Updates On Upper Gastrointestinal Malignancies 2015
-
Upload
osuccc-james -
Category
Health & Medicine
-
view
61 -
download
4
Transcript of Updates On Upper Gastrointestinal Malignancies 2015
Updates On Upper Gastrointestinal Malignancies 2015
Tanios Bekaii-Saab, MD Chief , Section of Gastrointestinal Cancers Disease Specific Research Group Leader
Professor of Medicine and Pharmacy OSUCCC- Arthur James Cancer Hospital
Advanced Gastro-esophageal Cancers
• Marginal differences between chemo doublets and triplets that perhaps do not justify the differences in toxicities.
• Trastuzumab should be considered as an option added to a platinum and 5FU in the presence of Her-2 overexpression
• Ramucirumab +/- Paclitaxel is a standard second line regimen
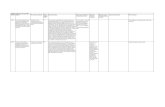
Phase 3, Randomized, Double-blind, Multicenter, Placebo-controlled Trial of Rilotumumab Plus Epirubicin,
Cisplatin, and Capecitabine as First-line Therapy in Patients with Advanced MET-positive Gastric or
Gastroesophageal Junction Cancer: RILOMET-1 Study
D. Cunningham,1 N. C. Tebbutt,2 I. Davidenko,3 A. M. Murad,4 S. Al-Batran,5 D. H. Ilson,6 S. Tjulandin,7 E. Gotovkin,8 B. Karaszewska,9 I. Bondarenko,10 M. A. Tejani,11 A. A.
Udrea,12 M. Tehfe,13 N. Baker,14 K. S. Oliner,15 Y. Zhang,15 T. Hoang,15 R. Sidhu,15 D. V. T. Catenacci16
1Royal Marsden Hospital, Sutton, Surrey, UK; 2Austin Health, Heidelberg, VIC, Australia; 3Krasnodar City Oncology Center, Krasnodar, Russia; 4Hospital das Clínicas da Universidade Federal e Minas Gerais, Horizonte, Brazil; 5Krankenhaus Nordwest, University Cancer Center, Frankfurt,
Germany; 6Memorial Sloan Kettering Cancer Center, New York, NY, USA; 7Russian Cancer Research Center, Moscow, Russia; 8Regional Budgetary Institution of Public Health Ivanovo Regional Oncology Dispensary, Ivanovo, Russia; 9Przychodnia Lekarska Komed Oddzial Jednego Dnia, Konin, Poland; 10Dnipropetrovsk Medical Academy, City Multifield Clinical Hospital 4, Dnipropetrovsk, Ukraine; 11University of Rochester
Medical Center, James P Wilmot Cancer Center, Rochester, NY, USA; 12SC Medisprof SRL, Cluj-Napoca, Romania; 13Centre Hospitalier de L'Universite de Montreal Notre-Dame, Montreal, QC, Canada; 14Amgen Limited, Cambridge, UK; 15Amgen Inc., Thousand Oaks, CA, USA; 16The
University of Chicago, Chicago, IL, USA
MET and Targeting in EGC • MET gene alterations in 6% gastric ca (TCGA) • MET overexpression (IHC) 40-60%+ • MET/HGF altered – poor prognostic subgroup • Early data suggests MET amplification biomarker
of response to MET-targeted agents with MET TKI
Bass. Nature, 2014. Kwak, E. J Clin Oncol, 33, 2015 Suppl 3; abst 1. Iveson, T. Lancet Oncol, 2014
Cunningham, D. J Clin Oncol 2015;33:4000 [abstr]
Phase III ECX +/- Rilotumumab (RILOMET -1)
Stratification: PS, Locally advanced vs Metastatic Primary endpoint: Overall survival (90% power, HR 0.69, N= 600)
Secondary endpoints: PFS, ORR, DCR, Safety, Immunogenicity, PK
Untreated Gastric/GE jn MET+ (≥ 25% cells tumor membrane staining IHC)
HER2- ECOG 0-1
N= 600 ECX + Placebo 15 mg/kg
q3 weeks Maintenance: placebo
ECX + Rilotumumab 15 mg/kg q3 weeks
Maintenance: Rilotumumab
R A N D O M I Z E
Overall Survival: ECX +/- Rilotumumab
More deaths in the rilotumumab arm, due to disease progression Study terminated 11/2014 (DSMC) Cunningham, D. J Clin Oncol 2015;33:4000 [abstr]
||||| ||||||||| ||||| |||||||||||||||||||||||||||||||||||||||||||||||||||| ||||||||||||||||||||||||||||||||||||| ||||||||||||||
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|||||| |||| |
||||| ||||||||||||||||||||||| ||
|||||||||||||||||
|||||||||
||||||| | |
||||||||||||||||| |
||||||||| |
||
|||||| | |
|| ||
| ||||| ||
| ||||| |
| |||||| | |
||
0 3 6 9 12 15 18 21Time (months)
0
20
40
60
80
100
Ove
rall
Sur
viva
l (%
) ||||| ||||||||| ||||| |||||||||||||||||||||||||||||||||||||||||||||||||||| ||||||||||||||||||||||||||||||||||||| ||||||||||||||
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|||||| |||| |
||||| ||||||||||||||||||||||| ||
|||||||||||||||||
|||||||||
||||||| | |
||||||||||||||||| |
||||||||| |
||
|||||| | |
|| ||
| ||||| ||
| ||||| |
| |||||| | |
||
304 209 121 66 32 15 3 1305 241 140 81 41 13 1 1
RilotumumabPlacebo
Patients at risk
Median OS months
ECX + Rilotumumab 9.6 (7.9–11.4)
ECX + Placebo 11.5 (9.7–13.1)
Unstratified HR: 1.36 (1.05–1.75); P= 0.021
Clinical activity of AMG 337, a highly selective oral MET kinase inhibitor, in adult patients with MET-amplified
gastroesophageal junction, gastric, or esophageal cancer
Eunice L Kwak,1 Patricia LoRusso,2 Omid Hamid,3 Filip Janku,4 Muaiad Kittaneh,5 Daniel VT Catenacci,6 Emily Chan,7 Tanios S Bekaii-Saab,8 Benny Amore,9 Yuying
C Hwang,10 Rui Tang,10 Gataree Ngarmchamnanrith,10 David S Hong4
1Massachusetts General Hospital, Boston, MA; 2Yale Cancer Center, New Haven, CT; 3The Angeles Clinic and Research Institute, Los Angeles, CA; 4The University of Texas MD Anderson Cancer Center, Houston, TX; 5Karmanos Cancer Institute, Wayne State University, Detroit, MI; 6The University of Chicago, Chicago, IL; 7Vanderbilt University Medical Center, Nashville, TN; 8The Ohio State University Comprehensive Cancer Center, Columbus, OH; 9Amgen Inc., Seattle, WA; 10Amgen Inc., Thousand Oaks, CA
RECIST Responses in Patients With MET-Amplified GEJ/Gastric/Esophageal Cancer
• 13 patients with MET-amplified GEJ/gastric/ esophageal cancer treated to date; ORR = 8/13 (62%)
%∆
SO
D Fr
om B
asel
ine
-100%
-80%
-60%
-40%
-20%
0%
20%
40%
60%
80%
PR per RECIST 1.1
4wk +21wk
4wk 17wk
9wk 17wk
4wk 29wk
4wk 25wk
4wk +96wk
4wk +155wk
aLocal read as of Dec 8, 2014. bLocal read as of Sept 10, 2014. Central read as of Sept 18, 2014 for all other patients. One patient not shown with non-target lesions had clinical progression.
b
4wk +9wk
a
On active treatment Off treatment
Time to response: On treatment:
Summary Anti-MET Therapies in EGC • MET targeting with rilotumumab
– No value in gastric/GE jn cancers in any MET positive subgp – Worse outcome with rilotumumab, HR 1.36 – Marked difference from phase II results; correlative analyses pending
• Substantial evidence that MET antibody targeting not of value – MetGastric*: FOLFOX +/- onartuzumab (anti-MET ab)
Negative phase III med OS 11.3 vs 11 mths, HR 0.82, p= 0.244 • Promising activity with AMG337 in MET amplified GE cancers • Focus: other strategies – angiogenesis, anti-HER2, FGFR, cancer
stem cell, immune therapies, and biomarker identification
*Shah, M. J Clin Oncol 2015;33:4012 [abstr]
Immune Therapies in EGC • PD-L1, PD-L2 associated with poor prognosis in esophago-gastric
cancers – Increased expression in certain subsets of gastric ca (EBV)
• Recognition that GI cancers may be targeted by immune system
– Higher mutation burden
• Pembrolizumab – IgG4 anti-PD-1, broad anti-tumor activity blocks PD1 interaction with
ligands PD-L1 and PD-L2
Cancer Genome Atlas Research Network, Nature, 2014. Alexandrov, Nature, 2013
Relationship Between PD-L1 Expression and Clinical Outcomes in Patients With
Advanced Gastric Cancer Treated With the Anti-PD-1 Monoclonal Antibody
Pembrolizumab (MK-3475) in KEYNOTE-012 Yung-Jue Bang,1 Hyun Cheol Chung,2 Veena Shankaran,3
Ravit Geva,4 Daniel Catenacci,5 Shilpa Gupta,6 Joseph Paul Eder,7 Raanan Berger,8 Archana Ray,9 Marisa Dolled-Filhart,9
Kenneth Emancipator,9 Kumudu Pathiraja,9 Jared Lunceford,9 Jonathan Cheng,9 Minori Koshiji,9 Kei Muro10
1Seoul National University Hospital, Seoul, South Korea; 2Yonsei Cancer Center, Yonsei University College of Medicine, Seoul,
Korea;3University of Washington, Seattle, WA; 4Tel-Aviv Sourasky Medical Center, Tel-Aviv, Israel; 5University of Chicago, Chicago, IL, USA; 6H. Lee Moffitt Cancer Center and Research Institute, Tampa, FL;
7Yale University, New Haven, CT, USA; 8Sheba Medical Center, Tel Hashomer, Israel; 9Merck & Co, Inc, Kenilworth, NJ, USA; 1Aichi Cancer Center Hospital, Nagoya, Japan
KEYNOTE-012: Gastric Cancer Cohort
65/162 = 40% PD-L1+ (+ in immune cells or ≥ 1% tumor cells by 22C3 ab) Primary Endpoint: Overall Response Rate q 8 wks central review Median age 63 yrs; 56% ECOG 1; 66% ≥ 2 lines therapy; 19 Asia, 20 ROW
Previously treated Gastric/GE jn
ECOG 0-1 PD-L1 Positive
N= 39
Pembrolizumab 10 mg/kg q 2 wks
Bang, Y-J. J Clin Oncol 2015;33:4001 [abstr]
Pembrolizumab in Gastric Ca: Maximum Percentage Change From Baseline in Tumor Size, N= 32
aOnly patients with measurable disease per RECIST v1.1 by central review at baseline and at least 1 post-baseline tumor assessment were included (n = 32). Analysis cut-off date: March 23, 2015.
-100
-80
-60
-40
-20
0
20
40
60
80
100 C
h a n g
e F r
o m B
a s e l
i n e
i n S
u m o
f L o
n g e s
t D i a
m e t
e r o
f T a
r g e t
L e s
i o n ,
%
53.1% decrease in target lesions
Overall RR 22%
Conclusions : PD1 in GCA • Significant activity of pembrolizumab in advanced gastric cancer
– 22% RR (central), 40 week duration of response, 66% OS at 6 mths, median OS 11.4 mths
– PD L1 expression – preliminary correlation with outcome – MSI-H? – Supporting data from KEYNOTE-028 in esophageal ca*
• 41% PD-L1+; N= 23; ORR 23% (N= 5)
• Ongoing trials in gastric/GE junction – Phase II pembrolizumab +/- cisplatin/5-FU (KEYNOTE-059): PD-L1 + or - – Phase III pembrolizumab vs paclitaxel 2nd-line (KEYNOTE-061) – Phase III nivolumab vs placebo in previously treated (Japan) – Phase IB/II MEDI4736 + tremilumumab, MEDI4736 or tremi. (2nd-line)
*Doi, T. J Clin Oncol 2015;33:4010 [abstr]. NCT02335411. NCT02267343
Pancreas Neuroendocine Tumors • Several treatment options
– Observation – Regional therapies e.g., embolization, SIRT, surgery – Somatostatin analogs
• Octreotide, lanreotide • Peptide Receptor Radionuclide Therapy
– Cytotoxic therapies • Temozolomide, streptozocin, fluoropyrimidines
– Pathway directed agents • mTOR: Everolimus • VEGF: Sunitinib
Randomized Phase II Study of Everolimus vs. Everolimus plus Bevacizumab in Patients with Locally Advanced or Metastatic Pancreatic Neuroendocrine Tumors
CALGB 80701 (Alliance)
Matthew H. Kulke,1 Donna Niedzwiecki,2 Nathan R. Foster,3 Briant Fruth,3 Pamela L. Kunz,4 Hagen Kennecke,5 Edward M
Wolin,6 Alan P. Venook7 1. Dana-Farber Cancer Institute, Boston, MA; 2. Alliance Statistics and Data Center and Department of Biostatistics and
Bioinformatics, Duke University, Durham, NC; 3. Alliance Statistics and Data Center, Mayo Clinic, Rochester, MN 4. Stanford Cancer Institute, Palo Alto, CA 5. Vancouver Center: BC Cancer Agency, Vancouver, CA 6. University of Kentucky,
Lexington, KY; 7. University of California San Francisco, San Francisco, CA
Kulke, M. J Clin Oncol 2015;33:4005 [abstr]
Randomized Phase II CALGB 80701
Stratification: Prior SSA, Prior cytotoxic therapy, Prior sunitinib Primary endpoint: Progression-free survival (9 14 mths, 90% power, 1-sided alpha 0.15)
Advanced PNET POD within 12 mths
No prior mTOR/ bevazicumab therapy
N= 150 Everolimus 10 mg daily +
Bevacizumab 10 mg/kg q 2 wks + Octreotide LAR
Everolimus 10 mg daily + Octreotide LAR
R A N D O M I Z E
Summary CALGB 80701, PNET’s • Important trial evaluating VEGF and mTOR pathway
inhibitors – Higher RR, PFS, but more AE’s for everolimus and bevacizumab
• Data do not support use of everolimus and bevacizumab outside of a trial, but continued focus on these pathways important – Sequential vs concurrent? – Patient selection – Newer agents, different disease settings – Sequencing of treatment modalities
• Gemcitabine and Nab-Paclitaxel (GA) is a preferred standard • FOLF + MM-398 , once approved will become a standard for second line treatment following
failure with GA • FOLFIRINOX can be considered in patients < 70 y.o. , with PS 0-1 , normal bilirubin and no
significant comorbidities • Kitchen sink approach vs. Sequential approach • Perhaps a better choice for patients with borderline or locally advanced pancreas
cancer. • mOS has not reached the 1 year despite all these agents • Ruxolitinib, a JAK1/JAK2 inhibitor, in combination with capecitabine exhibited clinical activity
relative to capecitabine alone in second-line metastatic pancreatic cancer in select patients with CRP levels > 13
• JANUS 1 and 2 underway
Advanced Pancreas Cancer
A modified regimen of gemcitabine and nab-paclitaxel in patients with metastatic pancreatic cancer
Chemotherapy Dose Administration Frequency Gemcitabine 1000 mg/m2 IVPB over 30 min given q2weeks Nab-paclitaxel 125 mg/m2 IVPB over 30 min
Survival analyses N Median (months) 95% CI (months) Progression free survival 57 5.4 4.1; 7.4
Overall survival 57 10 5.9; 13
Toxicities N(%) Grades All grades 3 / 4
Neutropenia 12 (25) 5 (10) Febrile neutropenia 1 (2.1) -- Thrombocytopenia 9 (15) 3 (2) Neuropathy 13 (27) 1 (2) Fatigue -- 3 (6)
Krishna K et al. Abstract 366 – ASCO GI 2015
High Response Rate and PFS with PEGPH20 Added to Nab-Paclitaxel/Gemcitabine in Stage IV Previously Untreated Pancreatic Cancer Patients with High-HA
Tumors: Interim Results of a Randomized Phase 2 Study
Sunil Hingorani, MD, PhD1, William Harris, MD2, Andrew Hendifar, MD, MPH3, Andrea Bullock, MD4, Wilson Wu, PhD5, Ya Huang5, Ping Jiang, MD5
1Fred Hutchinson Cancer Research Center, Seattle, WA 2University of Washington School of Medicine, Seattle, WA
3Cedars Sinai Medical Center, Los Angeles, CA 4Beth Israel Deaconess Medical Center, Boston, MA
5Halozyme Therapeutics, Inc., San Diego, CA
Microenvironment in Pancreas Adenocarcinoma
• Hypovascular, hypoxic
• Physical stromal barrier – Hyaluronan (HA)
glycosaminoglycans – Increased EMT, chemoresistance
• PEGPH20 rhuman hyaluronidase
– Depletes HA in stroma – Improves drug delivery
Jaocobetz, et al. Gut, 2013. Courtesy: J. Shia (MSKCC)
Hingorani, S. J Clin Oncol 2015;33:4006 [abstr]
Randomized Phase II Gemcitabine + nab-Paclitaxel +/- PEGHPH20
Primary endpoint: Progression-free survival Secondary endpoints: PFS by Hyaluronan, ORR, OS, Safety, Correlatives
Untreated Met Panc Adenoca
KPS 70-100% N= 260 planned
nab-Paclitaxel + Gemcitabine
nab-Paclitaxel + Gemcitabine + PEGPH20
3ug/kg SQ x 2 wk (C1)wkly
R A N D O M I Z E
Study Conduct • Hold April 2014
– DSMC/ FDA – increased thromboembolic (TE) events
– Re-opened later 2014 • Rigorous screening for TE’s • Primary prophylaxis: enoxaparin
• Data presented is early
0 2 4 6 8 1 0 1 2 1 40
5 0
1 0 0
S tu d y D u ra tio n (m o n th s )
K-M
Est
imat
e of
Pro
gres
sion
Fre
e S
urvi
val (
%)
A G
P A G
Rand Phase II: PFS In HA-High Pts Treated with PEGPH20 + nab-P+Gem (PAG) vs AG
AG 4.3 months
PAG 9.2 months
HR 0.39 (0.15, 1.04)
Summary PEGPH20 + nab-P+Gem • Interesting early data in HA high patients
– Improved PFS (HR 0.39), improved response rate, trend OS – Phase III planned in HA high patients – needs validation
• Value to primary prophylaxis with enoxaparin, supports CONKO-004
• Key theme of randomized phase II trials, biomarker exploration
• Maturation of series of randomized phase II’s with gemcitabine + nab-paclitaxel
backbone over next 1-2 yrs – Many promising agents/targets: PEGPH20, Notch, stem cell, wnt-β-catenin, JAK/STAT,
immunotherapy, etc. – Treatment selection – CRP, homologous repair deficient, Hyaluronan-high?
Pelzer, U. J Clin Oncol, 2015
Resectable Disease : The role of Adjuvant Therapy
• Pancreas cancer is a systemic disease
• The role of adjuvant therapy following resection of pancreas cancer is well established
• Patients spend 25-30% of their average lifetime on adjuvant therapy.
• What type of adjuvant therapy? • Gemcitabine or b5FU are standard for treating patients with resected
pancreas cancer ( R0 and R1) based on best Level 1 evidence. • Favor Gemcitabine Better toxicity profile
• Many questions about the role of radiation remain unresolved, with toxicity and
cost concerns, and a lack of proven added survival benefit to chemotherapy alone.
Adjuvant Therapy • Current investigational adjuvant questions
– Value of multi-drug cytotoxic combinations? • FOLFIRINOX vs gemcitabine (PRODIGE) • Gemcitabine + nab-paclitaxel vs gemcitabine (APACT) • Gemcitabine + capecitabine vs gemcitabine (ESPAC-04)
– Role of adjuvant fluoropryimidine-based RT (RTOG 0848)?
– Value of addition of EGFR-TKI erlotinib (CONKO-005)?
Sinn M, Liersch T, Gellert K, Messmann H, Bechstein W, Waldschmidt D, Jacobasch L, Wilhelm M, Rau BM, Grützmann R, Weinmann A,
Maschmeyer G, Pelzer U, Stieler JM, Striefler JK, Ghadimi BM, Bahra M, Oettle H, Dörken B, Riess H
Charité – Universitätsmedizin Berlin, Germany In cooperation with AIO Germany (Arbeitsgruppe Internistische Onkologie)
CONKO-005 Adjuvant therapy in
R0 resected pancreatic cancer patients with Gemcitabine plus Erlotinib vs Gemcitabine for 24 weeks
Sinn, M. J Clin Oncol 2015;33:4007 [abstr]
Phase III Open-Label Trial (CONKO-005)
Stratify: Nodal status N0 vs N1, Surgery, T stage, KPS Primary Endpoints: DFS 14 18 mths, power 80%, 0.05 Secondary endpoints: OS, Safety
R0 Resected Panc Adenoca
KPS 70-100% N= 436 Gemcitabine
N= 217
Gemcitabine + Erlotinib 100mg PO daily
N= 219
R A N D O M I Z E
Overall Survival CONKO-005
Sinn, M. J Clin Oncol 2015;33:4007 [abstr]
Gem + E N= 219
Gemcitabine N= 217
DFS 11.6 mths 11.6 mths HR 0.89 (95% CI 0.72- 1.1)
Med OS 24.6 mths 26.5 mths
HR 0.90 (95% CI 0.71-1.15)
Estimated Survival
2 years 54% 53%
5 years 28% 19%
Conclusions Adjuvant Therapy • Addition of erlotinib – not meaningful
– CONKO-005 first mature erlotinib data set in adjuvant setting
• No improvement in DFS, OS, no relationship between rash grade and improved DFS
• Correlative analyses pending – LAP-07* (locally advanced): no benefit to erlotinib – RTOG 0848 (adjuvant) revised 2014: removed erlotinib
randomization *Hammel, P. J Clin Oncol 2013;31:LBA4003 [abstr]
HCC
• Sorafenib in Child’s Pugh A patients is SOC in advanced disease
• Sorafenib may be SELECTIVELY used in select patients with Child’s Pugh B
• Sorafenib MAY NOT be used following locoregional procedures , including curative ones.
Phase 1/2 Safety and Antitumor Activity of Nivolumab in Patients With Advanced
Hepatocellular Carcinoma (HCC): CA209-040
Anthony B. El-Khoueiry,1 Ignacio Melero,2 Todd S. Crocenzi,3 Theodore H. Welling III,4 Thomas Yau,5 Winnie Yeo,5 Akhil Chopra,6
Joseph F. Grosso,7 Lixin Lang,7 Jeffrey Anderson,7 Christine dela Cruz,7 Bruno Sangro2
1University of Southern California Norris Comprehensive Cancer Center, Los Angeles, CA, USA; 2Clinica Universidad de Navarra and CIBERehd, Pamplona, Spain; 3Providence Cancer Center, Portland, OR, USA; 4University of Michigan, Ann Arbor, MI, USA; 5University of Hong Kong, China; 6Johns Hopkins Singapore International Medical Centre, Singapore; 7Bristol-Myers
Squibb, Princeton, NJ, USA
Abstract LBA 101
Maximal Change in Target Lesions From Baseline
120
100
80
60
40
20
0
-20
-40
-60
-80
-100
Patients (N = 40)†
Chan
ge in
Tar
get L
esio
n
From
Bas
elin
e, %
Uninfected
HCV
HBV
Confirmed response *
* * * * * *
* * †2 uninfected patients not shown: 1 had disease progression before the first assessment; 1 had a maximal change of +23% ‡Patient with resolved HCV infection
‡
41
Take Home Messages: Non-CRC GI • Few practice changes in 2015, however:
– Highlights • Emering role of immune-based therapies in EGC and HCC • Emerging potential for biomarker selection in pancreas
adenocarcinoma: Hyaluronan-High – needs validation
– Lowlights • End of MET ab targeting in EG cancers • End of erlotinib era in pancreas adenocarcinoma
Courtesy Eileen O’Reillye ,MD. MSKCC