RJ GI Bleed
-
Upload
muhammad-armghan -
Category
Documents
-
view
231 -
download
0
Transcript of RJ GI Bleed
-
7/30/2019 RJ GI Bleed
1/47
Acute Gastrointestinal
Bleeding
Rajeev Jain, M.D.
-
7/30/2019 RJ GI Bleed
2/47
GI Bleeding
Clinical Presentation
Acute Upper GI Bleed Acute Lower GI Bleed
-
7/30/2019 RJ GI Bleed
3/47
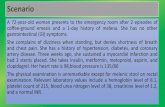
Case Presentation
CC: Melena
HPI: 54 yo man taking ibuprofen 200
mg po tid for the past 2 wks b/o acuteLBP after lifting presents with 2 day h/omelena
PMHx: neg All: NKDA SHx/FHx: neg Vitals: BP 105/75 P 90
PE: normal
-
7/30/2019 RJ GI Bleed
4/47
Clinical Presentation
Hematemesis: bloody vomitus (bright red or
coffee-grounds)
Melena: black, tarry, foul-smelling stool
Hematochezia: bright red or maroon blood
per rectum
Occult: positive guaiac test
Symptoms of anemia: angina, dyspnea, or
lightheadedness
-
7/30/2019 RJ GI Bleed
5/47
Patient Assessment
Hemodynamic status
Localization of bleeding source
CBC, PT, and T & C Risk factors
Prior h/o PUD or bleeding
Cirrhosis Coagulopathy
ASA or NSAIDs
-
7/30/2019 RJ GI Bleed
6/47
Resuscitation
2 large bore peripheral IVs
Normal saline or LR
Packed RBCs
Correct coagulopathy
-
7/30/2019 RJ GI Bleed
7/47
Location of Bleeding
Upper
Proximal to Ligament of Treitz
Melena (100-200 cc of blood)Azotemia
Nasogatric aspirate
Lower Distal to Ligament of Treitz
Hematochezia
-
7/30/2019 RJ GI Bleed
8/47
Acute UGIB
Demographics
10,000 - 20,000 deaths annually
Mortality stable at 10%
80% self-limited
Continued or recurrent bleeding -mortality 30-40%
-
7/30/2019 RJ GI Bleed
9/47
Cause of bleeding
Severity of initial bleed Age of the patient
Comorbid conditions
Onset of bleeding duringhospitalization
Acute UGIB
Prognostic Indicators
-
7/30/2019 RJ GI Bleed
10/47
NASOGASTRICASPIRATE
STOOLCOLOR
MORTALITY RATE(%)
Clear Red, brown, or black 10
Coffee Grounds Brown or black 10
Red 20
Red Blood Black 10
Brown 20
Red 30
Acute UGIB
Prognostic Indicators
Tedesco et al. ASGE Bleeding Survey. Gastro Endo. 1981.
-
7/30/2019 RJ GI Bleed
11/47
Acute UGIB
Differential Diagnosis
-
7/30/2019 RJ GI Bleed
12/47
Peptic ulcer disease Gastric ulcer
Duodenal ulcer
Mallory-Weiss tear
Portal hypertension Esophagogastric
varices Gastropathy
Esophagitis
Dieulafoys lesion
Vascular anomalies
Hemobilia Hemorrhagic
gastropathy
Aortoenteric fistula
Neoplasms Gastric cancer
Kaposis sarcoma
Acute UGIB
Differential Diagnosis
-
7/30/2019 RJ GI Bleed
13/47
DIAGNOSES % OF TOTAL
Duodenal ulcer 24
Gastric erosions 23
Gastric ulcer 21
Varices 10
Mallory-Weiss tear 7
Esophagitis 6
Acute UGIB
Final Diagnoses of the Cause in 2225 Patients
Tedesco et al. ASGE Bleeding Survey. Gastro Endo. 1981.
-
7/30/2019 RJ GI Bleed
14/47
DIAGNOSES % OF TOTAL
Peptic ulcer 55
Varices 14
Angioma 6
Mallory-Weiss tear 5
Erosions 4Tumor 4
Acute UGIB
Causes in CURE Hemostasis Studies (n=948)
Savides et al. Endos copy 1996;28:244-8.
-
7/30/2019 RJ GI Bleed
15/47
Acute UGIB
CORI Database
University, VA, & privatepractices
20 months (12/99-7/01)
7822 EGDs for UGIB
Boo npon gmaneeS. et al. Gastrointest Endos c 2004;59:788-94.
-
7/30/2019 RJ GI Bleed
16/47
Endoscopic Appearance
of Ulcers
-
7/30/2019 RJ GI Bleed
17/47
Prognostic Features at Endoscopy
in Acute Ulcer Bleeding
Lain e and Peterson New Eng J Med 1994;331:717-27.
-
7/30/2019 RJ GI Bleed
18/47
Thermal
Bipolar probe
Monopolar probe Argon plasma
coagulator
Heater probe
Mechanical Hemoclips
Band ligation
Injection
Epinephrine
Alcohol Ethanolamine
Polidocal
Endoscopic Therapy of PUD
-
7/30/2019 RJ GI Bleed
19/47
Endoscopic Therapy of PUD
Lain e and Peterson New Eng J Med 1994;331:717-27.
-
7/30/2019 RJ GI Bleed
20/47
Adjuvant Medical Therapy
of PUD Acid suppression (intragastric pH > 4)
Histamine 2 Receptor Antagonists
(H2RAs) Ranitidine (Zantac)
Famotidine (Pepcid)
Proton Pump Inhibitors (PPIs)
Pantoprazole (Protonix) Lansoprazole (Prevacid)
Esomeprazole (Nexium)
-
7/30/2019 RJ GI Bleed
21/47
Bleeding PUD: IV H2RAs
Meta-Analysis Duodenal ulcer: no
benefit
Gastric ulcer: mildbenefit Mortality
ARR 3%; NNT 33
Surgery ARR 7%; NNT 14
Rebleeding ARR 7%; NNT 14
Caveats Tolerance develops
within 24 hrs
More potent acidsuppressionavailable
Levi ne JE et al. Alim ent Pharm acol Ther 2002;16:1137-42.
-
7/30/2019 RJ GI Bleed
22/47
472 patients required no
endoscopic treatment
27 patients not included:
comorbid or no consent
120 patients received IV
omeprazole 80 mg bolus
then 8 mg/hr for 72 hours120 patients received placebo
267 received endoscopic treatment
739 patients admitted with GI bleeding
Lau et al. New Eng J Med 2000;343:310-316.
Adjuvant Medical Therapy of
PUD
Adj t M di l
-
7/30/2019 RJ GI Bleed
23/47
Adjuvant Medical
Therapy of PUD
Lau et al. New Eng J Med 2000;343:310-316.
-
7/30/2019 RJ GI Bleed
24/47
Bleeding PUD: PO/IV PPIs
Meta-Analysis Reduction in:
Rebleeding NNT* 4-17
Surgery NNT* 6-25 No change in mortality
PPIs add to endoscopic
therapy but do notsupplant endoscopictherapy
* Estimates from pooled ORsLeon tiadis , GI et al. BMJ 2005;330:568-75.
-
7/30/2019 RJ GI Bleed
25/47
Mallory-Weiss Tear
-
7/30/2019 RJ GI Bleed
26/47
Esophageal Varices
-
7/30/2019 RJ GI Bleed
27/47
Variceal Band Ligation
-
7/30/2019 RJ GI Bleed
28/47
Variceal Band Ligation
-
7/30/2019 RJ GI Bleed
29/47
Vasopressin/Glypressin
Nonselective vasoconstrictor
50% efficacy in controlling bleeding
25% vasospastic side effects
Octreotide
Cyclic octapeptide analog ofsomatostatin
Longer acting than somatostatin
Equivalent to sclerotherapy and
improves endoscopic results
MEDICAL THERAPY
Acute Variceal Bleeding
-
7/30/2019 RJ GI Bleed
30/47
TIPS
IVC
Portal Vein
Splenic Vein
Coronary Vein
-
7/30/2019 RJ GI Bleed
31/47
Aortoduodenal Fistula
Aorta
Duodenum
Graft
Fistula
-
7/30/2019 RJ GI Bleed
32/47
Acute Bleeding
Changes Before and After 2 Liter Bleed
0
1
2
3
4
5
6
Before During 24-72 Hrs
VOLUME(L)
Plasma RBC
27%45%45%
-
7/30/2019 RJ GI Bleed
33/47
Acute UGIB
Surgery
Recurrent bleeding despite
endoscopic therapy
> 6-8 units pRBCs
-
7/30/2019 RJ GI Bleed
34/47
Case Presentation
CC: Hematochezia
HPI: 74 yo woman presents with 6 hour
history of painless maroon blood per rectum PMHx: CAD, Chol, AFib, CABG, L-CEA
Meds: ASA, coumadin, digoxin, lovastatin
Vitals: BP 105/75 P 90 PE: irreg rhythm, maroon blood on DRE
-
7/30/2019 RJ GI Bleed
35/47
Acute LGIB
Differential Diagnosis
-
7/30/2019 RJ GI Bleed
36/47
Diverticulosis
Colitis
IBD (UC>>CD)
Ischemia
Infection
Vascular anomalies
Neoplasia
Anorectal
Hemorrhoids
Fissure
Dieulafoys lesion
Varices
Small bowel
Rectal
Aortoenteric fistula
Kaposis sarcoma
UPPER GI BLEED
Acute LGIB
Differential Diagnosis
-
7/30/2019 RJ GI Bleed
37/47
DIAGNOSES % OF TOTAL
Diverticulosis 40
Vascular anomalies 30Colitis 21
Neoplasia 14
Anorectal 10Upper GI sites 10
Acute LGIB
Diagnoses in pts with hemodynamic compromise.
Zuccaro. ASGE Clin ical Upd ate. 1999.
-
7/30/2019 RJ GI Bleed
38/47
Diverticulosis
-
7/30/2019 RJ GI Bleed
39/47
Diverticular Bleeding
-
7/30/2019 RJ GI Bleed
40/47
Urgent Colonoscopy for the Diagnosis
and Treatment of Severe Diverticular
Hemorrhage
121 pts with severebleeding (>4 hrsafter hospitalization)
1st 73 pts: nocolonoscopic tx
Last 48 pts eligiblefor colonoscopic tx
Colonoscopy w/in 6-12 hrs
-
7/30/2019 RJ GI Bleed
41/47
Urgent Colonoscopy for the Diagnosis and
Treatment of Severe Diverticular
Hemorrhage
Jens en DM, et al. New Eng J Med 2000:342:78-82.
-
7/30/2019 RJ GI Bleed
42/47
Hemorrhoids
-
7/30/2019 RJ GI Bleed
43/47
Bleeding AVM
-
7/30/2019 RJ GI Bleed
44/47
Radiation Proctitis
-
7/30/2019 RJ GI Bleed
45/47
Incidence 0.3 - 3.0 %
Etiology Incomplete obliteration of
the vitelline duct.
Pathology 50% ileal, 50% gastric,
pancreatic, colonic mucosa
Complications Painless bleeding (children, currant jelly)
Intussusception
Acute LGIB
Meckels Diverticulum
-
7/30/2019 RJ GI Bleed
46/47
StudyYield
%Comments
Colonoscopy 69-80 Therapeutic
Arteriography 40-781 ml/min,
risks
Tagged RBC Scan 20-72 Localization
Acute LGIB
Evaluation
Zuccaro. ASGE Clinic al Upd ate. 1999.
-
7/30/2019 RJ GI Bleed
47/47
Resuscitation
UGI source
Most bleeding ceases Colonscopy - early
No role for barium studies
5% Mortality
Acute LGIB
Key Points