Why Are In Vitro Platelet Characteristics Not Predicting ... · Why Are In Vitro Platelet...
Transcript of Why Are In Vitro Platelet Characteristics Not Predicting ... · Why Are In Vitro Platelet...

Why Are In Vitro Platelet Characteristics Not Predicting Clinical Outcomes?
Acknowledgments: We would like to thank the staff at the Transfusion Services at Vancouver General Hospital, Vancouver, Canada, for their help in carrying out this study.
• An in vitro assay that predicts in vivo outcome has long been thought to be the "Holy Grail" in transfusion medicine.
• Assays such as morphology score (m_score) by microscopy are not practical for routine use in hospitals to determine platelet (PLT) activation status.
• Flow cytometric assessment of P-selectin (CD62) expression is normalized which eliminates donor variability.
• Microparticle content (MP%) of single donor PLTs (SDP) indicates PLT activation status (the sum effect of donor, processing, and post-processing).
• Clinical validation of an association between high MP% and poor outcome of prophylactic transfusions is in progress.
Background
1LightIntegra Technology Inc, 2Canadian Blood Services, 3University of British Columbia, Vancouver, Canada.
MP content and morphology scores of platelet transfusions were compared with clinical outcomes to reveal the challenges and inform future studies.
Objective
• The Canadian CoDIVO study (ISRCTN01292427 ) conducted at the Vancouver General Hospital from 2011 to 2014 enrolled 200 hematology/oncology patients.
• Pre- and post-transfusion PLT counts and characteristics of SDP were prospectively collected.
• Patients were 56% male, 51 ± 13 years of age, 65% diagnosed with ALL/AML, 40% CMV+, 10.5% positive for anti-HLA antibodies, baseline PLT counts 57 ± 53 x 109/L, WHO bleeding >1 was rare.
• PLT activation status in SDP (N = 63) was measured as (1) MP% by dynamic light scattering (ThromboLUX, LightIntegra Technology Inc., Canada) and (2) m_score using phase contrast microscopy (Nikon, Japan, 100x).
• MP% of SDP suspended in plasma was compared to their m_score and clinical response measured as 1-hr and 24-hr corrected count increments (CCIs).
• MP% and CD62 expression (FACSCanto II, BD Biosciences) were compared for SDP stored for 14 days.
Methods
• In contrast to relative quality control parameters such as CD62 expression, MP% and m_score reflect the entire history of PLT units, including donor variability (Figure 2).
• Current production, storage, and shipping of PLT units aims to minimize activation but does not address the contribution of donors.
• Activated PLT transfusions with MP% > 15% or a low morphology score have a high probability of insufficient increase in 24hr CCI in CMV+ AML patients.
• Minimizing activated PLT transfusions for prophylaxis may be a practical approach to improving overall clinical outcomes.
Conclusions
Elisabeth Maurer-Spurej1,2,3
B C
Figure 2. MP content (%) correlates with CD62 expression in individual SDP. Each of 6 SDP was tested on days 1, 4, 6 and 14 of storage. PLTs that are more activated from the donor are more vulnerable to additional stress such as extended storage. Average correlation of MP% and CD62% for individual SDP was high (r = 0.991, P=.01).
Results
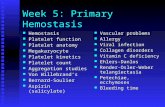
Figure 1. Correlation between two in vitro markers of PLT activation status, MP% and morphology score (m_score). (A) For activated PLTs (N=31), MP% and morphology scores of SDP showed a moderate inverse correlation (r =- 0.561, P=.001). (B, C) Phase contrast micrographs of fixed non-activated (8% MP, m_score = 270) and activated platelets (30% MP, m_score = 229).
• All patients received a total of 997 transfusions of which 328 were SDP. • MP content (MP%) and morphology score (m_score) of activated platelets show a
moderate correlation; non-activated platelets are difficult to differentiate by visual inspection (Figure 1).
• Activation status of SDP measured as MP% showed a moderate correlation with 24-hr CCIs in CMV+ patients diagnosed with AML (R2 = 0.304, P = 0.018) when confounding factors were excluded (major ABO mismatch, multiple transfusions in 24 hrs, patient testing positive for anti-HLA antibodies, patient older than 60 years; N = 54).
AB
C