Wound management of venous ulcer
-
Upload
scu-hospital -
Category
Health & Medicine
-
view
38 -
download
3
Transcript of Wound management of venous ulcer

Phase-specific wound management of venous leg ulcer
Wound management
medicaledition

Phase-specific wound management of venous leg ulcer

Published byPAUL HARTMANN AGD-89522 Heidenheimhttp://www.hartmann.info
Concept, designediting and production:CMC Medical InformationD-89522 Heidenheim
Scientific supervision:Dr. med. Andreas Gericke,phlebologist and angiologist,Traunstein
© PAUL HARTMANN AGMay 2006ISBN 3-929870-47-9Translated from the Germanedition (ISBN 3-929870-42-8)
Printed on chlorine-freebleached paper
Preface 5
Causes of venous leg ulcer 6– Anatomy of the leg veins 7– Physiology and pathophysiology of venous return 9– Pathophysiology of CVI 12
Clinical presentation and diagnosis of venous leg ulcer 16
Management of venous leg ulcer 24– Compression bandaging as basic therapy 25 – Invasive therapeutic procedures 26– Surgical treatment of ulcers 27 – Adjuvant medicinal therapy 28– Identification of wound healing disorders 28 – Pain management 30
Phase-specific wound management of venous leg ulcer 32– Wound management in the cleansing phase 37– Wound management in the granulation phase 40– Wound management in the epithelisation phase 42– TenderWet – wound pad with super absorber 44– Sorbalgon – calcium alginate dressings with excellent conformability 49– PermaFoam – hydroactive foam dressing 50– Hydrocoll – absorbent hydrocolloid dressing 53– Hydrosorb – transparent hydrogel dressing 55– Atrauman Ag – silver-containing ointment dressing 56
Compression bandaging as basic therapy 62– The bandaging materials 65– General principles of bandaging technique 70– Bandages for compression therapy 78
Glossary and index of key terms 84References and list of illustrations 87
Table of contents

Causes [4.5]
Preface
Venous alterations and venous diseases are among thecommonest impairments of health and well-being, and itis estimated that about two million citizens of the FederalRepublic of Germany are affected by a lower leg ulcer ofvenous origin. This statistic illustrates the social andsocio-economic relevance of this medical condition, butdoes not adequately describe the loss in quality of lifesuffered by persons with a chronic ulcerative disease.
Many ulcer patients have a decades-long history of suf-fering because of inadequate and failed attempts at ther-apy and ultimately often resign themselves fatalistically tothe apparently unavoidable. However, modern diagnosticprocedures involving little stress for patients, combinedwith appropriate therapeutic concepts, now mean thatvenous leg ulcers can be effectively brought under con-trol. Undoubtedly, this requires an adequate knowledgeof the complex medical problems involved and the physi-cian's ability to motivate patients to take upon them-selves a sometimes protracted program of therapy. Thevery fact that rapid ulcer healing occurs only in very fewcases causes problems. Both physicians and patients maylose patience, and the unscientific use of multiple med-ications is not infrequently substituted in place of consis-tently practised compression therapy.
This HARTMANN medical edition presents therapeuticconcepts involving conservative management of theseconditions in the light of pathophysiological knowledge.These approaches are based on the use of compressionbandaging as basic therapy and illustrate the possibilitiesoffered by phase-specific wound management withhydroactive wound dressings, since moist wound treat-ment has proved especially effective in the treatment ofchronic ulcerations.

Causes [6.7]
Anatomy of the leg veinsThe leg vein system is divided according to anatomicalcriteria into the superficial or suprafascial and the deepor subfascial venous system. The two regions are connect-ed by the communicating veins to form a single function-al unit.
The suprafascial veins are located in the cutis and sub-cutis, i.e. outside the fascia, a binding layer of connectivetissue surrounding the muscles. They are connected by anetwork of numerous lateral branches and take the formof extensive venous plexuses which drain the superficialblood into the deep veins, but because of their high stor-age capacity also have functions in regulating blood vol-ume. The superficial veins collect in the two main superfi-cial veins, the great (vena saphena magna) and small(vena saphena parva) saphenous veins. The small saphe-nous vein empties into the popliteal vein (vena poplitea)in the hollow of the knee, while the large saphenous veinpasses into the deep femoral vein (vena femoralis) belowthe inguinal ligament.
The subfascial veins run as larger vessels inter- and intra-muscularly within the fascia and are paired with the cor-responding arteries. They serve as blood collectors and
Venous leg ulcer is an expression of an extremelysevere metabolic derangement in the cutis andsubcutis resulting from chronic venous insuffi-ciency. Understanding the underlying pathome-chanism requires a knowledge of the anatomy ofthe leg vein system and the athophysiologicalprocesses involved.
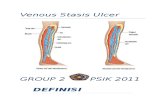
Causes of venous leg ulcer
Schematic diagram of the leg vein system (suprafascial veins: dark /subfascial veins: light)1) subfascial thigh vein (femoral vein)2) Dodd’s veins3) suprafascial superficial vein (great saphenous vein)4) subfascial vein of hollow of knee (popliteal vein)5) posterior subfascial shinbone vein (posterior tibial vein)6) Boyd’s veins7) anterior subfascial shinbone vein (anterior tibial vein)8) Cockett’s veins9) Dorsal venous arch of foot
1
2
3
4
5
6
7
8
9

Causes [8.9]
Schematic diagram of the calfmuscle pump during contraction(1) and relaxation (Relaxation/2) of the muscles: Circles = cross-sections through relaxed and con-tracted muscles with intramuscu-lar deep veins and transfascialveins on different levels, fascia =green
Schematic diagram1) vein2) open venous valve3) closed venous valve
Cross-section through an artery(left) and a vein (right) in a mus-cle tissue. The artery walls arethick and consist of highly con-tractile elastic fibres allowingthem to withstand suddenincreases in blood pressure. Theveins have a less contractilestructure, but a larger volumesuited to their drainage andtransport functions.
port the blood back to the heart and are thus also knownas deep or transport veins. The lower leg veins, the ante-rior and posterior tibial veins, unite to form the poplitealvein, which continues on towards the heart as thefemoral vein.
The interconnections within a venous system, e.g. only inthe suprafascial system, are provided by the communicat-ing veins (venae communicantes). The interconnectionsbetween the supra- and subfascial venous system, on theother hand, are created by numerous perforating veins(venae perforantes) which “perforate” the fascia for thispurpose. Main groups are Cockett’s veins above theankle, Boyd’s veins below the knee joint and Dodd’sveins in the thigh.
Almost all veins have more or less numerous venousvalves that serve as volume regulators. They make surethat the blood flows only in one direction, namelytowards the heart or from the superficial to the deeperlevels.
Physiology and pathophysiology of venous returnThe return transport of the blood to the right ventricle ofthe heart requires the presence of various physiologicaldriving forces and assistive mechanisms to overcome thehigh total hydrostatic pressure which acts on the leg veinsystem when the body is upright. The principle of com-municating tubes with postcapillary residual pressure,variations in respiratory pressure in the thoracic andabdominal space and the elastic aspiration of the heartprovides the necessary mechanisms. The most effectivefactor, however, is the functional unit of the calf musclepump.
During movement of the legs, the deep veins are com-pressed with every muscular contraction. This forces theblood out towards the heart and the venous valves pre-vent the blood from pooling back into the veins. Whenthe muscles relax, the deep veins expand to create a neg-ative pressure which results in blood being aspiratedthrough the perforating veins from the more distallylocated venous segments and the suprafascial venousplexuses. The alternating compression-suction effect ofthe muscle pump is complemented by similar mecha-nisms in the joints and the firm resistance surface provid-ed by the fascia which ensures that the pressure thatbuilds up during the contraction also acts in an inwarddirection.
The interplay of these mechanisms results in the bloodbeing raised towards the heart through several consecu-tive and coordinated levels on a kind of “paternoster”principle from the foot, through the ankle, through thecalf, the hollow of the knee, the thigh and the groin,while simultaneously being withdrawn through the perfo-rating veins from the suprafascial plexus. The bloodtherefore flows from the more superficial to the deeperlevels and from distal to proximal; the venous pressurefalls.
1 2
2
1
3

Causes [10.11]
The severity, localization and duration of the outflow dis-order and the degree and duration of stress on the legvein system determine the variable clinical presentationswhich appear gradually and with inexorably increasingseverity. This complex of clinical signs is subsumed underthe general term chronic venous insufficiency (CVI) and isusually assigned to three grades of severity according tothe Widmer classification.
Grade I chronic venous insufficiency is characterized by acollection of dilated venules (corona phlebectatica) andedema around the ankles and above the arch of the foot,and by ankle edema.
Grade II manifests as hyperpigmentation of the skin,lower leg edema and dermatoliposclerosis. The skin isthen firmly bonded with the lower leg fascia, cannot beraised in folds and has a more pronounced sheen thanusual. An extreme form of dermatoliposclerosis is atro-phie blanche (also known as capillaritis alba or white
It should be emphasized that, despite available scientificevidence, the above descriptions are in many respects stillonly a theoretical model and that the highly complexphysiological functional processes and relationships haveto date only been partially elucidated. It is certain, how-ever, that the complex functional unit - known for thesake of simplicity as the calf-muscle pump - is at the cen-tre of a programmed sequence of events that takes placeduring movement.
If the return of blood to the heart is disturbed (venousinsufficiency), less blood is withdrawn from the upstreamvenous segments and the fall in venous pressure is lesspronounced (venous hypertension). The overload on theveins acts as a backward decompensation extending asfar as the capillaries of the terminal vessels. The low pres-sure values necessary for a properly regulated exchangeof substances then cannot develop, and venous flowslows down or even ceases completely. The metabolicprocesses, especially in the subcutis or cutis, areimpaired. Eventually, the lymphatic system is also affect-ed, and is only able to compensate the increase in inter-stitial fluid in the initial phases of an outflow disorder byincreasing the flow of lymph
The earliest recognisable consequence of this disorderedcondition is edema, which leads to further increases inpressure and accumulations of fluid and thereby furtherexacerbates the already compromised metabolic situation.Further consequences are fibrotic, degenerative andinflammatory processes associated with trophic skin alter-ations. Finally, obliterative inflammatory processes in thevenules and arterioles lead, initially in regions withunfavourable venous hemodynamics, to the developmentof venous leg ulceration as the now visible sign ofdecompensated venous hypertension.
1) Pronounced dermatoliposcle-rosis in Grade II CVI, due toincreasing fibrosis of the cutis and subcutis2) Atrophie blanche with the white atrophic skin changes3) Florid venous leg ulcer in Grade III4) Ulceration covering the gaiterarea of the leg1 2
3 4

Causes [12.13]
Diagram of blood return:1) In the physiological situation. 2) In primary varicosis: valve clo-sure is no longer possible due tothe vascular dilatation, the direc-tion of blood flow reverses.3) In secondary varicosis: scarringand loss of elasticity of the super-ficial veins after deep leg veinthrombosis leads to valve incom-petence, the blood flows throughthe perforating veins back intothe suprafascial system.
Varicose veins are not merely a“cosmetic problem”. Vasculardilatation and valvular insuffi-ciency can progress through theperforating veins to affect thedeep veins, resulting in chronicvenous insufficiency and ulcera-tion.
atrophy), which occurs almost exclusively as a conse-quence of CVI. Characteristic signs of this skin alterationare white, atrophic focal lesions ranging in size from acoin to the palm of the hand, and are found mainly in theankle region or around scars of healed ulcerations.
Grade III manifests as a florid or healed venous leg ulcer.Its site of predilection is the perimalleolar region(Bisgaard region), but it can also occur elsewhere on thelower leg. Ulcerations can also spread to cover the entirelower leg in a circular pattern resembling a gaiter.
Pathophysiology of CVIChronic venous insufficiency can either be the result ofprimary varicosis or a consequence of a postthromboticsyndrome; the anatomical localization of the flow obsta-cle is the factor that determines the clinical prognosis.
Suprafascial venous insufficiency / primary varicosisThe most important disease of the superficial leg vein sys-tem is primary varicosis or varicose veins. Varicose veinsare abnormally and irregularly swollen veins with a typi-cally tortuous course visible below the skin. They can becaused by valve agenesia (congenital absence of venousvalves), but more often it is hereditary or age-related lossof elasticity of the venous walls that leads to vasculardilatation and valve incompetence. This congenital pre-
disposition is promoted by factors such as hormonal influ-ences during pregnancy, lack of exercise or inflammatoryprocesses. If lumen enlargement and valvular insufficien-cy occur in the large superficial leg veins (great and smallsaphenous vein), the disease is known as saphenous vari-cosity. Lateral branch varicosis is present when the lateralbranches of the saphenous vein are affected by thesechanges, while varicose extensions of the communicatingveins are known as reticular varicosis.
Since only about 10 % of the venous blood is returned tothe heart through the superficial veins, a functional disor-der of individual venous segments can usually be com-pensated without much difficulty by blood being divertedto other venous plexuses or by the intact deep communi-cating veins assuming the transport functions. The clinicalsituation undergoes a serious change, however, whenlumen enlargement and valve incompetence also begin toaffect the perforating and subfascial veins. The directionof venous flow is then reversed, leading to disorders ofphysiological return and retrograde flow conditions.
1 2 3

Causes [14.15]
Poststhrombotic vascular andflow situation: the deep vein isscarred and recanalised after thethrombosis (1). “Blow out”through dilated communicatingveins (2), resulting in secondaryvarices (3).
The drop in pressure caused by the calf-muscle pump dur-ing walking is reduced or completely absent (venoushypertension), and the functional capacity of the venousvalves is progressively impaired. The effects manifest aschronic venous insufficiency, characterized by the patho-physiological disorders of microcirculation in the cutisand subcutis already described, which can culminate inthe formation of a venous leg ulcer.
When the valvular apparatus is still sufficient in primaryvaricosis, however, ulcerations can also develop as aresult of injuries, blunt traumas or varicose ruptures. Theirprognosis is correspondingly more favourable.
Subfascial venous insufficiency /postthrombotic syndromeInsufficiency of subfascial veins can also occur in a pri-mary form consecutive to valve agenesia or congenitalunderdevelopment of the venous valves, but in mostcases appear as the secondary form after deep leg veinthrombosis (phlebothrombosis).
Thrombosis of the deep veins not treated immediately bythrombolysis or thrombectomy usually heals leaving adefect. The thrombus becomes organised like connectivetissue, and this collagenous remodelling results in scarformation. Incomplete obstruction of the venous volumemay often be followed by recanalisation, but because ofthe scar formation the vein loses elasticity and can nolonger adapt to the variable blood volumes. The venousvalves also can no longer fully perform their closure func-tion and often create additional flow obstacles which pro-mote turbulence of the blood. The alterations in thelumen due to scarring in the deep veins create new deadspace for the calf-muscle pump, with the result that suffi-
cient blood can no longer be withdrawn and the intravas-cular pressure increases. The continuous build-up of backpressure in turn results in metabolic derangements in theperipheral skin areas, and in the worst case to ulceration.Moreover, the increased pressure stress not infrequentlyleads to leakage of the valves of the perforating veins,causing blood to flow back from the subfascial into thesuprafascial system.
The consequences are secondary varices and edematousinfiltration of the cutis and subcutis with the known sec-ondary complications. Postthrombotic syndrome (PTS) isthe commonest cause of venous leg ulcer (postthromboticvenous leg ulcer).
1
2
3

Clinical presentation and diagnosis [16.17]
Medical historyThe medical history concentrates on familial or personalrisk factors, vascular risks (varicose veins, symptoms ofCVI, deep vein thrombosis, hypertension, arteriopathies,claudication), lifestyle habits (occupation, sedentarylifestyle, little exercise etc.), medication use, alcohol andtobacco consumption, type of onset and development ofthe ulcer (e.g. after injury or blunt trauma), but also pre-vious local or systemic treatments.
Localization and form of the ulcersVenous ulcers preferentially develop at the ankle(Bisgaard region) and allow a “prima vista” diagnosis. Inabout 20 % of cases, however, they also develop at othersites on the lower leg, a situation which always requiresdifferential diagnostic clarification. The shape and size ofthe venous ulcer are variable, and the ulceration canspread to cover the entire gaiter area of the lower leg.
Clinical presentation and diagnosis of venous leg ulcer
1) Typical localization of venousulcers, with postthrombotic ulceras an example2) Ulcerations resembling gaitersenclosing the lower leg 3) and 4) mixed venous leg ulcerdue to CVI and pAOD
1 2
3 4
About 90 % of leg ulcers develop as a result of venoushypertension secondary to severe chronic venous insuffi-ciency. About 6 % of venous leg ulcers are attributableto reduced peripheral arterial blood supply and about 4 % to specific skin diseases. An exact diagnosis istherefore essential. This requires taking a detailed med-ical history, a clinical and instrumental examination anddifferential diagnostic procedures to rule out non-venousetiopathological factors.

Clinical presentation and diagnosis [18.19]
Doppler ultrasonography as apainless, safe examination of theleg veins
1) Stasis dermatitis with “blow-outs“2) Contact eczema
Nature of the wound floorThe wound floor of purely venous ulcers has at the mosta coating of yellowish or whitish, fibrinous necroticslough, and the ulcer usually produces hardly any exu-date. Black necrotic tissue at the wound margins alsoindicates a disorder of arterial perfusion. This is classifiedas a mixed ulcer. A bloody-serous, purulent wound floorindicates the presence of infection.
State of peri-ulcer zoneDue to the venous and lymphatic stasis and the resultingskin alterations, patients with chronic venous insufficien-cy are predestined to develop stasis dermatitis and con-tact eczema. Stasis dermatitis, also known as varicoseeczema, develops on peri-ulcer skin and is not infrequent-ly encouraged by the use of greasy ointments. Contacteczema also develops as a reaction to sensitizing sub-stances, such as topical antibiotics.
Edema formationFor more pronounced edema, comparative girth measure-ments are indispensable to assess the effect of compres-sion therapy by monitoring the reduction in edema.
Symptomatology/painUlcerations associated with primary varicosis usuallycause less severe symptoms – and in these cases theedema is also less pronounced – than those developingas a result of CVI of postthrombotic origin. Especially thesmall ulcers developing in the region of a capillaritis albacan cause the patient considerable difficulties and pain.In general, however, ulcers with arterial involvement aremuch more painful than purely venous ulcers.
Orthopedic abnormalitiesIt is important – also in regard to the effectiveness ofcompression bandages – to check the mobility of thelarge joints, taking particular care to detect incipient stiff-ening of the ankle joints. Postthrombotic patients oftenexhibit talipes and rarely ankyloses of the upper ankle asa sign of ulcer disease already existing for several years,with cicatricial strictures resulting from frequent relapses.
Recording of arterial statusIt is also essential to establish the arterial blood flow sit-uation. Useful evidence is provided by the temperature ofthe extremity (cold when arterial perfusion is reduced)and palpation of the foot pulses. In patients with long-standing diabetes, however, palpation of the foot pulsescannot be used as a clinical criterion because consider-able microcirculatory disorders may already be presentdue to pronounced media sclerosis despite well-filledpulses, and the ulceration is therefore of mixed arterialand venous origin. Furthermore, diabetics may lack thetypical clinical signs of intermittent claudication becauseof diabetic neuropathy. Peripheral pressure measurementby Doppler ultrasound is also of little value in elucidatingthe arterial situation because excessively high pressurevalues are measured as a result of the media sclerosis.The only technique which can provide further diagnosticinformation in this situation is acral oscillography or pos-sibly colour duplex sonography.
Recording of venous statusIt is supremely important for therapeutic purposes toexactly localize the disorder of venous return within thevenous system. The diagnosis is based on clinical andinstrumental examinations. Doppler ultrasound especiallyis now a reliable routine diagnostic procedure for precise-ly determining the presence and extent of extrafascial

Clinical presentation and diagnosis [20.21]
1) Before an ulcer of arterial ori-gin develops, trophically alterednails, mycoses, erythema, mar-bling and loss of hair may benoticed.2) Arterial leg ulcer on the exten-sor side of the lower leg withexposed anterior tibial tendon.
Visualisation of the leg vein byphlebography
valve incompetence. Also very informative is colourduplex sonography which is recommended as a supple-mentary diagnostic procedure in suitable cases – espe-cially for the deep communicating veins.
Further, similarly non-invasive methods are venous occlu-sion plethysmography (VOP), used to measure venousoutflow and venous capacity, as well as light reflectionrheography (LRR), although the evidential value of thistechnique is greatly restricted by insufficient repro-ducibility.
Phlebography as an invasive imaging procedure involvingthe use of contrast media is now used with greater cau-tion, but is still indispensable in many cases to establishindications for surgery, especially in relapses followingvenous surgical interventions.
Recording of general conditionThe physician should always search for signs of latent orovert right ventricular failure. Clinical laboratory testsshould include postprandial blood glucose, hemoglobin,red blood count, erythrocyte sedimentation rate, C-reac-tive protein and, when appropriate, hematocrit.
Differential diagnostic clarificationAlthough, as already mentioned, about 90 % of leg ulcersare the consequence of chronic venous insufficiency, legulcers of non-venous origin must always be included indifferential-diagnostic deliberations. Possible causes mayinclude:
Obstruction of larger and smaller arteries by peripheralarterial occlusive disease (pAOD), which can lead to arte-rial leg ulcer or necrotising vasculitis. The localization ofarterial ulcers corresponds to the sites on the lower leg
which tend to be most exposed to mechanical injuries,e.g. the anterior edge of tibia. Typical signs are black skinnecroses, and subfascial structures such as tendons, mus-cles and bones may be visible. In vasculitis, pea- to coin-sized, occasionally extensive multiple ulcers are usuallypresent. Depending on the localization of the vasculiticvascular lesions, these ulcers are superficial (superficialvasculitis) or have a deeper, punched-out appearance(deep vasculitis).
Macro-and microangiopathies and peripheral neuro-pathies associated with diabetes mellitus may result inangiopathic (diabetic gangrene) or neuropathic ulcers(perforating disease). Because of their commonest local-ization – acral and on the sides of the feet when ofangiopathic etiology and on the sole of the foot underthe metacarpophalangeal joints when of neuropathic etiology – identifying these ulcers is unlikely to presentany problems.
Hematological diseases such as sickle-cell anemia, sphe-rocytic anemia, thalassemia or essential thrombocytosis,may be associated with an ulcer as a concomitant symp-tom. Infections, such as ecthymas caused by staphylococ-ci or erysipelas caused by streptococci are also possible

Clinical presentation and diagnosis [22.23]
causes. Ecthymas have the appearance of punched-out,sharply defined ulcers and tend to occur mainly on thelower leg. Erysipelas presents as an extensive erythemawhich, if left untreated, becomes necrotic and can lead toulcerative degeneration of relatively large areas of skin.
Traumatic events such as physical, chemical or thermaldamage are further potential causes of leg ulcers,although artefacts (self-damage) should also be includedin the physician's deliberations.
Neoplastic diseases such as basaliomas, spindle-cell carci-nomas, soft-tissue sarcomas or malignant lymphomas andmelanomas, with relevant localization, lead to neoplasticleg ulcer. In view of the anticipated increase in HIV-posi-tive patients, a growing incidence of Kaposi sarcomas isto be expected. The possibility of a malignant etiologyshould particularly be borne in mind when dealing withtherapy refractory “problem ulcers”. The diagnosis isestablished histologically, and the importance of takingbiopsy samples at an early stage is to be emphasized.Biopsy samples should be collected from several sites – atthe edges and in the middle of the ulcer.
Examples of leg ulcers of non-venous origin1) Ulcers due to very severe arte-rial blood flow insufficiency, fre-quent localization: lateral edge offoot and heel2) Ulcer due to diabetic macroan-giopathy on the lower leg3) Neuropathic ulcer associatedwith diabetes mellitus “perforat-ing disease”4) Venous leg ulcer caused bychemotherapy for primary throm-bocythemia5) Hemorrhagic-bullous erysipelas6) Necrotising erysipelas7) Leg ulcer caused by abasalioma8) Venous leg ulcer resulting fromspindle cell carcinoma
1 3
3 4
5 6
7 8

Therapy [24.25]
Therapeutic activities are concentrated on the followingaspects: The venous hypertension underlying the ulcermust be remediated as effectively as possible in order toimprove the nutritive situation in the damaged area ofskin. An ulcer can only heal when the edema has sub-sided and venous outflow in the leg has been restored toa compensated state (Hach). These therapeutic objectivescan essentially be achieved by means of compressiontreatment and, when appropriate, using invasive thera-peutic methods (surgery and/or sclerotherapy).
Local ulcer therapy is based on appropriate wound man-agement adapted to match the different phases of heal-ing. Wound management should also eliminate as far aspossible all the factors which generally compromisewound healing, such as infections, concomitant diseasesand side effects of other treatments or negative psy-chosocial factors.
Compression bandaging as basic therapy“There is no phlebology without compression therapy”.This dogma applies unreservedly for the management ofvenous ulcer, because the effect of the compressionbandage intervenes causally in the disease process. It sur-rounds the leg with pressure firm enough to compress thedilatated veins. This restores and/or a certain degree sub-stitutes the valvular function, reduces venous reflux fromsubfascial to suprafascial and increase the flow velocityof the venous blood. At the same time, compression caus-es an increase in the tissue pressure and therebyenhances absorption in the terminal vessels and thelymph vessels. The microcirculation is locally improved,which decisively improves the healing tendency of venousleg ulcer.
Management of venous leg ulcer
Venous leg ulcer is a chronic wound with a poor orabsent healing tendency. Especially the often extensiveulcers associated with severe chronic venous insufficiencyand pronounced sclerosis of the cutis and subcutis canbecome a therapeutic crux medicorum requiring protract-ed treatment and characterized by frequent relapses.Nevertheless, today’s knowledge of the pathophysiologi-cal mechanisms implicated in causing venous leg ulcersgenerally allows the application of effective therapeuticconcepts.

Therapy [26.27]
Healed venous leg ulcer afterparatibial fasciotomy
Vein stripping, “pulling-out” aninsufficient vein segment
The compression bandage also acts as a firm resistancesurface which helps to restore at least partially the func-tion of the calf-muscle pump and improve its effective-ness. When compression therapy is carried out in theproper manner, relief of pain and initial signs of healingare observed within a short time, which is seen as anencouraging sign by patients and can motivate them topersist with the often protracted course of treatment. The mode of action of compression therapy, importantinformation on bandaging materials and bandaging tech-niques for compression bandages as well as contraindica-tions are described in detail from page 62 onwards.
Invasive therapeutic procedures for compensation of chronic venous insufficiencyIn modern phlebology, sclerotherapy and surgery aremutually complementary therapeutic approaches. hichmethod is to be used ultimately depends on the anatomi-cal localization of the disorder of venous return and thedegree of chronic venous insufficiency.
In primary varicosis, remediation may possibly beachieved by sclerotherapy of peri-ulcer varicose veins,surgical treatment of saphenous insufficiency or scle-rotherapy of lateral branch varices. Compression treat-ment, performed initially using a compression bandageand later with a compression stocking, must always becontinued until complete healing of the ulcer is achieved.
In secondary varicosis and when there is severe venoushypertension in the suprafascial venous system, perma-nent closure of insufficient perforating veins supplyingthe ulcer is rarely successful. The temporary scleroticprocess induced by the sclerotherapy, however, providestemporary hemodynamic relief and greatly improves the
healing tendency. This applies especially to the varicoseveins passing through the ulcerated area and the proce-dure – when carried out by an experienced and skilledsclerotherapist – often results in rapid healing.
Sclerotherapy within or close to areas of atrophie blanchemust remain the exception. If sclerotherapy is unavoid-able, a much lower concentration of sclerotic agent mustbe used than would be indicated for an area of healthyskin.
If the chronic venous insufficiency cannot be compensat-ed on the basis of functional diagnostic criteria, after theulcer has healed at least the surrounding perforatingveins should be ligated to provide hemodynamic relief.
Surgical treatment of ulcersFor obstinate, therapy refractory ulcers, a surgical inter-vention proximal from the ulcer in the scar-free skin areas may be required. Procedures with good successrates include especially Hach's paratibial fasciotomy andits more advanced form, Hauer's endoscopic perforator ligation.
Hach's procedure is based on the notion that splitting themuscle fascia along the entire edge of the shinboneallows capillaries to grow from the well perfused muscletissue into the ulcer region, thereby promoting tissue neo-genesis. With Hauer's method, hemodynamic aspects pre-dominate in the presence of insufficient Cockett's perfo-rating and simultaneous insufficiency of the deep veinsystem.

Therapy [28.29]
Adjuvant medicinal therapySystemic treatment of venous leg ulcer with the variouspharmacological venotherapeutic agents is mainly of anadjuvant nature and is intended to support the deconges-tion induced by the compression therapy. Three groups ofsubstances are used: diuretics, vasoactive (venotonicising)drugs and edema-protective agents.
Diuretics may be indicated for short-term use especially inthe initial phase of treatment to mobilise local, reversibleedema. Under no circumstances, however, should they beused to provoke a potent diuretic effect. Contraindicationsare high-protein edema and lymphedema.
Venotonicising drugs are reported to cause a reduction inthe venous cross-section while simultaneously increasingblood flow velocity and reducing blood viscosity. Thetherapeutic objective of edema-protective agents is toinfluence the capillary vessel walls in order to reduce theextravasation of fluid into the tissue. Both medicationgroups include synthetic and purely plant-derived sub-stances such as horse-chestnut, boxholly and sweet cloverextracts in single-agent or combination preparations.Although the efficacy of the various pharmacologicalagents has been increasingly demonstrated in recentyears, they are by no means capable of replacing com-pression therapy.
Identification of wound healing disordersAlthough the course of healing of venous leg ulcer maybe expected to be irregular in view of its etiopathologicorigins, a variety of systemic and local influences can alsobe expected to induce further disorders which delay heal-ing of the ulcer for months or even years. It is thereforeimportant to identify and eliminate possible disorders.
Systemic disorders of wound healing mainly involve fac-tors that are generally relevant to the healing process ofchronic wounds, and thus also for venous leg ulcers.Primary factors are the patient's age and nutritional sta-tus, certain basic diseases and also medication relatedeffects.
Findings generated in clinical research allow the conclu-sion that physiological aging delays wound healingprocesses because of the generally reduced cellular activi-ties, which may ultimately also be reflected in a reductionin the quality of the wound healing outcome. Serious dis-orders of wound healing, however, are usually an expres-sion of the effects of age-related multimorbidity.
Wound healing requires a sufficient supply of protein,vitamins (especially C and A) and minerals (especiallyiron, copper and zinc). Because of inadequate nutrition,disorders of absorption or the effects of concomitant dis-eases, elderly patients frequently exhibit protein and vita-min deficiency states which should be diagnosed andtreated. If zinc replacement appears useful, this shouldnot be done externally with zinc ointments but by pre-scribing suitable oral zinc supplements.
Besides the vascular disorders which increase with ageand which, as already described, create the basis for thevarious leg ulcers, other diseases that compromise woundhealing are connective tissue diseases (e.g. rheumatic diseases), endocrinopathies (e.g. thyroid, adrenal) andmetabolic disorders (e.g. diabetes mellitus), but also alldiseases which influence the affected person’s immune status, such as malignancies, infectious diseases or hema-tological disorders.

� Clinical examination� Instrumental diagnosis� Differential diagnosis (arterial ulcers, mixed venous-
arterial ulcers diabetic ulcers, exgonous, infectious ulcers, ulcers due to hematologic diseases, neoplastic ulcers)
� Permanent zinc paste bandage� Temporary short-stretch bandage� General principle: The patient should be as mobile
as possible with the bandage
� For compensation of CVI: Sclerotherapy, phlebo-surgery
� For ulcer resection: paratibial fasciotomy or endo-scopic perforator ligation, as required
� Surgical debridement� Physical cleansing by moist wound treatment � Continuation of moist wound treatment during
granulation until spontaneous epithelisation, skin grafting if required
� Compression stocking to maintain the therapeutic result� Lifestyle promoting healthy veins with as much exercise
as possible/elevation of the legs, weight reduction where appropriate
� Adjuvant medication with edema-protective agents, where appropriate/venotonicising agents
Therapy [30.31]
The influence of medications is also to be evaluated.Various pharmacologic agents exert directly deleteriouseffects on wound healing, especially immunosuppres-sants, cytostatics, anti-inflammatories (mainly glucocorti-coids) and anticoagulants.
The patient's psychosocial situation also plays a notinconsiderable role. The management of chronic woundsalways requires a high level of compliance from thepatient because treatment is not confined to local proce-dures but also requires the consistent and conscientiousapplication of causal therapies such as compression treat-ment. The patient is to be adequately informed about thepurpose of and necessity for the individual elements oftreatment, otherwise compliance will be partially or com-pletely lacking.
Local interfering factors usually have their origins inincorrectly practised wound management. The use of mul-tiple topical therapeutic preparations is especially to bementioned in this respect. Such practices can not onlygreatly compromise the wound healing process, but alsodrastically increase the risk of local and systemic aller-gies. Especially those patients who all too readily resortto the use of “miracle cures” in their understandable wishto hasten the healing of their ulcer should be persuadedof the risks involved.
Pain management Anaesthetic topical therapeutic agents are contraindicat-ed due to the risk of contact allergies. The following pro-cedure is therefore recommended for severe pain: applycompresses immersed in ice water or cool the ulceratedarea with ice packs at intervals during the 20 to 30 min-utes before bedtime. In most cases the pain subsides rel-atively quickly with correctly applied compression therapy.An analgesic can be given to control nocturnal discomfortin the initial phase.
Course of treatment of venous leg ulcer
Compression therapy
Invasive therapy
Local ulcer therapy
Diagnosis
Continuation treatment
Treatment

Phase-specific wound management [32.33]
Regardless of the type of wound and the extent of tissueloss, every wound healing process proceeds in phaseswhich overlap in time and cannot be separated from eachother. Classifications into three or four phases of woundhealing are usual; the system postulating three basicphases will be used in the following presentations:▪ The inflammatory and exudative phase serves to stop
the bleeding and cleanse the wound, mainly by phago-cytosis.
▪ In the proliferative phase, blood vessels and replace-ment tissue, known as granulation tissue, are produced to fill the defect.
▪ The differentiation phase is characterized by maturationof the new tissue, its epithelisation and the concluding scar formation.
In practice, the three phases of wound healing are knownfor short as the cleansing, granulation and epithelisationphase.
Entstehungsursachen [0.0]
Phase-specific wound managementof venous leg ulcer
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21
Inflammatory phase:Cleansing
Proliferative phase:Fibroblast migration and formation of granulation tissue
Differentiation phase:Maturation and increasingwound contraction/epithelisation
Schematic diagram of the time course of the wound healing phases:
Chronic wounds like venous leg ulcer also heal in aphase-specific manner. However, the progression ofthese phases through the correct sequence is frequentlydisturbed by many different systemic and local interfer-ing factors; often, the cleansing phase persists for anunphysiologically protracted period. Proper wound man-agement will therefore be based on the premise of meet-ing the specific requirements of the disturbed woundhealing phases as exactly as possible.

Phase-specific wound management [34.35]
This physiological wound healing cascade, which alwaysrequires the cells involved in repair to appear in thechronologically correct order, only occurs spontaneouslywhen certain basic requirements are fulfilled:▪ The cell metabolism must be assured by an supply of
adequate blood and oxygen. ▪ A physiologically balanced, moist wound environment
with an adequate pH must be present in the wound to promote the cellular activities.
▪ All inhibiting factors together, such as microbial colo-nization and toxic degradation products of bacteria andtissue, must not exceed the autolytic capabilities of the wound.
If these conditions are not present due to the influence ofvarious deleterious factors (inadequate blood supply withtissue hypoxia, drying out of the wound floor, woundinfections etc.), more or less pronounced disorders ofwound healing and, without timely intervention, a chron-ic wound will develop: Cells die, necrotic tissue forms toan extent that can no longer be compensated by endoge-nous cleansing mechanisms. At the same time, toxicdegradation products of bacteria and tissue infiltrate theperi-wound area, giving rise to further tissue necrosis andmaintaining the chronicity of the wound.
The problems associated with the chronic wound becomemore severe if the ulcer has developed due to microcircu-latory and metabolic disorders in the cutis and subcutis,as is the case with venous leg ulcer. In contrast to anacute wound, in which the preconditions for the woundhealing cascade to proceed in the proper sequence arecreated in the inflammatory-exudative phase, with ulcersof ischemic origin the repair activities of the cells have tobe initiated in an area of skin with highly compromisedmetabolism, which makes a properly regulated process of
wound healing impossible from the outset.
The pathophysiological situation existing in venous legulcer, however, also indicates the kind of measures thatneed to be taken to achieve ulcer healing:▪ As a causal measure, the hemodynamics in the leg vein
system and the microcirculation in the wound area are to be improved by the methods already described, such as compression therapy and, if necessary, invasive procedures such as surgery and / or sclerotherapy.
▪ Locally, the chronic wound is to be transformed as far as possible into the state of an acute wound by means of adequate treatment. This offers the opportunity for the processes necessary for healing to be re-initiated in the physiologically correct cellular and temporal sequence and to proceed in a regular manner.
Which activities have proved beneficial in which phasesof wound healing is described below. Moist wound treat-ment has proved particularly successful; its principles willtherefore now be explained.
Moist wound treatment“A dry wound is a dead wound”. Based on this recogni-tion, the principle of moist wound healing has becomethe established approach to the management of second-ary healing wounds, i.e. wounds in which granulation tis-sue has to be formed, and for epithelial wounds. Thebenefits of this method of treatment, which is based onstudies by G. D. Winter (1962, first published in“Nature”), the underlying scientific principles of whichhave been scientifically validated in general terms, arewell known, and have effects on all phases of woundhealing:

Phase-specific wound management [36.37]
During the cleansing phase, moist wound dressingsachieve a thorough cleansing of the wound and renderpossible mechanical debridement without damaging cells.Inactivation of immunocompetent cells can also be avoid-ed by the moist environment (Seiler).
During the granulation phase, a physiological microcli-mate similar to a cell culture medium is created withinthe wound, which encourages cellular proliferation andconsequently the formation of granulation tissue. Turner /Beatty et. al (1990) have reported that permanent moisttherapy causes a significantly more rapid reduction in thewound area and a larger amount of granulation tissue.
In the epithelisation phase, the conditions for mitosis andmigration of epithelial cells improve under moist dress-ings. This generally results in more rapid epithelisationwith better cosmetic results.
Patients frequently report that their pain is relieved undermoist wound treatment. In addition, the dressing changeitself is atraumatic and causes less pain because moderndressings, as used for moist wound treatment usually donot adhere to the wound, i.e. have atraumatic properties.At the same time, this “nonstick” effect eliminates thestripping off of cell layers when the dressing is changed –the undisturbed state of the wound so important for heal-ing is preserved.
However, the success of moist wound treatment dependson a critical prerequisite: the wound requires a perma-nent, uninterrupted, balanced supply of moisture. If atany stage drying out is allowed to occur, the cellsinevitably die as a consequence. Further necroses developand can even eventually deepen the wound.
The most basic type of moist wound dressing is the tradi-tional gauze dressing, moistened with normal saline orRinger's solution. However, this is also the type of dress-ing most liable to create problems. Gauze dressings dryout rather quickly and stick to the wound, an unfortunateproperty that causes freshly formed cells to be torn awaywith the dressing as the latter is changed. Moreover,ensuring a permanent supply of moisture to the compressis time-intensive, not easy to manage and is difficult toreconcile with compression therapy.
The so called hydroactive wound dressings, in compari-son, are an innovation that represents a major advance,not only in regard to efficacy but also practicality. Theyinclude the gel forming calcium alginate dressingSorbalgon, the wound pad dressing TenderWet, thehydroactive foam dressing PermaFoam, the absorbenthydrocolloid dressing Hydrocoll and the transparenthydrogel dressing Hydrosorb. With these dressings,wounds can be kept permanently moist without difficulty.Moreover, the differentiated physical principles of actionof the various wound dressings ensure that the specificrequirements of many different wound conditions can beselectively fulfilled.
Wound management in the cleansing phaseExperience has shown that this initial phase demandsgreat patience and will need more time to complete thelonger the ulcer has existed. This is because the derangedmetabolic situation in the area of skin which is responsi-ble for the venous ulcer not only maintains the chronicityof the wound but also greatly hinders the self-cleansingmechanisms. The vicious cycle can only be broken by ade-quate treatment: compression therapy is indispensable toimprove the hemodynamics and selective cleansing proce-dures are also of major importance.

Phase-specific wound management [38.39]
Ulcers with a severely damagedperi-ulcer area require particularlygentle wound treatment, forexample with TenderWet com-presses.
The silver-containing ointmentdressing Atrauman Ag with reliable bactericidal action is indi-cated for infected wounds.
The healing tendency of a venousleg ulcer improves dramaticallywhen necroses and tissue inade-quately supplied with blood areremoved as completely as possi-ble.
Surgical removal of necrotic tissueIf the patient's medical situation allows, surgical debride-ment should be performed to remove necrotic and inade-quately perfused tissue and fibrinous necrotic slough ascompletely as possible. This results in a “fresh”, bleedingwound. Wound healing can then commence, as in anacute wound, with hemostasis followed by the release ofgrowth factors and migration of sufficient inflammatorycells into the wound, and can then reorganise itself intothe chronologically correct sequence of events. Thisapproach should be considered especially for therapy-refractory ulcers; after wound conditioning, there may bean indication for wound closure by split-thickness skingrafting.
For care of the surgically debrided ulcer and subsequentwound conditioning, wound coverage with the Sorbalgoncalcium alginate dressings, whose principle of action isdescribed from page 49 onwards, should be performed.
Cleansing by moist wound treatmentIf surgical debridement is impracticable, physical debride-ment by moist wound treatment may be substituted.Hydroactive wound dressings with different modes ofaction are available for this purpose and are to be usedselectively depending on the condition of the wound.
For ulcers with pronounced fibrinous and/or slimy coats(infected or non-infected), moist therapy with TenderWet24 active is recommended. The principle of action of this“absorbent-rinsing dressing” is described from page 44onwards. TenderWet is especially suitable in cases inwhich the ulcer environment is extremely sensitive due toeczematous lesions.
Particularly suitable for treatment under compressionbandages is the hydroactive foam dressing PermaFoam.This dressing has a high vertical wicking effect for rapidregulation of wound exudate as well as high retention forreliable fluid binding, thereby protecting the wound mar-gins and minimising the risk of maceration. Detailedproduct description from page 50.
For moderately exuding ulcers which still have a relativelyintact peri-ulcer area, the absorbent hydrocolloid dressingHydrocoll can be used, which because of its semi-perme-ability is particularly effective in supporting the autolyticprocesses of wound cleansing. The principle of action ofHydrocoll is described in detail starting on page 53.
Infection prophylaxis and controlThe problem of infection prophylaxis and control is mostlikely to arise in the cleansing phase, which is oftenfraught with uncertainties. In most cases, the ulcer canbe assumed to be colonized with microorganisms,although the contamination – especially in the case ofpurely venous ulcers – relatively rarely leads to a clinicallyovert infection. The rather low susceptibility to infectiongenerally observed with older wounds thus also seems toapply to venous leg ulcers. Prophylactic disinfection ofthe ulcer or topical antibiotic therapy is therefore notadvisable in most cases, especially considering the poten-tial of many of these substances to inhibit wound healingand the high risk of sensitization.
One treatment option for infected and infection-pronewounds is the silver-containing ointment dressingAtrauman Ag. It has a broad spectrum of action and asustained bactericidal action combined with proven goodtissue tolerability and only low toxicity. Details aboutAtrauman Ag from page 56.

Phase-specific wound management [40.41]
Hydrosorb reliably protects thedeveloping granulation tissuefrom drying out.
Atrauman Ag can also be used when systemic antibiotictreatment becomes necessary for severe infections withmarkedly elevated C-reactive protein. It may be useful tocarry out a microbial identification and antibiotic sensitiv-ity test to optimize the antibiotic therapy.
Wound management in the granulation phaseIf the wound floor is clean, granulation tissue can formprovided that the hemodynamic disorder underlying theulcer continues to be compensated by compression therapy.
The nature of the granulation tissue is an important indi-cator of the quality of the repair process. Granulation tis-sue itself reacts with extreme sensitivity to exogenousinfluences and interfering factors and should therefore betreated as gently as possible. Fresh red granulation tissueno longer requires to be cleaned and irrigated and needsno ointments or powders to promote its growth. However,granulation tissue must be kept permanently moist withsuitable hydroactive wound dressings. If the wound isallowed to become dry, cell necrosis again results in tis-sue death. Granulation tissue also has to be protectedagainst mechanical irritation caused by stripping of cellswhen changing the dressings.
This is because granulation tissue has an extremely adhe-sive quality because of the high-protein exudate and thelarge number of superfine capillaries. Chronic ulcers fre-quently show a constellation in which part of the woundis already granulated, while other parts are still in thecleansing phase. If wound disinfection is required andduring mechanical debridement, the granulation tissueshould be spared.
A hydroactive wound dressing that meets the require-ments of the granulation phase particularly well is thetransparent hydrogel dressing Hydrosorb. Its gel structurehas a high water content, allowing it to deliver moistureindependently to the wound over prolonged periods with-out itself drying out. Especially when the formation ofgranulation tissue is stagnating, a therapy trial with thehydroactive foam dressing PermaFoam may be useful. Thespecific mode of action of Hydrosorb is described frompage 55 onwards.
Peri-ulcer eczemaVenous leg ulcer is frequently accompanied by eczema.The eczema may be due to colonization of the damagedskin with bacteria and fungi (microbial eczema) or may bea contact allergy to topical medications.
The treatment is based on the general principles ofeczema therapy: The acute, weeping eczema is treated bymoist therapy, for example using moist tulle dressingswith astringent or disinfectant solutions. The skin, howev-er, should be prevented from drying out.
Subacute or chronic eczema should be treated in a differ-entiated manner, but using only non-allergic ointmentbases and substances. Zinc paste (Pasta zinci) and coldcream (Unguentum leniens) in equal parts has proved asuccessful therapy in such cases. Long-term therapy withcorticoid-containing topical preparations, however, shouldbe avoided due to the risk of skin atrophy.

Phase-specific wound management [42.43]
Ulcer grafted with split-thicknessskin (mesh graft 1:1.5)
Wound management in the epithelisation phaseWell-developed granulation tissue offering the epithelialcells a moist gliding surface is the prerequisite for themitosis and migration of epithelial cells. The most impor-tant function of the dressing is therefore to ensure thatthe wound also remains moist during the epithelisationphase. Again, the ideal product for this purpose is thehydrogel dressing Hydrosorb or the hydrocolloid dressingHydrocoll thin, which was developed especially foralready epithelised wounds.
An ulcer with a good healing tendency can be recognizedfrom the fact that epithelisation is proceeding inwardsfrom the ulcer margin or enlarging islands of epithelialtissue are spreading over the ulcer floor.
Certain topical therapeutic medications which inducescabbing of the ulcer can bring about a type of “spurioushealing”. In most cases these encrustations can easily bedetached again from the ulcer margin. The yellowishcoatings underneath also have to be removed, and onlythen is a prognostic evaluation of the cleansed ulcer floorpossible.
Because of the protracted course of healing, the woundmargins of chronic ulcerations sometimes tend to epithe-lise and protrude inwards. Since no further epithelisationcan then take place from the wound margin, the woundmargins should be refreshed by trimming with a scalpelor sharp scissors.
Like all chronic wounds, venous ulcers also sometimesexhibit a poor tendency to spontaneous epithelisation. Ifthe wound floor has been sufficiently conditioned, woundclosure by split-thickness skin grafting (mesh graft) or theReverdin method may be considered in these cases, espe-cially for larger wound surfaces. In the Reverdin proce-dure, the flaps of epidermis applied onto the granulation
tissue form islands from which epithelisation can pro-ceed. Another possibility is the grafting of autologousand in vitro cultured keratinocytes. These keratinocytecultures are prepared by isolating keratinocytes from apiece of the patient's skin.
Therapy-refractory ulcersIf the ulcer refuses to heal despite all endeavours, thetherapeutic concept should be reviewed. The followingcheck list may assist in identifying possible causes oftherapy-refractory ulcers:▪ Is the compression therapy being adequately per
formed? If appropriate, change from temporary to per-manent bandages, use stronger compression etc.
▪ Are the lesions being treated mixed arterial-venous ulcers?
▪ Doppler sonographic evaluation of peripheral blood circulation, further angiographic diagnostic imaging if required
▪ For arterial hypertension (Martorell ulcer!): treat the hypertension
▪ Is there latent or overt right ventricular failure (edema in healthy leg)?
▪ Additional outflow disorders due to secondary lym-phedema?
▪ Arthrogenic stasis syndrome in knee or hip arthrosis?▪ Lack of exercise (“rather run and lie down, sitting and
standing are bad”, obesity)?▪ Erysipelas, mycotic and/or bacterial superinfection
(clinical symptomatology)?▪ Ulcer of other etiology?▪ Therapy-refractory accompanying eczema: Allergy test-
ing.▪ Poorly managed diabetes mellitus (determine HbA1c).

1
Phase-specific wound management [44.45]
The principle of action ofTenderWet
TenderWet – wound pad with super absorberTenderWet is an extremely effective wound dressing forthe treatment of chronic, infected and non-infectedwounds during the cleansing phase and at the start ofthe granulation phase. This high efficiency is attributableto a special mode of action which allows continuous“rinsing” of the wound.
TenderWet is a multilayered dressing pad containingsuper-absorbent polyacrylate (SAP) as the central compo-nent of its absorbent core. The active agent-free superabsorber is activated before use with an appropriatequantity of Ringer’s solution which is then released con-tinuously into the wound for hours. The constant deliveryof Ringer’s solution softens, detaches and rinses awaynecrotic tissue (1).
At the same time, however, microbially contaminatedwound exudate is absorbed and bound into the wounddressing pad. This exchange – Ringer’s solution is deliv-ered and proteins are absorbed - functions because thesuper absorber has a greater affinity for the protein-con-taining wound exudate than for the sodium-containingRinger’s solution (2) and so the wound exudate displacesthe solution from the wound pad. As soon as the factorsinhibiting wound healing are removed, i.e. the wound hasbeen cleansed of necrotic tissue, detritus and coatings,the conditions necessary for the buildup of granulationtissue are present: proliferative cells can migrate into thewound area and capillary ingrowth is possible (3). Themoisture and the electrolytes contained in the Ringer’ssolution, such as sodium, potassium and calcium, con-tribute to the cell growth.
TenderWet has no contra-indications and can also beused on infected wounds. In certain cases, there is anapparent increase in the size of the wound during the initial cleansing phase with TenderWet.
TenderWet is available in different sizes and shapes toallow adaptation to different wound conditions. Tender-Wet is activated with Ringer’s solution or TenderWet solu-tion directly in the half-opened sterile peel pack.
This means that with this method devitalised tissue whichwas not recognisable as such was removed. In the case ofdeep wounds, TenderWet should be packed in loosely toensure the direct contact needed for the fluid exchange.The physical characteristics of the super absorber in com-bination with the outer covering of knitted fabric on thewound pad give TenderWet the necessary packing charac-teristics. With extensive wounds, the TenderWet woundpads should be applied with a slight overlap – he “tiling”.
TenderWet comes in a range of variants and is availablein round and rectangular shapes to meet differing appli-cation requirements.
The classical TenderWet maintains its absorbing and rins-ing effect for about 12 hours. Dressing changes shouldtherefore be carried out every 12 hours. The frequency ofdressing change, however, ultimately depends on theamount of exudate produced by the wound. How muchRinger’s solution is required to activate the dressingdepends on the size of the compress. For fault-free acti-vation of TenderWet (and also of TenderWet 24),TenderWet solution is supplied in convenient sizes of 10,15 and 30 ml. The composition of the sterile, pyrogen-free and isotonic solution corresponds to that of Ringer’ssolution.
TenderWet 24 is made from the same materials asTenderWet, but is designed so that the absorbing andrinsing effect is sustained for up to 24 hours. To protectthe dressing from strike through, a moisture -repellentlayer is integrated inside the dressing on the side facingaway from the wound.
2
3
TenderWet und TenderWet 24 areto be activated with TenderWetsolution or Ringer's solutionbefore use.
TenderWet is available in differentsizes and shapes to allow adapta-tion to different wound condi-tions. TenderWet is activated withRinger’s solution or TenderWetsolution directly in the half-opened sterile peel pack.

Phase-specific wound management [46.47]
Approximately 70-year-oldpatient with recurrent venous legulcer since1992 (Case study B.Kowollik, Neuss)1) 7 November 02, Status ofvenous ulcer after 5 days’ treat-ment with TenderWet 24, thewound is increasingly clean.2) 15 November 02, all threephases of wound healing are visi-ble: in the upper third epithelium,in the left third well-conditionedgranulation tissue, in the righthalf the wound is still in thecleansing phase. 3) After 12 weeks the woundarea is about two thirds reducedin size.4) 28 February 03, the rapidcourse of wound healing hasslowed down greatly.5) To influence the perforatingvein insufficiency, which wasidentified as the obstacle to heal-ing, the pressure was increased inthe ankle region by fitting a sup-port pad.6) Finished compression bandage7) 14 May 03, increasing thecompression was successful, theulcer had decreased in size byone half.8) 18 June 03, completely healedulcer
TenderWet 24 active is alreadyactivated with Ringer’s solutionready for use. The integrated pro-tective layer makes the dressingwell suited for treatment under acompression bandage.
The side of the compress with the integrated protectivelayer is identified by the presence of parallel colouredstrips to allow secure positioning of the wound pad.Because of this protective layer, TenderWet 24 should notbe packed into the wound. For greater ease of use,TenderWet and TenderWet 24 are supplied in already acti-vated form as TenderWet active cavity and TenderWet 24active. These active wound pads are saturated ready touse with Ringer’s solution and can be applied immediate-ly. This dispenses with time consuming preparations.Another advantage of the already activated wound padsis that a much greater volume of Ringer’s solution can beintroduced into the absorbent core than is possible withmanual impregnation. As a result, the wound can be keptmoist for longer.
Moreover, the pads are soft and easy to mould, especiallyin the case of TenderWet active cavity, which can be usedto pack even cavernous wounds without difficulty. In con-trast, TenderWet 24 active should not be packed into thewound because of its moisture-repellent protective back-ing layer.
The following applies generally to all TenderWet wounddressing pads: They are not self-adhesive and requireadequate fixation, e.g. complete-cover dressing retentionwith elastic non-woven sheet dressings (e.g. Omnifix) orelastic conforming bandages (e.g. Peha-crepp, Peha-haft).
1 2
3 4
5 6
7 8

Phase-specific wound management [48.49]
The principle of action ofSorbalgon
Sorbalgon is available in twodressing sizes and as ribbons.
76-year-old-patient with a venousleg ulcer on the left lower leg for30 years, with slimy coating, tor-pid granulation (Case study Prof.H. Winter, Berlin)1) Ulcer status on admission.2) Start of wound treatment withTenderWet 24. In the initial phaseactivated with local antiseptic(Lavasept).3) Therapy continued withTenderWet 24 combined withcompression treatment (short-stretch bandages).4) Clean wound conditions withformation of abundant granula-tion tissue 4 weeks after woundtreatment with TenderWet 24.5) Split-thickness skin graft (meshgraft technique).6) Result one year after grafting.
1 2
1
2
33 4
5 6
Sorbalgon – calcium alginate dressings with excel-lent conformabilitySorbalgon is the wound dressing ideally suited for cleans-ing and for supporting the buildup of granulation tissuein cavernous wounds and wounds in difficult anatomicalsites. By virtue of its excellent packing characteristics,Sorbalgon also provides effective cleansing and condi-tioning in deep wounds. In the treatment of venousulcers, Sorbalgon is especially indicated during the fol-low-up period in patients who have undergone surgicaldebridement of necrotic tissue.
Sorbalgon is a non-woven dressing made of high-qualitycalcium alginate fibres which are introduced in the drystate into the wound (1). As they absorb sodium salts,present for example in blood and wound exudate, thefibres start swelling and undergo transformation into amoist absorbent gel which expands to fill out the wound(2). Since Sorbalgon adapts closely to the wound sur-faces, microorganisms are also absorbed deep inside thewound and are reliably absorbed into the gel structure(3). This provides efficient microbial reduction and helpsavoid recontamination. Wounds are swiftly cleansed, andSorbalgon has therefore proved especially successful inthe treatment of chronic and infected wounds.
With its gel-like consistency, Sorbalgon also acts like amoist dressing that prevents the wound drying out. Thedressing creates a microclimate favourable for woundhealing, promotes the formation of granulation tissue andkeeps the wound surfaces supple. Sorbalgon’s gel-form-ing properties prevent it from sticking to the wound anddressing changes are painless. However, complete gelatinisation of the calcium alginate fibres requires thepresence of sufficient exudate.

Phase-specific wound management [50.51]
The hydrophilic foam dressingPermaFoam with its convincingphysical mode of action extendsthe range of treatment optionsfor chronic wounds.
The therapeutic efficacy ofPermaFoam derives from its spe-cial pore structure: Large poreson the wound-facing side becomeprogressively smaller in the direc-tion towards the top layer, whichproduces a high vertical capillari-ty. This causes exudate to bequickly drawn up into the body ofthe foam, but it also ensures highretention for reliable fluid bind-ing.
The frequency of dressing changes depends on the indi-vidual wound situation. In the wound cleansing phase, 1to 2 dressing changes daily may be required dependingon the amount of exudation. Later, as granulation tissueforms, a dressing change every two to three days may besufficient. Sorbalgon is available in two sizes as squaredressings. Sorbalgon T is available as a ribbon.
PermaFoam – hydroactive foam dressingThe foam dressing PermaFoam is indicated for non-infect-ed wounds with moderate to heavy exudate in the cleans-ing phase and during the granulation phase. Its therapeu-tic action is based on its special pore structure.
PermaFoam is a combination of two differently structuredfoams that are connected with each other by a specialform of lamination. The absorbent layer of PermaFoamconsists of hydrophilic polyurethane polymers that canstore up to nine times their own weight of liquid in theirpolymeric chains. The poyurethane matrix has a uniquepore gradient: the large pores on the wound-facing sidebecome progressively smaller in the direction towards thetop layer, which produces strong vertical capillary action.The top layer of PermaFoam consists a flexible, close-porous polyurethane foam and is semipermeable, whichmeans impermeable to germs but permeable to watervapour.
This material combination and design results in productcharacteristics which can counteract the maceration prob-lems often observed with chronic wounds: via the strong-ly marked vertical capillarity, the surplus aggressivewound exudate is quickly drawn up to underneath theouter layer. The large foam pores on the wound sideensure that viscous exudate and detritus are alsoabsorbed without blocking the pores. When absorbing
the wound exudate, the polyethylene foam swells slightlywhich ensures the contact necessary to draw off dis-charges from the wound floor.
The absorbed wound exudate then spreads out laterallyunder the outer layer. In this regard, it is also importantthat PermaFoam has – mainly due to the special porestructure – has a high retention capacity for fluids. Evenwhen pressure is applied from outside by, for example, apressure bandage, the exudate is retained in the foam.Also relevant is the fact that the absorptive capacity ofPermaFoam is only slightly reduced even under the pres-sure of a compression bandage. For example, under apressure of 42 mmHg, the absorptive capacity is reducedby only 12 % compared with the pressure-free condition.
Taken together, all these characteristics result not only inthe desirable rapid regulation of exudation, but also pro-tect the wound margins from maceration because theabsorbed wound exudates are not pressed back into thewound again. In addition, the high permeability of theouter layer to water vapour ensures a well-balancedmoist microenvironment for the wound, which furthersupports the healing process.

PermaFoam is atraumatic, sticking to the wound andgrowth of tissue into the foam structure are minimised.Due to the high absorptive capacity and the very goodretention, PermaFoam can – even with profuse exudation(when no complications exist) - remain on the wound forseveral days.
PermaFoam is soft and flexible and therefore clings wellto the wound contours. The dressing is held in place withelastic conforming bandages (e.g. Peha-haft) or over theentire area with elastic non-woven sheet dressing fordressing retention (e.g. Omnifix elastic). For easy fixation,PermaFoam has a adhesive border around the edges andthe adhesive is kind to the skin. PermaFoam is availablein a variety of versions and sizes.
Hydrocoll – absorbent hydrocolloid dressingHydrocoll is a self-adhesive, absorbent hydrocolloid dress-ing for cleansing and conditioning of non-infectedwounds with moderately severely to slightly secretion.
The term “colloid” comes from the ancient Greek andmeans a substance which is integrated in a very finelydispersed form in a matrix. Hydrocoll therefore consists ofhydrocolloids capable of absorbing and swelling and areincorporated in a self-adhesive elastomer. A semiperme-able layer serves to prevent bacterial and moisture pene-tration.
The central feature of the mechanism of action ofHydrocoll is the hydrocolloids incorporated in the carrierlayer. On absorbing wound exudate they swell to form agel which expands into the wound and maintains a moistwound environment. The gel remains absorbent until thehydrocolloids are saturated. During the swelling processthe absorbed wound exudate, which is always contami-nated with detritus, bacteria and their toxins, is securelyretained within the gel structure.
The adhesive power of the elastomer allows Hydrocoll tobe applied to the wound like an adhesive plaster. Whenthe gel forms, the adhesive power on the wound surfacedisappears, leaving Hydrocoll fixed only on the intactperiwound area in a manner atraumatic to the wound.
1 2
3 4
Phase-specific wound management [52.53]
The principle of action ofHydrocoll
Hydrocoll is easy to apply like aplaster. When the hydrocolloidsare saturated by absorbing exu-date, this is shown by a blister-like bulging of the dressing.Hydrocoll should then bechanged.
69-year-old female patient withan 8-year history of venous legulcer (Case study: M. Zimmermann, Heidenheim)1) State of the ulcer on 27 Marchon starting the new therapy con-cept starting with TenderWetfor initial cleansing.2) Treatment was changed toPermaFoam to influence the stillheavy flow of exudate and pre-vent maceration of wound mar-gins on 4 April.3) Continuation of PermaFoamtherapy, a strip of epithelial tissueis visible at the wound margin.4) State of the ulcer on 6 August,after changing to Hydrocoll twoweeks previously to promoteepithelisation.
PermaFoam is available in spe-cial, wound adapted sizes toallow optimal wound manage-ment in all cases. PermaFoamconcave (1) for use on the heelsand PermaFoam round (2) for thecare of smaller ulcers in problemzones.
1 2

Phase-specific wound management [54.55]
The principle of action ofHydrosorb
The “Hydrocoll thin” version isspecially suited for alreadyepithelising wounds.
Hydrocoll is manufactured using hydrocolloids with espe-cially good absorptive and swelling properties, and whichalso have the characteristic of retaining a compact gelstructure. Although Hydrocoll expands into the wound, inthe gelatinised state it can be removed from the woundas an entirely intact dressing. Hardly any gel remnantsremain in the wound, making it only exceptionally neces-sary to irrigate the wound to remove gel residues of pus-like consistency. This makes dressing change easier andmore pleasant. Moreover, a reliable wound assessmentcan be made immediately.
The mode of action of Hydrocoll is effective in all thephases of wound healing: Since microbially contaminatedwound exudate is quickly taken up into the hydrocolloidstructure of the dressing by the absorbent and swellingprocess, the wound is rapidly and effectively cleansed. Asgeneral studies have shown, the microcirculation in thewound area also improves with progressive cleansing. Thebody's own cleansing mechanisms are reactivated espe-cially in chronic wounds in which the cleansing process isstagnating. During the granulation phase, the moistwound environment maintained by Hydrocoll stimulatesthe formation of granulation tissue. With Hydrocoll, thebalanced moist wound environment can also be main-tained without difficulty over prolonged periods and thegranulation tissue is reliably prevented from drying out.In the epithelisation phase, the cell-friendly moist woundenvironment promotes mitosis and migration of theepithelial cells. In addition, undesirable scab formationwhich could delay healing is prevented. The impermeableto bacteria and liquid top layer forms a reliable barrieragainst microorganisms and protects the wound from dirtand moisture. Mobile patients can shower with the dress-ing in place. The “Hydrocoll thin” version is specially suit-ed for already epithelising wounds.
Hydrosorb – transparent hydrogel dressingHydrosorb is particularly suitable for keeping granulationtissue and young epithelium moist and protected and isthus the optimum wound dressing for phase-adapted fur-ther treatment after wound treatment with TenderWet,Sorbalgon or PermaFoam.
Hydrosorb is a ready-to-use gel dressing made ofabsorbent polyurethane polymers with a high water con-tent of 60 %. Hydrosorb provides the wound with mois-ture for several days from the start (1). At the same time,Hydrosorb absorbs excessive secretions which are thenheld in the gel structure. This exchange ensures the opti-mum moisture level for wound healing, thus promotingthe production of granulation tissue and epithelialisation(2). The surface is impermeable to water and bacteria toprotect against secondary infections.
Hydrosorb does not stick to the wound and can beremoved even after prolonged periods on the woundwithout the risk of wound irritation. Hydrosorb can beremoved in its entirety as the gel sheet structure does notbreak down because of the absorbed secretions. Noresidues remain in the wound and the condition of thewound can be assessed without prior irrigation.
The transparency of Hydrosorb isimportant for its cost-effectiveuse, since it makes it possible toinspect the wound at any time,allowing Hydrosorb to remain onthe wound for days, which saveson dressing changes.

Phase-specific wound management [56.57]
80-year-old patient, disorder ofwound healing with infection fol-lowing resection of the 4th toedue to osteomyelitis of themetatarsal bone1) Initial examination: The woundmeasures 3,2 x 2 cm, the woundfloor is 20 % covered with light-coloured and moist coating, 40 %with granulation and epithelialtissue.Treatment with Atrauman Ag incombination with PermaFoam.2) After two weeks underAtrauman Ag: 50 % of the woundfloor is granulated or epithelised.
Mechanism of action of AtraumanAg: Bacteria (green) are destroyedby contact with Atrauman Ag.The wound exudate (yellow)together with the dead bacteriaand the endotoxins produced bythis process are absorbed into thesecondary wound dressing.The persisting bactericidal actionof Atrauman Ag has been demon-strated in a laboratory test(Method ASTM 2180).
In addition, the transparency of Hydrosorb, which ismaintained even after prolonged use is particularly usefulin practice. It allows inspection of the wound without achange of dressing. This ensures the non-disturbance ofthe wound as well as being highly cost-efficient becauseof the longer intervals between dressing changes.
Hydrosorb is available in two versions as Hydrosorb andHydrosorb comfort. Both hydrogels have the same physio-logical mode of action but differ in their method of fixa-tion. Hydrosorb does not have an adhesive edge and issecured with adhesive tape, a dressing retention bandageor a compression bandage. Hydrosorb comfort is sur-rounded by a hypoallergenic adhesive film border for bac-teria-proof fixation. Together with the outer surface ofHydrosorb comfort, which is impermeable to bacteria andwater, this particularly facititates daily hygiene.
Atrauman Ag – silver-containing ointment dressingfor infection controlThe germicidal action of silver-containing wound dress-ings has long been known. The silver-containing ointmentdressing Atrauman Ag is a successful attempt to create aproduct with reliable bactericidal activity but only lowcytotoxicity so that wound healing is not compromised.
The support fabric for Atrauman Ag is made of an open-weave hydrophobic textile made from polyamide. It iscoated with metallic silver which is chemically bound, i.e.firmly fixed, to the support fabric. The silver-coated sup-port fabric is in turn impregnated with a hydrophilic oint-ment. The complete system is highly permeable to air andwater vapour. This design offers decisive advantages:When in contact with wound exudate, the silver-contain-ing ointment dressing releases silver ions from its metallicsurface. The majority of these ions remain in the immedi-ate vicinity of the dressing – only very few enter thewound itself – adhere to the surface of bacteria and reli-
ably destroy them. The wound exudate together with thedead bacteria and endotoxins produced by this processare absorbed into the secondary dressing.
The fewer silver ions that are released into the wound andinto the cell tissue, the lower the toxicity of the dressingcontaining silver. The low toxicity of Atrauman Ag hasbeen demonstrated in studies with the human keratinocytecell line HaCaT. The bactericidal spectrum of action ofAtrauman AG is extremely broad and includes gram-posi-tive as well as gram-negative bacterial strains. The effec-tive bactericidal action persists not only briefly but for aprolonged period. The ointment impregnation, finally,protects the wound margins and minimises adhesion.
Another aspect of practical importance is that AtraumanAg can be combined with many different wound dress-ings as a secondary dressing without loss of effective-ness, allowing the continuation of treatment with meth-ods in accordance with the indication. Combinations arepossible with, for example, PermaFoam hydroactive foamdressing, the calcium alginate dressing Sorbalgon, thewound pad TenderWet or traditional wound dressings likeES compresses.
1 2 2

Overview of hydroactive wound dressings Overview of hydroactive wound dressings
Phase-specific wound management [58.59]
high-quality calcium alginate dressing, by virtue of its absorptivecapacity and hemostatic properties, is outstandingly suitable forthe care of debrided and heavily exuding ulcers. When the exudateis absorbed, the fibres transform into a gel and trap microorgan-isms.
Sorbalgon Sorbalgon, sterile, 5x5, 10x10 and 10x20 cm;Sorbalgon T ribbons, sterile, 1 g/30 cm and 2 g/30 cm
wound pad dressing with super absorber with unique absorbingand rinsing effect for rapid detachment of coatings. It is particular-ly indicated for infected, purulent and slimy, but also necroticallyencrusted and dried-out ulcers. Ideal: TenderWet 24 and TenderWet24 active, which is activated ready-to-use with Ringer's solution.
TenderWet TenderWet 24 active, sterile, Ø 4, Ø 5.5, 4x7 and 7.5 x 7.5, 10x10 and 7.5x20 cm; TenderWet activecavity, sterile, Ø 4, Ø 5.5, 4x7, 7.5x7.5, 10x10 and7.5x20 cm; TenderWet 24, sterile, Ø 4, Ø 5.5,7.5x7.5 and 10x10 cm; TenderWet, sterile, Ø 4, Ø 5.5, 7.5x7.5 and 10x10 cm
double-layered hydroactive foam dressing with high capillarity.Exudate is rapidly taken up into and retained inside the absorbentcore. Wound exudate does is not pressed back even under com-pression, which also helps spare the wound margins.
PermaFoam PermaFoam, sterile, Ø 6, 10x10, 10x20, 15x15 and20x20 cm; PermaFoam comfort, sterile, 8x8, 11x11,10x20, 15x15 and 20x20 cm; PermaFoam sacral,sterile, 18x18 and 22x22 cm; PermaFoam concave,sterile, 16.5x18 cm; PermaFoam cavity, sterile,10x10 cm; PermaFoam tracheostomy, sterile,8x8 cm
silver-containing ointment dressing with a reliable bactericidalaction for the treatment of infected ulcers. The metallic silver ispermanently bound to the backing material, resulting in very goodproduct tolerability with proven low cytotoxicity.
Atrauman Ag Atrauman Ag, sterile, 5x5, 10x10 and 10x20 cm
self-adhesive hydrocolloid dressing with particularly absorbent andswellable hydrocolloids that transform into a gel on absorbingwound exudate. Microorganisms are also absorbed in the process.Suitable for cleansing, but especially for promoting the buildup ofgranulation tissue in non-infected ulcers.
Hydrocoll Hydrocoll, sterile, 5x5, 7.5x7.5, 10x10, 15x15 and20x20 cm; Hydrocoll sacral, sterile, 12x18 cm;Hydrocoll concave, sterile, 8x12 cm; Hydrocoll thin,sterile, 7.5x7.5, 10x10 and 15x15 cm
transparent, ready-to-use gel with a high water content of about60 %. As a result, Hydrosorb reliably supplies the wound withmoisture, protects it from drying out and prevents scab formation.Ideal for keeping granulation and fresh epithelial tissue moist.
Hydrosorb Hydrosorb, sterile, 5x7.5, 10x10 and 20x20 cm;Hydrosorb comfort, sterile, 4.5x6.5, 7.5x10,12.5x12.5 and 21.5x24 cm

Options for phase-specific wound management of venous leg ulcer
Wound cleansing Granulation Epithelisation
Necrosis Infection Fibrin coating
Exudate ++
Exudate +
� TenderWet 24 active� Sorbalgon� Atrauman Ag with absorbent
wound dressing
intact peri-wound area� PermaFoam comfort� TenderWet 24 activepre-damaged peri-woundarea� PermaFoam
intact peri-wound area� PermaFoam comfortpre-damaged peri-woundarea� PermaFoam
intact peri-wound area� Hydrocoll thin� Hydrosorb comfort� Hydrofilmpre-damaged peri-woundarea� Hydrosorb
TenderWet 24 active
� TenderWet 24 active� Atrauman Ag with absorbent
wound dressing
� TenderWet 24 active intact peri-wound area� Hydrocollpre-damaged peri-woundarea� Hydrosorb
Compression therapy
Permanent bandage:Varolast
Temporary bandage:Pütter bandage
Compression stocking:VitaSan
Fixationnormal skin:Omnifix elastic, Omniplast,Omnisilk, Peha-haft*, Stülpa-fixsensitive skin:Pehalast, Omnipor, Peha-crepp,Extremities:Peha-haft*, Pehalast, Stülpa-fix,StülpaJoints:Omnifix elastic, Stülpa-fix
* Caution: As a cohesive dressing
retention bandage Peha-haft is to be
used with care in patients with blood
circulation disorders and should not
be applied too tightly!
Phase-specific wound management [60.61]

Compression therapy [62.63]
Schematic diagram of an insuffi-cient vein (left) and its constric-tion by a compression bandage(right)
Compression bandaging as basic therapy
The exactly fitting compression bandage is recommendedboth for acute and initial treatment and for maintenancetherapy of all phlebological conditions. Many patientscan be successfully treated by this method alone. Thedecisive factor for therapeutic efficacy, however, is thatthe various available compression materials such asbandages and stockings should be used in accordancewith therapeutic needs.
Compression bandaging is to be regarded as the basictherapy for all venous leg ulcer conditions because itintervenes causally in the disease process. Compressionapplied to the leg causes▪ narrowing of the suprafascial veins with at least partial
restoration of valve function▪ closure of incompetent perforating veins and thus pre-
vention of reflux from sub- to suprafascial, as well as abolition of harmful “shear effects” accompanying mus-cle contraction
▪ when using a suitable technique, reduction of the lumen of the deep and muscle veins and thus a decrease in the dead space, acceleration of blood flow velocity and, to a certain extent, substitution or restora-tion of valve function when valves or valve remnants arestill preserved
▪ an increase in tissue pressure and an associated increase in reabsorption in the terminal vessels and the lymph vessels
▪ reinforcement of the fascia as a resistance surface for the muscles and hence an improvement in the joint muscle pump and self massage of the tissue during movement

Compression therapy [64.65]
Acceleration of the blood flow velocity also hasantithrombotic effects and, in combination with theresulting decongestion, has anti-inflammatory efficacy.
Moreover, the low resting pressure especially of bandageswith a high working pressure allow the small vessels tobe aerated during muscle relaxation and thus to berefilled with arterial blood; during muscle contractionthey are squeezed out again by the high working pres-sure. This interplay of forces increases the blood circula-tion in the nutritive vascular segments of the terminalvessels, thereby substantially improving the metabolicperformance.
Compression therapy is therefore indicated in diseasestates characterized by a tendency to edema, in throm-bophlebitis, deep thrombosis, postthrombotic syndrome,primary varicosis without and with perforator incompe-tence and in venous leg ulcer of any etiology.
The effectiveness of a compression bandage essentiallydepends on the physical properties of the compressionmaterial used in terms of its force-stretch behaviour, andon the application technique employed. However, itshould always be remembered: A compression bandagecan only be fully effective combination with active move-ment!
Certain constellations also place limitations on the use ofcompression therapy: Although pAOD is not consideredan absolute contraindication, in these patients compres-sion therapy may only be used with a thorough knowl-edge of the arterial pressure conditions (caution: arterialankle pressure below 70 mmHg).
Diabetic patients with media sclerosis are at particularrisk in this respect, since sonographic pressure measure-ments are of little diagnostic value in these cases. If neu-ropathy is also present, the patient feels no pain and this“warning signal” is also missing.
In patients with latent heart failure, the sudden increasein venous return induced by the compression can causeright heart decompensation.
Finally, a compression bandage is almost ineffective ifulcers that have been present on the ankle for decadesand frequent relapses have resulted in stiffening due todermatofibrosis.
The bandaging materialsIn compression bandage treatment, different clinical situ-ations require the use of bandage material with differingforce-stretch behaviour which may be described as theratio between working pressure and resting pressure.
The working pressure results from the resistance present-ed by the bandage to the expansion of the muscles dur-ing muscle contraction. This pressure is always measuredon the extremity while it is moving and is higher the lessthe bandage material can be stretched.
The resting pressure essentially corresponds to the appli-cation pressure, i.e. the force used to stretch the bandagewhen it is applied, but is also influenced by the individualrestoring force of a bandage. Restoring force is the ten-dency of elastic material to slowly contract when relievedof loading. The resting pressure is therefore measured onthe unmoved extremity. It is lower, the less stretchablethe bandage material.

Compression therapy [66.67]
Of all the compression bandages,the semi-rigid, unyielding zincpaste bandage provides thegreatest decongestion of deepvenous regions. Two-way-stretchbandaging materials, such as theVarolast zinc paste bandage, alsoallow less experienced persons toapply effective zinc paste band-ages.
py has to be interrupted during physical rest, especially atnight. On removing a bandage of this type, moreover, theblood shoots into the vessels from which the pressure hasbeen relieved and severe itching develops which is notonly unpleasant but also undesirable in view of thepatient's tendency to eczema.
Based on the criteria described, the materials availablefor bandage therapy can be divided into ▪ rigid zinc paste bandages exerting the highest working
pressure and lowest resting pressure; ▪ relatively inelastic, low-stretch bandages with high
working pressure and low resting pressure;▪ readily elastic, long-stretch bandages exerting relatively
low working pressure and high resting pressure. For thereasons already described, however, long-stretch band-ages are not suitable for the acute phase of treatment, although they are extremely popular because of their good adaptability. The actual domain of long-stretch bandages is functional bandages applied to produce a supporting or relieving function.
As regards application techniques, a distinction is madebetween permanent bandages which remain in place forprolonged periods, and temporary bandages.
The stage of treatment also has to be considered whenselecting which compression methods to use. In the acutephase, a compression bandage consisting of zinc paste orlow-stretch bandages is always used, since they canrespond more effectively to the variations in leg circum-ference. If the leg is permanently decongested and theulcer has fully healed, however, continuation treatmentcan be carried out using individually fitted compressionstockings.
The suitability of a compression bandage for a given ther-apeutic indication therefore depends on what ratiobetween working pressure and resting pressure can beachieved with the bandage.
Material which generates a high working pressure and alow resting pressure is most effective in supporting themechanism of the muscle vein pump. Due to the rhythmicalternation of very high and low compression pressure,the pressure peaks occurring during muscular contractionexert an effect extending deep inside the tissue, whileduring muscle relaxation the nutritive vascular regions ofthe terminal vessels are relieved and aerated.
Bandages with a relatively low working and a high rest-ing pressure, on the other hand, subject the blood vesselsto constant, permanent pressure, and the effect is con-fined to the superficial regions. The aeration effect is lost.Under resting conditions, compression techniques aretherefore tolerated better the lower the resting pressure.If the resting pressure is too high, the compression thera-
With low-stretch bandages, the difference in force ∆K is character-ized by the steep increase in the curve with a given stretch differ-ence ∆D. The pronounced amplitude is typical of a low-stretchbandage with its high working and low resting pressure.
Kraft
∆D
∆K
K2
K1
Dehnung % Kraft
∆D
∆K
Schematic diagram of the force-stretch behaviour of low-stretch band-ages during muscle activity: K1 is the application pressure of thebandage on the unmoved extremity (resting pressure), K2 the forceopposed by the bandage to the expansion of the muscle during mus-cle contraction (working pressure).

Compression therapy [68.69]
The high working pressure oflow-stretch bandages is still suffi-cient to therapeutically influence the deep venous regions,although they do not offer thehigh efficiency of zinc pastebandages. Their particular advan-tage, however, is that they adaptbetter to changes in leg circum-ference and are easier to changeif daily wound treatment isrequired.
It should always be remembered that the compressionbandage – regardless of the material and applicationtechnique – can only be fully effective when the patient isengaged in physical movement. It is also important tonote that only one type of bandage should be used atonce; for example low- and long-stretch bandages shouldnever be combined in a single layer.
Zinc paste bandagesAfter application, zinc paste bandages produce semi-rigid, unyielding bandages. Because of their non-elasticnature, among all the bandaging materials these are theones which can offer the greatest resistance to the work-ing muscles and exert a working pressure so intense thatit extends deep into the subfascial regions and rapidlyreduces swelling. The correspondingly low resting pres-sure assures a good aeration effect, so that blood circula-tion in the nutritive vessels is promoted, especially duringstagnation due to lacking withdrawal of blood by thedeep veins.
The zinc paste bandage is therefore indispensable for rap-idly reducing the leg swelling and removing stubbornedema especially on the back of the foot which resisttreatment with temporary low-stretch bandages or per-manent plaster bandages. Since the bandage cannotadapt to changes in leg circumference after the edemahas subsided, however, it has to be changed frequently inthis first phase of therapy.
Local ulcer care during the cleansing phase presentssome difficulties. A daily change of bandage is oftenrequired, and is more easily accomplished by using tem-porary, low-stretch bandages. If appropriate, however,rapid decongestion with the zinc paste bandage mayhave to be attempted; wound cleansing can then be com-menced.
The zinc paste bandage can be indicated as a substitutefor temporary bandages if the bandage is liable to manip-ulation or if dressing change on schedule is not alwayspossible.
Low-stretch bandagesLow-stretch bandages are characterized by relatively lowstretch, which causes the bandage to exert high compres-sion with a high working pressure and low resting pres-sure. Since these pressure conditions are still sufficient toinfluence the deeper regions, the mode of action of suchbandages corresponds to that of zinc paste bandages,although they do not have their high efficiency. On theother hand, low-stretch bandages have the advantagecompared to zinc paste bandages that they adapt betterto changes in leg circumference. When a good applica-tion technique is used, this means that they can be left inplace for about three days, except in the acute, highlyedematous stage.
Low-stretch bandages are suitable for all forms of chronicvenous insufficiency and are the treatment of first choicefor initiating or continuing treatment until the ulcer iscompletely decongested and epithelised.
Low-stretch bandages are available in a range of versionsmade possible by textile technology. Their stretch canrange from about 50 % to a maximum 90 % to achievethe required high working pressure and low resting pres-sure. The type of yarns used and the design determinethe typical use characteristics.
If bandages derive their elasticity from over-twisted, i.e.highly plied cotton chain-link threads, they are known astextile elastic. The best known and most commonly usedbandage of this type is the classical “Ideal” type band-age, textile elastic bandage, but the Pütter bandage is

Compression therapy [70.71]
These rules must be followed iftreatment is to be successful:1) Compression treatment canonly be effective if the correctpressure gradient is applied. Thepressure is highest at the ankleand decreases continuouslytowards the knee.2) The bandage must be heldproperly in the hand ...3) ... because only in this way can it be unwound on the leg. Ifthe roll of bandage is lifted fromthe skin, it cannot be guidedproperly, constrictions inevitablydevelop and the continuous pres-sure distribution is jeopardised.Too weak compression at theankle and strong compressionaround the calf, however, con-gests even more than a stockinggarter. 4) To apply the bandage, theankle should be held at a rightangle.
For correct bandage application,the bandage must always unrolldirectly on the skin and may onlybe pulled tight in the direction ofrunning.
also textile elastic and is made from a somewhat strongerfabric resembling the “Ideal” type bandage.
Bandages are classified as permanently elastic if theyderive their elasticity from fully synthetic chain-linkthreads. Crimped polyamides are mainly used for this pur-pose, and their degree of elasticity can be made suitablylow by texturising in order to meet the physical require-ments of a low-stretch bandage.
General principles of bandaging techniqueCompression therapy with bandages supports the jointmuscle pump, but only reaches its full effectiveness incombination with active movement. Consequently, thistreatment should usually be carried out on an outpatientbasis. Bed rest should also be avoided. Prolonged sitting,however, is even more unfavourable than lying. The fol-lowing principles should be observed when applying thebandage:▪ A good bandage should firmly enclose the leg all round,▪ be applied with a pressure gradient decreasing continu-
ously from proximal to distal▪ and not press or pinch at any point.
Every bandage that meets these requirements is correctand beneficial regardless of the technique used. A guid-ing principle is that the bandage should adapt to the leg,and not the leg to the bandage. This is only achieved,however, if both edges of the bandage are always ten-sioned with equal force and the bandage is closelymoulded onto the leg. To achieve this, the bandage mustalways unroll directly on the skin of the lower leg andshould only be pulled tight in the direction of application.The gaps that are initially left open should be closedlater.
Depending on the circumference of the leg, bandageswith a width of 8 cm or 10 cm are most suitable. The
bandage should be held in the hand such that the rolled-up part of the bandage is uppermost and faces outwards.Only in this way can it be unrolled on the leg. If, on theother hand, the roll of bandage is lifted off the skin, itcannot be guided properly, strangulating constrictionscan form and the correct pressure gradient decreasingfrom proximal to distal will be jeopardised.
To apply the bandage, the ankle is placed at a right angleand the lower leg is flexed at about 90°. Application ofthe compression bandage begins at the metatarsopha-langeal joints, taking care to include the heel. The skin ofthe toes becomes slightly cyanotic during this procedure.During walking, however, it becomes anaemic with everystep only to fill with blood again when relieved. Thepump action of the bandage can thus be observed direct-ly at this site.
The pressure exerted by a bandage is higher the greaterits curvature. Bony prominences (ankles) or edges overthe shin bone and the Achilles tendon should be padded
1 2
3 4
right
wrong
90˚
90˚

1
Compression therapy [72.73]
1) The heel is bandaged with theankle joint in mid position at 90°.2) To increase the local pressure,recesses and hollows should befilled with firm padding elements.
at the sides to compensate the greater prominence at thissite and reduce the local compression. Conversely, thelocal compression can be intensified if the curvature isincreased by incorporating rigid padding. Hollow areaslike Bisgaard's region should not merely be loosely filled,but padded out with firm support elements so that thebandage can be applied over them with a slight promi-nence. The effect of the compression bandage should beincreased over the ulcer itself by using pads whichmarkedly overlap the ulcer margins.
To prevent the bandage chafing in the hollow of theknee, it should end about two finger breadths below thehollow of the knee. For this reason, the lower leg shouldalso be flexed at a right angle when applying the band-age. It may be useful additionally to protect the hollow ofthe knee with soft, air-permeable padding material.
Bandages generally hold better if a second bandage isapplied in the opposite direction and crossing over thefirst one, resembling the Pütter crossover bandaging tech-nique.
A properly applied bandage gives the patient the feelingof having a firm support and is perceived as agreeable.Pain subsides. If pain worsens or if new pain develops
which does not disappear on walking, the bandage mustbe removed immediately. Every bandaging technique canbe taught and learned.
Each practitioner will gather their own experience andintroduce modifications into their individual bandagingtechnique.
2

Compression therapy [74.75]
Low-stretch bandage
The bandaging technique illus-trated here is a modified Pütterbandage consisting of two low-stretch bandages applied in thecounter-rotating technique. Thistechnique ensures high strengthand better durability of the band-age. 1 2
3 4
5 6
7 8
9 10
11
The first turn of bandage begins at the metatarsophalangeal joints,moving from inside outwards (1). The foot is held at a right angle.
After 2-3 circular or “ear of corn” turns around the midfoot, the next turn encloses the heel and runs over the medial malleolus andback to the instep (2).
Two further turns are applied to additionally fix the edges of the firstturn. The bandage first runs over the upper edge around the ankle (3)and then over the lower edge into the arch of the foot (4).
After a further circular turn over the midfoot, the bandage is takenover the ankle flexure back to the ankle (5), where following the con-tour of the leg it encloses the calf in steep turns (6).
The bandage runs from the hollow of the knee over the fibula headand back to the calf and then, following the contour of the leg, isagain taken downwards (7) to close the gaps in the bandage.
The second bandage is applied in the opposite direction from outsideto inside on the ankle (8) and its first turn runs over the heel back tothe dorsum of foot.
Two further turns fix the upper (9) and then the lower edge of the heelturn.
The bandage is then taken once again over the midfoot and then, inthe same manner as the first one, steeply upwards (1) and then backagain. The finished bandage (11) is secured with clips.

Compression therapy [76.77]
Bandage made from Varolast zincpaste bandages
An opposing bandaging tech-nique is not necessary for any ofthe zinc paste bandages becausethe fixation by the zinc pastemass provides the necessarystrength and permanency of thebandage.
For bandages made from thetwo-way-elastic Varolast zincpaste bandage, in contrast toconventional zinc paste bandagescontinuous bandaging is possible.Cutting of bandages to shape isunnecessary. The two-dimensionalstretch of the Varolast is onlypresent during application.
Alternative bandaging techniqueto increase the durability of thebandage on the foot.
1 2
3 4
The zinc paste bandage begins in the same manner as described onthe previous pages from inside to outside (1).
After the corresponding turns around the midfoot, the bandage shouldbe reinforced by repeating the turns around the heel (2) because asecond bandage is not applied in the opposite direction.
The bandage is then taken around the lower leg as for the low-stretchbandages already described (3).
Finally, the Varolast zinc paste bandage is covered with a Stülpa tubu-lar bandage for protection (4).
1 2
3 4
5 6
This technique begins with a circular fixation turn on the ankle running from inside to outside, then the bandage is taken across theinside of the heel to the hollow of the foot (1).
It encloses the midfoot (2), runs across the instep to the Achilles ten-don (3) and over the lateral malleolus like the one to the sole of thefoot (4). After lifting the arch of the foot, the bandage rolls, if a cross-wise bandage is to be applied, in steep turns upwards. If a zinc pastebandage is applied using only one bandage, however, the additionalheel and fixation turns described on page 74 are to be executed in theankle region (5).
All further turns are executed as described on page 74 and 75 (6).

Compression therapy [78.79]
Bandages for compression therapy
Varolasttwo-way elastic zinc paste bandages, ready to use: thetwo-dimensional deformability of the connective tissuealso allows the bandage to be applied exactly withoutslitting and cutting at anatomically difficult transitionalregions, which improves the continuous pressure gradientfrom proximal to distal; well tolerated by the skin andquick-drying.
Lastobindpermanently elastic, low-stretch bandages, elasticityabout 50 %; very high, intense working pressure with lowresting pressure; particularly suitable for permanentbandages – the working pressure also remains therapeu-tically effective during protracted use; aging resistant,washable up to 60°; skin-tone. Lastobind is also availableas Lastobind-Duo in a double economy pack with 8 cmand 10 cm width bandages; especially suitable for theSigg bandaging technique.
Pütter bandagevery strong, textile elastic low-stretch “Ideal” type band-ages, elasticity about 90 %; high working pressure withlow resting pressure; a sustained compression effect alsowhen used for permanent bandages, boiling and steriliza-tion proof; skin tone. The Pütter bandage is available inthe form of two 10 cm width bandages for the classicalreverse bandaging technique for compression therapy ofvenous disorders of the leg.
Lastocomplow-stretch foam rubber bandages laminated with “Ideal”type bandage fabric, elasticity about. 60 %, 3 mm thick;good massage effect on superficial venous blood flow;suitable as supplementary compression dressing on thethigh; breathable and well tolerated by the skin; particu-
larly hard-wearing due to the lamination; hand washable;skin-tone.
HARTMANN “Ideal” type bandagesclassical, textile elastic low-stretch bandages, loop-edgedaccording to E DIN 61632-IB, elasticity 90 %; high work-ing pressure with low resting pressure, can also be wornat rest; boiling and sterilization proof; the elasticity of thebandages, which decreases with wearing, can be restoredby washing.
Idealhaftcohesive, textile elastic low-stretch bandages, elasticityabout 60 %; latex microdot coating on both sides fornon-slip fit; very high working pressure with low restingpressure, can also be worn at rest; breathable; handwashable for multiple use, skin-tone.
Hypolasticelastic, hypoallergenic low-stretch plaster bandages, elas-ticity about 60 %, very high working pressure with lowresting pressure; non-slip and non-displaceable due tovery good adhesive strength, the stability of the bandageis preserved even during prolonged wear, well toleratedby the skin due to hypoallergenic polyacrylate adhesive,can be applied without skin protection and removes pain-lessly; especially suitable for patients with pre-damagedskin; thermostable, sterilization-proof.
Stülpaseamless knitted tubular bandage with high two-way-stretch; easy to apply without additional fixation; non-crease fit; used as a protective cover for zinc paste band-ages, prevents soiling of underwear by the adhesive con-sistency of the zinc paste during the drying phase.

Compression therapy [80.81]
The VitaSan medical compressionstockings offer quality in thedetails:1) Hidden seam at the front atthe toes and integrated alternat-ing heel for crease-free fit2) Below-knee stocking with non-slip fit and seamless transition tothe soft waistband to reducepressure points3) Thigh length stocking with sili-cone-coated, unobtrusive adhe-sion strip or fashionable laceband, perfect fit 4) Panty hose with perfect fit,comfortable panty section, non-ladder due to Micro-Mesh knit.
Medical compression and support stockings formaintenance therapyMedical compression hosiery with the following compres-sion behaviour is recommended for continuation treat-ment after acute therapy: Depending on the compressionclass, the resting pressure is low to high, while the work-ing pressure depends on the elasticity of the material. Thecompression force in the ankle region is the criterion forassignment to the different compression classes. InGermany, compression classes I to IV have been estab-lished by the Quality Seal Association (GZG). Since thecompression values, especially in the higher compressionclasses, reach the compression levels achieved with com-pression bandages, medical compression stockings arenow used not only for prophylaxis and follow-up care,but also as an alternative for certain basic treatments(see table on pages 82-83).
VitaSan – medical compression stockingsVitaSan compression stockings satisfy both therapeuticrequirements and patients‘ wish for wearing comfort andfashionable styling. These medical stockings are availablein compression classes I to III so that the correct com-pression values can always be applied to suit the specifictherapeutic requirements.
Made-to-measure versions are naturally also available.Optimal comfort is assured by the type of yarns used, e.g.special microfibres, but also the type of fabrication, asshown by the illustrations. The high in-use comfortundoubtedly enhances compliance, a factor which cannotfail to provide benefits for physicians and patients.
VitoFit – support stockingsTo complete the broad range of products for compressiontherapy, support stockings should also be mentioned.VitoFit support stockings from HARTMANN, with theiranatomically correct compression gradient provide aselectively dosed support effect decreasing from the ankleto the thigh. Tired and heavy legs are relieved and theblood circulation is stimulated. VitoFit support stockingscome in three strengths and up to eleven attractivecolours as below-knee stockings, thigh length stockingsor as panty hose.
1 2
3 4

Selected compression bandages and compression stockings and their use
Description
Compression class II:23-32 mmHg, medium superficial effect
milder varicosis with superficial edema, venous insufficiency due to varicosis, after healing of minor ulcerations, after superficial thrombophlebitis, after sclerotherapy, after stripping, for relatively severe varicosis of pregnancy, for thrombosis prophylaxis
permanently elastic low-stretch bandage; very high, intense working pressure with low resting pressure, working pressure remains effective even during prolonged wear
two specially strong, textile elastic low-stretch “Ideal” type bandages; high working pressure with low resting pressure, compression remains effective even after prolonged wear
cohesive, textile elastic low-stretch bandage adhesive effect on both sides for non-slip fit, very high working pressure with low resting pressure, can also be worn at rest, breathable
medical compression stockings made of different knitted fabrics: from coarse to fine-mesh, in compression classes I to III, satisfy the requirements of the Medical Devices Act, CE-marking and Quality Seal of the German Quality Association of Medical Compression Hosiery awarded the prize “TKO-Tex-Standard 100”
Two-way elastic zinc paste bandage for easier application withoutcutting, elasticity only present during application operation;intense working pressure extending into the deep veins
extensibility working and resting pressure
approx. 50 %+++ / +
approx. 90 %+++ / +
approx. 60 %++ / +
Compression class I:18-21 mmHg, light superficial effect
none+++ / +
Uses
temporary bandage for ulcer treatment, for all acute and chronic stasis edemas, after sclerotherapy of varicose veins, for throm-bophlebitis
temporary bandage for ulcer treatment, for all acute and chronic stasis edemas, after sclerotherapy of varicose veins, for throm-bophlebitis
bandage of good durability for chronic venous stasis ulcerations, for after-treatment of healed ulcerations
feeling of heaviness and tiredness in the legs, mild varicosis with out pronounced edema tendency, incipient varicosis of pregnancy
Compression class III*:34-46 mmHg, surface and depth effect
severe varicosis with edema, CVI secondary to postthrombotic syndrome, post-traumatic edema, following healed venous leg ulcer, after sclerotherapy, after stripping
for rapid decongestion and mobilization of stubborn edemas,permanent bandage for ulcerations in the non-exuding stage
Varolast
Lastobind
Pütter dressing/Pütter bandage
Idealhaft
VitaSan classic, sateen finish and fine, thigh-length stocking and panty hose
Compression therapy [82.83]
* only VitaSan classic

Glossary and index of key terms [84.85]
A
Acral � relating to the body and limbs (acra = extreme ends of thebody, e.g. fingers, toe digits)
Ankyloses � joint stiffness (boneadhesions) due to disease process-es inside the joints, e.g. in chronicpolyarthritis
Arterial status, recording of �19
Atrauman Ag (silver containingointment dressing � 56
B
Bandaging techniques � 74
C
Causal � originating
Causes � 6 f
Chronic venous insufficiency (CVI) � 11
Chronic wound � 34
Cleansing by moist wound treat-ment � 38
Clinical presentation and diagnosis� 16 f
Compensate � make up for (a weakness or dysfunction)
Complaints � 18
Compression bandage � applica-tion technique � 70
Compression bandage � bandag-ing material � 65
Compression bandage � 25
Compression bandage, mode ofaction � 63
Compression bandages -Hypolastic � 79
Compression bandages - Idealhaft � 79
Compression bandages -Lastobind � 78
Compression bandages -Lastocomp � 78
Compression bandages - Pütter bandage � 78
Compression bandages - Varolast � 78
Compression bandages - HARTMANN “Ideal” type bandages � 79
Compression stockings VitaSan � 80
Contraction � drawing togetherof an object, med.: e.g. contrac-tion, active tensing of muscles
Cutis � lat. skin, consisting of theepidermis (upper skin) and dermis(corium)
D
Decompensation � the derange-ment/failure of the body’s naturalcompensatory mechanisms inresponse to functional disorders
Differential diagnostic clarification� 20
Dilatation � widening/distentionof hollow organs or blood vesselsby pathological processes, orinstrumental for diagnostic-thera-peutic purposes
Disorders of wound healing � 28
M
Media sclerosis � calcium deposits in the middle layer(media) of the vessel wall of thelarge arteries, e.g. frequently indiabetes mellitus
Medical history � systematic (patient) interview � 17
Medicinal therapy � 28
Moist wound management � 35
Multimorbidity � simultaneouspresence of several diseases inone patient
O
Obliteration, obliterating � clo-sure of the lumen of a body cavi-ty, congenital, acquired throughinflammatory processes or surgi-cal, e.g. in vein ablation
Option � possibility to choose
Orthopaedic abnormalities � 19
Overt � evident, clear, med.: themanifestation of a disease by thecorresponding symptoms
P
Pain therapy � 30
Paratibial fasciotomy � 27
Pathophysiology � compositeterm from pathology = science ofdisease-related changes in thebody and physiology = science of the function of the body
Perforator ligation � 27
Peri � around something
Peri-ulcer area, state � 18
Peri-ulcer eczema � in the areaaround the ulcer � 41
Perivasular � in the area aroundblood and lymph vessels
PermaFoam � (hydroactice foamdressing) � 50
Polypragmasy � uncritical tryingout or use of numerous medica-tions and methods of treatmentin the same patient
Postthrombotic syndrome � 14
Predisposition � special tenden-cy/susceptibility, inherited oracquired, to develop certain dis-eases
Prognosis � reasoned forecastthat under certain conditions cer-tain events will occur, med.: pre-diction of the probable courseand outcome of a disease
Proliferation � increase in tissuedue to abnormal growth result-ing from inflammatory processes,e.g. following the inflammatoryphase of wound healing
Proximal � located closer to thecentre of the body
Pütter bandage � 74
R
Relapsing � occurring repeatedly,med.: recurrence of a disease afterit has healed
Relaxation � relief of tension,physiol.: relaxation of contractiletissue after active tensioning
Retention � holding back
S
Sclerotherapy � 26
Site of predilection � parts of thebody preferentially affected by acertain disease process
Sorbalgon (calcium alginate dress-ings with packing ability) � 49
Stülpa (seamless knitted tubularbandage) � 79
Subcutis � underskin, consistingof fatty tissue, next to leather skin(dermis)
Sufficient � adequate, enough(opposite: insufficient)
Support stockings � VitoFit � 81
Surgical debridement of necroticmaterial � 38
T
TenderWet (wound pad withsuper absorber) � 44
Therapy � 24 ff
Therapy-refractory � a diseaseno longer responds to the (usual)treatments
Therapy-refractory ulcers � 43
U
Ulcer localization � 17
V
Valve agenesia � Agenisia = lack-ing formation or development of apart of the body, congenital, here:
Glossary and index of key terms
Distal � far from the body, fur-ther away from the middle of thebody
Diuretics � substances that stim-ulate the excretion of urine � 38
E
Edema formation � 18
Edema-protective agents � 28
G
General status, recording of � 20
H
Hemodynamics � Science of themovement of blood flow in thevessels and the forces responsible
Hydrocoll (absorbent hydrocolloiddressing) � 53
Hydrosorb (transparent Hydrogeldressing) � 55
Hypertension � high blood pres-sure
I
Infection prophylaxis and control� 39
Insufficiency � inadequate function or performance of anorgan or organ system
Invasive therapeutic procedures� 26
L
Low-stretch bandage � 69

References and index of illustrations [86.87]
absence of venous valves
Varicosis � 12
Venotonicising drugs � 28
Venous insufficiency, chronic� 11
Venous insufficiency, subfascial � 14
Venous insufficiency, suprafascial� 12
Venous return � 9
Venous status, recording of� 19
W
Wound floor, nature � 18
Wound healing phases � 33
Wound management � 32 f
Wound management, cleansingphase � 37
Wound management, epithelisa-tion phase � 42
Wound management, granulationphase � 40
Z
Zinc paste bandage � 68
Zinc paste dressing � 76
Altenkämper, H., Felix, W., Gericke, A., Gerlach H.-E.,Hartmann, M.:Phlebologie für die Praxis,Walter de Gruyter, Berlin / New York, 1991
Galli, K.-H., Wolf, H., Paul, E.:Therapie des Ulcus cruris venosum unter Berücksichtigungneuerer pathologischer Gesichtspunkte,in: Phlebologie 1992; 21: 183-7
Gaylarde, P. et al:The effect of compression on venous stasis,British Journal of Dermatology, 1993; 128, 3, 255-258
Gericke, A.: Die Behandlung des Ulcus cruris venosum,in WundForum 1/98
Lohfink, H.-D.:Konservative Phlebologie,F.K. Schattauer Verlagsgesellschaft mbH, Stuttgart, 1997
Moffat, C.:Compression bandaging – the state of art.Journal of Wound Care, 1992, 1, 1, 45-50
Moffat, C., Harper, P.:Leg Ulcers (ACE) series, 1997, Edinburgh:Churchill Livingtone
Morison, M. et al.:Nursing Management of Chronic Wounds, 1988,London: C.V. Mosby
Niedner, R., Vanscheidt, W.: Ulcus cruris in: Sedlarik, K. M. (Hrsg.):
References

CNRI / SPL / Focus (S. 1, 6)Fermariello, M. / SPL / Focus (S. 16)King-Holmes, J. / SPL / Focus (S. 19)Kowollik, B (S. 47)Lange, N. / Okapia (S. 20)Lippert, H. (S. 39)Looks, A. (S. 17)Meckes, O. / Eye of Science / Focus (S. 8)Schepler, H. (S. 42)Tautenhahn, J. (S. 17, 21, 22)Vanscheidt, W. (S. 12, 18, 22, 26, 27, 38)Winter, H. (S. 22, 48)Zimmermann, M. (S. 52)
All other illustrations from the archive of PAUL HARTMANN AG
List of illustrations
Wundheilung,Gustav Fischer Verlag, Jena / Stuttgart, 1993
Sedlarik, K. M. (Hrsg.):Wundheilung,Gustav Fischer Verlag, Jena / Stuttgart, 1993
Venöse Beinleidenpharmdidakt, Band 2/80,pmi-pharm & medical inform. Verlags-GmbH, Frankfurt

PAUL HARTMANN Pty. Ltd.Homebush NSW 2140Australia
PAUL HARTMANN Egypt S.A.E.Giza/Cairo 12515 Egypt
PAUL HARTMANN AG89522 HeidenheimGermany
PAUL HARTMANN Ltd. Heywood/LancashireOL10 2TTGreat Britain
PAUL HARTMANN Hellas A.E.16675 Glyfada/AthinaGreece
PAUL HARTMANN Asia-Pacific Ltd. Kowloon Bay, KowloonHong Kong – China
HARTMANN-RICO Hungária Kft.2051 BiatorbágyHungary
HARTMANN-Vitamed(Pty) Ltd.Sandton 2128Republic of South Africa
PAUL HARTMANN Pte. Ltd. Singapore 609143
The HARTMANN medical editionseries of publications is devotedto current topics in medicine andnursing. The aim is not only toprovide basic knowledge, but alsoto profile medical and interdisci-plinary developments with specialemphasis on general productinformation.
In a time of rapid scientificadvancement, information mustabove all be up to date. In meet-ing this aspiration, this series ofbooks is designed to provideguidance not only for experiencedspecialists, but to all those newlyventuring into medicine and nurs-ing. Current therapeutic optionsare described and useful tips pro-vided.
ISBN 3-929870-47-9 B 33
VA/
E (0
506)
087
496
/1