Tongue and oropharynx
-
Upload
dr-neha-yadav -
Category
Health & Medicine
-
view
699 -
download
3
Transcript of Tongue and oropharynx

OROPHARYNX AND TONGUE
PRESENTED BY:DR. NEHA YADAVFIRST YEAR PG DEPARTMENT OF PERIODONTOLOGY AND ORAL IMPLANTOLOGY
GUIDED BY:DR. VIVEK CHATURVEDYDR. H. L. GUPTADR. PRADEEP CHAUDHARYDR. SHRADHA SETHI

OROPHARYNX AND TONGUE
GOOD MORNING

OROPHARYNX AND TONGUE Introduction Pharynx:
Boundaries Parts
Oropharynx: Relations Waldeyer’s lymphatic ring
Structure of pharynx: Layers of pharynx Muscles of pharynx
Blood supply: Arterial supply Venous supply

Lymphatic drainageNerve supply of pharynx
Physiology of deglutitionTongue:
PartsExternal featuresPapillae of the tongueMuscles of the tongueBlood supply of the tongueArterial supply Venous drainageLymphatic drainageNerve supply of the tongue

Development of the tonguePhysiology of taste sensationDevelopmental disturbances of the
tonguePeriodontal implicationsReferences

Oropharynx and Tongue INTRODUCTION
•Pharynx is a wide muscular tube situated behind the nose, mouth and the larynx.•It is a common passage for both food and air•It is about 12 cm in length •Width:
Upper part – Widest – 3.5 cm Middle part – narrow Lower part – narrowest
•Tongue is a muscular organ situated in the floor of the mouth with functions of taste, speech, mastication, deglutition.
•The tongue and oropharynx together form the gateway organs of the alimentary canal.

PHARYNX
Boundaries:
Superiorly – Base of the skull including the posterior part of the body of sphenoid bone and the basillar part of the occipital bone in front of the pharyngeal tubercle.
Inferiorly - It is continuous with oesophagus at the level of 6th cervical vertebra at the lower level of cricoid cartilage. Posteriorly – It glides freely on the prevertebral fascia which separates it from the cervical spine.
Anteriorly – It communicates with the nasal cavity, oral cavity and the larynx. Thus the anterior wall is incomplete.

On either sides:
A) It is attached to:
• Medial pterygoid plate• Pterygo mandibular raphe. • Mandible • Tongue • Hyoid bone • Thyroid and cricoid cartilages.
B) It communicates on each side with the middle ear cavity through the auditory tube.
C) It is related on either side to:
• The styloid process and the muscles attached to it.
• The CCA, ICA and ECA. • Cranial nerves related to them.


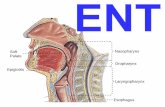
PARTS OF THE PHARYNX
It is divided into:
a) Nasopharynx
b) Oropharynx
c) Laryngopharynx

OROPHARYNX
It is the middle part of the pharynx situated behind the oral cavity where the pathways of air and food cross each other. Above : It communicates with the nasopharynx via the pharyngeal isthmus.
Below : It communicates with the laryngopharynx at the level of upper border of epiglottis.
Behind : It is supported by the body of axis vertebra and the upper part of the body of 3rd cervical vertebra. Lateral Wall: Presents the palatine tonsil which lies in the tonsillar fossa. This fossa is bounded anteriorly by palatoglossal and posteriorly by palatopharyngeal arches.
The wall of the oropharynx is formed posteriorly by inferior, middle and superior constrictor muscles of pharynx.


WALDEYER’S LYMPHATIC RING:
It is an aggregation of lymphoid tissue
in relation to the oropharyngealisthmus.The Waldeyer’s ring constitutes:
Pharyngeal tonsil: Posteriorly and above
Tubal tonsils: Laterally and abovePalatine tonsils: Laterally Lingual tonsil: Inferiorly over the
posterior part of the dorsum of the tongue.

Structure of the pharynx
The wall of the pharynx is composed of the following 5 layers:
1. Mucosa – lined by squamous epithelium.2. Sub mucosa.3. Pharyngobasilar fascia/pharyngeal aponeurosis: It is a fibrous sheet deep to the pharyngeal muscles. It
thick in the upper part where it fills the gap between the upper border of the superior constrictor and the base of the skull. Posteriorly, it forms the pharyngeal raphe .
Superiorly, it is attached to:• Basiocciput• Petrous temporal bone medial to carotid canal.• Posterior border of medial pterygoid plate.• Bridges under the auditory tube.• Pterygo mandibular raphe.




Inferiorly, it is gradually lost deep to muscles, and hardly extends beyond the superior constrictor muscle.
4. Muscle coat – consists of: Outer circular layer - made up of 3 constrictors. Inner longitudinallayer – made up of Stylopharyngeus, Salpingopharyngeus, Palatopharyngeus.
5. Buccopharyngeal fascia – Covers the outer surface of the constrictors and extends forwards across the pterygomandibular raphe to cover the buccinator.
The pharyngobasilar and the buccopharyngeal fascia are confined to the upper part of the pharynx, otherwise they would impede swallowing.
Beneath the buccopharyngeal fascia, on the muscular coat, there lies the pharyngeal plexus of veins and nerves.



BLOOD SUPPLY OF THE PHARYNX
Arterial supply:
•Ascending pharyngeal branch of ECA.•Ascending palatine and tonsillar branches of facial artery. •Dorsal lingual branches of lingual artery.•Greater palatine, pharyngeal and pterygoid branches of the maxillary artery.
Venous supply:
•Veins form a plexus on the posterolateral aspect of the pharynx. •It receives blood from, pharynx, soft palate and prevertebral region.• It communicates with the plexus above and drains into the IJV and facial vein.
Lymphatic drainage:
Drain into retropharyngeal and deep cervical lymph nodes.

NERVE SUPPLY
Supplied by pharyngeal plexus of nerves which lies on the middle constrictor. The plexus is formed by:•Pharyngeal branch of vagus.n.•Pharyngeal branch of glossopharyngeal.n.•Pharyngeal branches of superior cervical sympathetic ganglion.
Vagal fibers – motor.Glossopharyngeal fibers – sensory.Sympathetic fibers – vasomotor.
Motor fibers: are derived from cranial accessory nerve through the branches of vagus nerve. They supply all the muscles of pharynx except stylopharyngeus which is supplied by glossopharyngeal nerve.The inferior constrictor is additionally supplied by external laryngeal nerve and recurrent laryngeal nerve.The pharyngeal plexus also supplies all muscles of soft palate except tensor palati which is supplied by mandibular nerve.

•Sensory fibers are derived mostly from glosspharyngeal nerve and partly from vagus nerve. However soft palate and tonsil are supplied by lesser palatine nerve and glossopharyngeal nerves.
•Taste sensations from the vallecula and epiglottis area pass through internal laryngeal branch of vagus nerve.
•Parasympathetic secreto motor fibres to the pharynx are derived from greater petrosal nerve through the lesser palatine branches of pterygopalatine ganglion.

PHYSIOLOGY OF DEGLUTITION
It occurs in 3 stages:
A. First stage:
Voluntary
1.Anterior part of the tongue is raised and pressed against the hard palate by the intrinsic muscles of the tongue especially superior longitudinal and transverse muscles. This pushes the food bolus into the posterior part of the oral cavity.
2. The soft palate closes down onto the tongue to form a food bolus.
3. Hyoid bone is moved upwards and forwards by the suprahyoid muscles + elevation of posterior part of the tongue upwards and backwards by styloglossus muscle + palatoglossal arches are approximated by palatoglossal muscles. This pushes the bolus into the oropharynx.


B. Second stage:
Involuntary stage.
1. Food is pushed from the oropharynx to the lower part of laryngopharynx.
2. The nasopharyngeal isthmus is closed by the elevation of soft palate and approximation of posterior pharyngeal wall. This prevents food entering the nose.
3. The inlet of larynx is closed by the approximation of aryepiglottic folds. This prevents the food bolus from entering the larynx.
4. The larynx and pharynx are elevated behind the hyoid bond and the bolus is pushed down over the posterior surface of epiglottis, the closed inlet of larynx and the posterior surface of the arytenoid cartilages, by gravity and by contraction of the superior and middle constrictors and of the palatopharyngeus.

C. Third stage:
Involuntary.
1. Food passes from the lower part of the pharynx to the oesophagus.
2. This is brought about by the inferior constrictors of the pharynx.


TONGUE
It is a muscular organ situated in the floor of the mouth.Functions: taste, speech, mastication, deglutition.Parts: 1. Oral part2. Pharyngeal part
External features :
The tongue has 1. Body 2. Root 3. Tip/Apex
Body: It has a) curved upper surface called dorsum and
b) Inferior surface. Root:
Attached to the mandible and soft palate above and hyoid bone below.These 2 attachments prevent the tongue from being swallowed.
Tip:Forms the anterior free end which at rest lies behind the upper incisor teeth.
Separated by a V-shaped sulcus terminalis


Dorsum of the tongue
Convex in all directions
Divided into:
1) Oral part or anterior 2/3rds.
2) Pharyngeal or posterior post 1/3rd
The division is by a faint V-shaped groove called “sulcus terminalis” which contains a median pit called foramen caecum – represents the site from which the thyroid diverticulum grows down in the embryo.

The oral/papillary part of the tongue:
•Placed on the floor of the mouth.
•Its margins are free and in contact with the gums and teeth.
•The margin in front of the palatoglossal arch shows 4-5 vertical folds named foliate papillae.
•The superior surface shows a median furrow and is covered with papillae which make it rough.
•The inferior surface shows a median fold called the lingual frenum/frenulum linguae.
•On either side of the frenulum, there is a prominence produced by the deep lingual veins.
•More laterally, there is a fold called plica fimbriata that is directed forwards and medially towards the tip of the tongue.

The pharyngeal/lymphoid part of the tongue:
• It lies behind the palatoglossal arches and the sulcus terminalis.
• Its posterior surface i.e. the base of the tongue forms the anterior wall of oropharynx.
• The mucous membrane here is devoid of papillae and contains many lymphoid follicles that are collectively called as the lingual tonsil.
• This part is connected to the epiglottis by 3 folds of mucous membrane:1. Median glosso epitglottic fold.2. Right and left lateral glosso epiglottic folds.3. On either side of the median fold, there is a depression called
as vallecula.
• The lateral folds separate the vallecula from the piriform fossa.


PAPILLAE OF THE TONGUE
These are projections of mucous membrane or corium which give the anterior 2/3rds of the tongue, its characteristic roughness. They are:
1. Circumvallate papillae/vallate papillae:
• Larger in size • 8-12 in number and 1-2 mm in diameter.• Situated in front of the sulcus terminalis.• Each papilla is a cylindrical projection surrounded by a circular
sulcus and the walls of the papilla are raised above the surface.
2. Fungiform papillae:
• Present near the tip and margins.• Smaller than vallate papillae but larger than filiform papillae.• They are bright red in color and have a narrow pedicle with a large
round head.


3. Filiform papillae/conical papillae:
•Covers the presulcal area of the dorsum of the tongue.•They give the tongue surface, a velvety appearance.•They are the smallest and most numerous of the lingual papillae.•Each papilla is pointed and covered with keratin.•The apex is often split into filamentous processes.•They are non-gustatory.
4. Foliate papillae:
•Present on the posterolateral border of the tongue.•Each papilla is a pocket shaped invagination lined with the taste buds.•These invaginations protect the taste buds from direct physical damage.

Muscles of the tongue The tongue is divided into 2 halves by a middle fibrous septum.Each half contains:
4 intrinsic muscles –
1.Superior longitudinal2.Inferior longitudinal3.Transverse4. Vertical
4 extrinsic muscles –
1.Genioglossus 2.Hyoglossus3.Styloglossus4.Palatoglossus

Intrinsic muscles
•Occupy the upper part of the tongue.
•Attached to the submucous fibrous layer and to the median fibrous septum.
•They alter the tongue shape.
•Superior longitudinal muscle lies beneath the mucous membrane. It shortens the tongue and makes its surface concave.
•The inferior longitudinal muscles lies at the inferior surface of the tongue between the genioglossus and hyoglossus. It shortens and makes the dorsum of the tongue, convex.
•Transverse muscle extends from the median fibrous septum to the margins. It makes the tongue narrow and elongated.
•Vertical muscle is found at the borders of the anterior part of the tongue. It makes the tongue broad and flattened.

Extrinsic muscles
Genioglossus:
•It is a fan shaped muscle which forms the main bulk of the tongue.
•Arises from the upper genial tubercle of the mandible.
•From the tubercles, the fibers are divided as 3 groups –The upper fibers –inserted into the tip (they retract the tip)The middle fibers – into the dorsum (depress the tongue)The lower fibers – into the hyoid bone (pull the posterior part of the tongue forwards and hence protrude it out of the mouth).
•If this muscle is paralyzed, it will fall back on the oropharynx and block the air passage.
•During anaesthesia, the tongue is pulled forwards to clear the air passage.


Hyoglossus
•Forms an important land mark of the submandibular region.
•Arises from the whole length of greater cornua and lateral part of body of hyoid bone.
•Fibers run upwards and forwards and inserted into the side of the tongue between the styloglossus and inferior longitudinal muscle of the tongue.
•It depresses and makes the dorsum convex. It retracts the protruded tongue.
Styloglossus
•Arises from the tip and adjacent part of the anterior surface of the styloid process as well as from the upper end of the stylohyoid ligament.
•The fibers pass downwards and forwards and are inserted into the side of the tongue, intermingling with the fibers of the hyoglossus.
•During swallowing it pulls the tongue upwards and backwards.

Palatoglossus
•Arises at the oral surface of palatine aponeurosis.
•The fibers descend in the palatoglossal arch, and inserted to the side of the tongue at the junction of its oral and pharyngeal parts.
•It pulls up the root of the tongue, approximates the palatoglossal arches and thus closes the oropharyngeal isthmus.

Blood supply of the tongue
Arterial supply:
•Chiefly derived from the lingual artery, a branch of the ECA.•The root of the tongue is also supplied by the tonsillar and ascending pharyngeal arteries.
Venous drainage:
•Veins of the tongue are also called as venae comitantes.•2 venae comitantes accompany the lingual artery.•1 vena comitantes accompany the hypoglossal nerve.•The largest and principal vein of the tongue is the deep lingual vein which is visible on the inferior surface of the tongue. It runs backwards and crosses the genioglossus and the hyoglossus below the hypoglossal nerve.•These veins unite at the posterior border of the hyoglossus to form the lingual vein which ends either in the common facial vein or IJV.


Lymphatic drainage
•The tip of the tongue drains bilaterally to the sub mental lymph nodes.
•The right and left halves of anterior 2/3rds drain into the submandibular lymph nodes of the respective side.
•The posterior 1/3rd drain into the jugulo-omohyoid lymph nodes. These are called lymph nodes of the tongue.


Nerve supply of the tongue
Motor nerve: Hypoglossal nerve: supplies all the intrinsic and extrinsic muscles of the
tongue except palatoglossus.
Cranial root of the accessory nerve through the pharyngeal plexus: supplies palatoglossus muscle.
Sensory nerves:1.Lingual nerve – anterior 2/3 rds of the tongue (general sensation).
2.Chordatympani nerve – anterior 2/3rds of the tongue except circumvallate papillae (Taste sensation).
3.Glossopharyngeal nerve – posterior 1/3rd of the tongue and circumvallate papillae (both general sensation and taste).
4.Vagus nerve though internal laryngeal branch – posterior most part of the tongue.


Development of the tongue1.Epithelium : Anterior 2/3rds – From 2 lingual swellings and 1
tuberculum impar, which arise from the 1st branchial arch. The impar soon disappears. Therefore it is supplied by lingual nerve (post trematic) and chordatympani (pre trematic).
Posterior 1/3rd – From cranial large part of hypobranchial eminence i.e. from the 3rd arch. Therefore it is supplied by glossopharyngeal nerve.
Posterior most part - From 4th arch. Therefore it is supplied by the vagus nerve.
2.Muscles: They develop from the occipital myotomes which are supplied
by the hypoglossal nerve.
3.Connective tissue – Develops from the local mesenchyme



Taste sensation
The sensation of taste is perceived by end organs called ‘taste buds’.
Taste receptors in the young infant are about 10,000 in number but they begin to diminish as age advances.
Most of the taste receptors are situated in the dorsum of the tongue. A few receptors are also seen on the mucous membrane of the cheek and epiglottis.
Taste buds are scattered over the papillae present on the dorsum of the tongue.
Taste buds are commonly found along the sides of the vallate papillae, areas in between the papillae but are totally absent on the filiform papillae.
A single papilla may contain several taste buds. Thus a fungiform papilla may contain 8-10 taste buds and vallate papilla may contain 6-12 taste buds.

Taste bud •Each taste bud is an oval shaped structure which is packed with cells and in its tip, there is a pore, called the taste pore.
•The cells that fill the taste buds are 2 types: 1. Supporting/Sustentacular cells 2. Taste/Receptor cells.
•In an individual taste bud, the taste and supporting cells together constitute about 40-50 cells in number.•Amongst them about 12 cells are of ‘taste cell’ type and the remaining, ‘supporting cells’.
•Both the taste cells and the supporting cells are now believed to belong to the same class of cells and represent merely different stages of development.


• From the taste cells, hair like processes, the ‘microvilli’, project out of the pore.
• It is believed that the molecular receptors are present on these microvilli. Thus the taste sensation is received by the ‘taste cells’.
• Fine nerve fibers are found within each taste bud.• These nerve fibers carry taste sensation and constitute either the
chordatympani (anterior 2/3rds) or the glossopharyngeal nerve (posterior 1/3rd).
• Taste cells constantly degenerate and are replaced by new cells from the surrounding supporting cells throughout the life of an individual.
• Although the taste cells degenerate regularly the nerve terminals do not. But if the nerve fibers degenerate due to disease, the taste cells also die.

Mechanism of the taste sensation:
•The substance that causes taste sensation must be in solution and must attach itself with the molecular receptors of the microvilli.•This combination leads to some electro physiological changes to cause stimulation of the ‘taste cell’ and then the nerve fibers emerging from the taste bud are stimulated.•The impulse thus created then reaches the appropriate part of the brain.
Taste pathway:
•Taste sensation from the anterior 2/3 rd of the tongue, is carried by chordatympani nerve and then proceeds in the secondary division of the 7th cranial nerve and terminate on the nuclei of ‘tractus solitarius’ (NTS).•2nd order neurons arise from the NTS – relay to the opposite thalamus – further order neurons arise from the thalamus and terminate on the post central gyrus at its lower lateral part which is buried within the lateral sulcus.•This area is called as the highest cortical center for taste.


Features of taste sensation:
There are basically 4 fundamental taste sensations:
1. Salt2. Sweet3. Sour 4. Bitter
Admixture of these fundamental sensations in different proportions, produce different kinds of taste sensations.

•Salty taste is produced by: Inorganic and ionizable substances. NaCl is a classic example of the ions, the cation is the chief determinant for a salty taste.
•Sour taste is produced by substances which are acidic in nature, that is those substances which on ionization produces H+ ions. H+ ions produce the sour taste.
•Sweet tastes are produced by a large number of compounds, most of which are organic substances. E.g. : Various sugars like glucose, fructose, sucrose etc;
•Bitter tastes are produced by mostly organic compounds such as alkaloids. E.g.: Quinine, morphine, strychnine etc. Some inorganic compounds are also bitter in taste.
•Bile salt is an organic, non alkaloid substance with a bitter taste.

Specificity of taste buds:
• An individual taste bud can respond to more than one fundamental taste sensation, although the bud remain much more sensitive to one type of taste sensation than others.
• Individual taste cells in a given bud may also have varied sensitivity. For eg. in a given taste bud, some taste cells may be more sensitive to salt but much less sensitive to sweet or bitter tastes, other taste cells in the same bud might be less sensitive to salt but more sensitive to other tastes and so on.
Distribution of specific taste sensitivity:
1. Tip of the tongue – sweet taste2. The back (near the ‘V’) – bitter taste3. Sides – sour and salty tastes.4. Mid dorsum – insensitive to taste.


Biologic importance of taste:
•Sweet tastes provoke attraction and bitter tastes provoke rejection of food. This may be important for herbivorous animals where bitter plants often contain poisonous alkaloids.
•If there is a need for a specific nutrient in the body, the animal often develops a crave for it. Thus sodium deficient rats enjoy drinking of very salty solutions which normal rats would not touch.
Applied physiology:
•In radiotherapy, taste buds are destroyed and taste sensation is lost.
•The inability of few persons to sense the bitter taste of phenylthiocarbamide (PTC) unless given in a very high concentration is called as ‘selective taste blindness’. It is a genetic disorder.

Examination of the tongueExamination of the tongueDevelopmental disturbances of the Developmental disturbances of the
tonguetongueOther deformitiesOther deformitiesPeriodontal implicationsPeriodontal implicationsReferences References
OROPHARYNX AND TONGUE

Examination of the tongue
A routine periodontal examination should also include the examination of the tongue on the dorsal surface, lateral borders, and the base for:
ShapeColorSizeTextureConsistencyFissuresPapillaeCoatingsLesionsIndurations andMuscular actions.

DEVELOPMENTAL DISTURBANCES OF THE TONGUE

DEVELOPMENTAL DISTURBANCES OF THE TONGUE
MICROGLOSSIAPresence of a small or rudimentary tongue. Patients with
microglossia havedifficulties in eating and talking.MACROGLOSSIA An enlarged tongue, a somewhat more common condition
thanmicroglossia, may be either congenital or secondary in type. Congenital macroglossia is due to an over development of the
musculature as in:Down’s syndromeBeckwith's hypoglycemic syndromeIn cretinism or congenital hypothyroidism.
Secondary macroglossia may occur as a result of:A tumor of the tongue Acromegaly due to hyperpituitarism

•Macroglossia of either type may produce displacement of teeth and malocclusion because of the strength of the muscles involved and the pressure exerted by the tongue on the teeth.
•It is common to see crenation or scalloping of the lateral borders of the tongue in this condition, the tips of the scallops fitting into lie interproximal spaces between the teeth.
•There is no particular treatment for macroglossia except removal of the primary cause, although in some instances surgical trimming has been used to reduce the bulk of tissue present.


ANKYLOGLOSSIA •Complete ankyloglossia occurs as a result of fusion between the tongue and the floor of the mouth.•Partial ankyloglossia, or the common "tongue-tie," is usually a result of a short lingual frenum or one which is attached too near the tip of the tongue. Because of the restricted movement of the tongue, patients with this defect exhibit speech difficulties, chiefly in the pronunciation of certain consonants and diphthongs.•Although some cases of partial ankyloglossia are self-corrective, the majority are treated surgically by clipping the frenum. CLEFT TONGUE•A completely cleft or bifid tongue is a rare condition that is apparently due to lack of merging of the lateral lingual swellings of this organ.•A partially cleft tongue is considerably more common and is manifested simply as a deep groove in the midline of the dorsal surface.


•FISSURED TONGUE ("Scrotal" Tongue)
•The fissured tongue is a malformation manifested clinically by numerous small furrows or grooves on the dorsal surface, often radiating out from a central groove along the midline of the tongue.
•It has been reported to develop simultaneously with, or as a sequel to, geographic tongue or benign migratory glossitis.
•Fissured tongue is usually painless except in occasional cases in which food debris tends to collect in the grooves and produce irritation.
•Here the material may be removed by stretching and flattening the fissures and using a toothbrush or gauze sponge to cleanse the surface.


MEDIAN RHOMBOID GLOSSITIS (Central Papillary Atrophy of the Tongue)
Median rhomboid glossitis appears as an ovoid-, diamond-, or rhomboid- shaped reddish patch or plaque on the dorsal surface of the tongue immediately anterior to the circumvallate papillae.
Current evidence strongly suggests an etiologic relationship between median rhomboid glossitis and a localized chronic fungal infection, specifically Candida albicans.
Treatment:•There is no specific treatment for this lesion. Farman and his associates treated a group of patients with antifungal agents, either nystatin or amphotericin B, and found that the lesions regressed in some instances but not in others.•Sometimes these lesions will regress spontaneously without treatment.


BENIGN MIGRATORY GLOSSITIS (Geographic Tongue; Wandering Rash of the Tongue; Glossitis Areata Exfoliativa; Erythema Migrans)
•The condition consists usually of multiple areas of desquamation of the filiform papillae of the tongue in an irregular circinate pattern.
• The central portion of the lesion sometimes appears inflamed, while the border may be outlined by a thin, yellowish-white line or band.
•The fungiform papillae persist in the desquamated areas as small, elevated red dots.
•The areas of desquamation remain for a short time in one location and then heal and appear in another location, thus giving rise to the idea of migration.
Treatment and Prognosis:Since the etiology is unknown, the treatment is empirical. Because the condition is a benign one, there should be no need for concern other than to reassure the patient.


HAIRY TONGUE
•This condition is characterized by hypertrophy of the filiform papillae of the tongue, with lack of normal desquamation which may be extensive and form a thick matted layer on the dorsal surface.
•The color of the papillae may vary from yellowish white to brown or even black, depending upon their staining by such extrinsic factors as tobacco, certain foods, medicines, or chromogenic organisms of the oral cavity.
•The papillae, which may be of considerable length, occasionally will brush the palate of the patient and produce gagging.
Etiology:•Microorganisms, particularly fungi, including Candida albicans.
•Systemic disturbances (e.g., anemia, gastric upsets)

•Oral use of certain drugs (e.g., sodium perborate, sodium peroxide, and antibiotics such as penicillin and Aureomycin) may incite this condition. In the case of antibiotics, it is reasoned, there is suppression of growth of the normal oral bacterial population and a concomitant unrestrained growth of fungi.•Heavy smoking•In patients who have had exten sive x-ray radiation about the head and neck for the treatment of a tumor.
Treatment:•This is a benign condition. Treatment is empirical because the etiology is still unknown.•Food debris often collects deep between the papillae and produces irritation of the tongue. In such cases the tongue may be brushed with a toothbrush to promote desquamation and remove the debris.


ATROPHIC GLOSSITIS (Burning Tongue)
•In this situation the tongue appears smooth, shiny, and bald, with atrophied papillae.
•The condition is related to anemia that results from a deficiency of iron or combinations of deficiencies.


LINGUAL VARICES (Lingual or Sublingual Varicosities)
•A varix is a dilated, tortuous vein, most commonly a vein which is subjected to increased hydrostatic pressure but poorly supported by surrounding tissue.
•Varices involving the lingual ranine veins are relatively common, appearing as red or purple shotlike clusters of vessels on the ventral surface and lateral borders of the tongue as well as in the floor of the mouth.
•These varicosities represent an aging process and that, when they occur prior to 50 years of age, they may indicate premature aging.


LINGUAL THYROID NODULE
•The lingual thyroid is an anomalous condition in which follicles of thyroid tissue are found in the substance of the tongue, possibly arising from a thyroid anlage that failed to migrate to its predestined position or from anlage remnants that became detached and were left behind.
•The lingual thyroid may be manifested clinically as a nodular mass in or near the base of the tongue in the general vicinity of the foramen caecum
Etiology:•The benign enlargement of lingual thyroid tissue is thought to be due to functional insufficiency of the chief thyroid gland in the neck, since some patients with such a lingual lesion are without a demonstrable main thyroid gland.
•Other cases of lingual thyroid nodules occur in patients residing in goitrous areas.
•The failure of the primitive thyroid anlage to descend is the cause of the majority of cases of nongoitrous sporadic cretinism.


OTHER DEFORMITIES

OTHER DEFORMITIES
GLOSSODYNIA
•It is the pain and the burning sensation in the lingual and oral mucosa. It may also be experienced as a sandy feeling, tickling or itching sensation in the tongue.
•It occurs particularly in postmenopausal women with accompanying complaints of changes in the taste sensation and a dry mouth.
Etiology:
•Geographic tongue, fissured tongue, and median rhomboid glossitis may produce glossodynia.
•Lichen planus may also cause glossodynia which some authors refer it to as ‘lichen rubber glossodynicus’.
•Habits such as sucking, constantly moving the tooth along the teeth or dentures may also cause pain especially in the presence of sharp edges of broken down teeth and restorations.

• Pernicious anemia.• Plummer Vinson syndrome• Hormonal changes during menopause• Psychiatric diseases such as depression,
cancerophobia, neurosis, schizophrenia etc.• As a side effect to certain drugs used to modify
psychological functions or mental states.
Treatment:
• Stop spicy foods or beverages
• Psychotherapy
• Anti depressant drugs with little anticholinergic effects for depression induced glossodynia.

STOMATITIS AREATA MIGRANS
•Circular or arcuate lesions of ventral tongue, floor of the mouth and buccal vestibule are seen similar to benign migratory glossitis.
•Clinical behaviour- similar to that of benign migratory glossitis but no associated traumatic factors.
Treatment:
•Removal of local irritational causes and empirical treatment
•Patient to stop brushing the tongue as it intensifies and prolongs the condition.


CHRONIC ULCERS•They differ from ulcers of other parts of the oral cavity of the mouth as they tend to remain relatively unchanged for long periods.
•They are commonly found on the middle and posterior thirds of the lateral borders of the tongue.
•Appear as a shallow ulceration surrounded by a raised rolled border of fibrous tissue and an outer wide zone of induration.
Etiology:•Injury as a result of lack of tongue coordination during mastication caused by prescribed medication or a systemic condition such as a Parkinson’s disease or a stroke that involves the cranial nerves.
•Enlarged tongue also causes injury.
•In denture wearers, malpositioned posterior teeth on the denture base may be a contributing factor.


TONGUE WITH PERIODONTAL IMPLICATIONS

TONGUE THRUST HABIT
Tongue thrust is defined as:
The infantile pattern of suckle-swallow movement in which the tongue is placed between the incisor teeth or alveolar ridges which may result in an anterior open bite, deformation of jaws, and abnormal function.
Etiology of tongue thrust
•Genetic factors: Hypertonic orbicularis oris activity.•Learned behavior (habit):
a. Improper bottle feedingb. Prolonged thumb suckingc. Prolonged tonsillar and upper respiratory tract infectionsd.Prolonged duration of tenderness of gum or teeth can result in a change in swallowing pattern to avoid pressure on the tender zone

•Maturational: Sometimes the maturation is delayed and thus infantile swallow persists for a longer duration of time. •Mechanical restrictions: The presence of certain conditions such as macroglossia, constricted dental arches and enlarged adenoids predispose to tongue thrust habit.
•Neurological disturbance: Such as hyposensitive palate and moderate motor disability can cause tongue thrust habit.

Clinical features
The tongue thrust habit can be associated with the following features:
a. Proclination of anterior teeth.b. Anterior open bite.c. Bimaxillary protrusion.d. Posterior open bite in case of lateral tongue thrust.e. Posterior crossbite
Management of tongue thrust
The management of tongue thrust involves interception of the habit followed by treatment to correct the malocclusion.

ORAL MALODOR
• Oral malodor in healthy patients arises from the oral cavity and generally originates on the dorsum of the tongue.
• The volatile sulfur compounds (VSCs) producing anaerobic bacteria appear to be the primary source of these odors.
• The bacteria hydrolyze the proteins to amino acids, three of which contain sulfur groups and are the precursors to VSCs.
• These gaseous substances consist primarily of:
1. Hydrogen sulfide (H2S)2. Dimethyl sulfide ([CH3]2S)3. Methylmercaptan (CH3SH) and4. Sulfur dioxide (SO2).

The tongue plaque coating
•The tongue is an excellent site for the growth of microorganisms since the papillary nature of the tongue dorsum creates a unique ecological site that provides an extremely large surface area, favoring the accumulation of oral bacteria.
•The proteolytic, anaerobic bacteria that reside on the tongue play an essential part in the development of OM.
•The presence of tongue coating has been shown to have a correlation with the density or total number of bacteria in the tongue-plaque coating.
•Higher mouth odor organoleptic scores are associated with heavy tongue coating and correlate with the bacterial density on the tongue and with the BANA-hydrolyzing bacteria: T.denticola, P.gingivalis, and B.forsythus.
•Approximately 80% to 90% of the oral malodor originates from the dorsum of the tongue. Therefore, treatments targeted toward reduction of the oral malodor will require antimicrobial agents directed against the tongue microflora.

TONGUE CLEANING
Total mouth cleanliness includes tongue care.
A. Microorganisms of the Tongue
1. Main foci for oral microorganisms are: a. Dorsum of tongue. b. Gingival sulci and pockets. c. Bacterial plaque on all teeth.
2. Microorganisms in saliva are principally from the tongue.
3. The microflora of the tongue is not constant, but changes frequently. (Van der Weijden &Van der Velden in 1991)
B. Effects of Cleaning the Tongue
1. Retards bacterial plaque formation and total plaque accumulation.2. Reduces number of microorganisms.3. Reduces potential for halitosis.4. Contributes to overall cleanliness.

C. Anatomic Features of Tongue Conducive to Debris Retention
1. Surface Papillae: Numerous filiform papillae extend as minute projections, whereas fungiform papillae are not as high and create elevations and depressions that entrap debris and microorganisms.
2. Fissured Tongue: Fissures may be several millimeters deep and retain debris.
D. Brushing Procedure
1. Hold the brush handle at a right angle to the midline of the tongue and direct the brush tips toward the throat.
2. With the tongue extruded, the sides of the filaments are placed on the posterior part of the tongue surface.
3. With light pressure, draw the brush forward and over the tip of the tongue. Repeat three or four times. Do not scrub the papillae.

E. Tongue Scraper
• Tongue cleaners or scrapers may be made of plastic, stainless steel, or other flexible metal.
• They are curved and wide enough to fit over the tongue surface without hitting the teeth.
• Some are made with a single handle, whereas others have two ends to hold.
1. Purpose: By removing debris and microorganisms, the patient can expect tongue scraping to contribute to overall mouth cleanliness, reduce the numbers of bacteria available for plaque formation, and lessen mouth odors.The procedure can be especially helpful for the patient who has xerostomia, a coated tongue, deep fissures, or who smokes.
2. Procedure: Place the arch toward the posterior of the dorsal surface. Press with a light but firm stroke, and pull forward. Repeat several times, covering the entire surface of the tongue. Wash the tongue scraper under running water.


REFERENCES
1. A Colour Atlas Of Human Anatomy – Mc Minn & Hutchings.2. Human Anatomy – Regional and Applied - B.D.Chaurasia – 4th Edition.3. Atlas of Human Anatomy – Frank H. Netter – 3rd Edition.4. Gray’s Anatomy – 38th Edition.5. Text Book of Medical Physiology – Guyton & Hall – 10th Edition.6. Concise Medical Physiology – Chaudhuri – 3rd Edition.7. Physiology – Berne, Levy, Koeppen, Stanton – 5th Edition.8. Clinical Oral Physiology – Timothy S Miles, Bergitte Nauntofte, Peter
Svenson.9. Illustrated Physiology – Mackenna & Callander – 6th Edition 10. An Introduction to Human Embryology – Inderbir Singh – 6th Edition.11. Langman’s Medical Embryology - 9th Edition.12. Orthodontics: The Art & Science – S.I.Bhalajhi.13. A Textbook of Oral Pathology – Shafer, Hine, Levy – 4th Edition.14. Clinical practice of the Dental Hygienist – Wilkins – 8th Edition.15. Antibiotic & antimicrobial use in Dental Practice – 2nd Edition.16. Color Atlas of Clinical Oral Pathology – Neville, Damm & White – 2nd Edition.17. JCP 2001;28(10):970-978.18. JP 1972;43(7):418-422.