Tumor Necrosis Factor a Regulates in Vivo Intrapulmonary ...
Transcript of Tumor Necrosis Factor a Regulates in Vivo Intrapulmonary ...

American journal of Pathology, tol. 142, No. 6, June 199.3Coptright © Amitericani Socieltior Investigative Pathology
Tumor Necrosis Factor a Regulates in VivoIntrapulmonary Expression of ICAM-1
Michael S. Mulligan,* Ara A. Vaporciyan,*Masayuki Miyasaka,t Takuya Tamatani,t andPeter A. Ward*From the Departnent o1f Pathologiy.* the lniversitiy ofMlichigan medical School. Annii Arbor Mlichigani; anld theDepartment ofIjmnunologv.t TokioMlletropolitan Inistituite ofMedical Scienice, Bunkyio Japan
Lung injuryfollowing deposition ofIgG immunecomplexes is neutrophil-dependent and requiresboth tumor necrosisfactor a (TNFa) and CD18. Inthe current studies, we have evaluated the rela-tionship between TNFa and expression of intra-cellular adhesion molecule-i (ICAM-1) in vitroand in vivo. In both rat pulmonary artery endo-thelial ceUs and human umbilical vein endothelialcells, TNFa induced an early (within 60 minutes)increase in ICAM-1 expression, followed by apeak at 6to 8 hours, with relatively stable expres-sion at 24 hours. Expression ofE-selectin did notshow the early phase (within 60 minutes) of up-regulation, peaked at 4 hours, and then declinedthereafter. Using a radioimmunochemical assayin vivo, it was demonstrated that intrapulmonarydeposition of IgG immune complexes caused aprogressive increase in ICAM-1 expression inlung over an 8-hourperiod In animalspretreatedwith antibody to TNFa, the intrapulmonary ex-pression of ICAM-1 was significantly reduced.These results were confirmed by immunoperoxi-dase analysis of lung tissue. It was also shownthat airway instillation of TNFa caused up-regulation ofICAM-1 in lung. These data supportthe concept that deposition ofIgG immune com-plexes in lung induces intrapulmonary up-regulation of ICAM-1 in a manner that is TNFa-dependent. (AmJPathol 1993, 142:1739-1749)
resulted in the rolling phenomenon in which neutro-phils exhibit intermittent adhesive contacts with theendothelial surface under conditions of shear stress.1-3 The neutrophil molecules that are reactive withendothelial selectins seem to be the oligosaccharidesialyl Lewisx and related compounds (reviewed in ref.4). Leukocytic 12 integrins, leukocyte functionantigen-1 (CD1 1 a/CD1 8), and Mac-1 (CD1 1 b/CD18),are also brought into play and are reactive with endo-thelial intercellular adhesion molecule-1 (ICAM-1),the outcome of which is firm adhesive interactionsbetween neutrophils and the endothelial surface, set-ting the stage for transmigration.4 Up-regulation ofendothelial selectins as well as leukocytic Mac-1 alsoallows for further engagement of adhesion-promotingpathways.
The IgG immune complex model of lung injury hasbeen studied in some detail. In this inflammatorymodel, neutrophils are recruited into the interstitialand intra-alveolar compartments where parenchymalcells are injured by a combination of toxic oxygen andL-arginine derivatives.56 It is also known that TNFaand interleukin-1 (IL-1) are generated in the course ofthese inflammatory reactions and that their blocking(by antibody or by the use of natural antagonists) istissue-protective and results in diminished neutrophilrecruitment.6 6 We have also recently demonstratedthat blocking of ICAM-1 is tissue-protective in a man-ner in which neutrophil recruitment is attenuated (Mul-ligan MS, Wilson GP, Todd RF, Smith CW, Varani J,Issekutz TB, Miyasaka M, Tamatani T, Rusche JR, Va-porciyan AA, Ward PA: Role of b1, b2 integrins andICAM-1 in lung injury following deposition of IgG andIgA immune complexes. Submitted for publication).
In the current report, we provide quantitative evi-dence for the in vivo up-regulation in lung of ICAM-1during IgG immune complex deposition and demon-strate that anti-TNFa significantly reduces the in-crease in lung ICAM-1. Intrapulmonary instillation (via
Adhesion molecules of both neutrophils and endo-thelial cells seem to be required for the eventual trans-migration of leukocytes beyond the vascular barrier.Engagement of the endothelial selectin (E- and P-)with counter receptors in the surfaces of neutrophils
Supported in part by NIH grant HL-31963.
Accepted for publication January 4, 1993.
Address reprint requests to Dr. Peter A. Ward, Department ofPathology, The University of Michigan Medical School, 1301 Cathe-rine Street, Box 0602, Ann Arbor, MI 48109-0602.
1 739

1740 Mulligan et alAJPJiule 1993, Vol. 142, No. 6
the airways) of TNFa also results in the up-regulationof ICAM-1. These data provide evidence for a directrelationship in vivo between the role of TNFa in up-regulation of ICAM-1.
cold temperature compound, snap-frozen, and fro-zen tissue sections obtained.
Endothelial Cell Cultures
Materials and Methods
Reagents
Unless otherwise noted, allchased from Sigma ChemicalMO).
reagents were pur-
Company (St. Louis,
Monoclonal Antibodies
Antibody to rat ICAM-1 (designated 1A29) was de-veloped according to details provided in a recentpublication.9 This antibody reacted with an 85- to89-kd epitope present on cytokine-activated ratendothelial cells. The antibody was shown to recog-nize rat ICAM-1 (based on its ability to inhibit homo-typic aggregation of T cell blasts induced by phyto-hemagglutinin), by analysis in sodium dodecylsulfate-polyacrylamide gel electrophoresis of theantigen precipitated, by antigen distribution on fro-zen sections of postcapillary high endothelialvenules, and by cytokine-induced up-regulation ofthe antigen on rat endothelial cells.9 The antibodywas employed for immunohistochemical analysis oftissues and cell monolayers and for in vivo detec-tion of ICAM-1, as described below. Murine IgG1monoclonal antibody to human ICAM-1 (R6.5) was
kindly provided by Dr. C.W. Smith (Baylor College ofMedicine, Houston, TX).
Animal Model of Immune ComplexAlveolitis
Male Long-Evans, specific pathogen-free, 300 to350 g rats (Charles Rivers Breeding Laboratories,Inc., Wilmington, MA) were used for these studies.After ketamine-induced anesthesia (50 mg keta-mine/kg body wt.), 2.5 mg rabbit polyclonal IgG richin antibody to bovine serum albumin (anti-BSA, Or-ganon Teknika, West Chester, PA) were instilled in-tratracheally.10 The antigen, 10 mg bovine serum al-bumin (BSA), was then injected intravenously. Someanimals received 1.0 ml of rabbit serum rich in anti-body to TNFa, whereas reference positive controlsreceived 1.0 ml preimmune rabbit serum (intrave-nously administered immediately following the injec-tion of BSA). Animals were sacrificed 4 hours later,and the lungs inflated with 7 to 9 ml of optimum
Human umbilical vein endothelial cells (HUVECs)were isolated by collagenase treatment of umbilicalcords and the cells plated onto gelatin-coated plas-tic flasks. Dulbeco's modified Eagle's medium (withHam's F-12 and 20% heat-inactivated fetal calf se-rum) was supplemented with 2 mmol/L L-glutamine,50 lU/ml penicillin, 50 mg/ml streptomycin, 25 pg/mlendothelial cell growth supplement (CollaborativeBiomedical Research Inc., New Bedford, MA) andbovine heparin (15 units/ml) to maintain the cells.HUVECs were used between the first and third pas-sage. The monolayers were characterized by acobblestone appearance with specific staining forvon Willebrand factor. Rat pulmonary artery endo-thelial cells (RPAECs) were maintained in Dulbeco'smodified Eagle's medium (with 10% heat-inacti-vated fetal calf serum) which was supplementedwith 2 mmol/L L-glutamine, 50 lU/ml penicillin, and50 mg/ml streptomycin. These cells have been de-scribed in detail elsewhere.11
Immunohistochemical Assays for ICAM- 1and E-Selectin
Confluent monolayers of HUVECs and RPAECs11 in96-well flat-bottomed plates were obtained by seed-ing each well with 5 x 104 cells. Recombinant TNFa(25 ng/ml) was added to the appropriate wells forthe indicated times and the plates incubated at 37C with 5% CO2. Plates were then inverted and fixedwith 1% paraformaldehyde in phosphate-bufferedsaline (PBS) supplemented with 2% heat-inacti-vated fetal calf serum and 1% Tween 20 (PBS) for10 minutes. The cells were then washed with PBSand blocked with 5% nonfat dry milk in PBS for 45minutes. The primary anti-ICAM-1 antibody (5 pg/ml), in PBS, was added for 45 minutes, followed byblocking for an additional 10 minutes. A 1:1000 di-lution of the secondary antibody (rabbit anti-mouseIgG horseradish peroxidase conjugate; Dako Corp.,Carpinteria, CA) was then added for 40 minutes, fol-lowed by addition of the substrate (o-phenylene-diamine dihydrochloride). After 30 minutes, the re-action was stopped with 3 mol/L sulfuric acid andthe optical density at 490 nm determined in anenzyme-linked immunosorbent assay reader (Bio-Tek Instruments, Inc., Winooski, VT).

TNFa and ICAM-1 in Lung 1741A/P/tune 19923, l'ol. 142, Ao. 6
Lung Instillation of TNFa
Rats received intratracheal instillations of 200 unitsrecombinant human TNFa (Genentech Corp., SouthSan Francisco, CA) in 0.3 ml of saline. Animals weresacrificed 4 hours later and lungs inflated with 7 to9 ml of optimum cold temperature compound,snap-frozen, and sections obtained for immunohis-tochemical analysis.
Immunohistochemical Analysis of RatEndothelial Cells and Lung Tissue
Monolayers of RPAECs on plastic slides were incu-bated with 50 ng/ml human recombinant TNFa for 4hours at 37 C in a humidified chamber, washed withPBS, and fixed with acetone. Monolayers of stimu-lated and unstimulated RPAECs were then incu-bated with anti-ICAM-1 (1.0 ng/ml) for 45 minutesand the bound antibody detected by immunoperox-idase techniques using the Vectastain biotin/avidin-peroxidase system (Vector Laboratories, Inc., Burl-ingame, CA).1` Frozen sections of lungs (from IgGimmune complex-injured lungs, IgG immune com-plex-injured lungs of animals also treated with anti-body to TNFa, lungs instilled with TNFa, and lungsinstilled with saline) were mounted on poly-L-lysine-coated slides, fixed with acetone, and reacted withthe anti-ICAM-1 preparation as described above,followed by the staining procedures describedabove. Although constitutive expression of ICAM-1in rat lung tissue would be expected to be demon-strated in negative control lung, staining procedureswere employed to avoid staining of normal lung.Negative staining of control lungs from ICAM-1 wasachieved by using increasing doses of antibodiesuntil normal lung failed to reveal staining.
Transmission Electron Microscopy
Where indicated, lungs were fixed by vascular per-
fusion with 4% glutaraldehyde in 0.1 mol/L cacody-late buffer (pH 7.4) containing 5% sucrose, followedby standard postfixation in uranyl acetate and leadcitrate, plastic imbedding, and processing for trans-mission electron microscopy.
In Vivo ICAM-1 Quantification
The antibody (1A29) to rat ICAM-1 was labeled with1251 by standard technology (chloramine T). An iso-type matched antibody, MOPC-21, was also labeledto serve as a control. Male Long-Evans specific
pathogen-free rats (300 to 350 g) were subjected todevelopment of IgG immune complex alveolitis, un-der conditions of ketamine-induced anesthesia, asdescribed above. In the negative control group, theintravenous infusion of BSA was omitted. Some ani-mals received 1.0 ml of rabbit serum rich in anti-body to TNFa (described in ref. 7) whereas othersreceived 1.0 ml preimmune rabbit serum (intrave-nously injected immediately preceding the injectionof BSA). Fifteen minutes before sacrifice (at 3.75hours), animals were injected intravenously with 500p1 of PBS containing either 1.5 pCi [1251]anti-ICAM-1together with unlabeled anti-ICAM-1 in the amountsindicated in the text or identical amounts of radiola-beled and unlabeled MOPC-21. The animals werethen sacrificed and the pulmonary circulationflushed with 10 ml PBS. Total radioactivity in thelung was subsequently determined. Radioactivitymeasurements for detection of ICAM-1 were cor-rected by subtraction of radioactive counts due tothe presence of irrelevant [1251]MOPC-21.
Statistical Analysis
All values were expressed as the mean ± standarderror of the mean. Paired Student's t-tests and one-way analysis of normal variance (ANOVA) togetherwith Fisher protected least significant difference(PLSD) or Scheffe F-tests were employed usingStatview 11 (Abacus Concepts, Berkeley, CA) statis-tical software.
Results
Quantitation in Vitro Measurements ofEndothelial ICAM-1
RPAECs stimulated with human recombinant TNFcawere evaluated by a quantitative immunohistochem-ical assay described above. Expression of ICAM-1was measured as a function of time (0 to 24 hours).As shown in Figure 1A, there was substantial base-line expression (at time 0) of ICAM-1, with a mea-surable increase within the first hour, followed by aplateau and then another increase occurring be-tween 4 and 8 hours. This pattern has been notedin three separate experiments. There was no differ-ence between the amount of ICAM-1 measured at 8hours and 24 hours. Although early passages ofthese cells also showed up-regulation of E-selectin,the later passages failed to demonstrate the up-regulation (data not shown). When HUVECs wereused in companion studies, expression of both

1742 Mulligan et alAJP,June 1993, Vol. 142, No. 6
Effect of Duration of TNFa Exposure onEndothelial Expression of Adhesion Molecules
3000
2000
1 000
Tissue Expression of ICAM- 1
When frozen-sections from lungs of rats that re-~~~~ * r I - - i _ ~. C1e A *ceived intratracheal instillation ot 300 pl anti-BSA in
the absence of intravenously instilled BSA werestained immunohistochemically for ICAM-1, therewas little detectable expression of ICAM-1 (Figure2A). This was in striking contrast to lungs obtained
-ICAM-1 from animals 4 hours after deposition of immunecomplexes, in which an acute alveolitis had oc-
P4.05 curred. In this case, there was evidence of ICAM-1presence in the pulmonary venules and interstitialcapillaries (Figure 2B). When companion animalsIr-rA ir;r- r4 ;r-trnr- drnr% r% HAnr%citinn nf I4r. imn
U. nuvct_9 * *
T*/~~~~~~~~~
V1-0 2 4 6 8
Time of TNFa Exposure(hours)
Figure 1. Quantitative mieasurement of ICAM -1 qltcstimuiiilationi of RPAECs as a fiunction of tionCe anid e>(A). HIUECs were also stiniulated trith 7TFa anlICAVM-] anid E-.selectin expression (B). Statistical a,
med using AXVOA (P < 0.001) Jbllowed by nam!htests, Fisher PLSD anid the ScheJf F-te-st, uith signifi(P < 0.05) indicated uith ani asterisk, uhen the reftinie 0.
ICAM-1 and E-selectin were measured <of time of exposure of cells to TNFa (Fithe case of E-selectin, very little basawas found, and the up-regulation rose
tween 1 and 4 hours, at which timecurred, followed by a decline. InHUVECs, there was substantial basal ex
time 0) of ICAM-1 (approximately 10-than that found with E-selectin), and cleof early and increasing expression of IC)the first 3 hours, followed by a plateaugressive rise from 4 to 6 hours. After tIas late as 24 hours, there seemed to bpression of ICAM-1. These data si
ICAM-1 expression can occur rapidly aflial cell stimulation with TNFa and thaision, which peaks at 6 to 8 hours, is s
24-hour period.
unaergoing inirapuimonary cepositiori u1 iyu imT-* mune complexes were also treated systemically
with anti-TNFa, there was loss of staining forICAM-1 in the pulmonary vasculature (Figure 2C).To determine if extrinsic intrapulmonary TNFa wouldcause up-regulation of ICAM-1, 200 units TNFa
- selectin were instilled into the airways and the lung tissueexamined after 4 hours. As is shown in Figure 2D,
* P<.05 staining for ICAM-1 was found in pulmonary venulesand in the interstitial capillary network. In vitro, non-stimulated RPAECs revealed no immunohistochemi-
24 cal staining for ICAM-1 under the conditions ofstaining employed (Figure 2E), whereas cells thathad been incubated for 4 hours in vitro with TNFa
-r TXFa-induced stained intensely for ICAM- 1 (Figure 2F).vposlre to TAFaid evalu'ated fbrnIalsis was perntip/l cosparison In Vivo Quantitative Measurement oficanit difjirences ICAM- 1?rence poinit was
A technique (described above) was developed forthe measurement in vivo of ICAM-1 expression inlungs of rats undergoing intrapulmonary deposition
as a function of IgG immune complexes. Injury in this model hasigure 1B). In been shown to be CD18 and E-selectin-dependent.expression 1213 Three different doses (75, 125, 175 pg) of anti-rapidly be- ICAM-1 were injected intravenously. The total
peaking oc- amount of [1251]anti-ICAM-1 radioactivity (1.5 pCi)contrast, in infused was maintained at a constant level in spite<pression (at of different levels of unlabeled anti-lCAM-1 em--fold greater ployed. The antibody was infused 15 minutes be-Lar evidence fore sacrifice (which occurred 4 hours after initiationAM-1 during of intrapulmonary deposition of immune complex-and a pro- es). The negative controls received an intratracheal
his time and instillation of anti-BSA in the absence of intravenouse stable ex- BSA. After sacrifice, the lung vasculature was per-uggest that fused with 10 ml PBS and lung radioactivity countster endothe- assessed. Radioactivity present in 1.0 ml blood ob-t its expres- tained from the inferior vena cava at the time of sac-table over a rifice was also determined. For these studies, com-
panion groups of rats (both negative and positive
Ec0
._
0c:
._-QL0
n~ )V
-- --
..nn -
IR 141 IVF:r

TNFa and ICAM-1 in Lung 1743AJPJune 1993, Vol. 142, No. 6
.1"
rsl
_I
..
...A-, .. ,,f,........
#I. .A , _ . -k
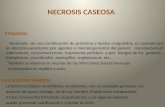
Figure 2. Immunohistochemical stainiing for the presence of enidothelial leukocyte adhesioni molecule-1 in frozenz sections of rat lung (A to D) andmonzolavers ofRPAECs (E, F). No stainzing for ICAA-1 uasfound ini Ilungfrom negative conitrols (A) butt initenise staininlg of venuiles and initerstitialcapillaries was evident 4.0 hours after deposition of IgG imimune complexes (B). In animals pretre-ate-d with anti-.JFa anid unldergoinlg IgG im-niune comnplex deposition, uip-regutlationi of ICAVJ-I was blocked (C). Four houorus aftier airwal, instillation of 7\Fa alonie, marked uip-regiulationi ofICAMI-1 occurred in the pulmonary vasculature (D). nIstimnulated mno/iolayers of RPAECs did niot denionstrate staining for ICAMI-I (E). However. 4houirs afier incubation nrith TN.'Fa, intense expression ofjICAM-1 was detec-table (F). (.1agnif/icationw A to D X 150; E anod F: X 400.)
controls, as described above) were treated at 75,125, and 175 pg MOPC-21 (irrelevant murine IgG1)together with 1.5 pCi [1251]MOPC-21, to measurenonspecific lung uptake of radioactivity, whichwould be due chiefly to a permeability change ac-companying the development of lung injury. Forthese three doses of MOPC-21, the amounts of non-specific accumulation of MOPC-21 in immune com-plex injured lung tissue were 7.3%, 28.1%, and
22.1% (respectively) of total MOPC injected. When150 pg MOPC-21 (together with 1.5 pCi [1251]_MOPC-21) were infused into rats without lung injury,the accumulation of MOPC-21 was 7.5% of the totalamount of radioactivity in 1.0 ml blood. Immunecomplex-injured rats were infused (at 3.75 hours)with 75, 125, or 175 pg anti-lCAM-1 together with1.5 pCI [1251]anti-ICAM-1; the resulting patterns oflung radioactivity are shown in Figure 3. With the 75
IW 1.
k.. .:1-
4-,&!,
.....
4 0. -'.1.11
uh..
k'

1744 Mulligan et alAJPJiune 1993, VW'l. 142, NVo. 6
Effect of Increasing Dose of Unlabeledanti-ICAM-1 on Binding of 1251-anti-ICAM-1
m000,
20000-
10000t
0-
T
75 Lg 125 ig 175 pg
Dose of Unlabeled antiICAM-1Figure 3. Lptak.e at 4 hours bh IgG ininione comiiplex-injured luings.as a fonction of doses of aniti-ICA I-I in the presence of constantamiounts (1.5 /CL) of[125IIanti-ICA -1. Llung radioactivitie was inlea-sured 15 miinutes after inifiusiont irith anti-ICAJI-1. For- each ierticalbar n = 5.
pg dose, there was a high level of radioactivity ac-
cumulation in the lung, which fell to half when dosesof 125 and 175 pg anti-lCAM-1 were employed. Onthe basis of these studies, in all subsequent experi-ments, 150 pg anti-lCAM or MOPC-21 were usedtogether with 1.5 pCi (1251) of corresponding anti-body. The data obtained from the use of MOPC-21(measuring nonspecific accumulation due topermeability change) were used to correct the dataderived from the use of anti-lCAM-1.
To explain further how these measurements were
made, data from a representative experiment are
shown in Table 1 in which radioactivity counts inlung after intrapulmonary deposition of IgG immunecomplexes were determined. As indicated above,the [1251]lgG MOPC-21 or 1A29 (anti-lCAM-1) prep-
arations containing 150 pg IgG and 1.5 pCi [1251]_lgG were infused 15 minutes before sacrifice. Accu-mulation of MOPC-21 radioactivity (c.p.m.) was very
small in the negative control (1,836 ± 671) when
compared to lung accumulation of [1251]anti-ICAM-1, which was 12.2-fold higher (24,460 + 918).This would be consistent with constitutive expres-sion of ICAM-1 in normal lung. In the injured lung,[1251]MOPC-21 increased 2.6-fold above that in theuninjured lung (to 4,881 + 511), reflective of leak-age of MOPC-21 associated with a damaged vas-culature. In the positive controls, the lung uptake of[1251]anti-ICAM-1 nearly doubled to 42,442 + 1,951;this was nearly ninefold above the amount of radio-activity in the positive controls infused with [1251]-MOPC-21. If the data in the anti-lCAM-1 infusedgroups were not corrected for the MOPC-21 accu-mulation, the expression of ICAM-1 in lung wouldhave increased by 73.5%. When the positive anti-ICAM-1 infused was corrected by subtraction of theparallel [1251]MOPC-21 data, ICAM-1 expression in-creased by 66.0%. In this and in all subsequentdata to be presented, [1251]anti-ICAM-1 counts werecorrected by subtraction of [1251]MOPC-21 countsbefore percent changes in ICAM-1 expression werecalculated. Data in Table 1 also show the expecteddifferences in retention of [1251]anti-ICAM-1 versus[1251]MOPC-21. In the case of the latter, there was asixfold increase in blood radioactivity at the time ofsacrifice, consistent with constitutive vascular ex-pression of ICAM-1.
Time Course for in Vivo Expression ofLung ICAM-1
Lung inflammatory reactions were induced in ratsby the deposition of IgG immune complexes. Theamounts of lung ICAM-1 were measured by the ra-dioactive technique (described above). The dataare shown in Figure 4. The negative controls con-sisted of animals with intratracheal administration ofanti-BSA but with omission of intravenously injectedBSA. The positive controls were similarly treated butreceived an intravenous infusion of BSA. All animalsreceived 150 pg anti-lCAM-1 along with 1.5 pCi
Table 1. Representative Luntg Radioactiv'ity ini IgG ilnizmine Complex-Indiced Luniigs*
Lung radioactivity§ Blood radioactivity§Conditiont [1251]lgG, infused5 (mean ± S.E.M.) (mean ± S.E.M.)
Negative control MOPC-21 1,836 ± 671 12,485 ± 691Positive control MOPC-21 4,888 + 511 11,900 ± 800Negative control anti-ICAM-1 24,460 ± 918 2,113 ± 184Positive control anti-lCAM-1 42,442 ± 1,950 2,019 ± 174
Lungs 8 hours after IgG immune complex deposition. Data are derived from an experiment described in Figure 4. For each entry data,n 4.
t Negative controls received intratracheal instillation of anti-BSA in the absence of intravenously infused BSA. In positive controls, both in-jections were made.
t 150 pg unlabeled IgG, together with 1.5 pCi IgG1 (containing 1 pg IgG1).§ Lung radioactivity expressed as total lung c.p.m., whereas blood radioactivity was cpm/ml blood.
Ed.U
wU.2:0U
aaJ

TNFa and ICAM-1 in Lung 1745AJPJuine 1993, Vol. 142, No. 6
Effect of IgG Immune Complex-inducedAlveolitis on Intrapulmonary ICAM-1 Expression
NMa vsCo"P vo_
E
d.i
I
C0
NouIve 2 3 4 6 8Control hours hours hours hours hours
Figure 4. Measurement oj lonlg ICAAI-I as a Jintctioni of time aJictrintrapulmonzar depositioni oj IgG immune comple.xes All statisticalcomparison% were to the niegative conitrol grouip. In all cases. Ilung,counts uere corrected for luniig accumulationi of/'J512./ PC. 21 candthsce values suhtracted from the /'25IIanlti-ICAlI-I valhes to correctobr inicreased vascularpermeability For each vertical bar, n =4 Sta-tistical anialy5is uas per/brmed uisinzg ANOVA (P' < 0 OO1)follow'ed bymultiple comparisont tests, Fisher PLSD anid Schebffe F-test (P < 0 005).
[1251]anti-ICAM-1. All animals received identicalamounts of radioactivity and, as stated, the nega-
tive and positive control values were corrected bysubtraction of radioactivity counts in negative andpositive controls receiving [1251]MOPC-21. As is ev-
ident in Figure 4, there was no measurable differ-ence between the negative controls and the posi-tive controls at 2 and 3 hours. However, at 4, 6, and8 hours, lung-specific radioactivity increased abovethe negative control groups by 47% (P < 0.01),46% (P < 0.01), and 73% (P < 0.01), respectively.Thus, it would seem that this technique demon-strates substantial increases in detectable lungICAM-1 after intrapulmonary deposition of IgG im-mune complexes. The inability to detect measur-
able increases at earlier time points may reflect therelative insensitivity of these techniques.
Effects of Anti-TNFa on Lung Expressionof ICAM- 1 after Immune ComplexDeposition
It is known that anti-TNFa is protective in the IgGimmune complex model of lung injury and thatthese protective effects are related to reduced tis-sue accumulation of neutrophils.7 The data in Figure2 suggest that, by immunohistochemical analysis ofrat lung, anti-TNFa suppresses expression ofICAM-1 after intrapulmonary deposition of IgG im-mune complexes. The method of in vivo measure-
ment of lung ICAM-1, as described above, was em-
ployed in rats undergoing IgG immune complex-
induced injury. Negative controls received airwayinstillation of anti-BSA in the absence of intravenousBSA, whereas positive controls received both mate-rials. Two groups of animals with intrapulmonary de-posits of BSA/anti-BSA were evaluated at 4 and 8hours. Comparisons were made not only to the neg-ative controls (sacrificed 4 hours after airway instil-lation of anti-BSA in the absence of intravenouslyadministered BSA), but also to companion positivecontrols that had been pretreated with anti-TNFa.The data are shown in Figure 5, where the effects ofanti-TNFa on up-regulation of lung ICAM-1 followingimmune complex deposition were evaluated. Whencompared to the negative controls, lungs containingIgG immune complexes demonstrated increasedICAM-1 expression of 47% (P < 0.001) and 66% (P< 0.001) at 4 and 8 hours, respectively. When ani-mals were pretreated with anti-TNFa, the expressionof ICAM-1 in lungs containing IgG immune com-plexes fell by 75% (P = 0.009) and 61% (P =
0.006) at 4 and 8 hours, respectively, when com-pared to reference positive controls. Thus, in ac-cord with the immunohistochemical features de-scribed in Figure 2, treatment of rats with anti-TNFasignificantly depressed IgG immune complex-induced increases in lung ICAM-1.
Increased ICAM-1 Expression in Lungafter Instillation of TNFa
Two hundred units of TNFa were instilled into theairways of rats and the uptake of [1251]anti-ICAM-1in lung was measured at 4 and 8 hours and com-pared to the findings in negative controls. Again, in
Effect of Anti-TNFa on ICAM-1 Expression InIgG Immune Complex-induced Alveolitis
EJ
a
Co
3Mu
3oo0o
P.001-r
o NHowsl ColU Po_usioNs* P..Uv. Corsg+
aIINIF*
T I
INqslv 4 aControl hours hours
Figure 5. ICAM-1 expression 4 anid 8 bows after intrapnlmonargdeposition ofIgG immtune complexes. The effects ofpretreatmentt uithanti-TNFa on ICAM-1 expression are also shown. For each verticalbar, n = 5. Statistical analvsis performed tusing Stuident's t-tests.
200 ff] --

1746 Mulligan et al4/P.mwme 199.3, Vol. 142, No. 6
every experiment, companion negativecontrols received [1251]MOPC-21 to cccumulation of lung radioactivity due tochanges. Radioactivity values found irwere then subtracted from the radioactnegative and positive controls that recanti-lCAM-1. The corrected data are sure 6. As compared to the negative corinstillation of PBS, with sacrifice 4 hothose animals receiving airway instillatthere were significant increases in lungpression at 4 and 8 hours, with 27%and 35% (P = 0.004) increases, respe(as would be predicted and as is consisdata in Figure 2, airway instillationcreases lung ICAM-1 expression, as dmonary deposition of IgG immune corrure 4).
Morphological Correlates ofImmunohistochemical Findings
Morphological evaluation by transmissmicroscopy of lung tissue revealed thato control lungs (in the absence of inplexes, Figure 7A), the lungs from ratintra-alveolar deposits of immune comonstrated the anticipated intra-alveolarand fibrin deposits, along with numephils with electron-dense cytoplasmi((Figure 7B). In anti-TNFa-treated animEing immune complex deposition, therea complete absence of neutrophil accthe alveolar compartment and little orof injury (Figure 7C). The lack of histdence of injury in the anti-TNFa treatedthe absence of neutrophils correlal
Expression of ICAM-1 After AirwalInstillation of TNFa
E
di
iUa
la 2500
aIC
N.gtlve 4 hour 8 hourControl
Figure 6. I.MoA,) 1(A4I-I cxpwes.sion 4 and 8 hoin)s q/fl0tioI( oJ/200 units oJ 7:\Th 1o each vertical bha n
and positive)rrect for ac-permeabilitythe groups
:ive counts of,eived [1251]ahown in Fig-itrols (airwaylurs later), in-ion of TNFa,] ICAM-1 ex-
blocked expression of intrapulmonary ICAM-1 (Fig-ure 2C). The airway instillation of TNFa, whichcaused up-regulation of ICAM-1 (Figure 2D), wasassociated morphologically with bleb formation in-volving interstitial capillary endothelium and alveolarepithelial cells, marked interstitial edema, and focalintra-alveolar hemorrhage (Figure 7D).
Discussion(P = 0.043) The data in this and in other recent studies providectively. Thus, support for the concept that events leading to lung;tent with the injury following intrapulmonary deposition of IgG im-of TNFa in- mune complexes require the participation of TNFa7loes intrapul- and ICAM-1 (Mulligan et al: Role of b1, b2 integrinsiplexes (Fig- and ICAM-1 ... ) and that there is a link between
TNFa appearance and ICAM-1 expression. WhenTNFa was blocked, there was a substantial reduc-tion in the lung expression of ICAM-1, whether mea-sured by immunohistochemical techniques or by ra-dioimmunochemical approaches. The findings
,ion electron support the interpretation that lung macrophaget, in contrast generation of TNFa (and perhaps IL-1) results innmune com- vascular expression of ICAM-1, which then leads to:s containing engagement of vascular ICAM-1 with the (2 inte-plexes dem- grins (leukocyte function antigen-1, Mac-1) of thehemorrhage neutrophil, followed by transmigration of the neutro-rous neutro- phil into the interstitial and intra-alveolar compart-c inclusions ments. In the last step, the cell migration responseals undergo- is presumably due to influences of chemotactic fac-was virtually tors, such as C5a. We have previously shown that:umulation in engagement of endothelial E-selectin is also a pre-no evidence requisite in this lung inflammatory reaction, presum--ological evi- ably via its reactivity with sialyl Lewisx and relatedanimals and oligosaccharides on the surfaces of neutrophils.12te with the These events would be consistent with the tripartite
sequence of selectin engagement resulting in therolling of neutrophils along the endothelial surface;
y ICAM/32 integrins engagement causing their firmattachment to the endothelium; and, finally, transmi-gration of neutrophils under the influences of
o Ngwcnwd chemotactic factors as has been suggested byothers. 1-3
The in vivo method for the measurement ofICAM-1 has confirmed the evidence obtained im-munohistochemically regarding the relationship be-tween TNFa and ICAM-1 expression. What seemsclear from the data is the prominence of constitu-tively expressed ICAM-1, as revealed by the re-quirement for a relatively large amount of anti-ICAM-1 that must be injected to be able to measureup-regulation of lung ICAM-1 (Figure 3). The sameconclusion derives from the substantial removal of
04
Ip--uQj
F
_I I
aowuu -
III-An

TNFa and ICAM-1 in Lung 1747A/P.june 1993, Ikol. 142, No. 6
Figure 7. Transmission electron inicroscoplv ofJ r-at longs. In comiparisosn to saline-inistilled. ohich appeared n1orm'7Cal (A). inl the IgG immiiiiiunecomipleX-injiured Ioings, there eremC)ar-ked inlcreases in intra-alieolar accumiulation of neittrophils, benionohage. and fibrin deposition. as well casendothelial cell blebhing andcl interstitial edema (B). Long sectioiis fioin rats llndergoing immune comiplex dep/)si/ion hot (1s1o treatedl iiith anti-TViFa (C) appear-ecd similar to negative control lonlgs (A). In animals receiving intratracheal iostillationi 0?/ lTslc aloiie. lmlgs shoii'ed blebbing o]'enclothelial cells, intraiascu/lar acciumuilation ojneutrophils. intersstitial edemia. ailnd ocal introc-alv'eolar hbemorrhaige (D). (fagnification.i X 2000
[1251]anti-ICAM-1 from the blood, especially as com-pared to the slow removal of [1251]MOPC-21 (Table1). This would suggest that approaches designedto block ICAM-1 expression in vivo in humans maybe complicated by the relatively large quantity ofICAM-1 that is constitutively expressed systemically.The data pertaining to the in vivo time course for ex-pression of ICAM-1 (Figure 4) are consistent withthe in vitro technique of quantitatively measuringICAM-1 on TNFa stimulated endothelial cells (Fig-ure 1), where up-regulated ICAM-1 reaches a pla-teau by 6 to 8 hours. What is of interest in vitro is therather rapid and early expression of ICAM-1, withinthe first 2 hours, even though this is still only a frac-tion of the total increase in measurable ICAM-1 ex-pression in TNFa-treated endothelial cells, it is notsurprising in view of the report by Wertheimer etal,14 who described a peak in transcriptional ex-
pression of messenger RNA for ICAM-1 within 30minutes after exposure of HUVECs to TNFa. Fur-thermore, the finding of ICAM-1 in guinea pig lungswithin 90 minutes after lung perfusion with TNFaalso indicates that ICAM-1 expression can occurrather early.15 Interestingly, the pattern of E-selectinexpression in HUVECs is different, exhibiting virtu-ally no basal expression, showing a lag (>1 hour)before any measurable expression, which peaks at4 hours and then recedes. The features of in vitroexpression of ICAM-1 by endothelial cells are con-sistent with published reports for this molecule.16-18The in vitro expression of E-selectin by TNFa-stimulated endothelial cells shows a relatively earlydown-regulation, commencing after 4 hours. Thisloss of E-selectin in the endothelium in vivo mayrepresent a natural mechanism for turn-off of the in-flammatory process. It is also possible that other

1748 Mulligan et alA/P .June 1993. Vol. 142. .V. 6
cytokines, such as IL-4 and IL-10, both of whichhave been demonstrated capable of reducing ex-pression of TNFa,1920 are being produced in vivoand play a role in regulation of the inflammatory re-sponse. The combined effects of such events maynegate the effects of continued expression ofICAM-1 and may override the ability of ever increas-ing ICAM-1 expression in vivo to perpetuate and in-tensify the inflammatory response.
Obviously, there may be other factors affectingthe amount of lung damage resulting from thesephlogistic events. For instance, it has been previ-ously shown that in the IgG immune complex modelof lung injury bronchoalveolar lavage (BAL) fluidscontain both TNFca and IL-1.7,21 Furthermore, block-ing of either cytokine (with antibody or by the use ofrecombinant soluble TNFca receptor-1 or recombi-nant IL-1 receptor antagonist) is protective.8 Itseems that TNFa and IL-1 both contribute to eventsrelated to the recruitment of neutrophils, and itseems likely that both function, at least in part, viathe up-regulation of endothelial adhesion mole-cules. It is also possible that these cytokines haveother contributions, such as the priming of phago-cytic cells in the lung for exaggerated generation of02-. Another possibility that militates against a strictin vivo correspondence between the in vitro and invivo appearance of cytokines (and adhesive mole-cules) would be that, early in the intrapulmonary in-flammatory reaction, released TNFa and IL-1 wouldbind to receptors on lung macrophages and on re-ceptors of neutrophils as they accumulate in thelung parenchyma. Furthermore, neutrophil protein-ases would likely inactivate TNFa and IL-1. All ofthese possibilities would explain why there are noclear-cut correlations between appearance in theBAL fluids of TNFa and IL-1, tissue expression ofICAM-1, and development of tissue injury.The ability of exogenously administered TNFa to
induce up-regulation of lung ICAM-1 in rats is notsurprising nor is the fact that the in vivo time coursefor ICAM-1 up-regulation approximates that found invivo in the IgG immune complex model. It seemsthat the airway instillation of TNFa is not an espe-cially effective inducer of lung injury, whether basedas permeability and hemorrhage parameters thatare minimally increased (data not shown) or as as-sessed by morphological findings (Figure 7). Eventhough airway instillation is a relatively ineffectivemode of instillation with respect to induction of in-jury, up-regulation of lung ICAM-1 seems to be ef-fectively induced. The limited evidence of injury andthe absence of neutrophils in lungs of animalstreated with airway instillation of TNFa likely reflect
the fact that up-regulation of ICAM-1 is, per se, nota sufficient event to bring about neutrophil recruit-ment and that engagement of E-selectin as well asgeneration of chemotactic factors must occur be-fore leukocyte emigration can occur. This would bein keeping with the concepts described above.
With respect to other data supporting the role forICAM-1 in the inflammatory response, there is am-ple evidence that ICAM-1 participates in a variety oflung inflammatory responses (reviewed in ref. 22).ICAM-1 dependence has been shown in rabbitphorbol myristate acetate-induced lung injury23and in ischemia-reperfusion events related to unilat-eral pulmonary artery occlusion followed by 2 hoursof reperfusion.24 In both models, a reduction in neu-trophil influx occurred in the anti-lCAM-1-treated an-imals. In the latter model, a quantitative increase inICAM-1 expression in vivo was demonstrated. Inisolated guinea pig lungs perfused with TNFa for 90minutes, increased immunohistochemical evidenceof lung ICAM-1 was found.15 In the same model, in-fusion of anti-ICAM-1 before addition of phorbolmyristate acetate-stimulated neutrophils preventedthe increase in pulmonary artery pressure, pulmo-nary capillary pressure, and pulmonary edemafound in controls, suggesting the requirement forICAM-1 in this model of lung injury. These studiesas well as the findings present in the current papersuggest that ICAM-1 can be up-regulated in vivoand that its expression in the lung may be impor-tant for the full development of neutrophil-mediatedinjury.
References1. Smith CW, Kishimoto TK, Abbass 0, Hughes B, Roth-
lein R, McIntire LV, Butcher EC, Anderson DC: Chemo-tactic factors regulate lectin adhesion molecule 1(LECAM-1 )-dependent neutrophil adhesion to cyto-kine-stimulated endothelial cells in vitro. J Clin Invest1991, 87:609-618
2. Lawrence MB, Springer TA: Leukocytes roll on a se-lectin at physiologic flow rates: distinction from andprerequisite for adhesion through integrins. Cell 1991,65:859-873
3. Von Andrian VH, Chambers JC, McEvoy LM, Bar-gatzerf AR, Arfors KE, Butcher EC: Two-step model ofleukocyte-endothelial cell interactions in inflammation:distinct roles for LECAM-1 and the leukocyte f2 inte-grins in vivo. Proc Natl Acad Sci USA 1987, 88:7538-7542
4. Paulson JC: Selectin/carbohydrate-mediated adhesionof leukocytes, Adhesion Its Role in Inflammatory Dis-ease. Edited by Harlan JM, Liu DY, New York, WHFreeman and Co. 1992, pp 19-42

TNFa and ICAM-1 in Lung 1749AJPJune 1993, Vol. 142, No. 6
5. Johnson KJ, Ward PA: Role of oxygen metabolites inimmune complex injury of lung. J Immunol 1981, 126:2365-2369
6. Mulligan MS, Hevel JM, Marletta MA, Ward PA: Tissueinjury caused by deposition of immune complexes isL-arginine dependent. Proc Natl Acad Sci USA 1991,88:6338-6342
7. Warren JS, Yabroff KR, Remick DG, Kunkel SL, Chen-sue SW, Kunkel RD, Johnson KJ, Ward PA: Tumor ne-crosis factor participates in the pathogenesis of acuteimmune complex alveolitis in the rat. J Clin Invest1989, 84:1873-1882
8. Mulligan MS, Ward PA: Immune complex-induced lungand dermal vascular injury: differing requirements forTNFa and IL-1. J Immunol 1992, 149:331-339
9. Tamatani T, Miyasaka M: Identification of monoclonalantibody reactive with the rat homologue of ICAM-1,and evidence for differential involvement of ICAM-1 inthe adherence of resting versus activated lympho-cytes to high endothelial cells. Int Immunol 1991,2:166-172
10. Johnson KJ, Ward PA: Acute immunologic pulmonaryalveolitis. J Clin Invest 1974, 54:349-357
11. Phan SH, Gannon DE, Varani J, Ryan US, Ward PA:Xanthine oxidase activity in rat pulmonary arteryendothelial cells and its alteration by activated neutro-phils. Am J Pathol 1989, 134:1201-1211
12. Mulligan MS, Varani J, Dame MK, Lane CL, Smith CW,Anderson DC, Ward PA: Role of ELAM-1 in neutrophilmediated lung injury in rats. J Clin Invest 1991, 88:1396-1406
13. Mulligan MS, Varani J, Warren JS, Till GO, Smith CW,Anderson DC, Todd RF, Ward PA: Roles of f2 integrinsof rat neutrophils in complement- and oxygen radical-mediated acute inflammatory injury. J Immunol 1992,148:1847-1857
14. Wertheimer SJ, Myers CL, Wallace RW, Parks TP: In-tercellular adhesion molecule-1 gene expression inhuman endothelial cells: differential regulation by tu-mor necrosis factor-a and phorbol myristate acetate. JBiol Chem 1992, 267:12030-12035
15. Lo SK, Everitt J, Gu J, Malik AB: Tumor necrosis factormediates experimental pulmonary edema by ICAM-1
and CD18-dependent mechanisms. J Clin Invest1992, 89:981-988
16. Bevilacqua MP, Pober JS, Mendrick DL, Cotran RS,Gimbrone MA Jr: Identification of an inducible endo-thelial leukocyte adhesion molecule. Proc Natl AcadSci USA 1987, 84:9238-9242
17. Bevilacqua MP, Stengelin S, Gimbrone MA Jr, Seed B:Endothelial leukocyte adhesion molecule-1: an induc-ible receptor for neutrophils related to complementregulatory proteins and lectins. Science 1989, 243:1160-1165
18. Smith CW, Marlin SD, Rothlein R, Lawrence MB, McIn-tire LB, Anderson DC: Role of ICAM-1 in the adher-ence of human neutrophils to human endothelial cellsin vitro. Structure and Function of Molecules Involvedin Leukocyte Adhesion. Edited by Springer TA, Ander-son DC, Rothlein R, Rosenthal AS, New York,Springer-Verlag, Inc., 1989, pp 170-189
19. Hart PH, Vitti GF, Burgess DR, Whitty GA, Piccoli DS,Hamilton JA: Potential anti-inflammatory effects ofinterleukin-4: suppression of human monocyte tumornecrosis factor alpha, interleukin 1 and prostaglandinE2. Proc Natl Acad Sci USA 1989, 86:3803-3807
20. deWool MR, Abranes J, Bennett B, Figdor CG,deVries C: Interleukin 10 (IL-10) inhibits cytokine syn-thesis by human monocytes: an autoregulatory role ofIL-10 produced by monocytes. J Exp Med 1991, 174:1209-1220
21. Warren JS: Intrapulmonary interleukin-1 mediatesacute immune complex alveolitis in the rat. BiochemBiophys Res Comm 1991, 175:604-610
22. Wegner CD, Gundel RH, Rothlein R, Gordon L: Ex-pression and probable roles of cell adhesion mole-cules in lung inflammation. Chest 1992, 101:34S-39S
23. Barton RW, Rothlein R, Ksiazek J, Kennedy C: The ef-fect of anti-intercellular adhesion molecule-1 onphorbol-ester-induced rabbit lung inflammation. J Im-munol 1989, 143:1278-1282
24. Horgan MJ, Ye M, Gu J, Rothlein R, Malik AB: Role ofICAM-1 in neutrophil-mediated lung vascular injury af-ter occlusion and reperfusion. Am J Physiol 1991,(Heart Circ Physiol 30) 261:H1578-H1584