to 2 .7)
Labour augmentation 1 .2 (1 .1 to 1 .4) 0 .7 (0 .2 to 2 .6)
Tocolytic therapy 1 .3 (1 .1 to 1 .5) 0 .4 (0 .1 to 2 .2)
continued

AUGUST JOGC AOÛT 2011 l 817
Risk Factors for Postpartum Hemorrhage: Can We Explain the Recent Temporal Increase?
Table 3. continued
VariablePPH
aOR (95% CI)Severe PPH
aOR (95% CI)
Duration of labour > 12 hours 1 .0 (0 .9 to 1 .2) 1 .9 (0 .7 to 5 .6)
Delivery mode
Spontaneous vaginal 1 .0 (reference) 1 .0 (reference)
Forceps or vacuum 1 .5 (1 .3 to 1 .7) 1 .9 (0 .2 to 16 .1)
Caesarean section 1 .3 (1 .1 to 1 .5) 4 .8 (1 .4 to 16 .0)
Trauma at delivery
None 1 .0 (reference) 1 .0 (reference)
Uterine 3 .8 (2 .4 to 6 .2) 0 .7 (0 .2 to 2 .8)†
Cervical 4 .0 (2 .3 to 7 .0)
Other (vaginal, perineal) 1 .1 (1 .0 to 1 .2)
Gestational age, weeks
< 32 2 .9 (1 .9 to 4 .4) 7 .3 (1 .0 to 56 .6)
32 to 36 1 .3 (1 .04 to 1 .5) 1 .7 (0 .4 to 6 .3)
≥ 37 1 .0 (reference) 1 .0 (reference)
Birth weight, g
< 2500 0 .6 (0 .4 to 0 .8) 1 .0 (0 .2 to 5 .4)
2500 to 3999 1 .0 (reference) 1 .0 (reference)
4000 to 4499 1 .8 (1 .6 to 2 .1) 1 .2 (0 .4 to 3 .6)‡
≥ 4500 2 .2 (1 .6 to 2 .8)* Because of insufficient numbers, transverse lie was compared to all other presentations .
† Because of insufficient numbers, uterine, cervical, vaginal, and perineal trauma were combined into a single category .
‡ Because of insufficient numbers, birth weights ≥ 4000g were combined into a single category .
Table 4. Sequential logistic regression analysis of temporal (yearly) trends in PPH
OR (95%)
Year only 1 .029 (1 .024 to 1 .034)
Plus maternal age 1 .028 (1 .023 to 1 .033)
Plus parity 1 .027 (1 .022 to 1 .033)
Plus prior Caesarean section 1 .006 (1 .000 to 1 .012)
Plus labour induction 1 .005 (0 .999 to 1 .011)
Plus augmentation 0 .998 (0 .992 to 1 .004)
Plus placenta previa or low-lying placenta 0 .997 (0 .991 to 1 .004)
Plus abnormal placenta 0 .995 (0 .988 to 1 .001)
lying placenta, uterine or cervical trauma at delivery, and gestational age < 32 weeks. For the last six years of the study (2001 to 2006), we were also able to study risk factors associated with severe PPH, defined as postpartum blood loss ≥ 1500 mL. Strong associations with severe PPH were observed for maternal age ≥ 35 years, prior Caesarean section, history of uterine surgery, uterine fibroids, pre-pregnancy hypertension, placenta previa or low-lying placenta, transverse presentation, and gestational age < 32 weeks. Similar associations were observed over the entire study period for PPH accompanied by blood transfusion and/or hysterectomy and were extremely strong with uterine or cervical trauma at delivery.
We observed a temporal increase in the incidence of PPH at the study hospital over the study period. The rise was not continuous, however, decreasing between 1994 and 1997 and stabilizing (at a rate of approximately 2% of deliveries) from 1997 to 2006. We observed temporal increases in the rates of several of the important risk factors for PPH, including prior Caesarean section, labour induction, augmentation of labour, placenta previa or low-lying placenta, and abnormal placenta. Once these five risk factors were entered into a multiple logistic
regression model, along with maternal age and parity, the crude increase in occurrence of PPH over the study period disappeared, suggesting that in the absence of temporal changes in these risk factors, the hospital would not have experienced any rise in the occurrence of PPH. Previous population-based studies from Canada5 and Australia6 have not succeeded in explaining temporal trends in PPH incidence by concurrent trends in the incidence of risk factors, perhaps because of their reliance on ICD-based diagnoses and procedure codes and limited information

818 l AUGUST JOGC AOÛT 2011
OBSTETRICS
on prior clinical history, details of labour and delivery, and placental examination.
Although the benefit of routine post-term induction of labour has been convincingly demonstrated,16 recent reports have documented substantial increases in rates of induction even at early term and late preterm gestations.17–22 When combined with reports of increased risk of amniotic fluid embolism associated with labour induction,23,24 our findings suggest that recent interventionist policies regarding labour and delivery may have adverse consequences for the mother in addition to those recently reported for the newborn infant and for subsequent child development.25–27
Several limitations of this study should be acknowledged. Primary among these is the fact that the study is based on deliveries from a single hospital. This is a tertiary-care referral hospital, and although the referral base did not change over the study period, we have no way of assessing whether more or different kinds of women at high risk for PPH were delivered at the study hospital over this period. Other selection factors might be operating that could bias associations between risk factors and PPH upwards or downwards, although many of the risk factors we identified are consistent with those reported in previously published studies.8 We have no data on placenta accreta or percreta, which could have been used to better understand the relationship between prior Caesarean section or other uterine surgery and the occurrence of PPH in subsequent pregnancies. Nor can we ensure the validity of obstetricians’ estimates of blood loss during or after delivery, or their uniformity over the prolonged
study period. The similar results observed in our analysis of PPH accompanied by blood transfusion and/or hysterectomy, however, strengthen the validity of our overall findings. Our inability to determine the temporal sequence of risk factors and PPH is another limitation of our data source. Thus the positive association of PPH with Caesarean section for the index birth may reflect the use of Caesarean section to control excessive bleeding, rather than it being a cause of subsequent bleeding. We also have no assurance that blood transfusions or hysterectomies occurred after (rather than before) the PPH in all cases. The temporal increase in some risk factors could be partly explained by closer diagnostic surveillance, especially for those diagnosed by ultrasound: placenta previa or low-lying placenta, fibroids, and polyhydramnios. As shown in Table 4, however, placenta previa or low-lying placenta was the only one of these factors whose rise had a perceptible impact on the temporal increase in PPH, and that impact was small. Finally, no observational study (including ours) can adequately control for confounding by indication for such obstetric interventions as labour induction and augmentation. Thus uterine hypotonicity (of any or unknown cause) may be an underlying cause of labour induction and/or augmentation and may lead to PPH independently of these obstetric interventions.
Strengths of our study include the large number of deliveries, consistently extracted and coded risk factors and pregnancy complications, and a study period that was long enough to observe and assess risk factors for temporal trends.
0
1
2
3
4
5
6
1978 1982 1986 1990 1994 1998 2002 2006
Rat
e (%
)
Birth year
Temporal (yearly) trend in occurrence of any PPH, Royal Victoria Hospital, 1978–2006

AUGUST JOGC AOÛT 2011 l 819
Risk Factors for Postpartum Hemorrhage: Can We Explain the Recent Temporal Increase?
CONCLuSION
Our results suggest that the temporal increase in the incidence of PPH, at least at the study hospital, was attributable to rises in the incidence of several key risk factors, including previous Caesarean section, labour induction and augmentation, placenta previa, and abnormal placentation. These results raise some troubling questions about the consequences of current trends in obstetric intervention, particularly the rises in rates of Caesarean section, labour induction, and augmentation of labour. The evidence suggests an urgent need for randomized trials of these interventions to ensure that the benefits of their increased use outweigh their harmful effects.
ACKNOWLEDGEMENTS
Our study was funded by a grant from the Canadian Institutes of Health Research.
REFERENCES
1. World Health Organization. The world health report: 2005: make every mother and child count. Geneva: WHO; 2005.
2. Miniño AM, Heron MP, Murphy SL, Kochanek KD; Centers for Disease Control and Prevention National Center for Health Statistics National Vital Statistics System. Deaths: final data for 2004. Natl Vital Stat Rep 2007;55:1–119.
3. Cameron CA, Roberts CL, Olive EC, Ford JB, Fischer WE. Trends in postpartum haemorrhage. Aust N Z J Public Health 2006;30:151–6.
4. Haynes K, Stone C, King J. Major morbidities associated with childbirth in Victoria: obstetric haemorrhage and associated hysterectomy. Melbourne: Public Health Group, Department of Human Services; 2004.
5. Joseph KS, Rouleau J, Kramer MS, Young DC, Liston RM, Baskett TF. Investigation of an increase in postpartum haemorrhage in Canada. BJOG 2007;114:751–59.
6. Ford JB, Roberts CL, Simpson JM, Vaughan J, Cameron CA. Increased postpartum hemorrhage rates in Australia. Int J Gynaecol Obstet 2007;98:237–43.
7. Cabero Roura L, Keith LG. Post-partum haemorrhage: diagnosis, prevention and management. J Matern Fetal Neonat Med 2009;22:38–45.
8. Al-Zirqi I, Vangen S, Forsen L, Stray-Pedersen B. Prevalence and risk factors of severe obstetric haemorrhage. BJOG 2008;115:1265–72.
9. Knight M, Callaghan WM, Berg C, Alexander S, Bouvier-Colle M-H, Ford JB, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International
Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth 2009;9:55.
10. Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol 2005;106:1357–64.
11. Sebire NJ, Jolly M, Harris JP, Wadsworth J, Joffe M, Beard RW, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes 2001;25:1175–82.
12. Knight M, Kurinczuk JJ, Spark P, Brocklehurst P. Cesarean delivery and peripartum hysterectomy. Obstet Gynecol 2008;111:97–105.
13. Daltveit AK, Tollånes MC, Pihlstrøm H, Irgens LM. Cesarean delivery and subsequent pregnancies. Obstet Gynecol 2008;111:1327–34.
14. Cruikshank DP. Intrapartum management of twin gestations. Obstet Gynecol 2007;109:1167–76.
15. Guerra GV, Cecatti JG, Souza JP, Faundes A, Morais SS, Gulmezoglu AM, et al. Factors and outcomes associated with the induction of labour in Latin America. BJOG 2009;116:1762–72.
16. Sanchez-Ramos L, Olivier F, Delke I, Kaunitz AM. Labor induction versus expectant management for postterm pregnancies: a systematic review with meta-analysis. Obstet Gynecol 2003;101:1312–8.
17. Zhang J, Yancey MK, Henderson CE. U.S. national trends in labor induction, 1989–1998. J Reprod Med 2002;47:120–4.
18. MacDorman MF, Mathews TJ, Martin JA, Malloy MH. Trends and characteristics of induced labour in the United States, 1989–98. Paediatr Perinat Epidemiol 2002;16:263–73.
19. Russell SK. Trends in labor induction in the United States: is it true that what goes up must come down? Birth 2004;31:148–51.
20. Wing DA. Elective induction of labor in the USA. Curr Opin Obstet Gynecol 2000;12:457–62.
21. Rayburn WF, Zhang J. Rising rates of labor induction: present concerns and future strategies. Obstet Gynecol 2002;100:164–7.
22. Grobman WA. Elective induction: when? ever? Clin Obstet Gynecol 2007;50:537–46.
23. Kramer MS, Rouleau J, Baskett TF, Joseph KS, for the Maternal Health Study Group of the Canadian Perinatal Surveillance System. Amniotic-fluid embolism and medical induction of labour: a retrospective, population-based cohort study. Lancet 2006;368:1444–8.
24. Knight M, Tuffnell D, Brocklehurst P, Spark P, Kurinczuk JJ, on behalf of the UK Obstetric Surveillance System. Incidence and risk factors for amniotic-fluid embolism. Obstet Gynecol 2010;115:910–7.
25. Zhang X, Kramer MS. Variations in mortality and morbidity by gestational age among infants born at term. J Pediatr 2009;154:358–62.
26. Yang S, Platt RW, Kramer MS. Variation in child cognitive ability by week of gestation among healthy term births. Am J Epidemiol 2010;171:399–406.
27. Zhang X, Joseph KS, Kramer MS. Decreased term and postterm birthweight in the United States: impact of labor induction. Am J Obstet Gynecol 2010;203:124.e1–124.e7.

















![[XLS] 1A... · Web viewJitendra M. Kambad N/C/201108/129 Rajkumar Sharma N/C/201108/130 Radhey Shyam Sharma E/C/201108/131 Rajat Sen N/C/201108/132 Jitendra mohura E/C/201108/133](https://static.fdocuments.net/doc/165x107/5aadeb7f7f8b9a3a038b828b/xls-1aweb-viewjitendra-m-kambad-nc201108129-rajkumar-sharma-nc201108130.jpg)