178612907 Penyakit Kel Adrenal Ppt
-
Upload
matthew-kevin-hendrianto -
Category
Documents
-
view
251 -
download
0
description
Transcript of 178612907 Penyakit Kel Adrenal Ppt
-
PENYAKIT PADA KELENJAR ADRENALCalvin Damanik
Bagian Penyakit Dalam FK UMIMedan
-
HistologyCortex90% of adult glandDerived from mesodermBegins during 5th week of developmentMesothelial cell migrationGlomerulosa, fasciculata, reticularisZonation occurs until about 18 months of age
-
HistologyMedullaDerived from neuroectodermNeural crest cell migrationBegins during 7th week of developmentPrimitive medulla by 20th weekContinues growth until cortex atrophy (18 months)
-
Cross section through the adrenal gland cortex and medulla saltsugarsex
-
Cortisol and Glucocorticoid Receptors
The vast majority of glucocorticoid activity in most mammals is from cortisol, also known as hydrocortisone. Cortisol binds to the glucocorticoid receptor in the cytoplasm and the hormone-receptor complex is then translocated into the nucleusOnly about 10% of circulating cortisol is free. The remaining majority circulates bound to plasma proteins, particularly corticosteroid-binding globulin (transcortin).
-
Hypothalamus-Pituitary-Adrenal axisKirk LF. Am Fam Physician 2000 CRH=corticothropin releasing hormone; ACTH=adrenocorticothropin hormone.
-
Aldosterone synthesisACTH also stimulates aldosterone synthesis. However the ACTH stimulation is more transient than the other stimuli and is diminished within several days. ACTH provides a tonic control of aldosterone synthesis. In the absence of ACTH, sodium depletion still activates renin-angiotensin system to stimulate aldosterone synthesis. Aldosterone levels fluctuate diurnallyhighest concentration being at 8 AM, lowest at 11 PM, in parallel to cortisol rhythms.
-
Regulation of aldosterone secretion: Activation of renin-angiotensin system in response to hypovolemia is predominant stimulus for aldosterone synthesis.
-
Components of renin-angiotensin-aldosterone system
-
Action of aldosterone on the renal tubule. Sodium reabsorption from tubular urine into the tubular cells is stimulated. At the same time, potassium secretion from the tubular cell into urine is increased. Na+/K+-ATPase, and Na+ channels work together to increase volume and pressure, and decrease K+.
-
Adrenocortical disorders
-
Cushings SyndromeExcess CortisolProtein catabolic stateLiberation of amino acids by muscleAA are transformed into glucose and glycogen and then transformed into fatLoss of calcium in urineWeakened muscles and elastic tissues
-
Causes of Cushings SyndromeACTH Dependent (80%)Cushings Disease (85%)Primary excretion of ACTH from pituitary95% have identifiable pituitary adenomaBasophilic or chromophobeBilateral adrenocortical hyperplasia70% of endogenous casesF>M (3:1)Ectopic source (15%)Produce ACTH or CRHSmall cell lung CA (most common), carcinoid tumors, medullary thyroid, pancreas, ovarian, pheochromocytoma, small-cell CA of prostate
-
Causes of Cushings SyndromeACTH IndependentExogenous steroid use (common)PO or topicalMost common cause (overall)
Adrenal adenomas (10%)Adrenal carcinoma (5%)Most common cause in children
-
Cause of Cushings SyndromePseudo-Cushings diseaseMimic clinical signs and symptomsNon-endocrine causesAlcoholismMajor depressionMorbid obesityAcute illness
-
Cushings SyndromeDiagnosis of Cushings syndromeHistory / Physical Examination ------> CLINICAL DIAGNOSIS (Symptoms and signs)Laboratory Examination (Screening Test & Defenitive Test) THE PRINCIPLE OF LABORATORY INTERPRETATION
-
Cushings SyndromeDiagnosis of Cushings syndromeLabs24 hour urinary cortisol2-3 consecutive daysVerify with creatinine valuesSpot AM/PM serum cortisol Circadian variationAM ACTH surge causes increased cortisolPM should see at least 50% drop in cortisol levelLow-dose dexamethasone suppression test
-
Cushings SyndromeDexmethasone suppression testSynthetic glucocorticoid (30x more potent as inhibitor)Low dose0.5mg po q6 hours x48 hoursMeasure cortisol, 17-hydroxycorticosteroidFall in all steroid levels in pseudo-Cushing and normalsDifferentiates presence/absence of Cushings syndromeAlternative dosing1mg po at midnight and measure 8am cortisolMuch less sensitive
-
Cushings SyndromeDiagnose cause of Cushings syndromeHistory (steroid use?)Serum ACTHElevated : Cushings disease, ectopic ACTHSuppressed: primary adrenal sourceCorrelate with cortisol levelsHigh-dose dexamethasone suppression test Metyrapone test
- Cushings SyndromeDexmethasone suppression testHigh Dose2mg po q6 hours x48 hoursMeasure cortisol and urinary free cortisolEctopic ACTH and adrenal tumors- no suppressionCushings disease- suppress to
-
Cushings SyndromeMetyrapone testInhibits 11-B-hydroxylaseBlocks conversion of 11-deoxycortisol to cortisolPlasma cortisol levels fall and ACTH increasesMarked increase in 17-hydroxycorticosteroid levels and 11-deoxycortisol levelsCushings Disease- normal or supernormal increase in levelsEctopic ACTH or adrenal sources- no responseRisks adrenal insufficiency
-
Cushings SyndromePetrosal vein samplingMeasure petrosal venous sinus ACTH level and correlate to plasma levelsInvasive with morbidityUsually not usedAdrenal venous samplingMeasure cortisol and aldosteroneNot used anymore
-
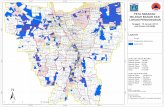
Cushings SyndromeRadiographic LocalizationCT of sella turcicaUnenhanced and gadolinium enhanced MRIRadionuclide imaging for somatostatin receptors>60% sensitive1st study if diagnosed with Cushings syndromeCT of chest/abdomen with 3mm cuts through adrenalAdrenal hyperplasiaThickening and elongation of adrenal rami bilaterallyMultinodularity of cortex bilaterally
-
Cushings SyndromeRadiographic LocalizationCT of adrenal glandsAdenomas- usually >2cm but 5cmNecrosis, calcifications, irregularity, invasionMRI of adrenal- usually not neededSignal intensity much higher than in spleen = carcinomaAdjacent organ and/or vascular involvement
-
Cushings syndrome suspect11 pm salivary cortisolDisrupted circadian rhythm24-hour UFC Filtered load of cortisolLow dose dexamethasoneSupression testAttenuated negative feedbackNormalEquivocalAbnormalCushings syndromeexcludedRepeat if high index of suspiciousDexamethasone testCushings syndromeestablished
-
Confirm CSACTHUndetectableNormal to increased AdrenalPituitary MRIUnilateralmassBilateral massesPituitary tumorNormal-equivocalIPSS withSearch ectopic
-
Cushings SyndromeTreatment: SurgicalCushings diseaseTransphenoidal hypophysectomy >90% cure rate 1st time, 50% salvage cure 2nd attemptExploration even if no obvious adenomaTransient post-op diabetes insipidus, adrenal insufficiency, CSF rhinorrhea, meningitisTansphenoidal irradiationHigh success rate in kids (80%)Low success in adults (20%)
-
Cushings SyndromeTreatment: SurgicalCushings diseaseBilateral adrenalectomyIf failed pituitary surgeryLife-long steroid replacementAdrenal lesions/carcinomaRemoval of primary lesionSurvival based on underlying diseaseEctopic ACTH lesionsRemove lesionSurvival based on primary diseaseMay need bilateral adrenalectomy to control symptoms if primary tumor unresectable
-
Cushings SyndromeTreatment: MedicalUsed as prep for surgery or poor operative candidateMetyrapone- inhibits conversion of deoxycortisol to cortisolAminoglutethimide-inhibits desmolaseCholesterol to pregnenoloneBlocks synthesis of all 3 corticosteroidsSide effects: N/V, anorexia, lethargyKetoconazole- an imidazole that blocks cholesterol synthesisMitotane (O-P-DDD)-inhibits conversion to pregnenoloneInhibits final step in cortisol synthesisDestroys adrenocortical cells (spares glomerulosa cells)
-
Addisons DiseasePrimary adrenal insufficiencyCausesInfectiousTB most common cause in 3rd world countriesHIV, histoplasmosis, blastomycosis, coccidiomycosisAutoimmune disorders anti-adrenal antibodies (most cause common)Medications ketoconazole, aminoglutethamide, etomidateAdrenal hemorrhageLymphoma, bilateral adrenal metastasis, Kaposis sarcomaInfiltrative amylodosis, sarcoidosis, adrenoleukodystrophy
-
Addisons DiseaseSecondary adrenal insufficiencyPituitary failure panhypopitutarism, Sheehans syndrome (post-partum pituitary injury)Tertiary adrenal insufficiencyAdrenal suppression due to glucocorticoid useChronic suppressionSudden cessation of replacement glucocorticoidsInadequate increase during stress, trauma, surgery
-
Addisons Disease
Response to cosyntropin test or rapid ACTH stimulation testCortisolAldosteronDiagnosisCommentsIncreasedDecreased
Decreased
IncreasedIncreasedDecreased
Increased
DecreasedNormalPrimary adrenal insufficiencySecondary adrenal insufficiencyIsolated aldosterone deficiencyEnd organ failure (Addisons disesase)Pituitary diseases, hypothalamic diseaseVery rare
-
Addisons CrisisAcute adrenal insufficiencySimilar causesAdrenal hemorrhageChronic steroid use and trauma/stress/surgeryHypotension, volume depletion, fever, nausea and vomiting, tachycardia, weakness, hypoglycemiaPremed prior to interventions
-
Addisons CrisisTreatment acut of adrenal crisisGlucocorticoid replacementAdminister hydrocortisone 100 mg every 6 hours for 24 hoursWhen the patient is stable, reduce the dosage to 50 mg every 6 hoursTaper to maintenance theraphy by day 4 or 5 and add mineralocorticoid theraphy as requiredMaintain or increase the dose to 200-400 mg/d if complications persist or occurGeneral and supportive measureCorrect volume depletion, dehydration, and hypoglycemia with IV saline and glucoseEvaluate and correct infection and other precipitating factors
-
PATOFISIOLOGI PENYAKIT ADDISONCortisol ACTH Abd.Pain Anorexia VomitingSkin HyperpigmentationGlukoneogenesisGlucose Uptake HYPOGLYCEMIARenal K Secretion Renal Na secretion HIPERKALEMIAHIPONATREMIAHYPOTENSIONHYPOVOLEMIA Diarrhea Fluid Intake + DEHIDRASIRENAL PERFUSION B.U.N General WeaknessDecreased Body Weight
-
Addisons CrisisMaintenance therapyGlucocorticoid and mineralocorticoidOral dose hydrocortisone : 10-20 mg in the morning and 5-10 mg later in day. Fludrocortisone : 0,05-0,2 mg/d orally in the morning. Response to theraphyGeneral clinical sign, good appetite and sense of well being. Signs of Cushings syndrome indicate overtreatment
-
Disorders of adrenal medullary function
-
PheochromocytomaAdrenal medullary tumor composed of chromaffin cells and capable of secreting biogenic amine and peptides, including epinephrine, norepinephrine, and dopamine.Such tumor arise from neural crest-derived cellsBecause of this common origin, neoplasma of the sympathetic ganglia , such as neuroblastoma, paragangliomas, and ganggliomneuromas, may produce similar amines and peptides.
-
COMT = Catecholamine Ortho Methyl Transferase)
-
Receptor catecholamine : Receptor (NE) Receptor (EPI)
-
PheochromocytomaSigns and symptoms : The classic triad of sudden severe headaches, diaphoresis, and palpitations Hipertensive in 95-95% of cases and is paroxismal in 25-50% of these.Orthostatic hypotension, tremor, pallor, flushing, anxiety and constipation Nonclassic manifestations :Hyperglycemia, severe diarrhea, hypercalcemiaArrhytmia, congestive cardiomyopathy, seizure, altered mental status, cerebral infarction/hemorrhage
-
PheochromocytomaDiagnosis : Demonstration of excessive amounts catecholamines in plasma or urine or degradation product in urineUrinary metanephrine, normetanephrine, vanilmandelic acid (VMA), and free catecholamine in 24-hour periodeDirect measurement plasma NE and EPI. Levels > 2000 pg/ml are abnormal and suggestive PheochromocytomaClonidine suppression testClonidine orally 0,3 mg; plasma catecholamine : before oral clonidine and again at 1,2 and 3 hr after oral clonidinePlasma catecholamine >500pg/mlGlucagon stimulation test
- PheochromocytomaTreatment : Surgical resection is only definitive therapyPreoperative preparation : prazosin 1mg 3 times/day, advanced to 5 mg3 times/day (7-28 days before surgery)Other agents labetalol or Ca channel blockerGoals of theraphy : BP
-
Glucocorticoid therapy for non endocrine disorders
-
PrinciplesAntiinflamatory and immunosuppressive therapy; rheumatoid arthritis, SLE, asthma, glomerulonephritisBecause of their side effect : minimum effective dose and shortest possible duration of therapyModes of administration : orally, parenterally, topically or inhalation
-
Synthetic glucocorticoid
Relative Potencies of Steroid HormonesCompound Glucocorticoid activityMineralocorticoid activityDurationHydrocortisone CortisonePrednisoneMethylprednisoneDexamethasoneFludrocortisone 10,745301010,70,70,50400ShortShortShortShortLongLong
-
Side effectsHPA axis suppressionSuppress CRH and ACTH secretion (negative feedback)Doses of prednisone >5mg/dIt is difficult to predict the development or degree of supression : Clinical feature Cushings syndromeGlucocorticoid equivalen to 10-20mg of prednisone/day for 3 weeks or moreCushings syndromeSteroid induced osteoporosisInhaled glucocorticoid : local effect (dysphonia and oral candiasis) and systemic effect, glaucoma, cataracts, osteoporosis, and growth retardationSteroid withdrawalGlucocorticoids must be tapered downwardPatients may develop fatigue, arthralgia, and desquamation of the skinEven after the dose to physiologic levels, HPA axis suppression persists for 9-10 months or more
-
Terima kasih
*












![Adrenal Imaging - University of Floridaxray.ufl.edu/files/2010/02/Adrenal-Imaging.pdfadrenal glands [3], and a metastasis might ... CT, adrenal imaging, adrenal lymphoma imaging, adrenal](https://static.fdocuments.net/doc/165x107/5b26814c7f8b9a8c0f8b4820/adrenal-imaging-university-of-glands-3-and-a-metastasis-might-ct-adrenal.jpg)