Treatment of Conjunctival Intraepithelial Neoplasia with ......6a 2.0 × 4.0 0.02/14 None 8 24 7 60...
Transcript of Treatment of Conjunctival Intraepithelial Neoplasia with ......6a 2.0 × 4.0 0.02/14 None 8 24 7 60...

Treatment of Conjunctival Intraepithelial Neoplasiawith Topical Drops of Mitomycin C
Yaacov Rozenman, M.D., and Joseph Frucht-Pery, M.D.
Purpose. To evaluate the efficacy and risks of complications oftopical mitomycin C (MMC) for small-size conjunctival intra-epithelial neoplasia (CIN). Methods. Eight patients with clini-cally diagnosed CIN <8 mm were included in the study. Pa-tients received topical drops of MMC, 0.02–0.04%, 4 timesdaily for 14 days. Retreatment was done when lesions were noteliminated or recurred after the first treatment. Results. Threepatients remained disease free after one course of MMC appli-cation. Retreatment was done in four patients because of le-sions that decreased in size but were not eliminated, and forregrowth in one case. After retreatment, the lesions were eradi-cated in four patients, whereas in one patient, the treatmentfailed, and the lesion was surgically excised. The complicationsof MMC use included mild conjunctival hyperemia in two pa-tients and mild allergy in one patient, which resolved afterdiscontinuation of the treatment. Conclusion. Application oftopical MMC is an effective treatment for most but not all casesof small-size CIN.Key Words: Mitomycin C—Conjunctival intraepithelial neo-plasia—Conjunctival hyperemia.
Conjunctival intraepithelial neoplasia (CIN) is a be-nign, slowly progressing unilateral lesion with low ma-lignant potential (1,2).
The accepted treatment for CIN includes excision andcryotherapy (1,3). Excisional biopsy without prior con-firmation of the diagnosis is an appropriate approach forsuspected small-size malignant conjunctival lesions of�8 mm (4).
Recently several reports indicated that a chemothera-peutic approach with application of topical interferon,topical 5-fluorouracil, or topical mitomycin C (MMC)
can eliminate conjunctival and corneal intraepithelialneoplasia of various sizes (5–8).
Mitomycin C is a non–cell-cycle-specific alkylatingagent (9,10). It inhibits cell proliferation and serves toprevent recurrence of pterygium and posttrabeculectomybleb failures (11–16), and recently, eliminated of pri-mary acquired melanosis (17).
We report our experience with the use of MMC forsmall-size CIN.
METHODS
Eight patients, five men and three women, aged 37–69years, with clinically diagnosed small-size (<8 mm indiameter) CIN were treated with topical MMC (Table 1).In each case, clinical diagnosis of CIN was made by oneof the authors, based on a history of a growing lesion andclinical findings of conjunctival lesion consistent withCIN.
In seven patients, elevated and vascularized conjunc-tival/limbal lesions with leukoplakia were found, and inone patient (case 7, Table 1), a slightly elevated grayishirregular epithelium with underlying vascularity (but notleukoplakia) was discovered at the conjunctival and lim-bal area.
Drops of MMC, 0.02%, were freshly prepared by dis-solving a powder of the drug in a sterile saline solution.After signing an informed consent form, patients weretreated with MMC eye drops, 0.02%, 4 times daily for 14days, as described by Hayasaka et al. (14). A fresh so-lution of MMC was supplied after 1 week, and the oldbottle was retrieved from all the patients. Patients wereretreated when CIN was not eliminated after the firstcourse of MMC use, or when regrowth of the lesionoccurred. For the retreatment, we used MMC, 0.02 or0.04%, for 14 days. Excisional biopsy was done whenthe lesion was not eradicated by the drug. Topical ste-roids were applied 3 times daily when adverse reactionsof conjunctival hyperemia and accompanying symptomsmanifested.
Patients were followed up on a weekly or biweeklybasis until the lesion was eradicated or ceased to decrease
Submitted August 29, 1998. Revision received May 12, 1999. Ac-cepted May 17, 1999.
From the Departments of Ophthalmology, Shaarei-Zedek MedicalCenter (Y.R.), and Hadassah University Hospital (J.F.-P.), Jerusalem,Israel.
Address correspondence and reprint requests to Dr. Y. Rozenman,Department of Ophthalmology, Shaare-Zedek Medical Center, P.0.Box 3235, Jerusalem, Israel.
Each author states that he has no proprietary interest in the devel-opment or marketing of this or a competing drug.
Cornea 19(1): 1–6, 2000. © 2000 Lippincott Williams & Wilkins, Inc., Philadelphia
1

in size and was excised. Thereafter patients were exam-ined biweekly for 1 month, and then were followed upmonthly for 3 months, followed by examinations onceevery 6 months.
RESULTS
Patients were followed up between 24 and 44 months,except in case 8, in which the medical treatment failed,and the lesion was surgically excised. All eight patientscompleted the first MMC treatment course as planned(Table 1). Seven patients received drops of MMC,0.02%, 4 times daily for 14 days, and one (case 5) re-ceived drops of MMC, 0.04%, 4 times daily for 14 days.In all eight patients, after administration of MMC, thesize of the CIN started to decrease after 1–2 weeks, andin seven cases, the lesions were eliminated within thenext 4 months. However, in only three cases were thelesions eradicated after the first treatment with MMC. Inthese patients (cases 1, 3, and 4; Table 1), the lesionsdisappeared within the first 7 weeks and did not recur
during the 31–44 months of follow-up. In the other fivecases, retreatments with MMC were required.
In four of the five remaining patients, retreatmenteradicated the CIN (Tables 1 and 2). After the firstcourse of MMC, in two of the five patients (cases 5 and6, Table 1), the decrease in lesion size stopped; retreat-ment with the same dose of MMC was applied, and thelesions were eradicated within 6 and 8 weeks of theretreatment. In the third case (case 7), 1 month after thefirst treatment course, the decrease of the lesion stopped,and enlargement of the lesion was noticed. Retreatmentwith MMC, 0.02%, 4 times daily, was discontinued after4 days because of itching, conjunctival hyperemia, andmild conjunctival and lower-lid edema. Topical dexa-methasone phosphate, 0.1%, 3 times a day, cleared thesigns and symptoms within 10 days. Three weeks later, asponge soaked with MMC, 0.02%, was applied for 5 min(under the microscope) to the lesion site, once a day for6 consecutive days, with no allergic response. The lesiondisappeared after 8 weeks and did not recur during the 38months of follow-up. In one case (case 2, see case re-
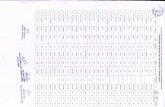
TABLE 1. Patients treated with drops of mitomycin C for CIN
No.AgeM/F Eye
Lesionsize (mm) Diagnosis
MMC (%)/duration(d) Complications
Eliminationtime (wk)
FU(mo)
1 44 M OS 4.0 × 3.0 CIN; leukoplakia 0.02/14 None 6 312 69 M OD 6.0 × 3.0 CIN; leukoplakia 0.02/14 Hyperemia; irritation 4 11 (regrowth)3 44 F OS 3.0 × 3.0 CIN; leukoplakia 0.02/14 None 7 344 48 F OD 2.7 × 1.5 CIN; leukoplakia 0.02/14 None 3 445 40 M OS 2.5 × 2.0 CIN; leukoplakia 0.04/14 None Decreased size 1.56 56 M OS 6.0 × 3.0 CIN; leukoplakia 0.02/14 Hyperemia Decreased size 27 60 F OS 5.0 × 3.0 CIN 0.02/14 None Decreased size 18 37 M OS 4.0 × 3.0 CIN; leukoplakia 0.02/14 None Decreased size 1.5
Cases 1 to 3 are described in the text as case reports.CIN, conjunctival intraepithelial neoplasia; F, female; M, male.
TABLE 2. Outcome after retreatment of conjunctival CIN with mitomycin C
No.Age (y)
M/F EyeLesion
size (mm) DiagnosisMMC (%)/
duration (wk) ComplicationsEliminationtime (wk)
FU(mo)
2 69 M OD 6.0 × 3.0 CIN 0.02/10 Hyperemia; irritation 4 112a Regrowth 5.0 × 3.0 0.02/10 None — —
0.02/7 None 8 325 40 M OS 2.5 × 2.0 CIN 0.04/14 None Decreased size 1.55a 2.0 × 1.0 0.04/7 None 6 466 56 M OS 3.0 × 6.0 CIN 0.02/14 Hyperemia Decreased size 26a 2.0 × 4.0 0.02/14 None 8 247 60 F OS 5.0 × 3.0 CIN 0.02/14 None Decreased size 17a Regrowth 4.0 × 2.5 0.02/4 Hyperemia, edema,
itching, MMC stoppedNo change 1
7b 4.0 × 2.5 MMC + spongea None 8 388 37 M OS 4.0 × 3.0 CIN 0.02/14 None Decreased size 1.58a 3.0 × 3.0 0.02/14 None Failure 2.58b 3.0 × 3.0 Excisional biopsyb
Case 2 is a case report in the text; 2a, 5a, 6a, 7a, 8a: first retreatment; 7b, 8b: other treatment approach after failure (8b)/complication(7b) of topical MMC drops use.
CIN, conjunctival intraepithelial neoplasia; F, female; M, male.a Sponge containing MMC, 0.02%, placed for 1 min. on the lesion. One daily application for 6 days.b CIN diagnoses based on histologic examination.
Y. ROZENMAN AND J. FRUCHT-PERY2
Cornea, Vol. 19, No. 1, 2000

port), the lesion disappeared after the first treatment, butregrowth occurred after 11 months, and the lesion waseradicated after retreatment. Finally, in case 8, twocourses of MMC failed to eradicate the lesion, and ex-cisional biopsy was done. Clinical diagnosis of CIN wasconfirmed by histologic findings.
No significant adverse reactions to MMC treatmentwere found. Two patients (cases 2 and 6) had mild con-junctival hyperemia with irritation, and one had a local-ized allergic response (case 7), which required discon-tinuation of the treatment. In these three cases, the symp-toms disappeared within 10 days after discontinuation ofthe medication and administration of dexamethasonephosphate, 0.1% drops, 3 times daily.
Case 1
A 44-year-old woman with xeroderma pigmentosumhad bilateral pterygia for many years. She complained ofa growing lump in the left eye in the past months withperiodic conjunctival hyperemia and discomfort. In July1994, her visual acuity was 20/30 in each eye. The lefteye had a pterygium with an overlying fleshy lesion, 4.0× 3.0 mm in size, with leukoplakia (Fig. 1A). In botheyes, the remainder of the ophthalmic examination wasnormal, except for a small and nonsymptomatic pte-rygium in the right eye.
After signing an informed consent, she receivedMMC, 0.02% drops, 4 times daily for 14 days. Twoweeks later, the lesion significantly decreased in size,and after an additional month, the tumor completely van-ished, leaving a pterygium and a quiet eye (Fig. 1B) Thepatient was last seen after 35 months (December 1996)with no complaint or recurrence of the lesion and nochange in the pterygium.
Case 2
A 69-year-old man was referred with a diagnosis of agrowing lesion (Bowen’s disease) on the right temporal
limbus. The patient complained of right-eye ocular dis-comfort, pain, and a growing lesion over the past months.In May 1993, his visual acuity was 20/30 in the right eyeand 20/20 in the left eye. On the temporal limbal area ofthe right eye, a 6.0 × 3.0 mm, mildly vascularized, ge-latinous leukoplakic lesion was discovered (Figs. 1 and2A). In both eyes, the remainder of the ophthalmic ex-amination was normal, except for bilateral nuclear cata-racts.
After signing an informed consent, the patient re-ceived MMC, 0.02% drops, 4 times daily for 14 days.One week later, the lesion started to decrease in size.After 14 days, at the completion of the treatment course,the eye became hyperemic and irritated. Drops of dexa-methasone, 0.1%, were applied 3 times daily. The lesiondisappeared during the next month. Regrowth of the le-sion, to a size of 5.0 × 3.0 mm, was identified after 12months. Because of the patient’s history of toxic re-sponse, retreatment was divided into a 7-day course ofMMC, 0.02%, followed by an additional 7-day course 2weeks after completing the first part. The lesion waseradicated without complications after 8 weeks. The pa-tient was last seen 32 months (April 1997) after the lasttreatment, with a quiet eye and no recurrence of thelesion (Figs. 1 and 2B).
Case 3
A 44-year-old man noticed, over the last months, agrowing lesion on a long-standing left eye nasal pin-gueculum. Eye examination in April 1994 revealed vi-sual acuity of 20/20 in each eye and bilateral nasal pin-gueculae. In the left eye, a white cauliflower-like el-evated lesion, 3.0 × 3.0 mm in size, was discovered onthe nasal pingueculum with a dellen formation on theadjacent cornea (Figs. 1 and 3A). In both eyes, the re-mainder of the ophthalmic examination was normal.
After signing an informed consent, he received MMC,
FIG. 1. A: Leukoplakia, 4.0 × 3.0 mm, overlying a pterygium in left eye of case 1 (Table 1).B: Noninflamed pterygium after elimination of leukoplakia (case 1, Table 1).
MITOMYCIN C FOR CIN 3
Cornea, Vol. 19, No. 1, 2000

0.02% drops, 4 times daily for 14 days. Within the next2 months, the lesion slowly decreased in size and finallyvanished, leaving a pingueculum and a quiet eye (Figs. 1and 3B). This patient was last seen after 32 months (Feb-ruary 1997) with a quiet eye, unchanged pinguecula, andno recurrence of the lesion.
DISCUSSION
The accepted treatment for CIN is excision; however,repeated surgeries are required in one third of the pa-tients because of incomplete excision and recurrence(18). Cryotherapy on completion of the excision of neo-plasia reduces the recurrence rate (3). These treatmentsmay cause a variety of complications, including scarringof conjunctiva and cornea, formation of retrocornealmembranes, and incomplete excision of the lesion. Fur-thermore, the possibility that during the surgical proce-dure, some tumor cells may be reimplanted and causerecurrence of a neoplastic process, cannot be excluded.
Topical MMC has been successfully used for the treat-
ment of conjunctival/corneal intraepithelial neoplasia(CCIN) in a small group of patients (5). In this group, nosevere complications were reported, which encouragedus to proceed with the same treatment in other patients.Our experience in a larger group of patients with CCINsupports these observations (unpublished data).
Our study included eight cases with clinically diag-nosed primary CIN. Seven of these cases also had leu-koplakia. All the lesions were of a small size, located atthe conjunctival or limbal areas without invading into theclear cornea. In seven of the eight cases, the lesion waseliminated after application of MMC, whereas in onecase, the treatment failed. Close observation of the casesshowed a gradual decrease in the size and thickness ofthe conjunctival lesions starting from ∼1 to 2 weeks afterinitiation of the treatment, and in the course of 3 weeksto 4 months, they completely disappeared.
In our group of patients, in only three of eight casesdid a single treatment course with MMC eradicate thelesions, and in an additional three cases, the lesions de-creased in size but were eradicated only after retreatment
FIG. 2. A: Gelatinous leukoplakia, 6.0 × 3.0 mm, temporal side of right eye (case 2, Table1). B: Intact conjunctiva after elimination of gelatinous leukoplakia (case 2, Table 1).
FIG. 3. A: Cauliflower-like leukoplakia, 3.0 × 3.0 mm, overlying a pinguecula in left eye(case 3, Table 1). B: Intact conjunctiva with noninflamed pinguecula after elimination ofcauliflower-like leukoplakia (case 3, Table 1).
Y. ROZENMAN AND J. FRUCHT-PERY4
Cornea, Vol. 19, No. 1, 2000

within the first 2 months of the first treatment. Further-more, in one case, a regrowth of CIN occurred within thefirst year after treatment with MMC, which indicates thatsome invisible neoplastic cells survived the first treat-ment course with MMC. This lesion was eradicated afterretreatment with MMC, 1 year after the first treatmentcourse. This study suggests that retreatment is logicalwhen the lesion is still visible 7 weeks after the treatmentbegan. The follow-up in our patients was >24 months,and although recurrence of CIN is possible after thatperiod, our previous experience suggests that the recur-rence of CCIN takes place within a year of the applica-tion of MMC (unpublished data).
Chemotherapy with topical MMC has some advan-tages over the surgical approach. It does not rely onhistological identification of the lesion, and it eradicatesthe histological, nonvisible nest of neoplastic cells. Che-motherapy spares the surrounding normal tissue, whichis usually excised around the lesion. Furthermore, pa-tients prefer treatment with application of the dropsrather than surgery. On the other hand, the chemothera-peutic treatment is longer, requires close follow-up andcompliant patients, and may cause adverse reactions. Inthis group of eight patients, two patients had drug-relatedmild conjunctival hyperemia, and one had a mild allergicresponse; all received small doses of topical steroids andwithin several days were free of symptoms. No long-term complications were reported. Various degrees oftoxicity to MMC use for CIN have been reported (5,8).However, use of MMC on epithelialized, intact ocularsurface caused mild complications that resolved after ap-plication of small doses of topical steroids, as was re-ported in this study. Severe MMC-related complicationswere reported when the drug was used on a nonepithe-lialized ocular surface after surgery (11,12,19).
The optimal required dose of topical MMC for eradi-cation of CIN lesions is still unknown. Courses of 14days of MMC, 0.02%, application showed efficacy ineradication of all except one small-size CIN lesions, withminimal adverse reactions and no damage to the intactocular surface epithelium. Longer duration of MMCtreatment may cause marked toxicity such as ocular pain,blepharospasm, hyperemia of the conjunctiva, sym-blepharon, corneal erosions, and uveitis (5,11,13,19). Onthe other hand, a shorter course may be insufficient: inone patient in our group, two courses of MMC applica-tion only decreased but did not eradicate the lesion. Al-though MMC is a very potent alkylating agent, sometumors may be resistant to this drug (20,21). In suchcases, other chemotherapeutic drugs can be used insteadof MMC (6,7). Both topical interferon and topical 5-flu-orouracil were reported as alternative treatments forMMC. Only one report indicated efficacy of topical in-terferon for CIN (6). A small number of CIN cases weresuccessfully treated with topical 5-fluorouracil (7).
Larger series of cases with long-term follow-up andcomparative studies are required to consider topical5-fluorouracil as an alternative to MMC.
Of concern is a report of lower punctal occlusion 4months after use of MMC, 1 mg/ml, for prevention ofrecurrence of pterygium (12). This event is very unusualand is probably related to the extreme concentration ofMMC used. No such event has been reported after usingMMC, 0.2 mg/ml. Although we did not encounter such acomplication during almost 10 years of MMC use, weagree with the suggestion to occlude the puncta tempo-rarily when MMC drops are prescribed for application athome (22).
The proper approach to presumed CIN lesions requireshistologic diagnosis by excisional biopsy for small le-sions and incisional biopsy for large lesions before fur-ther treatment is considered (4,22). Impression cytology,brush or scraping for histologic diagnosis of the conjunc-tival cells also may be useful. We believe that the generalophthalmologist, with limited clinical exposure to intra-epithelial lesions, should use one of the diagnostic mea-sures before prescribing MMC. However, an experi-enced expert in the field of cornea or ocular tumors whoclinically diagnoses a small-size growing CIN with typi-cal leukoplakia may use a topical chemotherapy based onclinical impression, particularly in patients who refuseany surgical approach and those who can comply withthe treatment and be easily monitored. Because theselesions are slow growing, one can closely follow up thesepatients and proceed with excisional biopsy when topicalchemotherapy fails. We used this approach in all thepatients in this study. We could follow up the shrinkageof the tumor mass and identified five lesions that de-creased in size but were not eliminated (Table 2). Asecond course of MMC was applied in these cases. Incase 8, two courses of MMC only decreased the size ofthe lesion. This lesion was excised, showed histologicCIN, and did not recur. Although the chemotherapyfailed to eradicate the whole mass in case 8, it decreasedthe lesion’s size, eliminated the irregular borders, andallowed excision of less tissue.
Of interest are cases 1 and 3, with CIN located onpterygium (Fig. 1A and B) or pinguecula (Fig. 3A andB). In both cases, MMC eradicated the CIN lesions over-lying the pterygium and pinguecula. During the follow-up period of almost 3 years, we did not observe anyclinical changes in the pingueculae and the pterygium,which looked noninflamed and quiet in the eyes of bothpatients.
This study suggests that the use of topical MMC forsmall-size CIN is safe and effective in most cases. Wesuggest the use of MMC, 0.02%, for 14 days for treat-ment of small CIN. Retreatment is required when thelesion recurs, and excisional biopsy should be done whenthe treatment fails. The optimal dosage of MMC for CIN
MITOMYCIN C FOR CIN 5
Cornea, Vol. 19, No. 1, 2000

and its long-term effect require further investigation.Long-term follow-up is required in these patients, as CINlesions may recur years after the treatment.
REFERENCES
1. Erie JC, Campbell RJ, Liesegang TJ. Conjunctival and cornealintraepithelial and invasive neoplasia. Ophthalmology 1986;93:176–83.
2. Waring GO III, Roth AM, Elkins MB. Clinical and pathologicaldescription of 17 cases of intraepithelial neoplasia. Am J Ophthal-mol 1984;97:547–59.
3. Fraunfelder FT, Wingfield D. Management of intraepithelial con-junctival tumors and squamous cell carcinomas. Am J Ophthalmol1983;95:359–63.
4. Smolin G, Thoft RA. The cornea. 3rd ed. Boston: Little, Brown,1995:579–95.
5. Frucht-Pery J, Rozenman Y. Mitomycin C for corneal intraepithe-lial neoplasia. Am J Ophthalmol 1994;117:164–8.
6. Yeatts PR, Ford JG, Stanton CA, Reed JW. Topical 5-fluorouracilin treating epithelial neoplasia of the conjunctiva and cornea. Oph-thalmology 1995;102:1338–44.
7. Maskin SL. Regression of limbal epithelial dysplasia with topicalinterferon. Arch Ophthalmol 1994;12:1145–6.
8. Frucht-Pery J, Sugar J, Baum J, et al. Mitomycin C treatment forconjunctival/corneal intraepithelial neoplasia: multicenter experi-ence. Ophthalmology 1997;104:2085–93.
9. Gilman AG, Rall TW, Nies AS, Taylor P, eds. Goodman andGilman’s the pharmacological basis of therapeutics. 8th ed. NewYork: Pergamon Press, 1990:1247–8.
10. Bowman WC, Rand MJ, eds. Textbook of pharmacology. 2nd ed.Oxford: Blackwell, 1980:14–5.
11. Singh G, Wilson MR, Foster CS. Mitomycin eye drops as treat-ment for pterygium. Ophthalmology 1988;95:813–21.
12. Singh G, Wilson MR, Foster CS. Long-term follow-up study ofmitomycin eye drops as adjunctive treatment for pterygia and itscomparison with conjunctival autograft transplantation. Cornea1990;9:331–4.
13. Hayasaka S, Noda S, Yamamoto Y, Sgtogawa T. Postoperativeinstillation of low-dose mitomycin C in the treatment of primarypterygium. Am J Ophthalmol 1988;106:715–8.
14. Hayasaka S, Noda S, Yamamoto Y, Sgtogawa T. Postoperativeinstillation of mitomycin C in the treatment of recurrent pterygium.Ophthalmic Surg 1989;20:580–3.
15. Chen CW, Huang HT, Bair JS, Lee CC. Trabeculectomy withsimultaneous topical application of mitomycin C in refractoryglaucoma. J Ocul Pharmacol 1990;6:175–9.
16. Palmer SS. Mitomycin as adjunct chemotherapy with trabeculec-tomy. Ophthalmology 1991;98:317–21.
17. Frucht-Pery J, Pe’er J. The use of mitomycin C in the treatment ofprimary acquired melanosis with atypia. Arch Ophthalmol 1996;114:1261–4.
18. Pizzarello LD, Jakobiec FA. Bowen’s disease of the conjunctiva: amisnomer In: Jakobiec FA, ed. Ocular and adnexal tumors. Bir-mingham: Aesculapius, 1978:553–71.
19. Rubinfeld RS, Plister RR, Stein RM, et al. Serious complicationsof topical mitomycin-C after pterygium surgery. Ophthalmology1992;99:1647–54.
20. Tsuruo T, Iida-Satio H, Kawabata H, et al. Characteristics of re-sistance to Adriamycin in human myelogenous leukemia K562resistant to Adriamycin and in isolated clones. Jpn Cancer Res1986;77:682–92.
21. Dulhanty AM, Li M, Whimore GF. Isolation of Chinese hamsterovary cells mutants deficient in excision repair and mitomycin Cbioactivation. Cancer Res 1989;49:117–22.
22. Grossniklaus HE, Aaberg TM. Mitomycin C treatment of conjunc-tival intraepithelial neoplasia. Am J Ophthalmol 1997;124:381–3.
Y. ROZENMAN AND J. FRUCHT-PERY6
Cornea, Vol. 19, No. 1, 2000











![[2] - YUDO · tina gpsb 08 open gate bush tina gpsb 08 flange tina gpsb Øh Ød 41 45 Ød1 32 m6x25l +0.02 0 +0.02-0.02 +0.02 0 0 -0.02 Øh 5 Ød1 Ød 20.5 Ø3 20 ca type Øg 0.8](https://static.fdocuments.net/doc/165x107/6023623d9fe9761d7326bcdd/2-yudo-tina-gpsb-08-open-gate-bush-tina-gpsb-08-flange-tina-gpsb-h-d-41.jpg)