Vibrant Winter 2016
-
Upload
clementine-words -
Category
Documents
-
view
216 -
download
0
description
Transcript of Vibrant Winter 2016

porterhospital.org :: Spring 2013 1PHOTO BY ELLEN JASKOL
Your Connection to Healthy Living
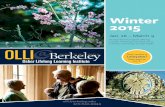
Volume 4, Issue 1 | Winter 2016
A BRIGHTER OUTLOOKTeaming up for
Advances in imaging and genetics mean a more positive future in women’s battle with breast cancer.
2 Putting together the PSA puzzle
3 PCPs: A partnership for good health
7 Surgical solution for ulcerative colitis
Genetic counselor Josie Kagey and breast surgeon Dr. Caitlyn Truong team up to find and fight breast cancer at its earliest stages.

2 VIBRANT :: Porter Adventist Hospital
Learn more about the signs and symptoms of prostate cancer and prostate screenings at a FREE seminar with Dr. Mark Jones on March 3. See Page 8 for details.
PHOT
O: P
UZZL
E ©
ISTO
CKPH
OTO.
COM
/ANT
IMAR
TINA
; TRE
ADM
ILL
©IS
TOCK
PHOT
O.CO
M/J
USTI
NHOR
ROCK
S
MIDLIFEMOTIVATION?If brain health is on your mind, it’s time to take a step. And another step. In fact, maybe it’s time to get on the treadmill.
According to new research presented at the American Heart Association EPI/Lifestyle 2015 meeting, people with higher fitness in midlife may have larger brain volumes and higher cognitive function by the time they hit 60.
While the study did not track fitness levels over time and it only finds an association — not a true cause-and-effect correlation — it does suggest that midlife physical fitness may help ensure healthy brain aging.
“We can’t necessarily say that larger brain volumes are a direct result of exercise. However, what we do know is that people in their 40s who were healthy and performed well on an exercise stress test tended to have healthier brains later in life,” says Susan Anzalone, MD, a neurologist who specializes in multiple sclerosis (MS) at Porter Adventist Hospital.
In other studies, exercise has been linked to better brain function. For
example, exercise has been shown to: Decrease fatigue in MS patients
Lower risk for cognitive decline Improve memory in older women with probable mild cognitive impairment (MCI) Slow disease progression in patients with Alzheimer’s disease or Parkinson’s disease
Anzalone says it’s important to go over your exercise regimen with your physician, especially before beginning anything new.
The Puzzle
Dr. Mark Jones
We are part of the Centura Health Cancer Network, delivering integrated, advanced cancer care across
Colorado and western Kansas.
Dr. Susan Anzalone
PSAGUYS, LISTEN UP: If you’re confused about PSA testing, let us help you put the pieces together. PSA testing measures the amount of a protein called prostate-specific antigen in the blood. While noncancerous conditions, such as prostatitis and benign prostatic hyperplasia, can cause PSA to rise, so can cancer. The higher a man’s PSA level, the higher his risk for prostate cancer.
So, what’s the big controversy?In 2012, the U.S. Preventive Services Task Force (USPSTF) recommended against routine PSA testing based on a finding that overtreatment with surgery, radiation, or hormone therapy outweighs the harms of not diagnosing the cancer at all. In many men, prostate cancer is slow-growing and produces no symptoms.
Statistics show that men are listening. In fact, a recent study shows that PSA testing has dropped by 28 percent since the USPSTF recommendation.
However, Mark Jones, MD, a urologist at Porter Adventist Hospital, says there’s a smarter approach. “The question isn’t, ‘Should I get screened or not?’ The question is, ‘Should I get treated or not?’”
“Statistically, we have seen a 40 percent decrease in prostate cancer mortality since PSA testing was introduced,” Jones says.
Meanwhile, molecular testing has “changed the game,” Jones says, adding that looking at cancer at the molecular level sorts the aggressive cancers from the ones that can be treated with a “watch and wait” approach. Jones says an estimated 70 percent of prostate cancer patients in his practice (The Urology Center of Colorado) go on active surveillance, which simply involves regular PSA tests and biopsies to actively recheck cancer progression over time.
Men who do not get screened, meanwhile, could be missing intermediate or high-risk cancers that require surgery.
The American Cancer Society recommends that men at average risk make an informed decision with their health care provider about PSA testing beginning at age 50.Join Dr. Susan Anzalone to
learn more about multiple sclerosis, the symptoms, treatment options, and if you may be at risk at a FREE community seminar on Jan. 27.

3PHOT
OS: C
ONSU
LT ©
ISTO
CKPH
OTO.
COM
/XM
ONKE
YBUS
INES
SIM
AGES
; STH
ETHO
SCOP
E ©
DOLL
ARPH
OTOC
LUB.
COM
/KM
IT
porterhospital.org :: Winter 2016
PRIMARY BENEFITSConnecting with a primary care provider can keep you healthier and happier
Studies show that when you have a primary care physician, you’ll live a healthier life and be more satisfied with your care. But what are the tangible benefits, really?
Ernesto Herfter, MD, a board-certified family medicine physician at Centura Health Physician Group Primary Care Porter, offers his thoughts on what patients gain by choosing a primary care physician (PCP) — and what they stand to lose if they don’t.
PCP Trumps ERThere’s another aspect to primary care — the things you give up — when you rely on the emergency room or urgent care for nonurgent health needs.
“These providers don’t know your health history. They don’t know your values. They may order excessive tests to cover their bases,” Herfter says. This can end up costing patients far more money in the end, not to mention peace of mind. “When a certain treatment is recommended, you may not be as receptive as you would be with a PCP you know and trust,” Herfter says.
In the end, he urges patients to get connected with a primary care physician. Find one who’s a good fit. Make regular appointments. Keep up with routine screenings. And then, when health conditions arise, you’ll have a ready answer.
When choosing a primary care provider, look for someone who: Encourages you to ask questions Takes time to listen to you Speaks in language you understand Makes you feel comfortable during visits Knows your values and how they guide your care
Area Centura Health Physician Groups accepting new patients:CHPG Primary Care Porter 303-649-3200950 East Harvard Avenue, Suite 200
CHPG Primary Care Cherry Creek 303-316-0416300 South Jackson Street, Suite 340
CHPG at Clermont Park 303-649-31552479 South Clermont Street
CHPG at Holly Creek 303-649-38205500 East Peakview Avenue
Dr. Ernesto Herfter
RELATIONSHIPIn an increasingly specialized health care system, a PCP can be that one physician you build a strong relationship with over time. In fact, an October 2015 article in Harvard Business Review cites surveys showing that patients value the people skills of their providers and their individual relationships with providers above all else.
What you can do: Talk to your doctor about your health goals, your values and, of course, your symptoms.
TRUSTTrust is paramount in any relationship. “If you grow to trust your doctor over time, it’s easier to weigh the risks and benefits of treatment with that doctor,” Herfter says. “He or she knows your family and medical history, your values, and your full medical picture.”
What you can do: If you are unsure about a treatment plan or a medication, share your concerns with your PCP.
ACCESSTo be blunt, it’s easier to get in to see a family medicine or internal medicine physician if you’re an existing patient. “If you are my patient and I know I’m seeing you for a sinus problem or pain, I can get you in that day. I don’t have to do an extensive history because I already have an extensive history,” Herfter says.
What you can do: If you aren’t already, get established with a PCP.
TIMEWhen you are established with a primary care physician, you’ll have more time during appointments — and possibly even access to your physician via email — to ask questions.
What you can do: Come prepared to appointments with a list of questions.

VIBRANT :: Porter Adventist Hospital4 PHOTOS BY ELLEN JASKOL
Ahead of the curve
While breast cancer continues to be the second most common cancer among women (behind skin cancer), the good
news is that fewer women die from it every year.
The key reason is summed up in a single word: early. Early detection of breast cancer leads to early treatment. In fact, cancer can be diagnosed while it is still contained within the ducts. These are called “stage 0” cancers. Much of this is owed to advancements in imaging that help find cancer at its earliest stages. Meanwhile, new frontiers in genetic testing and counseling — including models that can predict your lifetime risk of breast cancer — are changing the game.
Here’s what you need to know.
Advancements in imaging, genetics take the fight against breast cancer to new levels
Josie Kagey, certified genetic counselor, and Dr. Caitlyn Truong, medical director of breast surgery, team up at Porter Adventist Hospital to help women make the best decisions about their care.
It’s in the genesTesting for genetic predispositions to breast cancer
has opened up a whole new frontier in early breast cancer detection and prevention.
As the field continues to expand — and with genetic counselors now in every Denver-area Adventist hospital — Josie
Kagey, MS, a certified genetic counselor at Porter Adventist Hospital, says it’s important to
know the difference between genetic counseling and genetic testing.

porterhospital.org :: Winter 2016 5
What is DCIS, and what’s the big controversy?
A: Ductal carcinoma in situ, sometimes called DCIS or stage 0 cancer, is when cancer is still confined within the milk ducts. “In situ” means “in place,” meaning these cells have not left the milk ducts to invade nearby breast tissue. A study published in JAMA Oncology last summer has reenergized the discussion about whether surgical treatments for DCIS are necessary. The study suggests that women treated for DCIS with lumpectomy or mastectomy ended up having about the same chance of dying of breast cancer as the average woman.
So, why then do we treat DCIS?
A: The JAMA Oncology study wasn’t a bombshell for breast surgeons and those who weigh treatment decisions every day. “Some DCIS has a higher chance of recurrence, and some has a lower chance. The problem is we don’t yet know which ones are which,” says Caitlyn Truong, MD, medical director of the breast surgery program at Porter Adventist Hospital.“The really new information will come on that day when we can predict how DCIS will behave,” she says.“The bottom line is, until we discover which DCIS needs treatment and which can be observed, we have to treat DCIS,” she says. Why? “We want to prevent it from coming back. Unfortunately stage 0 cancer can come back. And if it does, it has a 50 percent chance of coming back as an invasive cancer.”
How is DCIS diagnosed?
A: Mammogram is still the gold standard for diagnosing breast cancer, and that includes DCIS. “Mortality from breast cancer has decreased, and early diagnosis is one of the most commonly cited reasons,” Truong says. Porter’s new 3D mammography machine (see box at right) helps detect smaller cancers than standard screenings.
We are part of the Centura Health Cancer Network, delivering integrated, advanced cancer care across Colorado and western Kansas.
Genetic counseling: “Some people do not realize that genetic counseling is not just about genetic testing,” Kagey says. Genetic counseling takes a variety of factors into consideration — such as weight, personal health history, hormone exposure, and all the breast cancer diagnoses in a three-generation family tree. “Based on all that information, we run models that give us a woman’s lifetime risk for breast cancer,” Kagey says, adding that the results help guide screening recommendations.
One huge upside of genetic counseling? “Genetic counseling opens up family and generational health discussions that weren’t taking place in the past,” Kagey says. “We owe it to the generations following us to let them know if we have a gene mutation that has been identified. It triggers a responsibility.”
Genetic testing: Genetic testing involves a blood test that looks for known genes that cause cancer. “The genetic testing piece is cool because now not only are we testing the BRCA1 and BRCA2 genes — specific genes that increase breast and ovarian cancer risk — but there is a whole host of other genes that we’re able to test for in multigene panels, rather than testing one gene at a time like in the past,” Kagey says.
Call 303-765-3923 to learn more about genetic counseling at Porter Adventist Hospital.
Understanding DCISUnderstanding DCIS
Q
Q
Q
Q Q
Q
Q
3D MammographyPorter Adventist Hospital is now home to tomosynthesis, a type of mammogram that may outperform standard mammography at detecting small, more lethal, invasive cancers.
In conjunction with standard mammography, tomosynthesis is available to all women who are screened for breast cancer at Porter Adventist Hospital.
“I’m pretty excited about tomosynthesis,” Truong says. “Instead of just giving us two pictures per breast, it gives us many more images. It also helps us image dense breast tissue better.”
Schedule your screening mammogram today by calling 303-765-6500 or text your full name to 303-872-7469, and we’ll call you to set up your appointment.
See you soon!
How common is DCIS?
A: DCIS now accounts for 20 to 25 percent of all cancers detected by screenings, such as mammography.
Why are we hearing more about it these days?
A: As mammography rates have risen and imaging technology advances, smaller cancers are being found earlier. That includes DCIS.
What are the treatment options?
A: Surgical treatments include lumpectomy to remove the affected area or mastectomy. Follow-up radiation therapy and hormone blockers also may be recommended. “DCIS is one of those diseases that is traditionally thought to be almost cured with surgery. When we do radiation and hormone blockers, that’s to prevent recurrences,” Truong says.
What should I ask my doctor?
A: In the end, Truong urges DCIS patients to remember that the prognosis for DCIS is very good. “A woman treated for DCIS has a survival rate of 99 percent after five years,” she says.There is also plenty of time to make a decision, so it’s OK to take the time to sort through your options, starting with these questions for your doctor:❋ What combination of treatment options
might be right for me?❋ If I choose not to treat DCIS, what is the
natural progression of DCIS? ❋ How often should I have mammograms?❋ How do you feel about me getting a second
opinion?

6 VIBRANT :: Porter Adventist Hospital
PHOT
O: C
ONSU
LT ©
ISTO
CKPH
OTO.
COM
/LAF
LOR;
GLA
SS ©
ISTO
CKPH
OTO.
COM
/TET
IANA
RYSH
CHEN
KO
Colonoscopy is the only cancer screening test that can actually find precancerous growths and remove them. Yet, a recent study shows that two in five adults ages 50 to 75 are not up-to-date with colorectal cancer screening. Meanwhile, a separate study shows that more than three in five adults with a close relative who had colon cancer are not getting screened early enough.
What gives?
A study commissioned by StopColonCancerNow.com, a community of physicians dedicated to promoting colon cancer screening, shows the reasons people avoid colonoscopy are varied.28 percent don’t think it’s necessary20.1 percent say it’s too expensive20.1 percent dislike the procedure15.8 percent rely on other methods to avoid colon cancer6.5 percent say they didn’t know they need one6.5 percent are too busy
Don’t play with fireColorectal cancer is the No. 2 cancer killer in the United States. Gavin Sigle, MD, a colorectal surgeon at Porter Adventist Hospital and Littleton Adventist Hospital, says patients who skip screenings are playing with fire. “If you do not get a screening colonoscopy at age 50 or follow screening recommendations, you’re really at risk of developing a cancer or developing a late-stage cancer that doesn’t allow for surgical intervention,” he says.
He sees the consequences firsthand.
“Once colon cancer has spread beyond the colon, it typically goes to the liver. Then you are really looking at different options from a surgical standpoint. It’s not as much of a cure option as it is a prolonging-life option,” he says.
The good news is when colorectal cancer is diagnosed early, before it has spread, nine out of every 10 colorectal cancer patients are still alive five years later.
“The whole point of a colonoscopy is to prevent colon cancer or catch colon cancer at an early stage when it is treatable,” Sigle says.
becoming less routineScreenings
MANY AMERICANS NOT UP-TO-DATE ON COLORECTAL CANCER SCREENING
DO THE PREPYou’ve heard the stories. There’s no question that bowel prep is one of the reasons people avoid colonoscopy. But newer bowel preps are lower in volume; they taste better; and they can be taken in separate doses or even mixed with Sprite, or light-colored Crystal Light and Gatorade. Some say drinking the prep solution through a straw helps it go down faster with less bad taste.
Other colonoscopy “survivors” suggest preparing for your day of prep by getting together a good book, a tablet to binge watch a show you’ve been wanting to see, and diaper rash ointment (just in case you get sore).
Whatever you do, don’t miss a chance to keep your colon cancer-free. If you’re due for a colonoscopy, schedule it today.
Porter Adventist Hospital is part of the Centura
Health Cancer Network, delivering integrated, advanced cancer care across Colorado and
western Kansas.
Join Dr. Gavin Sigle to learn about the symptoms and treatment options of Crohn’s disease at a FREE seminar on March 16. See Page 8 for details.

porterhospital.org :: Winter 2016
HELP for ulcerative colitisElective surgery may prolong years of life and quality of life
PHOT
O BY
MIC
HAEL
RIC
HMON
D
About 240 out of every 100,000 adults in the U.S. lives with ulcerative colitis, or chronic inflammation of the bowels. While those stats may not knock your socks off, those living with the condition understand what it’s like to take medication every day and hope for remission of symptoms.
Elective surgery can help.
In fact, adults 50 and older with advanced ulcerative colitis who opt for surgery may have extended life, compared with those who choose long-term drug treatment.
“Surgery for ulcerative colitis is curative. It’s a one-time thing, unlike medication, which patients have to take the rest of their lives — often with side effects,” says Gavin Sigle, MD, a colorectal surgeon at Porter Adventist Hospital and Littleton Adventist Hospital. The surgery involves removing the colon and rectum and making a new rectum out of the small intestine.
Symptoms of advanced ulcerative colitis may include: Loose, bloody bowel movements Fever Severe abdominal cramping Anemia Loss of appetite Weight loss
In addition to alleviating these symptoms, surgery offers another important potential benefit. “Patients with ulcerative colitis have a significantly increased risk of colon cancer. By removing the colon and rectum, you remove that risk essentially to zero,” Sigle says.
GET TO KNOW GAVINHailing from Evergreen, Gavin Sigle, MD, colorectal surgeon at Porter Adventist Hospital, likes to tell people he literally grew up in the mountains. A fan of mountain biking, white-water kayaking, hiking, backpacking, and — of course — skiing, Sigle also has several years of collegiate and professional soccer under his belt, having competed in two pre-Major League Soccer leagues prior to medical school. He played professionally for the Cleveland Whitecaps (D3 pro league) and the Pittsburgh Riverhounds (A-League). “I still play quite a bit of soccer recreationally,” he says.
His day job is surgery, a specialty he fell in love with early in his training. “In medical school, you learn pretty quickly whether you’re a surgeon or not,” he says, adding that he ultimately decided on colon and rectal surgery for two primary reasons. “Most of my patients are curable. I can make them better right away,” he says. Secondly, he wanted the opportunity to use scopes, specialized instruments used to view and perform laparoscopic, or minimally invasive, surgery.
Sigle earned his medical degree at West Virginia University School of Medicine, completed his residency at University of California San Francisco-Fresno, and his fellowship training at the University of Southern California. He is board-certified in both general surgery and colon and rectal surgery.
He has extensive training in laparoscopic and minimally invasive colon and rectal surgery, including complicated pelvic laparoscopy for rectal cancer, ulcerative colitis, and fecal incontinence. He also specializes in sphincter-saving operations for patients with low rectal cancers who want to preserve continence.
Right before medical school, Dr. Gavin Sigle lived on the island of Trinidad for
a year to play soccer.
“ Patients with ulcerative colitis can leave the operating room cured.”
— DR. GAVIN SIGLE
7
Dr. Sigle treats patients with ulcerative colitis, irritable bowel syndrome, Crohn’s disease, colorectal cancer, and other diseases of the lower digestive system. To make an appointment, call 303-794-6747.
Pelvic health issues, such as incontinence, do not have to impact your quality of life! Learn about treatment options at a FREE seminar on Jan. 21. See Page 8 for details.

Non-ProfitOrganizationU.S. Postage
PAIDDenver, CO
Permit No. 47732525 South Downing Street Denver, CO 80210
Portercare Adventist Health System
UPCOMING EVENTSJoin the health experts at Porter Adventist Hospital to learn ways to stay healthy. All programs are FREE and are held in the Porter Adventist Hospital Conference Center unless otherwise indicated. For programs held in the Porter Adventist Hospital Conference Center, there is a free parking garage as well as free valet parking at the hospital’s main entrance. Registration is required for all events; register online at porterhospital.org/events or call 303-765-3825.
Register online at porterhospital.org/events
Porter Adventist Hospital is a regional medical center that provides care for complex health issues. We specialize in complex surgery, cardiovascular care, spine care, joint replacement, liver and kidney transplants, and cancer care. We are part of Centura Health, the region’s leading health care network. Vibrant is published quarterly by Porter Adventist Hospital – Portercare Adventist Health System. The purpose of this publication is to support our mission to improve the health of the residents in our community. No information in this publication is meant as a recommendation or to substitute for your physician’s advice. If you would like to comment or unsubscribe to this magazine, please email us at [email protected]. Vibrant is produced by Clementine Health Marketing.
PELVIC HEALTH — GET BACK INTO YOUR ACTIVE LIFEOften men and women don’t talk about pelvic health and symptoms such as incontinence. Millions of people have the same issues, but they don’t seek treatment. However, it can be treated successfully and is not simply a part of aging. Get the facts and start enjoying your life again! Date: Thu, Jan 21 Time: 6-7 p.m.
PHOT
OS: M
ENOP
AUSE
©DO
LLAR
PHOT
OCLU
B.CO
M/H
IGHW
AYST
ARZ;
SKI
©IS
TOCK
PHOT
O.CO
M/B
OGDA
NHOD
A
GET THE FACTS ON MULTIPLE SCLEROSISMore than 2 million people worldwide are impacted by MS. Dr. Susan Anzalone will break down the facts about this disease. Find out who is at risk, how to identify symptoms, and what the treatment options are. Date: Wed, Jan 27 Time: 6-7 p.m.
MENOPAUSE — WHAT YOU SHOULD KNOWIf you’re concerned about menopause, it’s time to get the facts. Learn how this hormonal change can impact you and how to turn it into a good time to reassess your approach to your overall health. Date: Tue, Feb 2 Time: 6-7 p.m.
CONCUSSIONS — NOT JUST FOR ATHLETES Concussions are a serious injury and not limited to athletes and kids. For older adults, the risks of falling and sustaining a concussion are all too real. Learn how to identify the symptoms of a concussion and how to avoid injury by preventing falls. Date: Wed, Feb 10 Time: 6-7 p.m.
SILENT HEART ATTACKSA heart attack isn’t always obvious. A silent heart attack is more common in women, and they may not even know it is happening. Learn how reducing high blood pressure, high cholesterol, smoking, and controlling your weight can help you reduce your risk. Date: Thu, Feb 18 Time: 6-7 p.m.
porterhospital.org
Pioneering Health in Denver
PROSTATE HEALTH — GUYS, IT’S TIME YOU KNOWProstate cancer is the second most common cancer in American men. Dr. Mark Jones will discuss prostate health, the effects of aging, and how it may impact the body. Find out what age you should begin prostate screenings, the signs and symptoms of prostate cancer, and what to do if you are diagnosed. Date: Thu, Mar 3 Time: 6-7 p.m.
CROHN’S DISEASE — DON’T SUFFER IN SILENCECrohn’s disease is an inflammatory bowel disease (IBD), which can lead to abdominal pain, fatigue, weight loss, and malnutrition. Dr. Gavin Sigle will discuss the available therapies that can reduce symptoms. Date: Wed, Mar 16 Time: 6-7 p.m. Location: Cherry Hills Country Club,
4125 S. University Boulevard, Englewood
FREE HEALTH AND WELLNESS PROGRAMInterested in learning more about a FREE six-week course designed to improve your overall health? This course includes individual assessments of cholesterol, diabetes, height, weight, body mass index (BMI), blood pressure, and lifestyle. Learn more at a FREE information session at Porter Adventist Hospital on Jan. 11, 12, or 13 at 6:30 p.m. Must be 18 years or older to qualify. Call 303-778-5710 to RSVP.
Part of Centura Health, the region’s leading health care network.Centura Health does not discriminate against any person on the basis of race, color, national origin, disability, age, sex, religion, creed, ancestry, sexual orientation, and marital status in admission, treatment, or participation in its programs, services and activities, or in employment. For further information about this policy, contact Centura Health’s Office of the General Counsel at 303-804-8166. Copyright © Centura Health, 2016.