Visual pathway and defects
-
Upload
prashanth-reddy -
Category
Health & Medicine
-
view
3.397 -
download
4
Transcript of Visual pathway and defects

Visual Pathway
Dr Prashanth Reddy DNB PGT in Paediatrics, CSI Hospital, Bangalore.

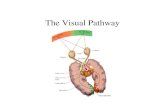
Visual pathway starting from retina consists of—Components:A. Optic nerveB. Optic chiasma. C. Optic tract D. Lateral geniculate body (of the thalamus).E. Optic radiationsF. Visual cortex


Optic Nerve• 2nd cranial nerve.• 47-50 mm in length.• Starts from optic disc & extends upto optic chiasma where the
two nerves meet.• Backward continuation of nerve fibre layer of retina which
consist of axons originating from ganglion cells.• Contains the afferent fibres of light reflex
• Has 4 parts : 1)intraocular (1mm) 2)intraorbital (30mm) 3)intra canalicular (6-9mm) 4)intracranial (10mm)

• Optic nerve is an outgrowth of brain.
• Not covered by neurilemma so does not regenerate when cut.
• Fibres of optic nerve are very thin(2-10 um in diameter)& are million in number.
• surrounded by meninges unlike other peripheral nerves.
• Both primary & secondary neurons are in retina

Intraocular part:• Starts from the optic disc, pierces the choroid
and sclera (converting into a sieve like structure- lamina cribrosa).
• At the back of eye ball it becomes continuous with intraorbital part.

Intraorbital part :• Extends from back of eyeball to optic foramina.• This part slightly sinuous to give play for the eye movements.• Here optic nerve is surrounded by all 3 layers of meninges &
subarachnoid space.• The central retinal artery along with enters the subarachnoid
space to enter the nerve on its inferomedial aspect.• Near optic foramina, optic nerve is closely surrounded by
annulus of zinn & the origin of four recti muscles.• Some fibres of superior & medial rectus are adherent to its
sheath & account for painful occular movements in retrobulbar neuritis.

Intracanalicular part
• This part is closely related to ophthalmic artery.
• it crosses the nerve from medial to lateral side in dural sheath.
• Sphenoid & posterior ethmoidal sinuses lie medial to it & separated by thin bony lamina, this relation accounts for retrobulbar neuritis following infection of sinuses

Intracranial part:• About 10mm• Lies above cavernous sinus & converges with
its fellow to form chiasma.• Ensheathed in piamater.• Internal carotid artery runs below then lateral
to it.

Optic chiasma
• Flattened structure,12 mm horizontally & 8mm anteroposteriorly.
• Ensheathed by pia & surrounded by CSF.• Lies over diaphragma sellae so visual field defects
seen in patient with pituitary tumor having suprasellar extension.
• Posteriorly chiasma continuous with the optic tracts & form the anterior wall of 3rd ventricle.
• Nerve fibres arising from nasal half of two retina decussate at the chiasma.

Optic tract
• Cylindrical bundle of nerve fibres.• Run outwards & backwards from
posterolateral aspect of optic chiasma.• Fibres from temporal half of retina of same
eye & nasal half of opposite eye.• Posteriorly each ends in Lateral Geniculate
Body.

Lateral Geniculate body -A nucleus in the thalamus,
which projects to the 1° visual cortex and serves visual perception.- This body is the site of termination of all optic nerve fibres except few which reach and relay in the pretectal region and superior colliculus of Midbrain.
Consists of 6 lamina.Contralateral retina – 1,4,6Ipsilateral retina – 2,3,5

0ptic radiation
• From LGB to the occipital cortex.• Pass forwards then laterally through the area of wernicke as
optic peduncles.• Anterior to lateral ventricle ,traversing the retrolenticular part of
internal capsule, medial to auditory tract.• Its fibres then spread out fanwise to form medullary optic
lamina.• Inferior fibres subserve upper visual fields & sweep
anteroinferiorly in meyer’s loop & temporal lobe to visual cortex.
• Superior fibres subserve inferior visual field proceed posteriorly through parietal lobe to visual cortex.


Visual cortex
• It is located on the medial aspect of occipital lobe, above and below the calcarine fissure.
Visual cortex
Visuopsychic area
Peristriate area 18
Parastriate area 19
Visuosensory area
Striate area 17

feature Visual sensation Somatic sensation
Sensory end organ Rods and Cones Nerve endings in the skin
Neurons of 1st order Lie in bipolar layer of retina
Lies in posterior root ganglion
Neurons of 2nd order Lies in ganglion cells of the retina
Lies in nucleus gracilis and nucleus cuneatus
Neurons of 3rd order Lie in geniculate body Lie in geniculte body

Neural pathway for vision
• Ist order sensory neurons – Arise from the bipolar cells of the retina.
• II nd order neurons are the Multipolar neurons whose axons run along the optic nerve to the optic chiasma
• Nasal fibres – Cross to opposite side and terminate in LGB of opposite side.
• Temporal fibres – Doesn’t cross and terminates in ipsilateral LGB.

• The cell bodies of III order sensory neurons are located in LGB.
• Their axons form optic radiation which project into the visual cortex.

Visual reflexes
• Light reflex or pupillary reflex:When light is shown to one eye, normally the pupils of both eyes constrict.
- Direct light reflex: The constriction of pupils
upon which light is shown is called direct light reflex.
- Indirect or consensual:The constriction of pupil on the other eye even though no light is shown


ACCCOMODATION REFLEX• When the eyes are focussed
from a distant to near object, three reactions take place
• 1. Constriction of pupils• 2. thickening of lens due to
contraction of ciliary muscles• 3. Convergence of both eye
ballsThese three reactions together
constitute Accommodation or near reflex

Clinical correlation
• Loss of vision in one half of the visual field (Rt or Lt) is termed as hemianopia.
• Homonymous hemianopia: Loss of vision in the same halves of the visual field.
• Heteronymous Hemianopia: Loss of vision in the different halves of the visual field.

Lesions of the visual pathwayLesions of the optic nerve:• Characterised by marked loss of vision or complete
blindness on the affected side associated with abolition of direct light reflex on the ipsilateral side and consensual on contralateral side.
Causes: optic atrophy indirect optic neuropathyacute optic neuritis traumatic avulsion of optic nerveEg : right optic nerve involvement

2)Lesions through proximal part of optic nerve : ipsilateral blindness. contralateral hemianopia abolition of direct light reflex on affected side
& concensual light reflex on contralateral side. near reflex intact.Rt optic nerve Involvement in Proximal part

Central lesions of chiasma (sagittal):Characterised by: Bitemporal hemianopia Bitemporal hemianopic paralysis of pupillary reflex. (usually lead to partial descending
optic atrophy)
causes: suprasellar aneurysm tumors of pituitary gland craniopharyngioma suprasellar meningioma & glioma of 3rd ventricle. third ventricular dilatation due to obstructive hydrocephalus. chronic chiasmal arachnoiditis

Lateral chiasmal lesions :Characterised by • Binasal hemianopia• Binasal hemianopic parallysis of pupillary reflex (usually lead to partial
descending optic atrophy)causes: • Distension of 3rd ventricle causing pressure on
each side of optic chiasma• Atheroma of carotids & posterior communicating
artery.

Lesions of optic tract :Characterised by :• Incongruous homonymous hemianopia with C/L
hemianopic pupillary reaction( wernicke’s reaction)• These lesions usually lead to partial descending optic
atrophy & may be associated with C/L 3rd nerve paralysis & ipsilateral hemiplegia.
Causes:Syphilitic meningitis/ gumma.Tuberculosis Tumors of optic thalamusAneurysm of superior cerebellar or posterior cerebral
arteries.

Lesions of lateral geniculate body :
leads to homonymous hemianopia with sparing of pupillary
reflexes & may end in partial optic atrophy

Lesions of optic radiations :Causes: Vascular occlusionPrimary & secondary tumorsTraumaCharacterised by :
TOTAL OPTIC RADIATION
INVOLVEMENT
COMPLETE HOMONYMOUS
HEMIANOPIA( sometimes sparing macula)

LESIONS OF PARIETAL LOBE (involving superior fibres of optic radiations)
INFERIOR QUADRANTIC
HEMIANOPIA( PIE ON THE FLOOR)
LESIONS OF TEMPORAL
LOBE (involving
inferior fibres of
optic radiations)
SUPERIOR QUADRAN
TIC HEMIANO
PIA( PIE ON THE ROOF)

• Pupillary reactions are normal as fibres of light reflex leave the optic tracts to synapse in the superior colliculi.
• Lesions of optic radiations do not produce optic atrophy as the 1st order neurons (optic nerve fibres) synapse in LGB.

Lesions of visual cortex: pupillary light reflex is normal & optic atrophy does not occur following visual cortex lesions.
Congruous homonymous hemianopia(sparing macula)
Occlusion of posterior cerebral artery supplyin anterior part of
occipiatl cortex

Abnormalities of pupillary reactions
Amaurotic light eye reflex: absence of direct light reflex on affected side and absence of consensual light reflex on the normal side.
• Indicates lesions of the optic nerve or retina on the affected side leading to complete blindness.
• In diffuse illumination both pupils are of equal size.

Efferent pathway defect: absence of both direct and consensual reflex on the affected side and presence of both on the normal side.
• Near reflex is also absent on the affected side.Causes : • Effect of parasympatholytic drugs.• Internal opthalmoplegia.• Third nerve paralysis.

Wernick's hemianopic pupil: • It indicates lesion of the optic tract.• Light reflex (ipsilateral direct and contralateral
consensual) is absent when light is thrown on temporal half of retina on the affected side and nasal half of the opposite side
- while it is present when light is thrown on nasal half of the affected side and temporal half of the opposite side.

Marcus gun pupil :• It is the paradoxical response to light in the
presence of a relative affarent pathway defect( RAPD).
• It is tested by swinging flash light test.• It is the earliest indication of optic nerve
disease even in the presence of normal visual activity.

Argyll Robertson Pupil(ARP):• Here the pupil is slightly small in size and
reaction to near reflex is present but light reflex is absent, i.e, there is light near dissociation.
• Both pupils are involved and dilate poorly with mydriatics.
• It is usually caused by a lesion ( usually neurosyphilis ) in the region of tectum.


The Adie's tonic pupil:• Reaction to light is absent and to near reflex is
very slow and tonic.• The affected pupil is large( anisocoria).• It is caused by postganglionic parasympathetic
pupillomotor damage.• It is usually unilateral, associated with absent
knee jerk and occurs more often in young women.

15 sq.Km of rain forest disappear every minute