Tremor
Click here to load reader
-
Upload
dr-ibg-fajar-manuaba-spog -
Category
Documents
-
view
18 -
download
1
Transcript of Tremor

into postural, isometric, or kinetic tremors.Postural tremor occurs when the affectedbody part maintains position against gravity(e.g., extending arms in front of body). Iso-metric tremor results from muscle contrac-tion against stationary objects (e.g., squeezingthe examiner’s fingers). Kinetic tremor, whichoccurs with voluntary movement, is eithersimple kinetic tremor or intention tremor.Simple kinetic tremor is associated withmovement of extremities (e.g., pronation-supination or flexion-extension wrist move-ments). Intention tremor occurs during visu-ally guided movement toward a target (e.g.,finger-to-nose or finger-to-finger testing),with significant amplitude fluctuation onapproaching the target2 (Table 1).1,6
Although this classification helps in deter-mining cause, the presentation of tremor syn-dromes varies. Other aspects of the historyand physical examination should be consid-ered when evaluating patients with tremor.
Tremor SyndromesPHYSIOLOGIC TREMOR
All normal persons exhibit physiologictremor, a benign, high-frequency, low-ampli-tude postural tremor. Usually invisible to thenaked eye, it can be amplified by holding apiece of paper on the outstretched hand orpointing a laser at a distant screen.1,2
Tremor—a rhythmic, involun-tary, oscillatory movement ofbody parts1—is the most com-mon movement disorder.2 Thediagnosis is based on a careful
assessment of the history and physical exami-nation, although some tests, includingpositron emission tomography (PET) andsingle photon emission computed tomogra-phy (SPECT), are being investigated as diag-nostic aids.2-5 This article reviews the classifi-cation and causes of tremor and providesevaluation guidelines.
ClassificationTremors are classified as rest or action
tremors. Rest tremor occurs when the affectedbody part is completely supported against grav-ity (e.g., hands resting in the lap). Amplitudeincreases during mental stress (e.g., countingbackwards) or with general movement (e.g.,walking) and diminishes with target-directedmovement (e.g., finger-to-nose test).1,2,6
Action tremors are produced by voluntarymuscle contraction. They are further divided
Tremor, a rhythmic, involuntary, oscillatory movement of body parts, is the most com-mon movement disorder. Tremors are classified as rest or action tremors. Rest tremoroccurs when the affected body part is completely supported against gravity. Actiontremors are produced by voluntary muscle contraction and are further divided intopostural, isometric, or kinetic tremors. This article describes clinical signs and symp-toms of six tremor syndromes, including physiologic tremor, essential tremor, Parkin-son’s disease, toxic and drug-induced tremor, cerebellar tremor, and psychogenictremor, and presents a detailed diagnostic approach to tremor. Although new tech-nologies such as positron emission tomography and single photon emission computedtomography are under investigation for possible use in diagnosing specific tremor syn-dromes, they have no widespread applicability or use at this time. The history andphysical examination remain the most important diagnostic tools available to clini-cians in identifying and classifying tremor syndromes. (Am Fam Physician 2003;68:1545-52,1553. Copyright© 2003 American Academy of Family Physicians.)
All normal persons exhibit physiologic tremor, a benign,high-frequency, low-amplitude postural tremor.
TremorSHARON SMAGA, M.D., Southern Illinois University School of Medicine, Carbondale, Illinois
PROBLEM-ORIENTED DIAGNOSIS
Members of variousfamily practice depart-ments develop articlesfor “Problem-OrientedDiagnosis.” This articleis one in a series coor-dinated by the Depart-ment of Family Medi-cine at the SouthernIllinois UniversitySchool of Medicine,Springfield, Illinois.Guest editor of theseries is John G.Bradley, M.D.
O A patient informa-tion handout aboutessential tremor, writ-ten by the author ofthis article, is providedon page 1553.
Downloaded from the American Family Physician Web site at www.aafp.org/afp. Copyright© 2003 American Academy ofFamily Physicians. For the private, noncommercial use of one individual user of the Web site. All other rights reserved.

Enhanced physiologic tremor is a visible,high-frequency postural tremor that occurs inthe absence of neurologic disease and iscaused by medical conditions such as thyro-toxicosis, hypoglycemia, the use of certaindrugs, or withdrawal from alcohol or benzo-diazepines. It is usually reversible once thecause is corrected1,2 (Table 2).6,7
ESSENTIAL TREMOR
Essential tremor is a visible postural tremorof hands and forearms that may include a
kinetic component.1 It is the most commonmovement disorder worldwide; prevalenceranges from 4.1 to 39.2 cases per 1,000 per-sons, to as high as 50.5 per 1,000 in personsolder than 60 years.8 These figures mayunderestimate the true prevalence, however,because up to 50 percent of persons with mildessential tremor are unaware of it.9 Reports offamily history vary widely, with 21.7 percentof patients in one study9 and 62 percent inanother study10 reporting a family history oftremor.
Essential tremor develops insidiously andprogresses slowly, presenting as a postural,distal arm tremor in 95 percent of patients.Onset peaks bimodally in the teens and 50s.The tremor may start in a single limb, but itbecomes bilateral over time, most often as aflexion-extension movement of the wrist with
1546 AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 68, NUMBER 8 / OCTOBER 15, 2003
Essential tremor is the most common movement disorder inthe world, ranging from 4.1 to 39.2 cases per 1,000 personsyounger than 60 years.
TABLE 1
Classification and Characteristics of Tremor
Type of tremor Frequency Amplitude Occurrence Examples
Rest tremor Low to medium High; decreases with Limb supported against Parkinson’s disease; drug-induced (3 to 6 Hz) target-directed gravity; muscles are not parkinsonism (neuroleptics;
movement activated metoclopramide [Reglan])
Action tremor — — Any voluntary muscle contraction
Postural tremor Medium to high Low; increases with Limb maintains position Physiologic tremor; essential (4 to 12 Hz) voluntary movement against gravity tremor; metabolic disturbance;
drug or alcohol withdrawal
Kinetic tremor
Simple kinetic Variable (3 to Does not change with Simple movements of —10 Hz) target-directed the limb
movement
Intention Low (< 5 Hz) Increases with target- Target-directed movement Cerebellar lesion (stroke, multiple directed movement sclerosis, tumor); drug-induced
(lithium, alcohol)
Isometric tremor Medium Variable Muscle contraction against Holding a heavy object in stationary objects one hand
Task-specific Variable (4 to Variable Occurs with specific action Handwriting tremor; musician’s tremor 10 Hz) tremor
Information from references 1 and 6.

a frequency of 4 to 12 Hz. It may involve thehead, appearing as a yes-yes or no-no headmovement. Amplitude increases with stress,fatigue, and certain medications such as cen-tral nervous system stimulants, and mayincrease with certain voluntary activities suchas holding a fork or cup. Rest, beta blockers,primidone (Mysoline), and alcohol ingestiondecrease the tremor.2,10,11
PARKINSON’S DISEASE
Parkinson’s disease (PD) is 20 times lesscommon than essential tremor.8 Nevertheless,approximately 1 million Americans have PD.12
Because specific treatment options are avail-able, accurate diagnosis is essential.2,6,12,13
Symptoms develop insidiously, often afterage 50, although early-onset disease mayappear in the 20s.13 Initial symptoms includeresting tremor beginning distally in one armat a 4- to 6-Hz frequency. Typically, the tremoris a flexion-extension elbow movement, apronation-supination of the forearm, or apill-rolling finger movement. It worsens withstress and diminishes with voluntary move-ment. It may have postural or kinetic compo-nents.2,12 However, 10 to 20 percent of patientshave no tremor during the course of PD.2,14
Other signs of PD include rigidity, bradyki-nesia, and impaired postural reflexes. Thephysician may note cogwheel rigidity (i.e.,ratchet-like resistance) during passive range ofmotion while examining the extremities.Bradykinesia includes a slow, shuffling gait,decreased arm swing with walking, difficultyrising from a seated position, and reducedfacial animation (masked facies).12,13,15 Pos-
tural reflexes are examined by the pull test: thepatient stands with arms hanging loosely atthe sides; from behind, the examiner holds thepatient’s upper arms just under the shouldersand gently pulls backward; if the patientbegins to fall, postural instability is indicated12
(Table 3).16
CEREBELLAR TREMOR
Cerebellar tremor presents as a unilateral orbilateral, low-frequency (less then 5 Hz) inten-tion tremor caused by stroke, brainstem tumor,or multiple sclerosis.2,17 It may include posturaltremor.1 Classically, cerebellar lesions produce
Tremor
OCTOBER 15, 2003 / VOLUME 68, NUMBER 8 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN 1547
TABLE 2
Potential Effects of Drugs on Physiologic Tremor
May exacerbate physiologic tremorAmphetaminesBeta-adrenergic agonists
(albuterol [Proventil])CaffeineCarbamazepine (Tegretol)EpinephrineFluoxetine (Prozac)Haloperidol (Haldol)Hypoglycemic agents
Information from references 6 and 7.
Lithium Methylphenidate (Ritalin)PseudoephedrineTerbutaline sulfate (Brethine)TheophyllineThyroid hormonesTricyclic antidepressantsValproic acid (Depakene)
May reduce physiologic tremorAlcoholBenzodiazepinesBeta-adrenergic antagonists
(propranolol [Inderal])Primidone (Mysoline)
TABLE 3
Comparison of Essential Tremor and Parkinson’s Disease
Clinical features Parkinson’s disease Essential tremor
Age at onset > 50 years Bimodal: teens and 50s
Gender Men more than women Men and women equal
Family history > 25 percent > 90 percent
Asymmetry Affects ipsilateral limbs Often symmetricat first
Character At rest Postural, kinetic
Frequency 4 to 6 Hz 4 to 10 Hz
Distribution Hands, legs Hands, head, voice
Effect of alcohol Unaffected Reduced by alcoholon tremor
Associated findings Bradykinesia, rigidity, —postural instability
Adapted with permission from Jankovic J. Essential tremor: clinical characteris-tics. Neurology 2000;54(11 suppl 4):S24.

kinetic tremor on the ipsilateral side of thebody. Finger-to-nose, finger-to-finger, andheel-to-shin testing results in worsening tremoras the extremity approaches the target.2 Othersigns include abnormalities of gait, speech, andocular movements; inability to perform rapidalternating hand movements;6 and titubation, apostural tremor of the trunk and head.5
DRUG-INDUCED AND TOXIC TREMORS
Drug-induced tremor may follow ingestionof certain drugs (Table 4)1; toxic tremorsoccur following intoxication. Tremors also arepresent during withdrawal from certain drugsand alcohol.1
The most common drug-induced tremor isenhanced physiologic tremor following use ofsympathomimetics such as pseudoephedrine,bronchodilators, or theophylline, and antide-pressants such as tricyclics or fluoxetine(Prozac).1,7 This tremor also may accompanybenzodiazepine withdrawal.2,7 Approximately25 percent of patients taking long-term val-proic acid (Depakene) therapy exhibit posturaltremor three to 12 months after starting ther-apy. Lowering the dosage decreases the tremor.2
Lithium can induce a fine postural tremorof the hands (8 to 12 Hz). Directly correlated
with serum concentration, lithium toxicitymay cause permanent damage to the cerebel-lum that precipitates postural and intentiontremors. Amiodarone (Cordarone) may causea dose-dependent reversible neurologic syn-drome consisting of postural tremor, ataxia,and peripheral neuropathy; symptomsdevelop in the first week of treatment andimprove following dosage reduction or dis-continuation. One study2 failed to demon-strate that moderate caffeine intake causes orexacerbates tremor. Neuroleptic agents suchas haloperidol (Haldol) or dopamine–recep-tor-blocking drugs like metoclopramide(Reglan) may induce parkinsonian tremor.7
Acute alcohol intake temporarily reducesphysiologic and essential tremors,2,16 whilealcohol withdrawal may cause posturaltremor.18 Chronic alcoholism may producecerebellar tremor1,5 (Table 4).1
PSYCHOGENIC TREMOR
Psychogenic tremor presents as a variabletremor that may decrease or disappear when
1548 AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 68, NUMBER 8 / OCTOBER 15, 2003
Drug-induced tremor commonly occurs after use of sympatho-mimetics such as pseudoephedrine, bronchodilators, or theo-phylline, and antidepressants such as tricyclics or fluoxetine.
The Author
SHARON SMAGA, M.D., is associate professor in the Department of Family and Com-munity Medicine at Southern Illinois University School of Medicine in Carbondale, Ill.She received her medical degree from the University of Chicago and completed threeyears of residency training at Southern Illinois University School of Medicine, Carbon-dale Family Practice Center, in Carbondale. She has a certificate of added qualificationin geriatric medicine.
Address correspondence to Sharon Smaga, M.D., Southern Illinois University School ofMedicine, Department of Family and Community Medicine, SIU Family Practice Center,305 West Jackson, Suite 200, Carbondale, IL 62901 (e-mail: [email protected]).Reprints are not available from the author.
TABLE 4
Common Causes of Drug-Induced Tremor
Postural tremorAmiodarone (Cordarone), amphetamines, beta-
adrenergic agonists (albuterol [Proventil]), caffeine,calcitonin (Salmonine, Miacalcin), cocaine,cyclosporine (Sandimmune), dopamine (Intropin),lithium, procainamide (Pronestyl), steroids, theophylline, thyroid hormones, tricyclic antidepressants, valproic acid (Depakene)
Intention tremorAlcohol (chronic), lithium toxicity
Rest tremorMetoclopramide (Reglan), neuroleptics (haloperidol
[Haldol], trifluoperazine [Stelazine])
Adapted with permission from Deuschl G, Bain P,Brin M. Consensus statement of the Movement Dis-order Society on Tremor. Ad Hoc Scientific Commit-tee. Mov Disord 1998;13(suppl):13.

not under direct observation, or with psy-chotherapy or placebo. The patient is asked totap a beat with the limb contralateral to thetremulous limb: if the tremor decreases orshifts to the frequency of the tapping (i.e.,entrainment), psychogenic tremor is sus-pected.19 Co-activation of antagonistic mus-cles of the tremulous limb may be detectedclinically or electrophysiologically.19
UNCOMMON TREMOR SYNDROMES
AND TREMORS IN CHILDREN
Less common tremors include primarywriting and other task-specific tremors17;tremor secondary to peripheral neuropathies;and primary orthostatic tremor.1,2 Tremors
occasionally presenting during childhoodinclude essential, enhanced physiologic, andprimary writing tremors, and tremor follow-ing severe head injury.20
A rare but important cause of tremor in theyoung is Wilson’s disease, an inborn error ofcopper metabolism that can be fatal if leftuntreated. Symptoms begin between 11 and25 years of age, although they may present asearly as 4 years of age. Tremor may be of theintention type or, more commonly, a wing-beating movement when the arm is abductedat the shoulder. Other signs are findingsrelated to liver dysfunction and ring-shapedcopper pigmentation in the cornea, calledKayser-Fleischer rings21 (Table 5).3
Tremor
OCTOBER 15, 2003 / VOLUME 68, NUMBER 8 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN 1549
TABLE 5
Clinical and Diagnostic Features of Tremor Syndromes
Tremor syndrome Clinical features Diagnostic tests
Enhanced physiologic Postural tremor: absence of neurologic disease Chemistry profile (glucose, liver function tests); tremor thyroid function tests; review of medications
Essential tremor Postural tremor: affects arms and head; increases No specific test; rule out other problems with with stress, fatigue, and stimulants; increases with general chemistry profile, CBC, and thyroid voluntary activities; decreases with alcohol; function tests.responds to beta blocker, primidone (Mysoline)
Parkinson’s disease Resting tremor: increases with stress, decreases with No testing needed for typical presentation; voluntary movement of limb, responds to MRI for atypical presentations; consider PET or dopaminergic agents; bradykinesia, rigidity, SPECT scanning, if available.impaired postural reflexes
Cerebellar tremor Intention tremor (same side of body as the lesion); CT scan or MRI; cerebrospinal fluid examination abnormal heel-to-shin testing, rapid alternating for IgG gamma globulins (if multiple sclerosis is hand movements; gait abnormalities; dysarthria suspected); screen for alcohol abuse (if suspected); (speech problems); nystagmus check lithium level if lithium toxicity is suspected.
Psychogenic tremor Variable (resting, postural, or intention): increases Electrophysiologic testingunder direct observation, decreases with distraction, changes with voluntary movement of contralateral limb; somatization in past history
Wilson’s disease Wing-beating tremor: ascites, jaundice, signs of hepatic Liver function tests; serum ceruloplasmin; urine disease; intracorneal ring-shaped pigmentation; copper; slit-lamp examinationrigidity, muscle spasms; mental symptoms
CBC = complete blood count; MRI = magnetic resonance imaging; PET = positron emission tomography; SPECT = single photon emissioncomputed tomography; CT = computed tomography.
Information from reference 3.

Diagnostic ApproachA thorough history should explore onset,
exacerbating and relieving factors, medica-tions, family history, and associated symp-toms. It also should assess functional limita-tions including job-related disabilities, socialembarrassment, and difficulty with holding acup or with handwriting.
Observation is the initial step in the physicalexamination. The physician observes thepatient sitting with hands resting in the lap orstanding with arms at the sides. When seekingevidence of postural tremor, the physician asksthe patient to extend the arms and perform thefinger-to-nose or finger-to-finger movementto identify an intention tremor. It is useful toobserve the patient drinking from a glass, writ-ing, or drawing a rhythmic pattern such as aspiral. The tremor should be classified as tobody part (arms, head), activation condition(when the tremor is present), frequency (fastor slow), and amplitude (fine or coarse).
In the examination of a patient with restingtremor, the physician checks for rigidity andbradykinesia by flexing and extending thepatient’s arms, seeking signs of cogwheel rigid-ity. Tremor and rigidity may become morepronounced if patients perform voluntarymovements with the opposite limb (e.g., thepatient draws a circle in the air with the oppo-site hand). The patient is asked to stand and towalk, thus displaying evidence of difficulty ini-tiating movement, reduced arm swing, orshuffling gait. If PD is suspected, a trial of ther-apy with a dopaminergic agent such as levo-dopa-carbidopa (Sinemet) is appropriate.Referral to a neurologist is indicated whenpatients fail to respond to the medication ordemonstrate an atypical presentation.
In patients with intention tremor, the physi-cian asks about the onset of symptoms. If thetremor is caused by stroke, onset is usuallyacute, and the patient may appear ill and com-plain of headache, vertigo, and difficulty withbalance. The physician observes for nystag-mus, difficulty with speech or swallowing, and
uneven gait (falling to one side). Multiple scle-rosis is suspected if the tremor is associatedwith visual disturbances and diverse neuro-logic symptoms and signs. The physicianshould check for evidence of chronic alco-holism, including spider angiomata, gyneco-mastia, enlarged liver, or abnormal blood testresults (elevated mean corpuscular volume or�-glutamyl transferase level).
Postural tremor can be relatively constantor episodic, and of acute or insidious onset. Itshould be noted whether stress or fatigueincreases the amplitude of the tremor. Ifweight loss, irritability, racing heart, or neckswelling is described, the patient should beexamined for thyroid enlargement, exophthal-mos, brisk reflexes, and tachycardia. The thy-roid-stimulating hormone level is checked torule out hyperthyroidism.
Tremor occurring three to four hours aftereating may suggest hypoglycemia. Other signsof hypoglycemia include altered sensorium,sweating, and pallor. A blood glucose test or aglucose tolerance test performed while thepatient is having symptoms may be appropri-ate. Tremor in conjunction with feelings ofsuffocation, chest tightness, and racing heartmay indicate panic disorder.
Hand tremor, sleep disturbance, irritability,sweating, nausea, and difficulty with concen-tration may indicate benzodiazepine with-drawal.5,7 The physician should ask about thepatient’s use of prescription or over-the-counter medications that are known to causetremor. Essential tremor is indicated if theexamination is normal except for posturaltremor and a positive family history (Figure 1).
Special StudiesWhile it is reasonable to order routine
chemistry, hematology, and thyroid functiontests in the evaluation of a patient with tremor,other testing depends on the tremor’s sus-pected etiology.3 Liver function tests are help-ful in young patients with non–drug-inducedtremor. In patients with Wilson’s disease,24-hour urine copper and serum ceruloplas-
1550 AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 68, NUMBER 8 / OCTOBER 15, 2003

min determinations are helpful. Cerebrospinalfluid examination for oligoclonal IgG bands isappropriate in patients suspected of havingmultiple sclerosis.
In some PD patients, magnetic resonanceimaging (MRI) studies have shown a narrow-ing of the high signal region between the rednucleus and the substantia nigra. However,patients with characteristic presentations andpositive responses to anti-Parkinson medica-tion do not require such imaging.3 A computed
tomographic scan or an MRI is more impor-tant in cases of intention tremor, when strokes,tumors, and multiple sclerosis are suspected.
PET and SPECT scanning have demon-strated decreased uptake in the brains ofpatients with Parkinson’s disease, mainly inthe posterior striatum, and may assist in theevaluation of rest tremor.3,15 Studies of SPECTscanning as a tool for evaluating isolated pos-tural tremor are mixed, with one study4
demonstrating no difference in uptake, and a
Tremor
OCTOBER 15, 2003 / VOLUME 68, NUMBER 8 www.aafp.org/afp AMERICAN FAMILY PHYSICIAN 1551
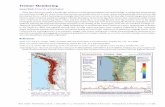
Evaluation of Tremor
FIGURE 1. Algorithm for evaluating tremor. (MRI = magnetic resonance imaging, CT = computed tomography)
Classic Parkinson’s disease
Possible early Parkinson’s disease
Possible drug-induced parkinsonism
Other signs of Parkinson’s disease (rigidity, bradykinesia,postural instability)?
Trial off drug
RestingPatient taking medications
that may cause tremor?
PosturalPatient taking medications
that may cause tremor?
KineticTask-specific (handwriting,
occupational)?
MonitorTrial of dopaminergicagent Enhanced
physiologic tremor
Essential tremor
Alcohol tremor
History of lithium toxicity?
Toxic tremor
MRI/CT of head to rule out stroke, tumor, multiple sclerosis
Trial of beta blocker, primidone (Mysoline)
History of chronic alcoholism?
Test for hyperthyroidism,hypoglycemia, panic attack, benzodiazepinewithdrawal
NoYes
NoYes
Possible alcohol withdrawal tremor
Other signs or symptoms of systemic disease?
Possible drug-inducedtremor
History of alcohol abuse?
Task-specific kinetic tremor
Intention tremor
Trial off medication
NoYes NoYes
NoYes
NoYes
NoYes
NoYes

Tremor
review of other studies5 indicating significantdifferences in uptake or activation. At thistime, functional imaging with PET or SPECTscanning is not widely available and is consid-ered to be of little clinical use in evaluatingtremor.3
Other evaluation tools include surface elec-tromyography, accelerometers, potentiome-ters, handwriting tremor analysis, and long-term tremor records.1,3 These tools generallyare used in research or specialty centers andare not used routinely in the office setting.
The author indicates that she does not have any con-flicts of interest. Sources of funding: none reported.
REFERENCES
1. Deuschl G, Bain P, Brin M. Consensus statement ofthe Movement Disorder Society on Tremor. Ad HocScientific Committee. Mov Disord 1998;13(suppl3):2-23.
2. Zesiewicz TA, Hauser RA. Phenomenology andtreatment of tremor disorders. Neurol Clin 2001;19:651-80,vii.
3. Anouti A, Koller WC. Diagnostic testing in move-ment disorders. Neurol Clin 1996;14:169-82.
4. Lee MS, Kim YD, Im JH, Kim HJ, Rinne JO, Bhatia KP.123I-IPT brain SPECT study in essential tremor andParkinson’s disease. Neurology 1999;52:1422-6.
5. Boecker H, Brooks DJ. Functional imaging oftremor. Mov Disord 1998;13(suppl 3):64-72.
6. Charles PD, Esper GJ, Davis TL, Maciunas RJ,Robertson D. Classification of tremor and updateon treatment. Am Fam Physician 1999;59:1565-72.
7. Cooper G, Rodnitzky R. The many forms of tremor.Precise classification guides selection of therapy.Postgrad Med 2000;108:57-8,61-4,70.
8. Louis ED, Ottman R, Hauser WA. How common isthe most common adult movement disorder? Esti-mates of the prevalence of essential tremorthroughout the world. Mov Disord 1998;13:5-10.
9. Elble RJ. Tremor in ostensibly normal elderly peo-ple. Mov Disord 1998;13:457-64.
10. Lou JS, Jankovic J. Essential tremor: clinical corre-lates in 350 patients. Neurology 1991;41(2 pt 1):234-8.
11. Evidente VG. Understanding essential tremor. Dif-ferential diagnosis and options for treatment. Post-grad Med 2000;108:138-40,143-6,149.
12. Uitti RJ. Tremor: how to determine if the patienthas Parkinson’s disease. Geriatrics 1998;53:30-6.
13. Young R. Update on Parkinson’s disease. Am FamPhysician 1999;59:2155-67,2169-70.
14. Gelb DJ, Oliver E, Gilman S. Diagnostic criteria forParkinson disease. Arch Neurol 1999;56:33-9.
15. Waters CH. Diagnosis and management of Parkin-son’s disease. 2d ed. Caddo, Okla.: ProfessionalCommunications, 1999:55-82.
16. Jankovic J. Essential tremor: clinical characteristics.Neurology 2000;54(11 suppl 4):S21-5.
17. Hallett M. Classification and treatment of tremor.JAMA 1991;266:1115-7.
18. Koller W, O’Hara R, Dorus W, Bauer J. Tremor inchronic alcoholism. Neurology 1985;35:1660-2.
19. Brown P, Thompson PD. Electrophysiological aidsto the diagnosis of psychogenic jerks, spasms, andtremor. Mov Disord 2001;16:595-9.
20. Haslem RA. Movement disorders. In: Behrman RE,Kliegman RM, Jenson HB, eds. Nelson Textbook ofpediatrics. 16th ed. Philadelphia: Saunders, 2000:1842.
21. Menkes JH. Disorders of metal metabolism. In:Rowland LP, ed. Merritt’s Textbook of neurology.9th ed. Baltimore: Williams & Wilkins, 1995:584-9.
1552 AMERICAN FAMILY PHYSICIAN www.aafp.org/afp VOLUME 68, NUMBER 8 / OCTOBER 15, 2003