Ward Rounds - cdn.i3l.ac.id
Transcript of Ward Rounds - cdn.i3l.ac.id
Session Learning Objectives
• At the end of the session, the student should be able to:– Elaborate services given during ward visit,– identify importance of medication-use
evaluation, –elaborate steps to do medication-use
evaluation and the follow-up action
Course Outline
• Definition• Benefit of ward round• Role and main duties of ward pharmacis• Stages of ward round• Involvement of health care professionals in
ward round• Evaluation of ward pharmacist• Medication-use evaluation
Introduction
• In our context, pharmacist observe the patient's clinical condition directly, and examine drug-related problems, monitor drug therapy and unwanted drug reactions, improve rational drug therapy
• Pharmacists who focuses on doing ward round à ward pharmacist• Ward round can be done:
– Independently– Active collaboration with physician & other professional health care in the
process of establishing a decision related to drug therapy
A ward round is a visit made by a medical practitioner, alone or with a team of health professionals and medical
students to in-patients at their bed side to review and follow up the progress in their health
Benefits of Ward Round
• Humanistic aspects – Improvement of patient's quality of life, patient
satisfaction
• Clinical aspects– Improvement of clinical signs, decrease in incidence,
unwanted drug reactions, decreased morbidity and mortality, reduction in length of stay
• Economical aspects– Reduced drug costs and whole medical costs
Benefits of Ward Round
• According to research done by Klopotowska et al., 2010, Nederland – Participation of pharmacist in ward rounds on ICU
resulted in 659 recommendation from 1173 prescription with level of acceptance from physicians is 74%
– Able to reduced prescription error significantly – There is a cost reduction about 26-40 euro
Scope of Activities• Visit to patients in the ward that is done by pharmacist,
consist of: – Identification of the DRP– Recommendations of solution/ DRP prevention– Monitoring the implementation of recommendations and
therapeutic outcomes of the patient• Must communicate effectively to patients/families, doctors
and other health professions• Actively involved in the decision of drug therapy to achieve
optimal clinical outcome• Documentation of all actions taken as professional
responsibility, as educational and research material, and improving the quality of professional practice
Role of Ward Pharmacist
• Encourage the effectiveness and safety of patient’s treatment
• Implement dispensing based on legality and standards of profession
• Establish a good work team by respecting the ethic code of each profession and the confidentiality principle
• Carry out education and training in order to fulfill the standard professional competencies
• Actively involved in drug research
Main Duties of Ward Pharmacist
Resolve DRPEnsure
appropriate dispensing
Education
ResearchActive
participation in team
Resolve DRP• Ensuring that the information related to drugprescription, medical records & other documents arecorrect and complete
• Ensure there are no prescribing errors throughprescription screening (administrative,pharmaceutical, clinical)
• Provide information, explanations, counseling,advice regarding the drug that is the most suitable forpatient to the doctor, nurse, patient / patient's family(care giver) or other health professionals
• Ensuring the accuracy of indications for drug use
Resolve DRP
• Actively perform drug use assessments• Perform independent ward rounds or in collaboration
with physicians or other health professions, and searchfor medication history à involved in the patient'sdrug treatment decision process
• Hold discussions with doctors, nurses and other healthprofessionals about the therapy in order to achievedefinite clinical outcome
• Perform active monitoring, documentation and reporting of medication’s side effects, including medical devices, cosmetics and herbs
Ensure Appropriate Dispensing
• Ensuring the sustainability of dosage regimen throughout the patient’s treatment
• Ensuring the correct compounding & dispensing, including: right patient, dose, dosage form, route, time, along with adequate information (oral and written)
• Ensuring the correct preparation of high alert medication
• Ensuring the reconstitution of sterile preparations is in line with aseptic technique while considering compatibility & solubility
Ensure Appropriate Dispensing
• Ensuring the correct use of special techniques (e.g use of inhalers, nasal spray, insulin injection)
• Ensuring the availability of emergency medication and medical devices so it always matches the stock prepared in a ward (if any)
• Ensuring that the medication are properly stored according to their requirements and legal aspects
• Ensuring the process of non-sterile preparations dispensing in the ward using standardized equipment while minimizing contaminants
Education
• Participation in educating pharmacy students, pharmacy technician, and other health professions
• Participation in the training process of pharmacists, pharmacy students, pharmacy technician, and other health professions
• Assisting health professionals who are not able and inexperienced in compounding
• Participation in continuing professional development
Preparation
• Pharmacist should be able to:– be familiar with various knowledge, such as
pathophysiology, medical terminology, pharmacokinetics, pharmacology, pharmacotherapy, pharmacoeconomics, pharmacoepidemiology, evidence based treatment
– interpretate laboratory data and other diagnostic supporting data
– Communicate effectively with patients and other health care professionals
Preparation
• Patient selection:– New patients (admitted within the first 24 hours)– Patients in intensive care– Patients receiving > 5 medications (polypharmacy)– Patients who have impaired organ function, especially
the liver and kidney– Patients whose laboratory results reach a critical value
(e.g electrolyte imbalance, decreased albumin levels)– Patients receiving medication with narrow therapeutic
index or potential adverse drug reaction
Preparation• Activities in the preparation stage:
– Information collection about medication use• Medical records• Interview with patient or family• Patient’s medication profile
– Assessment of DRP• Assess patient’s DRP (which one is “actual” and potential)
– Prepare a “quick reference” that will be taken during rounds:• Hospital formulary, antibiotics usage guidelines, guidelines for
diagnosis and therapy, list of universal health coverage medication, British National Formulary (BNF), Drug Information Handbook (DIH), American Hospital Formulary Services (AHFS): Drug Information, etc
– Bring calculator
ImplementationIndependent ward round Team ward round
Advantage a. Schedule is adjusted with other activities
b. Include counseling & monitoring drug response
c. As a preparation to do ward round with other health professionals
a. Gain up-to date & comprehensive information
b. Facilitate learningc. Communicate directly
regarding DRP and can directly implement the recommendation
Disadvantage a. Recommendation that is made can not be quickly implemented before informing the physician who prescribe the medication
b. Limited knowledge in patient’s pathophysiology
a. Schedule needs to be adjusted with others
b. Limited ward round time and informationprovided is less complete
Independent Ward Round Implementation
• Gain trust à open & cooperativeIntroduce yourself
• Communicate effectively to identify the “real problem” • Asses whether the patient’s complaints related to medication use•à Establish problem (actual/potential) & identify if there is a new
problem
Listen to the patient’s response & identify the problem
• Directed to increase compliance, how to use, special consideration à counseling, education, how to use special medication
• Recommendation also involves other professionals
Giving evidenced-based
recommendation related to DRP
Ward Round Implementation as a Team
• Introduction by head of ward round Introduction
• Physician in-charge will explain the clinical condition of the patients à update • Pharmacist should be actively participate in digging background related to DRP
Carefully follow the presented case
• Phamacist actively enganged in discussion to clarify, confirm & complete medication use information
• Recommendations are addressed to physician to improve therapeutic outcomes, specifically in the choice of drug therapy (e.g when injection of antibiotic is replaced to oral, appropriate duration use of antibiotics according to guideline)
Giving evidenced-based
recommendation related to DRP
Monitoring
• Monitor the implementation of the recommendation to patient, physican & nurse– Check through medical record & medication
administration record– If not followed, figure out why
• Monitor effectivity & safety related to medication use– SOAP
Documentation
Active Participation in Team
• During ward round, collaborate with physicians, nurses, and other health professions to ensure the safety, efficacy, benefit, and affordability of medication
• Collaborate with other team (palliative team, infection control team, etc) in the hospitals
Professions Involved
Patient
NursePhysician
Pharmacist Nutritionist
Other health care professionals
Medical care
pharmaceutical care Nutrition care
Nursing care
Other medical care
Interaction with Other Professional Health Care
• Understand the responsibility of each profession
• Use technical language• Focus on the problem• Evaluate problem from all aspects• Recommendation given needs to be based on
an up to date reference and trustable
Evaluation of Ward Pharmacist
• Part of ensuring the quality of pharmaceutical service
• Evaluation:– Assesment on medication plan of the patients– Assesment on medication administration
documentation– Frequency of discussion of patient-related clinical
problems including the plan to overcome the problem– Pharmacist recommendation in modifying the
medicine regimen
Medication-use Evaluation (MUE)
• A process to structurally ensure quality of medication use.
• Intended to continuously monitor and ensure the quality of medication used in a hospital
• Can be used as one of the indicator in patient care by healthcare professional
• NOT therapy drug monitoring
Goals & Objectives
• Ensure impact of drug therapy monitoring àpolicy or local guideline
• Quality assurance for drug use in a hospital (or country)– Ensure continuous quality improvement– Evaluation and monitoring of medication
management & use• Optimize patient therapy à improve quality,
safety, and cost-effectiveness
How MUE Achieve its goals?• facilitating multidisciplinary consensus on drug use• conducting regular evaluations to assess
appropriateness of drug use• providing feedback of results to prescribers and other
stakeholders (i.e healthcare profs and management);• promoting judicious, appropriate, safe and cost-
effective therapy through provision of information, advice and education;
• minimising variations in practice that contribute to suboptimal clinical outcomes;
• And enhancing opportunities to perform standardised assessment of the value of drug use practices.
Steps1. Identification of medication and medication use process for evaluation.2. Assembling the team.3. Design of the study.4. Approval of the study.5. Development of criteria and measurement instruments.6. Data collection.7. Evaluation with pre-determined criteria and analysis of results.8. Reporting and feedback.9. Design and implementation of intervention strategies.10. Reassessment and revision of problem.
1. Identification of medication and medication use process for evaluation• Target areas for evaluation may include individual drugs, drug classes, or
components of clinical procedures or disease state management. • MUE should be considered when new drugs are added to a formulary or
as part of drug usage guidelines evaluation (audits)• Certain drugs or events serve as indicators of potential problems in the
drug use process and may highlight potential target areas, including:– drugs known to be associated with adverse events– Drugs associated with poor patient outcomes– drugs used in high-risk patients– drugs with high-unit or high-volume cost (affect large number of patients or
frequently prescribed)– drugs or processes where suboptimal use is likely to have a negative effect on
patient outcomes or system cost– adverse medication events (actual or averted)– signs of treatment failure (e.g. bacterial resistance)– Drugs are most effective if used in a specific way– New indication
2. Assembling the Drug Use Evaluation Team
• Relevant experts should be recruited to assist with assessment of practice performance – Pharmacists– Prescribers– Quality officers– Nurses– Other experts
• There will usually be a need to include different team members for different studies, to ensure appropriate expertise– E.g: evaluation of antibiotic would need to include clinical
microbiologist
3. Design of the Study• The objectives and study method will be dependent on the
project• Can be quantitative or qualitative, or combine both elements. • Reviews may range in scope from routine screening activities
to expansive reviews of all aspects of drug therapy. • Can be conducted retrospectively, concurrently or
prospectively.• A decision on appropriate sampling methods should be made
prior to the study• The project design should be documented • The project design should be endorsed by the Pharmacy and
Therapeutics Committee or other authoritative committee.
Types of Study• Prospective
– Evaluating a patient's planned drug therapy before a medication is dispensed– allows for identification and resolution of problems before the patient has
received the medication• Concurrent
– Concurrent review is performed during treatment– involves the ongoing monitoring of drug therapy to ensure positive patient
outcomes. • Retrospective
– Most commonly used– The simplest to perform – Drug therapy is reviewed after the patient has received the medication. – May detect patterns in prescribing, dispensing, or administering drugs to
prevent recurrence of inappropriate use. – Patient medical charts or computerized records are screened to determine
whether the drug therapy met approved criteria
4. Approval of the Study
• Approval for access to patient data should be obtained from the institutional ethics committee where appropriate
• In some facilities blanket approval may be provided for all quality activities either by Ethics Committee or by Management
• Prior approval must be sought before access can be gained to patient medical records.
• All MUE must be mindful of ethical and privacy considerations.
5. Development of Criteria and Measurement Instrument
• Criteria must be valid, explicit, pre-determined, easily measured, relevant to the practice environment, and outcome oriented
• Where possible, criteria should be based on recognised standards
• Criteria should be explicitly agreed by the team with input from expert clinicians, prior to data collection.
6. Data Collection
• There should be data collection instrument that is unambiguous, simple, and focused to answer the specific question in the study
• Where possible, data collection should take advantage of existing automated information systems.
• Data collection instruments should be tested in pilot studies to ensure they are suitable for the purpose
• Confidentiality of data must be ensured.
7. Evaluation with Pre-determined Criteria and Analysis of Results
• Drug use will usually be compared with pre-determined criteria
• Criteria should be evidence-based and should be developed in consultation with expert clinical advice
• Criteria should be explicit, practical, relevant and measurable.
• Treatment courses not matching the audit criteria should be reviewed with clinicians to determine if there is valid clinical justification for divergence from criteria
8. Reporting and Feedback
• A mechanism should be developed for reporting and feedback of audit results to prescribers and other relevant stakeholders.
• Reporting can be to hospital management or certain committee/authorities– Study results and recommendations should be
reported in writing
• Wide and constructive feedback of positive and negative findings is fundamental to program
9. Design and Implementation of Intervention Strategies
• Should specifically targets findings of MUE • Effective and efficient, may employ various
methods• Approaches may include:– Formulary changes– procedure modifications– additional pharmacy services– publication of therapeutic guidelines – A variety of educational activities– Monitoring
10. Reassessment and Revision of Problem
• MUE is a cyclical process• Lessons learned from one cycle of study should
be incorporated into subsequent study cycles. • MUE projects need to be evaluate– Follow up of Intervention implementation à success
of intervention– Reassessment of areas or target groups – Periodic screening of one or more aspects of drug use
for which specific interventional activities were introduced
Pharmacist’s Role in MUE• Expert in drug à should play a leadership role • Roles and responsibilities include:
– Recommendation and promotion of the goals and objectives of MUE
– Program development, supervision and coordination– Education of hospital staff about the theory and practice of MUE– Coordination of development and/or review of audit criteria,
guidelines, study protocols and other– educational material– Coordination of development of data collection instruments,
field testing, data collection, analysis, development of recommendations for intervention, and report writing.
– Documentation of program outcome, effectiveness and cost benefit.
– Dissemination of program results
Common Parameters for MUEParameters
Right Dose
Right Route of Administration
Right frequency and duration
Right Indication
Drug Interaction
Duplication
Contraindication
ADR incidence
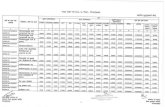
Method in Antibiotic Use Evaluation
Combination of:• Gyssens Algorithm– Qualitative Study
• ATC/DDD Method– Quantitative Study
ATC/DDD• ATC: Anatomical Therapeutic Chemical Classification System• DDD: Define daily dose
– Standards from WHO– assumed average maintenance dose per day for a drug used for its
main indication in adults.
• Purpose: to serve as a tool for drug utilization monitoring and research in order to improve quality of drug use à can be use for other drugs
The classification of a substance in the ATC/DDD system is not a recommendation for use and it does not imply any judgements about efficacy or relative efficacy of drugs and groups of drugs.
The DDD is a unit of measurement and does not necessarily reflect the recommended or Prescribed Daily Dose. Therapeutic doses for individual patients and patient groups will often differ from the DDD as they will be based on individual characteristics (such as age, weight, ethnic differences, type and severity of disease) and pharmacokinetic considerations.
ATC/DDD – DDD Indicators
• Can be presented as:– DDD per 1000 inhabitants per day – DDD per 100 bed days– DDD/patient
𝐷𝐷𝐷 𝑝𝑒𝑟 100 𝑏𝑒𝑑 𝑑𝑎𝑦𝑠 =𝐴𝑚𝑜𝑢𝑛𝑡 𝑜𝑓 𝑑𝑟𝑢𝑔 𝑔𝑟𝑎𝑚𝑠 𝑢𝑠𝑒𝑑
𝐷𝐷𝐷 𝑊𝐻𝑂 𝑠𝑡𝑎𝑛𝑑𝑎𝑟𝑑 𝑥 (𝑛𝑜. 𝑜𝑓 𝑜𝑐𝑐𝑢𝑝𝑖𝑒𝑑 𝑏𝑒𝑑 𝑑𝑎𝑦𝑠)𝑥 100
𝐷𝐷𝐷 𝑝𝑒𝑟 𝑝𝑎𝑡𝑖𝑒𝑛𝑡 =𝐴𝑚𝑜𝑢𝑛𝑡 𝑜𝑓 𝑑𝑟𝑢𝑔 𝑔𝑟𝑎𝑚𝑠 𝑢𝑠𝑒𝑑
𝐷𝐷𝐷 𝑊𝐻𝑂 𝑠𝑡𝑎𝑛𝑑𝑎𝑟𝑑 𝑥 (𝑛𝑜. 𝑜𝑓 𝑝𝑎𝑡𝑖𝑒𝑛𝑡𝑠)