Triadic relationship between doctor, computer and patient
-
Upload
derek-scott -
Category
Documents
-
view
212 -
download
0
Transcript of Triadic relationship between doctor, computer and patient

htemcting with Computers uol 8 no 4 (1996) 347-363
Triadic relationship between doctor, computer and patient
Derek Scott and Ian N. Purves
Much has previously been said regarding dyadic relationships between physician and patient, use of computers in the consulting room, and human-computer interaction generally. The paper reviews major empirical reports and places them within a triadic framework. A model is presented suggesting that much of the dynamic interaction along any one of the ‘three sides of the triangle’ is lost without consideration of how the third component, the opposite apex, affects the otherwise two-way relationship. As the use of micro-computers within general practice continues to increase, it would appear important to consider all three interacting components when investigating doctor-patient relationships.
Keywords: doctor-patient relationship, computers in medicine
General practitioners/family physicians (GPs) have been at the leading edge of medical computing in developed countries for the past two decades. For instance, within the UK, the Department of Health sponsored the development of a system that recorded consultations for the first time in 1972. The second main impetus for computers in the doctor’s consulting room came ten years later in 1982 with the ‘Micros for GPs’ scheme, funded by the Department of Trade and Industry (HMSO, 1985), which put computers into 137 practices across the UK. But it was in 1987, when two companies (VAMP and Meditel) began offering relatively sophisticated computer systems to GPs free of charge, that practice computing moved towards its present position (Millman ef al., 1995). Having raised this perspective, it must be stressed that this article is not ethnocentrically describing the UK scene. Similar developments are occurring globally from Australia to North America (see, for example, Hovenga and Kidd, 1996; Cesnik, 1996). Issues concerning computer use in doctor-patient consultations within developing countries, such as the high cost, general reservation and fears about computer interference in the relationship, are discussed by Moidu et al. (1995).
The 1993 UK survey showed that the use of computers in GP practices stood at 79%, representing an increase of 25% since the previous survey in 1991. It is
Sowerby Unit for Primary Care Informatics, Medical School, University of Newcastle, Newcastle- upon-Tyne NE2 4AA, UK
0953-5438/96/$09.50 0 1996 Elsevier Science Ltd B.V. All rights reserved 347

estimated that 90% of practices will be ‘computerised’ by the end of 1996 and 92% by 1997 (NHS Management Executive, 1993). Thus, the vast majority of practices are now equipped with computers and making increasing use of these facilities. Whilst no precise figures are readily available for other technologically advanced countries, there can be little doubt that the trends are similar. Typically, computers provide facilities for patient registration, recall, screening, repeat prescriptions and entries to case notes. Further uses now include decision support aids, prompts for opportunistic preventive measures, and providing treatment protocols to use for particular conditions (Brownbridge et al., 1985a; NHS Management Executive, 1993). Their use as a decision support tool, for instance in issuing prescribing guidelines nationally and consistently across GPs in response to “READ code” input (diagnoses), is the latest development of this technology. What this involves, in practice, is for the physician to enter the diagnoses and the computer to issue standardised suggested prescriptions in the presence of the patient. With the constantly increasing amount of information with which doctors need to practice in conjunction with increasing patient expectations, some form of support is needed. Computers are clearly the most effective way of presenting information which helps solve information dilemmas. The PRODIGY project (Prescribing Rationally with Decision-support In General practice study) involves collecting data from 137 practices in England for whom five suppliers of hardware/software are presently installing their respective versions of a computerised prescribing aid system. Further details of the wider scope of this project may be found in Purves (1995). Whilst computers are used in the consulting room for many purposes and ‘computerising’ in primary health care can mean many things, it is the experience of computers in this specific decision support context, that provides the scenario and impetus for this article. Whilst there are obvious and undeniable benefits of such a computer application, any possible detriment to the doctor-patient relationship needs to be borne in mind (Scott et al., 1996).
Whereas much has previously been written describing doctor-patient relation- ships, the physician’s use of the microcomputer, and human-computer inter- action generally, such relationships have largely been discussed within a two-way or dyadic perspective only. It is important to consider the doctor, computer, and patient elements within a three-way interactive model, here termed the ‘DCP model’, where each component has an undeniable effect on the relationships between the other two. This paper aims to review the salient empirical work over the past two decades and proposes the triadic framework as the most parsimonious way of viewing the situation.
For some time there have been fears expressed generally that the use of computers may ‘dehumanise’ medicine. There are certain differences between the use of computers within primary care settings such as the general practitioner’s consulting room and the hospital setting. Whereas sophisticated-looking equip- ment is a familiar sight within accident and emergency units, operating theatres, and the wards in general, patients may be surprised to see a computer in the consulting room. It is a characteristic of general practice that the relationship between doctor and patient can be of long duration, yet remains a delicate one, and it is likely that it is within general practice where the impact of the computer
348 interacting with Computers vol 8 no 4 (1996)

is most felt by the patient. This paper limits itself to the effects of the computer within general practice consulting rooms.
The doctor-patient dyadic relationship had traditionally been viewed as one of compliance (Thompson, 1984) with the direction of influence within the DCP model as from doctor to patient. However, more recently, the patient has been regarded as an active consumer rather than merely a passive recipient of treatment, thereby viewing the relationship as more of a two-way dyadic one. As Good et al. (1983) note, this is especially so in primary care where attendance at the GP’s consulting room is the patient’s own prerogative, and where, generally speaking, those attending are keen to continue to be involved in decisions about their treatment. There has therefore been increasing concern over measuring patients’ satisfactions with the services given (e.g. Treadway, 1983; Felletti et al., 1986).
Medical care presents a very interesting case. It is an environment which has made far less use of information technology than we might expect, and the reasons for this are predominantly human ones. Whilst the physician’s notes record much, they do so in a way that makes later reference very difficult. It seems reasonable to wonder why computer systems are not routinely used for capture and access to such information. It is hoped that the model presented here provides a framework for answering some of the complex issues posed. The environment of particular consideration (prescription decision-making support) should high- light the importance of the computer’s presence and activity alongside the two human protagonists.
Patient rating of doctors using computers
Brownbridge et al’s (1985b) study addresses two interrelated issues: firstly the impact of consulting room computer use on patients’ reactions to the consultation, and secondly whether particular groups of patients respond differentially to computer use. Whilst it was demonstrated that the patients were definitely aware of the doctor’s use of the computer, no significant effects were obtained as regards patients’ perceptions of the doctor’s attentiveness and rapport, the information provision by the doctor, or their expected ease of compliance, intention to comply, confidence in the treatment, satisfaction with the standard of treatment or self- reported post-consultation stress. In other words, the introduction of the computer had no effect on any of the measures used, other than that of perceived computer use. Of the patients who were directly asked whether they felt that the consultation had been affected as a result of the computer’s use, 81% replied “not at all”, only nine per cent answered “possibly a little”, and less than one per cent responded “yes, a fair bit” or “yes, a great deal”.
Brownbridge et al. acknowledge some reservations against too-ready accept- ance of the conclusion that computer use by doctors during consultations does not negatively influence patients’ experiences of the consultation. For instance, it is possible that patients have an overriding tendency to present their doctors in a favourable light, and responses to many of the measures employed did in fact demonstrate a positive skew. It is possible, therefore, that ceiling effects masked changes in patients’ perceptions and that the scales were therefore insensitive to changes in doctor behaviours. Countering this, the analysis did show significant
Scott and Purves 349

differences on a number of variables, suggesting that these measures are sensitive to consultation activity, and therefore able to show important computer effects should there be any
Brownbridge et al. conclude with the comment that: “Difficulties may arise with particular patients or with particular styles of use, and the long term effects must remain a subject for further inquiry. It seems likely, however, that it is the doctors that have to be convinced of the merits of such use. In this process, patient views must play a part, but they are assuredly not the only consideration” (1985a, p. 51).
A brief initial view of the four major studies of the eighties summarises the general view of patients. In Potter’s study (1981), nearly 30% of patients thought that the presence of a computer might adversely influence the consultation and some patients even stated that they would leave the practice. In 1984, Cruickshank reported that over half of the responders thought that the presence of computers in general practice would adversely affect the personal touch of the doctor, and Pringle et al. (1984) found that 17% of patients were opposed to computerisation largely on the grounds of possible loss of confidentiality. However, Rethans et al.‘s study (1988) suggested that patients are on the whole in favour of personal computers in the consulting room.
Attitudes change over time, and have rapidly been changing with regards to computers in all fields of life over recent years, and it is now unlikely that patients would leave a practice due to computerisation. Indeed, with almost 100% of practices likely to be computerised in the near future, there are few alternatives available. In 1990, Tooley published results from a simple questionnaire study of over 1000 patient respondents from general practice which looked at whether their attitudes had changed overall now that computers were more widely used and now that more patients have some experience of computers in medicine and also at home. The results showed that 93% considered that computer-generated letters and recall were advantageous, whilst 74% felt that standards of medical care would improve. Eighty-four per cent held no objections to the storage of medical records on computer although several did raise the issue of confiden- tiality. While the majority of patients did not mind the use of computers in general practice as, for instance, in checking records, and were not threatened by them given certain safeguards, a substantial proportion (one in four) would not feel comfortable with the computer as part of the consultation. As Tooley noted, patients usually tolerate whatever is done in practices providing that it is designed to be helpful and is not overtly threatening. However, a computer on the desk could appear threatening.
Whilst the overall impact on patients generally has been regarded as small, the discomfort caused to some warrants note. For instance, one early study by Cruickshank (1982) did show increased stress in patients with dyspeptic symptoms whose GPs employed a diagnostic computer system; prompting a call to preserve the ‘human touch. A recent Israeli video study by Urkin and colleagues (1993) indicated that GPs who used computerised medical records during consultations had modified their working styles to devote more attention to the computer and longer uninterrupted intervals for data entry than when using a traditional paper record. It is reported that these physicians changed from a ‘conversational pattern’ in which they frequently alternated between the patient
350 interacting with Computers vol 8 no 4 (1996)

and the record to a ‘block pattern’, in which a number of items of information were first established and then entered into the record. Unfortunately, patients’ reactions to the encounter were not included in this study
In an important item of research conducted in the USA on patients’ reactions to computers in the examination room, Aydin et al. (1995) focus on patients in the second phase of an interactive health appraisal system in preventative medicine. The first phase (Aydin et al., 1994) saw it hypothesized that the use of a particular interactive system would increase patient satisfaction with the thoroughness of the examination and their confidence in the examiner’s findings. Some clinicians, however, felt that using the computer might depersonalise patient care. Concerns about this, and also concerns centred on such feelings as the concerted effort needed to maintain eye contact with the patient rather than with the monitor and keyboard, led to the 1995 report comparing the reactions of patients whose clinician used the computer against those who did not. The measures used included overall satisfaction with their experience; cognitive, affective, behavioural, and advice scale; and specific items concerning the clinician’s focus on the chart or computer and whether the clinician seemed rushed during the examination.
No differences were found in affective or cognitive patient satisfaction between the two groups with regards any aspect of their experience. On the other hand, the fact that scores on the behaviour scale, measuring perceptions of the thoroughness of the examination and confidence in the examiner, also demon- strated no difference indicates that computer use also did not actually enhance patient satisfaction. Whilst patients in the ‘computer group’ agreed that they would choose an examiner who used a computer, their scores on this item were considerably lower than their highly positive ratings on the other scales. Aydin et al. commented: “Clearly, the computer was less important to patients than the other aspects of their relationship with the clinician, with which they were highly satisfied.” (p. 826)
A second US study by Solomon and Dechter (1995) also looked into whether the use of computers in the examination room would interfere with the patient- physician relationship. Their experiment surveyed patient satisfaction following examination by either of two physicians, one using pen-and-pencil note-taking, and the other taking notes with the computer. Sixty patients took part in this prospective, randomised cross-over study which simply involved the patients completing a questionnaire to assess their degree of satisfaction after the examination. It was found that there were no significant differences in satisfac- tion between the group whose physician made a hand-written record as compared with those whose physician used a computer, and nor was there an interaction between type of note-taking and physician. Furthermore, no correlation was found between previous patient exposure to and use of computers. It was therefore concluded that the study demonstrated no decrease in patient satisfaction when a computerised patient record was introduced.
Confidentiality
Rosen (1978) considered whether confidentiality is abused when patients’ records
Scott and Purves 351

are computerised. It was suggested that patients comply with computerisation of their records apparently because they believe they should obey, as in Milgram’s classic studies (e.g. 1974), and/or because the desired services are contingent on disclosure. She suggests that professionals should be sensitive to operating procedures which “subtly force people to give up their rights”.
With regard to this issue, a minority of patients in Rethan et al.‘s study (1988) agreed that it was now easier for others to obtain information from their personal files and most disagreed that their privacy was more secure than before the introduction of the computer. It is of concern that 66% of patients disagreed with the statement that their privacy was more secure when their files were computerised. However, 69% disagreed with the statement that: “With the computer it would be easier for others to get my medical information without my permission”. Rethans et al. suggest that the apparent ambiguity of feelings over this aspect is due to the word ‘privacy’ being too heavily loaded for most people; having being used largely in a negative context within various discussions on computers over the years. As a result of this paradox these practitioners report that they then started to inform their patients that there was no connection between their computer and any computer or telephone line outside the practice.
Confidentiality is essential to a patient’s willingness to talk freely and thereby enhance medical care, and the patient ought to be involved in deciding on what, and to whom, aspects of their personal information is passed on by an automated system. The confidentiality and secrecy ethical issues are discussed more fully by Vuori (1977) who cites five characteristics of computer system storage that promote the use of extensive records and may therefore pose a threat to confidentiality.
The concern over security and confidentiality of electronic medical records is often voiced, but this must be balanced against regular stories in the media concerning the appearance in public places e.g. refuse-disposal sites, of carelessly disposed paper records. Barrows and Clayton (1996) have recently reviewed the conflicting goals of accessibility and security for electronic medical records and discuss non-technical and technical aspects that constitute a reasonable security solution. Indeed, it is argued that with guided policy and current technology, an electronic medical record may offer better security than a traditional paper record.
“He cares more about the computer than me”
Disruption of attention An analysis of videotapes made by Fitter and Cruickshank (1982) suggests that the computer does have a substantial impact at a detailed level on communica- tion between doctor and patient. One cognitive area which is affected is direction of attention. The actual use of the computer in retrieving or inputting information requires the doctor’s attention and gaze to be directed towards the terminal, thereby seemingly distancing themselves from the patient and not giving them their direct attention. Although this pattern is similar to that used to refer to written notes, it is suggested that it appears to result in more attention spent on the computer than on the patient.
352 Interacting with Computers vol 8 no 4 (1996)

Fitter and Cruickshank (1983) report further on the distinct styles of interaction with the computer and patient employed by the doctors. One strategy was to attempt to minimise the use of the computer during the consultation. This could be achieved by entering the basic data (age, sex, etc.) before the patient enters, and entering symptoms elicited during the history-taking at convenient moments such as when the patient is undressing. This ‘minimal’ approach has the benefit of keeping the consultation simple for the doctor as it requires no switching of attention, and does not allow for the technology to intrude upon the patient. It does, on the negative side, require the doctor to store information, thereby increasing memory load, and thus when the symptoms are eventually entered they are likely to be influenced by the medical decision itself.
Some doctors chose the opposite approach, attempting to use the terminal ‘conversationally’. Thus, they would obtain a symptom from the patient, then turn to the terminal and input it, and then return to the patient for more information; a pattern of interaction requiring frequent alterations of attention. This strategy has the corresponding opposite pros and cons. Fitter and Cruickshank point out that it is less susceptible to memory load and interpretation, but needs the mental load of frequently alternating between two tasks, and the pressure to formalise the interaction with the patient can make substantial demands on the GP’s interaction skills. It is also noted that the response times of the system are critical when used conversationally, with response times to provide a menu and to process a symptom being approximately 8-10 seconds. It may be assumed, as it is not explicitly stated, that such response times are highly technological and context-dependent, rather than general; but if they are general then this is of concern as in the complex dynamics of the consultation, a 10 second pause in the doctor-patient side of the three-way interaction would appear oddly long to the patient. At least four strategies were observed for dealing with this delay:
l asking the patient to confirm the symptom to be entered; l staring intently at the screen to indicate that the doctor was busy; l staring into space between the patient and screen ‘as if in thought’; l returning to the patient (probably prematurely) and pursuing the next topic.
A third, compromise, strategy was also observed whereby the doctor would elicit information on a number of symptoms and then turn to the terminal and enter them in a block of activity with the computer. This, however, requires the patient to sit inactive while the doctor uses the terminal. Naturally, the compromise strategy carried a lesser degree of for and against associated factors. This was held by Fitter and Cruickshank to be the most successful of strategies in that it made good use of the information system whilst simultaneously allowing the doctor to conduct their general patient-centred consultation, interspersed with periods of computer-centred activity. Fitter and Cruickshank comment: ” Thus the doctors were able to incorporate this in a way that made it clear to patients that they were now about to devote their attention somewhere else; in the same way that one might apologize before turning to talk to someone else for a few moments.” (1983, p. 254)
It is worth having a fresh and closer look at the main relevant work from the last
Scott and Purues 353

decade, such as that of Cruickshank and Fitter. Cruickshank’s 1985 report was an attempt to probe patients’ expectations of the doctors and intentions of the consultation by comparing ratings of three doctors when they used and did not use the computer. A 38-item semantic differential-type scale was developed to look at the contrast between a patient’s rating of the doctor they had just seen and their notion of the ideal doctor. Items related to the human aspect of the doctor’s manner (sympathetic-unsympathetic), the doctor’s manner (listening- not-listening), the authority of his or her manner (convincing-unconvincing), the effectiveness of communication (explaining-not-explaining), and the direct impact of the computer (modem-old-fashioned). As a comparison, a group of patients who saw the doctors before the computer was introduced were also asked to employ the scale to rate the doctor they had just seen and their ideal doctor. It was found that, according to patients’ views, the prime quality is that doctors must listen and pay attention. Asking questions, thoroughness, helpfulness and explaining were given the next highest ratings. Usefulness and professionalism were also rated highly. “From this it would seem that patients put professional competence above the more human skills” (Cruickshank, 1985, p. 617).
The only two statistically significant differences from the 38 items were that the computer-using doctors were rated as less talkative and that computer-exposed patients assessed their doctor as paying less attention. There were also trends (substantial but not significant) in that computer-exposed patients described their doctors as paying less attention, as less helpful, less busy, and less confident. They rated the doctors more highly than had non-computer-exposed patients on 14 items. These included “asking questions”, which was consistent with findings by Brownbridge et al. (1984), and also “professional”, “clever”, and “important”, which suggests that the computer may have enhanced the doctors’ perceived competence and status. In addition, they managed to stay calm, were unhurried and not busy, unforgetful, good tempered, sympathetic, open, equal, courteous and modem.
Cruickshank concluded on a note of warning: “It may be possible to see patient ratings of doctors as an indication of the doctor-patient relationship, in which case a less than ideal rating may be indicative of a breakdown of (or failure to establish) doctor-patient rapport. . . Some doctors may take easily to the computer, whilst some may find that patients and the doctor-patient relationship suffer without special effort. The results are reasonably encouraging for those doctors that can incorporate the computer successfully into their routines - even using the computer ‘conversationally” while interviewing patients. It may be, however, that such doctors are already highly competent - the doctor who used this approach had received the best ratings of the three doctors without the computer” (1985, p. 621-622).
Doctor-computer relationship
Reduction of cognitive demands Within the DCP model, the doctor can be percevied as an information filter, extracting information from the patient and then, on the basis of medical and
354 Interacting with Computers vol 8 no 4 (1996)

social knowledge, interpreting the information and categorising it into a form suitable for use by an information system such as that of the computer (Fitter and Cruickshank, 1982). The potential for increased structuring of the information gathering is also likely to have an impact on the doctor’s decision processes. Increased structure, routine and formalisation of the interview may, indeed, lead to better medical decisions. Fitter and Cruickshank suggest that it is the basic requirement to provide information for a computer system, rather than the feedback it provides, which results in better decisions. These investigators pose the question - one of important psychological interest to all decision-based information processing systems - as to what extent can the formal model implied by the requirements of the information system integrate with the doctor’s usual and typically informal model of the decision process. It might be noted here, anticipating any argument that the format of physicians’ notes are also formal in the sense that what is entered has a particular syntax. Whilst it is true that some doctors may write in a structured style obeying grammatical rules, this is not typical of a doctor’s notes; one of the anecdotal comments cited by GPs is that one of the benefits of computer-written notes (apart from sheer legibility) is that they make sense, and are not mere notes and two-word comments.
Fitter and Cruickshank outline several reasons whereby this formal or predefined information system may constrain the doctor-patient interaction.
Coverage If doctors are informed that the more data they enter (for what is by necessity a predefined number of topics) the greater is the likelihood of an accurate diagnosis, then the coverage of symptom topics may be influenced by a tendency to pursue ‘computer topics’ at the expense of ‘non-computer topics’.
Discrete topics The normal medical consultation is characterised by an informal integration of topics. The visual feedback from topics entered as discrete entities may encourage users to structure the consultation so that topics are discussed more independently
Sequencing Even though topics might be listed in an order intended to emulate a normal or intuitive sequence, the ordered list may encourage the doctor to rigidly conform to a corresponding sequence for gathering symptom data. One of the commonest criticisms from GPs using one of the particular systems involved in this study was that the programme required a diagnosis to be entered at the outset, whereas Gl’s would more likely enter personal details, symptoms and course of illness, before entering the diagnosis. The important point therefore is that whilst computers may be regarded as sequential by necessity, human factors (i.e. how things actually occur between doctor and patient) must be accommodated within the software.
Categorisation When entering symptoms it is necessary for the doctor to categorise the information for each topic into one of a small range of alternatives (often
Scott and Purves 355

binary; present or absent) which may lead the doctor to couch questions to patients in a way that will produce unambiguous answers “to meet the computer’s requirements”. The doctor will either have to use their own terminology, in which case the computer symptoms are potentially inaccurate, or he/she must attempt to gather information and use it in two distinct ways; i.e., one terminology for data entry and another for decision making. Again, the issue is against inadequate consideration of the particular sort of human-human interaction.
Patient-computer relationships
Patients’ attitudes towards computers in medicine Cruickshank (1984) constructed a 26-item scale, whose analysis suggested five main factors: positive attitudes, negative attitudes, concern about doctors’ mistakes, concern that the doctor-patient relationship may be affected, and the financial implication of computers. It was found that their general practice patient group with experience of a computer being used scored on par with controls whilst other patients scored substantially lower. This was consistent with Fitter and Cruickshank’s (1982) report concerning hospital outpatients. Other differ- ences found were that males had more favourable attitudes towards computers than did females, and that the attitudes of patients aged over 50 were less favourable. A multiple regression analysis showed that the degree of experience of computers was the best predictor of attitudes towards their use, but age and sex were also significant.
Overall, the consulting room patients agreed most strongly with suggestions that the new technology was inevitable (89%), that computers would be a useful check against mistakes (80%), that they would be ‘a good thing’ if, as a result, patients did not have to wait so long to see a doctor (78%), and that they would save time for doctors (70%). They disagreed most strongly with suggestions that money spent on computers was wasted money (67%), that they would not believe a doctor who had used a computer (64%), that computers would not catch on (59%), and that doctors would forget how to treat them (58%).
However, despite these rejections, there remained quite large proportions that agreed with some of these items. Twenty-eight per cent, for instance, felt that doctors would forget how to treat people if they used a computer. Considering that patients tend to give positive responses to satisfaction surveys (Hulka et al., 1970; Wooley et al., 1978), these proportions may be more important than first impressions suggest. Also of concern is the 52% of patients who agree that the personal touch of the doctor would be lost. As Cruickshank remarks, with this sort of expectation, it is hardly surprising that patients may be less than enthusiastic at the prospect of their general practitioner acquiring a computer.
Whereas in some studies up to half of the patients believed that the introduction of computers would lead to a loss of the personal touch, the detailed study by Cruickshank (1984) reported that the vast majority of patients experience no difference between the doctor using the computer and writing notes. An important point is that patients generally qualified this statement by adding that computers were not impersonal providing that doctors continued to use
356 Interacting with Computers vol 8 no 4 (1996)

verbal skills and maintained eye contact with them as much as possible during the consultation.
In a more recent study, Ridsdale and Hudd (1994) aimed to answer three questions:
l What do patients perceive to be the advantages and disadvantages to doctors of the use of computers in the consultation?
l Which aspects of computer use particularly concern patients? l What do patients want to see about themselves on a computer screen?
To answer these questions, open-ended interviews with a sample of patients were undertaken in one general practice. The results suggested that computers were viewed by most patients as an efficient tool providing rapid access to medical histories and for saving doctors’ time. Studies from the 1980s (e.g. Pringle et al., 1984; Rethans et al., 1988) described earlier found that one-third of patients were concerned about the reduced confidentiality with computer-held records, and this caution did not seem to have been dispelled a decade later with two-thirds of Ridsdale and Hudd’s subjects expressing such concerns. Whilst subjects with experience of computers were more aware of the limitations of computers in terms of possibility of error, breakdown or loss of confidentiality, they still favoured use of computers in the consultation room.
It may be that any distrust of the computer is reduced by actually having it physically near the patient, as distinct from being set a distance away, with the attendant connotations of remoteness, inaccessibility and non-accessible one-way intrusion. One study gives weight to this physical and psychological barrier theory in that patients did tend to prefer the near rather than far position of the computer (Bright, 1991).
Educational use
Studies (e.g. Kincey et al., 1975) have shown that patients want more information about health, and the computer offers enormous potential for interactive patient education (e.g. Ackerman, 1989). Provision of information and patient education would be most effective if tailored to the individual patient by linkage to the medical record. In the UK, it is a legal necessity to provide patients with a copy of information held about them in a manner that they can understand (Data Protection Act, 1984) and it is therefore necessary to have a way of automatically converting medical terminology to terms which are acceptable and readily understood by the patient. This requirement might be borne in mind in other countries where the need is not legally stipulated. Patient-held records, including computer-generated patient-held records, are becoming more popular (McGhee et al., 1991), and with the increasing use of computers in general practice, the direct use of the computer by the patient needs to be investigated. To this end, Jones et al. (1992) examined on-line access by patients in general practice to their medical records and associated explanatory information. There is even the potential scenario of doctor and patient together entering particular data, such as symptoms, and jointly observing, as an educational exercise, the computers response output.
Scott and Purues 357

It might at this point be noted that, as yet, pen-based tablets, allowing hand- written machine-recognised entry, have made no impact within the GP/physician user group.
There is a commonly raised argument that patients might be confused and frightened by seeing their records, and that this might be detrimental to doctor- patient communication (Burrows, 1986; Ross, 1986). In the Jones et al. (1992) study, the GP felt that six out of the 113 were unsuitable to be given access and of the 70 who participated four did not look at any information. Of those who chose to look, there were none who, as judged by the researcher, were confused or frightened by the information.
The most popular feature of using the computer to obtain information was the search on medical history. More than one in four of the problems were not understood until the further explanation screen had been seen, and one in four also queried items or thought that something (e.g. their address) was incorrect. It was felt that most patients clearly enjoyed the opportunity of using the computer to see their own medical record and to discuss matters with the researcher. Several patients commented that because the GP did not have enough time, the computer would prove a useful tool. Eighty-seven per cent thought that the computer system was easy to use, and 84% said that they would use it again; despite the fact that 61% felt that they were given sufficient information by their Gl? The researchers comment that whilst from a health promotion perspective it would be logical to concentrate on the major public health problems associated with smoking, drinking, diet, exercise, etc., campaigns would not necessarily provide patients with the types of information they want. In a consumer-oriented health care service, the provision of such information should have a higher priority.
Skinner et al. (1993) suggest that computer technology is shifting away from the typical patient education computer programmes of the past, which were didactic and which often failed to suit information to an individual’s specific needs. The capacity to elicit and report back information concerning factors influencing patients’ health behaviours gives these programmes the ability to tailor an educational message at an individual level. Such programmes are intended to enhance, rather than replace, the personal interaction between GPs (and others in health care) and patients.
Interpersonal communication and human-computer interaction
In a paper by Greatbatch et al. (1993) the relationship between human-computer interaction (HCI) and interpersonal communication is examined within general practice consultations. Video recordings were analysed of 200 consultations conducted by four doctors both before and after the system’s implementation. Drawing on detailed analyses of these consultations, they describe how patients recurrently co-ordinate their actions with visible and audible aspects of the doctors’ use of a computer. The initiation and extension of a patient’s unsolicited turns at talk seemed to follow keystrokes that either accomplished or completed one of the tasks involved in the generation of a prescription. The data suggested that the patients were informed when to speak by these visible and audible
358 interacting with Computers vol 8 no 4 (2996)

COMPUTER
Effects of prior experience
delivery 01 care wllh computers
Reduction of manual workload
Pat~enis attitude towards computers
cognwe demands RELATIONSHIP ?
mhlbltlon ard perceived threat
Patlent’s perceotlons of docto:
/ / Patient’s expectatibns and mtentlons \ \/
DOCTOR How doctors present themselves (e.g. carlog (and?) up-to-date) Adequate attention to patient
PATIENT
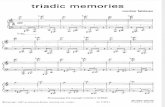
Figure 2. Examples wifhin the triadic model between doctor, computer and patienf
features. Aspects of the doctors’ behaviour (e.g. having eye contact with the patient, paper records or monitor) were also identified.
Conclusions
Previous research looking at the effects of computers in the consulting room suggest that this technology has a minimal invasive effect on the doctor-patient relationship. Brownbridge et al. (1985) summarised their research on the effect of computer use in general practice consultations by simply reiterating Cruickshank’s earlier (1984) conclusion: “. . Use of the computer during consultation need not result in less satisfied patients” (p. 46). The general conclusion from this review might once again echo this statement. Nevertheless, it seems undeniable that the ever-increasing sophistication of software being employed is likely to necessitate demands on the GP’s attention and visual focus to the extent that thresholds of acceptability for the patient are exceeded and the patient may feel of secondary importance. Such increasing demands on the doctor may negatively affect the patient’s faith in the doctor, the perceived infallibility of medical advice, and hence compliance with prescription-taking. Consequently, a study is currently underway to examine, by before-and-after questionnaires and by video analysis, what areas of the traditional doctor-patient relationship might be impaired by a more demanding software system in terms of entering data and checking its output (e.g. reading the screen).
Scott and Purues 359

The importance of considering the doctor, computer, patient elements within a three-way interactive DCP model, where each component has an undeniable effect on the relationships between the other two, was stressed at the outset of this review. In the light of the aforementioned findings, we can now model this tripartite approach within a triangular paradigm with each of the three sides being affected negatively and/ or positively by a third component at their opposite apex (see Figure 1). The use of the perceptually ‘impossible’ triangle is not fortuitous. Such illusions alternate their perspective as the viewer ponders over which is foreground and which is background, which two sides are prominent and which are not in primary focus. It is not possible to be sure. Should we regard the GP as a decision-making information filter between the patient and the computer, within a PDC model as opposed to a DCP model, deciding what - from all the information offered by the patient - warrants being entered into the computer and, conversely, making the decision as to what advice (e.g. prescribing- suggestions from the software) are put into practice in the form of the actual drug prescribed? Should we, from a progressive medical perspective, take a patient- centred approach (e.g. Stewart et al., 1995), seeing the patient as central and perhaps being more prepared to talk in terms of a DPC model? Should we, from a human-factors/ergonomics or even a social psychological perspective, see the computer as possibly intruding upon the doctor-patient rapport? Alternatively, from a more positive perspective, should it be regarded as an educational tool alongside doctor and patient, being interactively used to guide the patient through differential diagnoses, prompting at appropriate points for general health questioning, and readily displaying on-screen information whilst simultaneously printing out the tangible hard copy for the patient to retain? Perhaps we should put ourselves in the patient’s seat and see ourselves as the raison d’etre for the consultation; again, a DPC model. We might well feel that the computer is a wonderful aid; invaluable but not indispensable.
No one view is correct. In the GP consultation scenario, it is inadequate to talk in terms of HCI as simply a dyadic interaction; either between doctor and computer, or as a problem of attitudes of the patient towards the machine. Nor is it sufficient any longer to analyse the consultation, whether by describing it in terms of conversation analysis or by way of traditional doctor-training appraisal schedules, without considering the third ubiquitous component. We must see all components collectively, all sides simultaneously; a ‘cubist’ perspective of a triangle not impossible, but now made feasible.
Finally, it is intended to develop the details of this model with particular regard for the patient educational benefits which might arise from attempting to integrate the patient more fully with the computer. Certain consequences of the three-way interaction have been raised; for instance the need for the physician to attend (in different ways) to the two other members, at times in series and at times in parallel, and also it may be advantageous for the GP to try to contain computer- based interaction in blocks separate from attention devoted to the patient. Within England and the Netherlands, at least, the wheels are now well in motion for standardised decision-making support systems for medical prescribing within the consultation room, and so regarding the computer as an ‘optional extra’ is increasingly unrealistic. It is hoped that the general implications alluded to
360 interacting with Computers vol 8 no 4 (1996)

throughout this article (e.g. alternating attentional demands) will be taken up by other HCI practitioners.
References
Ackerman, M.J. (1989) ‘New media in medical education’ in Salaman, R., Protti, D. and Moehr, J. (eds), Conf. Proc. lnt. Symp. Medical lnformatics and Education 75-79
Aydin, C.E., Rosen, P.N. and Felitti, V.J. (1994) ‘Transforming information use in preventative medicine: learning to balance technology with the art of caring’ J. American Medical lnformatics Association Symp. Supplement: Proc. 18th Ann. Symp. Computer Applications in Medical Care IEEE Computer Society Press, 563-567
Aydin, C.E., Rosen, P.N., Jewell, SM. and Felitti, V.J. (1995) ‘Computers in the examining room: the patient‘s perspective’ J. American Medical lnformatics Association Symp. Supplement: Proc. 19th Ann. Symp. Computer Applications in Medical Care. IEEE Computer Society Press, 824-828
Barrows, R.C. and Clayton, P.D. (1996) ‘Privacy, confidentiality and electronic medical records’ J. American Medical lnformatics Association 3, 139-148
Bright, S. (1991) ‘Nearest and dearest’ British J. Healthcare Computing 8, 58-59
Brownbridge, G., Fitter, M. and Sime, M. (1984) ‘The doctor’s use of a computer in the consulting room: an analysis’ Int. J. Man-Machine Studies 21, 65-90
Brownbridge, G., Evans, A. and Wall, T. (1985a) ‘Effect of computer use in the consultation on the delivery of care’ Brit. Medical 1. 291, 639-642
Brownbridge, G., Herzmark, G. and Wall, T. (1985b) ‘Patient reactions to doctors’ computer use in general practice consultations’ Social Science in Medicine 20, 47-52
Burrows, M. (1986) ‘A legal right - or a dangerous bludgeon? BMA News Review 12,23
Cesnik, B. (1996) ‘History of health informatics’ in Hovenga, E. et al. (eds) Health lnformatics: An Overview Churchill Livingstone, 7-12
Cruickshank, P.J. (1982) ‘Patient stress and the computer in the consulting room’ Social Science in Medicine 16, 1371-1376
Cruickshank, P.J. (1984) ‘Computers in medicine: patients’ attitudes’ 1. Royal College of General Practitioners 34, 77-80
Cruickshank, P.J. (1985) ‘Patient rating of doctors using computers’ Social Science in Medicine 21, 615-622
Felletti, G., Firman, D. and Sanson-Fisher, R. (1986) ‘Patient satisfaction with primary care consultations’ 1. Behavioral Medicine 9, 389-399
Fitter, M.J., Garber, J.R., Herzmark, G.A. and Robinson, D. (1986) A Prescription for Change: A Report on the Longer Term Use of Computers in General Practice HMSO
Fitter, M.J. and Cruickshank, P.J. (1982) ‘The computer in the consulting room: a psychological framework’ Behav. info. Technol. 1, 81-92
Fitter, M.J. and Cruickshank, P.J. (1983) ‘Doctors using computers: a case study’ in Sime, M.E. and Coombs, M.J. (eds) Designingfor Human-Computer Communication Academic Press, 239-260
Freeman, B., Negrete, V.F., Davis, M. and Korsch, B.M. (1971) ‘Gaps in doctor patient communications: doctor-patient interaction analysis’ Paediatric Research 5, 228-311
Good, M.D., Good, B.J. and Nassi, A.J. (1983) ‘Patient requests in primary health care settings: development and validation of a research instrument’ 1. Behavioral Medicine 6, 151-168
Scott and Purves 361

Greatbatch, D., Luff, P., Heath, C. and Campion, P. (1993) ‘Interpersonal communication and human-computer interaction: an examination of computers in medical consulta- tions’ lnteracfing with Computers 5, 193-216
HMSO (1984) Data Protection Act HMSO
HMSO (1985) General Practice Computing HMSO
Hovenga, E.J.S. and Kidd, M.R. (1996) ‘Health informatics in Australia’ in Hovenga, E. et al. (eds) Health Informatics: An Overview Churchill Livingstone, 3-6
Hulka, B.S., Zyzanski, S.J., Cassel, J.C. et al. (1970) ‘Scale for the measurement of attitudes towards physicians and primary medical care’ Medical Care f&429-436
Jones, R.B., McGhee, S.M. and McGhee, S.M. (1992) ‘Patient on-line access to medical records in general practice’ Health Bull. 50, 143-150
Kincey, J., Bradshaw, P. and Ley, P. (1975) ‘Patients’ satisfaction and reported acceptance of advice in general practice’ J. Royal College of General Practitioners 25, 558-566
Ley, P., Whitworth, M., Skilbeck, C. Woodward, R., Pinsent, R., Pike, L., Clarkson, M. and Clark, P. (1976) ‘Improving doctor-patient communications in general practice’ 1. Royal College of General Practitioners 26, 720-724
McGhee, S.M., Hedley, A.J., Jones, R.B. and Cheng, K.K. (1991) ‘Patient-held records: their current status and implications for health care in Hong Kong’ Hong Kong Practilioner 13, 1374-1381
Milgram, S. (1974) Obedience to Authority Harper & Row
Millman, A., Lee, N. and Brooke, A. (1995) ‘The ABC of medical computing: computers in general practice’ Brit. Medical J. 311, 864-867
Moidu, K., Wigertz, 0. and Trell, E. (1995) ‘Multicenter systems-analysis study of primary health care: a study of socio-organizational and human-factors’ Int. 1. Bio-Medical Compufing 1,27-42
NHS Management Executive (1993) Computerisation in GP Practices: 1993 Survey Department of Health, Leeds, UK
Potter, A.R. (1981) ‘Computers in general practice: the patient’s voice’ J Royal College of General Practitioners 31, 683-685
Pringle, M., Robins, S. and Brown, G. (1984) ‘Assessing the consultation: method for measuring changes in patient stress and arousal’ Brit. Medical J. 288, 1657-1658
Purves, I.N. (1995) PRODIGY: Information for Participants Sowerby Unit for Primary Care Informatics, University of Newcastle-upon-Tyne, UK
Rethans, J-J., Hoppener, P., Wolfs, G. and Diederiks, J. (1988) ‘Do personal computers make doctors less personal?’ bit. Medical J. 296, 1446-1448
Ridsdale, L. and Hudd, S. (1994) ‘Computers in the consultation: the patient’s view’ Brit. J General Practice 44, 367-369
Rosen, C.E. (1987) ‘The compliant client’ Man and Medicine 3, 1-7
Ross, A.P. (1986) ‘The case against showing patients their records’ Brit. Medical 1. 292, 578
Scott, D., Purves, I.N. and Beaumont, R. (1996) ‘Computers in the GP’s surgery’ in Robertson, S.A. (ed) Contemporary Ergonomics 1996 Taylor & Francis, 397-402
Skinner, C.C., Siegfreid, J.C. and Kegler, M.C. (1993) ‘The potential of computers in patient education’ Patient Education and Counselling 22, 27-34
Solomon, G.L. and Dechter, M. (1995) ‘Are patients pleased with computer use in the examination room?’ J. Family Practice 41, 241-244
Stewart, M., Brown, J.B., Weston, W.W., McWhinney, I.R., McWilliam, C.L. and Freeman, T.R. (1995) Patient-Centred Medicine Sage
362 Interacting with Compufers uol 8 no 4 (1996)

Thompson, J. (1984) ‘Compliance’ in Fitzpatrick, R. et al. (eds) The Experience of Illness Tavistock
Tooley, P.J. (1990) ‘Computers in general practice: patients’ views’ Brit. I. General Practice 40, 333, 167
Treadway, J. (1983) ‘Patient satisfaction and the content of general practice consultations’ J. Royal College of General Practitioners 33, 769-771
Urkin, J., Warshawsky, S.S., Pliskin, J.S., Cohen, N., Sharon, A., Binstok, M. and Margolis, C.Z. (1993) ‘How does a computerised medical record (CMR) affect physicians’ work style? A video recorded study’ Proc. American Medical lnformatics Association 1993 Spring Congress 89
Vuori, H. (1977) ‘Privacy, confidentiality and automated health information systems’ J. Medical Ethics 3 174-178
Wolf, M.H., Putnam, S.M., James, S.A. and Stiles, W.B. (1978) ‘The Medical Interview Satisfaction Scale: development of a scale to measure patient perceptions of physician behavior’ 1. Behavioral Medicine 1, 391-401
Wooley, F.R., Kane, R.L. Hughes, C.C. et aI. (1978) ‘The effects of doctor-patient communication on satisfaction and outcome of care’ Social Science in Medicine 12, 123-128
Received March 1996; accepted September 1996
Scott and Purves 363