TISSUE DIELECTRIC CONSTANT (TDC) MEASUREMENTS AS A … · paired forearm TDC values and arm-to- arm...
Transcript of TISSUE DIELECTRIC CONSTANT (TDC) MEASUREMENTS AS A … · paired forearm TDC values and arm-to- arm...

142
Lymphology 47 (2014) 142-150
TISSUE DIELECTRIC CONSTANT (TDC) MEASUREMENTS AS A MEANS OF CHARACTERIZING LOCALIZED TISSUE WATER IN ARMS OF WOMEN WITH AND WITHOUT BREAST CANCER
TREATMENT RELATED LYMPHEDEMA
H.N. Mayrovitz, D.N. Weingrad, S. Davey
College of Medical Sciences (HNM), Health Professions Division, Nova Southeastern University, Ft. Lauderdale; Cancer HealthCare Associates (DNW), Aventura; Healing Hands of Lymphatics (SD),Hallandale Beach, Florida, USA
ABSTRACT
Quantitative measurements to detectlymphedema early in persons at-risk for breastcancer (BC) treatment-related lymphedema(BCRL) can aid clinical evaluations. SinceBCRL may be initially manifest in skin andsubcutis, the earliest changes might best bedetected via local tissue water (LTW)measurements that are specifically sensitive to such changes. Tissue dielectric constant(TDC) measurements, which are sensitive toskin-to-fat tissue water, may be useful for thispurpose. TDC differences between lymphe-dematous and non-lymphedematous tissue hasnot been fully characterized. Thus we measuredTDC values (2.5 mm depth) in forearms ofthree groups of women (N=80/group): 1)healthy with no BC (NOBC), 2) with BC butprior to surgery, and 3) with unilaterallymphedema (LE). TDC values for all armsexcept LE affected arms were not significantlydifferent ranging between 24.8 ± 3.3 to 26.8 ±4.9 and were significantly less (p<0.001) ascompared to 42.9 ± 8.2 for LE affected arms.Arm TDC ratios, dominant/non-dominant for NOBC, were 1.001 ± 0.050 and at-risk/contralateral for BC were 0.998 ± 0.082 withboth significantly less (p<0.001) than LEgroup affected/control arm ratios (1.663 ±0.321). These results show that BC per se does
not significantly change arm LTW and thatthe presence of BCRL does not significantlychange LTW of non-affected arms. Further,based on 3 standard deviations of measuredarm ratios, our data demonstrates that an at-risk arm/contralateral arm TDC ratio of 1.2and above could be a possible threshold todetect pre-clinical lymphedema. Furtherprospective measurement trial are needed toconfirm this value.
Keywords: lymphedema, tissue dielectricconstant, skin water, breast cancer,lymphedema detection
Quantitative measurements for earlydetection of lymphedema in persons at-riskfor breast cancer treatment-related lymphe-dema (BCRL) can be an aid to standardclinical evaluations. To be useful in a clinicalsetting, such measurements and associateddevices should optimally be noninvasive andreadily implemented in an ordinarily busyand time pressured environment. Potentialcandidates that have been used or may besuitable for routine use include various armmetrics including arm girth and arm volumes(1-12) based on manual or automatedmethods and arm bioimpedance measured atsingle or multiple frequencies (13-24).
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

143
However, since BCRL may be initiallymanifest as subtle small increases in dermaland hypodermal fluids (25-28), optimumdetection of these earliest changes mightrequire localized measurements of skin-to-fattissue water changes. Such changes areevaluable by measuring the local tissuedielectric constant (TDC) since TDC valuesare directly related to tissue water content(29-35). A feature of the TDC method, notpresent in other methods, is its ability tomeasure at almost any body site in whichchanges in tissue water are of clinical interest.Although the TDC method has been appliedin a variety of ways to assess tissue fluid andits change (36-48), the needed comprehensivecharacterizations of expected differencesbetween lymphedematous and non-lymphedematous tissue has not been fullyestablished. Thus, our main goal was toprovide such a characterization by comparingpaired forearm TDC values and arm-to- armTDC ratios, measured to 2.5 mm depth, inthree groups of women: 1) healthy womenwith no breast cancer (NOBC), 2) womenrecently diagnosed with breast cancer (BC)but prior to their surgery, and 3) women with clinically diagnosed overt unilaterallymphedema (LE).
METHODS
Subjects
A total of 240 women, equally dividedinto three groups of 80, were evaluated aftersigning a University Institutional ReviewBoard approved informed consent. Thegroups consisted of 1) healthy women with no breast cancer (group NOBC), 2) womenrecently diagnosed with breast cancer butprior to their surgery (group BC), and 3)women with unilateral BCRL (group LE).Entry requirements for the BC group werethat they had recently (within one month)been diagnosed with breast cancer and wereawaiting surgery. These patients werereferred by their surgeon for a pre-surgery
evaluation. Entry requirements for the LEgroup were that they had unilateral lymphe-dema and had been referred for lymphedematherapy. Entry requirements for the NOBCgroup were that they had no history of breastcancer, had no previous surgery or serioustrauma to either arm, and were in self-reported good health. Pertinent features ofthe three study groups are shown in Table 1.From data available for the LE group, theaverage number of axilla nodes removed atsurgery was (mean ± SD) 13.3 ± 9.7 with arange of 3-27 and the average reportedduration of the lymphedema was 74.6 ± 91.1months with a range of 2-433 months. Asmay be seen from the Table 1, ages and BMIof the groups were significantly differentfrom each other in the order NOBC < BC <LE (p<0.001) indicating a wide representativerange of subject features.
Tissue Dielectric Constant (TDC)Measurement Device
TDC was measured with theMoistureMeter-D (Delfin Technologies Ltd,Kuopio, Finland). The skin-contacting part of the device consists of a cylindrical probethat is connected to a control unit thatdisplays the tissue dielectric constant whenthe probe is placed in contact with the skin.The probe itself acts as an open-ended coaxialtransmission line (29,49) and the principle of operation has been well described(29,31,34,49,50). In brief, a 300 MHz signal,generated within the control unit, istransmitted to the tissue via the probe incontact with the skin. The portion of theincident electromagnetic wave reflected fromthe tissue depends on the tissue’s dielectricconstant, which itself depends on the amountof free and bound water in the tissue volumethrough which the wave passes. Reflectedwave information is processed in the controlunit and the dielectric constant is displayed.For reference, pure water has a value ofabout 78 and the display scale range is 1 to80. The effective measurement depth depends
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

144
on the probe dimensions, with larger spacingbetween inner and outer conductors corres-ponding to greater penetration depths. Probesare available to measure to effective depths of 0.5, 1.5, 2.5 and 5.0 mm, but this studyutilized only the 2.5 mm depth probe so as toinclude the epidermis, the dermis, and part of the hypodermis of the target forearm skin.This probe has an outside diameter of 23 mmand inner-to-outer conductor spacing of 5 mm.
TDC Measurement Procedure
TDC measurements began after a subjectwas lying supine for 10 minutes on a paddedexamination table with arms at her side and hands positioned with palms up therebyexposing the anterior surface of bothforearms. A standardized measurement sitelocated 6 cm distal to the antecubital fossaalong the forearm midline was marked with adot to serve as a reference center point forprobe placement. A single TDC measurementwas obtained by placing the probe in contactwith the skin of one arm and held in positionusing gentle pressure. After about 10 secondsan audible signal indicated completion of the
measurement. The probe was then used tomake a measurement on the other arm tocomplete a measurement pair. This processwas continued to obtain triplicate measure-ment pairs. Alternating between arm sideswas used as a way to help obtain pairedvalues as close in time as possible. For eacharm, the three measurements were averagedand used to characterize the arm site averageTDC value.
Arm Girth Measurements
After the TDC measurements, circum-ferences (girth) of the arm at the referencecenter point were measured using a calibratedGulick-type spring-loaded tape measure witha tension gauge to help insure uniformmeasurements.
Data Reduction and Analysis
BC group paired-arms were designatedas at-risk and contralateral and LE grouppaired-arms were designated as affected andcontralateral. NOBC group paired-arms weredesignated as dominant and non-dominant
TABLE 1Study Group Features
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

145
depending on the subject’s self report. Pairedarm mean values ± SD and paired-arm ratioswere determined as dominant/non- dominant,at-risk/contralateral, and affected/contralateralfor NOBC, BC, and LE groups, respectively.Overall differences among the three groupswith respect to each arm-side TDC or girthvalue and the TDC or girth arm-to-arm ratiowas tested for using an analysis of variancemodel (ANOVA) with Bonferroni post hoccomparison tests. Differences between armside TDC and girth values were subsequentlytested for using paired t-tests. In all cases, ap-value <0.05 was taken as significant. Testsfor correlations among parameters were doneusing Pearson coefficients. All statisticalanalyses were done using SPSS version 13.0(SPSS Inc., 233 S. Wacker Drive, Chicago, IL).
RESULTS
Arm Girths
Arm girth differences between sides andbetween groups were insignificant for boththe NOBC and BC groups, whereas, as was tobe expected, the girth difference betweensides for the LE group was highly significant(p<0.001) as summarized in (Table 2).
Although the LE group arm-to-arm girthdifference was highly significant, the LEcontralateral arm girth was insignificantlydifferent from the girth of any arm of theNOBC or BC group. Girth ratios, assessed asthe at-risk to the contralateral arm in the BCgroup (0.997 ± 0.034), was insignificantlydifferent than the dominant/non-dominantratio for the NOBC group (1.013 ± 0.033)with both ratios being significantly less thanthe affected/contralateral ratio of the LEgroup (1.216 ± 0.152, p<0.001).
TDC and Local Tissue Water
As with the girth findings, arm TDCdifferences between sides and between groups were insignificant for both the NOBCand BC groups, whereas inter-arm TDCdifferences for the LE group were highlysignificant (p<0.001) as summarized in Table 2. Although the LE group inter-armTDC difference was highly significant, theTDC value of the LE contralateral arm wasinsignificantly different from TDC valuesmeasured on all arms of the NOBC or BCgroups. TDC ratios, assessed as at-risk tocontralateral arms in the BC group (0.998 ±0.080, range 0.838-1.159), were insignificantly
TABLE 2TDC and Girth Results
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

146
different than dominant/non-dominant armratios for the NOBC group (1.001 ± 0.050,range 0.871- 1.158) with both of these TDCinter-arm ratios significantly less than theaffected/contralateral TDC ratio of the LEgroup (1.663 ± 0.319, p<0.001, range 1.176-2.438). Girth ratios compared to TDC ratiosdid not significantly differ between NOBC orBG groups but the TDC ratio was signifi-cantly (p<0.001) greater than the girth ratiofor the LE group.
Correlations of Parameters
As might have been anticipated, therewas a strong positive correlation (p<0.001)between paired-arm TDC values and paired-arm girths within groups. Group NOBCcorrelation coefficients for TDC and girthwere respectively 0.958 and 0.942. However,there was no significant correlation betweenTDC and girth either for absolute values orfor arm-to-arm ratios. Correlation patterns ofthe BC group were similar to the NOBCgroup with correlation coefficients for TDCand girth being respectively 0.843 and 0.948with no other significant correlations amongparameters. For the LE group, these corre-lations were also significant (p<0.001) butwith smaller correlation coefficients being forTDC and girth 0.463 and 0.790, respectively.
DISCUSSION
Measuring local skin-to-fat tissue waterbased on the tissue dielectric constant (36,51-53) represents an adjunctive approachto better characterize lymphedema and topotentially provide a method for an earlierdetection of latent or incipient lymphedema.The TDC method differs from limb volume(1,3,4,7,8) and bioimpedance methods(22,23,54,55) in that with a 2.5 mm measure-ment depth as used here, it only interrogatesskin and subcutaneous tissue compartmentsin which some of the earliest changes arelikely to occur (27,28). Since it is a localmeasurement, it can be used at almost any
anatomical site that is at-risk for lymphe-dema development. Although differences intissue water between frankly lymphedematousand contralateral non-affected limbs havebeen determined by TDC measurements(36,39), differentials between limbs of healthypersons and persons with breast cancer butwithout lymphedema have only been partiallycharacterized (56). Thus, a major goal of thisstudy was to characterize forearm local tissuewater parameters, as assessed by TDCmeasurement, among women without breastcancer (NOBC) and with breast cancer (BC)in comparison with women with breast cancertreatment related lymphedema (LE). Animportant major intended component of thischaracterization was the assessment of therange of TDC variability among groups withthe thought of devising suitable referenceranges and TDC thresholds potentially usefulto detect early lymphedema development.
One main result shows that, except forpatients with lymphedema (the LE group),absolute TDC values of arms are similar andinsignificantly different from each other. This includes all arms of the BC and NOBCgroups and the contralateral arm of the LEgroup. The ratio of affected to contralateralarm TDC values, expressed as mean ± SD forthe 80 evaluated women with lymphedema(1.663 ± 0.319) was much greater than thenear unity ratios found in women in the BCgroup (0.998 ± 0.082) or the NOBC group(1.001 ± 0.050). The closeness of the TDCvalues of all arms for the BC and NOBCgroups strongly suggests that breast cancer in the BC group did not significantly affectlocal tissue water in either arm. The TDCfindings also indicate that lymphedemapresence in the LE group did not significantlyaffect local tissue water in the contralateralarm of these women.
Because the at-risk arm may be thepatient’s dominant or non-dominant arm(Table 1), it is useful to characterize thedominant/non-dominant TDC ratio with aslarge a data set as meaningfully available.Since the present analyses indicated no
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

147
difference between BC and NOBC groupswith respect to arm-to-arm TDC values, wecombined these groups (N=160) to determinethe combined dominant/non-dominant TDCratio of 0.995 ± 0.067 (range 0.838 - 1.159).Corresponding girth ratios were 1.014 ± 0.032(range 0.829 - 1.084). This combined data set provides values from a wide age range (18-82 years) and a wide BMI range (14.7 - 48.1Kg/m2) that can be used to estimate the effectsof age and BMI on TDC and girth ratios.
For this combined data set, correlationanalyses revealed a near zero Pearsoncorrelation coefficient between age or BMIand TDC or girth ratios. This indicates thatage and BMI are not factors of significantrelevance with respect to dominant/non-dominant arm ratios. The local TDC andgirth ratios here obtained may be comparedwith whole arm ratios obtained viabioimpedance measurements for a group of60 control subjects (23) where a dominant
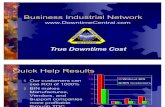
Fig. 1. Distribution of Arm-to-Arm TDC Ratios. NOBC, BC, and LE correspond to groups with no breast cancer,breast cancer, and lymphedema respectively each with N = 80 subjects. BC ratios were calculated as at-riskarm/contralateral, LE ratios were calculated as affected arm/contralateral, and NOBC ratios were calculated asdominant arm/non-dominant. Short horizontal bar on each plot indicates group average. NOBC and BC ratios wereinsignificantly different from each other and both were significantly less than for the LE group (p<0.001). Thethreshold line indicates the mean dominant/non-dominant ratio for all non-lymphedematous subjects (N=160) plus3SD. The cut-point line indicates the TDC ratio that is less than observed for any patient with lymphedema and isgreater than any observed for non-lymphedematous persons.
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

148
to non-dominant ratio of 0.964 ± 0.034 wasobtained and for a group of 32 subjects inwhich a dominant to non-dominant ratio was 1.024 (21). It should be noted that withimpedance measurements higher values ofarm water yield lower impedance values.
As previously stated, one of the goals ofthis study was to provide a reference data set from which estimates of deviations inlocal TDC values from normality might bedetected early in the process of lymphedemadevelopment. One methodological approachis to define a threshold for sub-clinicallymphedema as a value that equals or exceedsthe reference mean plus some multiple of thereference standard deviation. This approachhas been utilized when whole arm impedancevalues were to be used as the assessmentparameter (13,23) and a threshold inter-armimpedance ratio of between 1.106 to 1.134was determined depending on hand domi-nance (13). Applying the same conservativecriteria to the present TDC data, using thestandard deviation of the 160 dominant tonon- dominant TDC ratios indicates a 3SDvalue of 0.201 that when added to the meanTDC ratio yields a threshold value of 1.196which we may round up to 1.200. It isnoteworthy that all subjects within our non-lymphedematous sample population(combined BC and NOBC groups) had aninter-arm TDC ratio less than this thresholdwith the overall arm- to-arm TDC distribu-tions shown in Fig. 1. For the LE group, 78 of80 women (97.5%) had TDC ratios exceedingthis threshold. This implies that had thethreshold criteria been applied, 2/80 (2.5%) of the group that actually had lymphedemawould not have been detected with thismethod. An alternate approach to arriving at suitable cut-point criteria is to determine if there is a TDC ratio that is less thanobserved for any patient with lymphedemaand is greater than observed for any non-lymphedematous patient. For the presentevaluated population a value satisfying thiscriterion is 1.165 and is shown as the smalldotted line in Fig. 1.
In summary, the present results providereference TDC values derived from a largegroup of female forearms and also provide apractical at-risk/contralateral arm TDC ratioof 1.200 and above that could be useful toindicate pre-clinical or impending lymph-edema if measured in women who havepreviously been surgically treated for breastcancer. It is emphasized, however, that thesetheoretically calculated TDC thresholds havenot as yet been prospectively substantiatedand should conservatively be viewed asreferenced-based targets for future prospec-tive research investigations.
REFERENCES
1. Mayrovitz, HN, N Sims, J Macdonald:Assessment of limb volume by manual andautomated methods in patients with limbedema or lymphedema. Adv. Skin WoundCare 13 (2000), 272-276.
2. Armer, JM, BR Stewart, RP Shook: 30-Monthpost-breast cancer treatment lymphoedema. J. Lymphoedema. 4 (2009), 14-18.
3. Armer, JM, BR Stewart: A comparison offour diagnostic criteria for lymphedema in apost-breast cancer population. Lymphat. Res.Biol. 3 (2005), 208-217.
4. Casley-Smith, JR: Measuring andrepresenting peripheral oedema and itsalterations. Lymphology 27 (1994), 56-70.
5. Cormier, JN, Y Xing, I Zaniletti, et al:Minimal limb volume change has a significantimpact on breast cancer survivors. Lymphology42 (2009), 161-175.
6. Latchford, S, JR Casley-Smith: Estimatinglimb volumes and alterations in peripheraledema from circumferences measured atdifferent intervals. Lymphology 30 (1997),161-164.
7. Mayrovitz, HN: Limb volume estimates basedon limb elliptical vs. circular cross sectionmodels. Lymphology 36 (2003), 140-143.
8. Ridner, SH, LD Montgomery, JT Hepworth,et al: Comparison of upper limb volumemeasurement techniques and arm symptomsbetween healthy volunteers and individualswith known lymphedema. Lymphology 40(2007), 35-46.
9. Zimmermann, A, M Wozniewski, ASzklarska, et al: Efficacy of manual lymphaticdrainage in preventing secondarylymphedema after breast cancer surgery.Lymphology 45 (2012), 103-112.
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

149
10. Sander, AP, NM Hajer, K Hemenway, et al:Upper-extremity volume measurements inwomen with lymphedema: A comparison ofmeasurements obtained via water displace-ment with geometrically determined volume.Phys. Ther. 82 (2002), 1201- 1212.
11. Taylor, R, UW Jayasinghe, L Koelmeyer, et al: Reliability and validity of arm volumemeasurements for assessment of lymphedema.Phys. Ther. 86 (2006), 205-214.
12. Fife, CE, S Davey, EA Maus, et al: Arandomized controlled trial comparing twotypes of pneumatic compression for breastcancer-related lymphedema treatment in the home. Support Care Cancer 20 (2012),3279-3286.
13. Ward, LC, E Dylke, S Czerniec, et al:Confirmation of the reference impedanceratios used for assessment of breast cancer-related lymphedema by bioelectricalimpedance spectroscopy. Lymphat. Res. Biol.9 (2011), 47-51.
14. Ward, LC, E Dylke, S Czerniec, et al:Reference ranges for assessment of unilaterallymphedema in legs by bioelectricalimpedance spectroscopy. Lymphat. Res. Biol.9 (2011), 43-46.
15. Ward, L, A Winall, E Isenring, et al:Assessment of bilateral limb lymphedema bybioelectrical impedance spectroscopy. Int. J.Gynecol. Cancer 21 (2011), 409-418.
16. Smoot, BJ, JF Wong, MJ Dodd: Comparisonof diagnostic accuracy of clinical measures ofbreast cancer-related lymphedema: Areaunder the curve. Arch. Phys. Med. Rehabil. 92(2011), 603-610.
17. Kim, L, JY Jeon, IY Sung, et al: Prediction of treatment outcome with bioimpedancemeasurements in breast cancer relatedlymphedema patients. Ann. Rehabil. Med. 35(2011), 687-693.
18. Gaw, R, R Box, B Cornish: Bioimpedance inthe assessment of unilateral lymphedema of alimb: The optimal frequency. Lymphat. Res.Biol. 9 (2011), 93-99.
19. York, SL, LC Ward, S Czerniec, et al: Singlefrequency versus bioimpedance spectroscopyfor the assessment of lymphedema. BreastCancer Res. Treat. 117 (2009), 177-182.
20. Ward, LC, S Czerniec, SL Kilbreath:Quantitative bioimpedance spectroscopy forthe assessment of lymphoedema. BreastCancer Res. Treat. 117 (2009), 541-547.
21. Ridner, SH, MS Dietrich, J Deng, et al:Bioelectrical impedance for detecting upperlimb lymphedema in nonlaboratory settings.Lymphat. Res. Biol. 7 (2009), 11-15.
22. Cornish, B: Bioimpedance analysis: Scientific
background. Lymphat.Res.Biol.4 (2006), 47-50.23. Cornish, BH, M Chapman, C Hirst, et al:
Early diagnosis of lymphedema using multiplefrequency bioimpedance. Lymphology 34(2001), 2-11.
24. Ward, LC, BH Cornish: Measuring peripheraloedema and bioimpedance. Lymphology 28(1995), 41-47.
25. Mellor, RH, NL Bush, AW Stanton, et al:Dual-frequency ultrasound examination ofskin and subcutis thickness in breast cancer-related lymphedema. Breast J. 10 (2004), 496-503.
26. Modi, S, AW Stanton, RH Mellor, et al:Regional distribution of epifascial swellingand epifascial lymph drainage rate constantsin breast cancer-related lymphedema.Lymphat. Res. Biol. 3 (2005), 3-15.
27. Stanton, AW, RH Mellor, GJ Cook, et al:Impairment of lymph drainage in subfascialcompartment of forearm in breast cancer-related lymphedema. Lymphat. Res. Biol. 1(2003), 121-132.
28. Stanton, AW, S Modi, RH Mellor, et al:Recent advances in breast cancer-relatedlymphedema of the arm: Lymphatic pumpfailure and predisposing factors. Lymphat.Res. Biol. 7 (2009), 29-45.
29. Aimoto, A, T Matsumoto: Noninvasivemethod for measuring the electrical propertiesof deep tissues using an open-ended coaxialprobe. Med. Eng. Phys. 18 (1996), 641-646.
30. Alanen, E, T Lahtinen, J Nuutinen:Variational formulation of open-ended coaxial line in contact with layered biologicalmedium. IEEE Trans. Biomed. Eng. 45(1998), 1241-1248.
31. Alanen, E, T Lahtinen, J Nuutinen:Penetration of electromagnetic fields of anopen-ended coaxial probe between 1 MHz and 1 GHz in dielectric skin measurements.Phys. Med. Biol. 44 (1999), N169-176.
32. Lahtinen, T, J Nuutinen, E Alanen: Dielectricproperties of the skin. Phys. Med. Biol. 42(1997), 1471-1472.
33. Nuutinen, J, R Ikaheimo, T Lahtinen:Validation of a new dielectric device to assesschanges of tissue water in skin and subcutan-eous fat. Physiol. Meas. 25 (2004), 447-454.
34. Stuchly, MA, TW Athey, SS Stuchly, et al:Dielectric properties of animal tissues in vivoat frequencies 10 MHz-1 GHz.Bioelectromagnetics 2 (1981), 93-103.
35. Stuchly, MA, A Kraszewski, SS Stuchly, et al: Dielectric properties of animal tissues invivo at radio and microwave frequencies:Comparison between species. Phys. Med. Biol.27 (1982), 927-936.
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.

150
36. Mayrovitz, HN: Assessing local tissue edemain postmastectomy lymphedema. Lymphology40 (2007), 87-94.
37. Mayrovitz, HN: Assessing lymphedema bytissue indentation force and local tissue water.Lymphology 42 (2009), 88-98.
38. Mayrovitz, HN, S Davey: Changes in tissuewater and indentation resistance of lymphe-dematous limbs accompanying low level lasertherapy (LLLT) of fibrotic skin. Lymphology44 (2011), 168-177.
39. Mayrovitz, HN, S Davey, E Shapiro:Localized tissue water changes accompanyingone manual lymphatic drainage (MLD)therapy session assessed by changes in tissuedielectric constant inpatients with lowerextremity lymphedema. Lymphology 41(2008), 87-92.
40. Mayrovitz, HN, S Davey, E Shapiro: Localtissue water changes assessed by tissuedielectric constant: Single measurementsversus averaging of multiple measurements.Lymphology 41 (2008), 186-188.
41. Mayrovitz, HN, M Bernal, F Brlit, et al:Biophysical measures of skin tissue water:Variations within and among anatomical sitesand correlations between measures. Skin Res.Technol. 19 (2013), 47-54.
42. Mayrovitz, HN, M Bernal, S Carson: Genderdifferences in facial skin dielectric constantmeasured at 300 MHz. Skin Res. Technol.(2011), 504-510.
43. Jensen, MR, S Birkballe, S Nørregaard, et al:Validity and interobserver agreement of lowerextremity local tissue water measurements inhealthy women using tissue dielectricconstant. Clin. Physiol. Funct. Imaging 32(2012), 317-322.
44. Laaksonen, DE, J Nuutinen, T Lahtinen, et al: Changes in abdominal subcutaneous fatwater content with rapid weight loss andlong-term weight maintenance in abdominallyobese men and women. Int. J. Obes. Relat.Metab. Disord. 27 (2003), 677-683.
45. Petaja, L, J Nuutinen, A Uusaro, et al:Dielectric constant of skin and subcutaneousfat to assess fluid changes after cardiacsurgery. Physiol. Meas. 24 (2003), 383-390.
46. Papp, A, T Lahtinen, M Harma, et al:Dielectric measurement in experimentalburns: A new tool for burn depthdetermination. Plast. Reconstr. Surg. 119(2007), 1958- 1960.
47. Nuutinen, J, T Lahtinen, M Turunen, et al: A dielectric method for measuring early and late reactions in irradiated human skin.Radiother. Oncol. 47 (1998), 249-254.
48. Miettinen, M, J Monkkonen, MR Lahtinen,
et al: Measurement of oedema in irritant-exposed skin by a dielectric technique. SkinRes. Technol. 12 (2006), 235-240.
49. Stuchly, MA, TW Athey, GM Samaras, et al:Measurement of radio frequency permittivityof biological tissues with an open-endedcoaxial line: Part II - Experimental Results.IEEE Trans. Microwave Theory andTechniques 30 (1982), 87-92.
50. Alanen, E, T Lahtinen, J Nuutinen:Measurement of dielectric properties ofsubcutaneous fat with open-ended coaxialsensors. Phys. Med. Biol. 43 (1998), 475-485.
51. Mayrovitz, HN, D Brown-Cross, ZWashington: Skin tissue water and laserDoppler blood flow during a menstrual cycle.Clin. Physiol. Funct. Imaging. 27 (2007), 54-59.
52. Mayrovitz, HN, S Davey, E Shapiro: Localtissue water assessed by tissue dielectricconstant: Anatomical site and depthdependence in women prior to breast cancertreatment-related surgery. Clin. Physiol.Funct. Imaging 28 (2008), 337-342.
53. Mayrovitz, HN, S Davey, E Shapiro:Suitability of single tissue dielectric constantmeasurements to assess local tissue water innormal and lymphedematous skin. Clin.Physiol. Funct. Imaging 29 (2009), 123-127.
54. Ward, LC: Bioelectrical impedance analysis:Proven utility in lymphedema risk assessmentand therapeutic monitoring. Lymphat. Res.Biol. 4 (2006), 51-56.
55. Ward, LC, S Czerniec, SL Kilbreath:Quantitative bioimpedance spectroscopy forthe assessment of lymphoedema. BreastCancer Res. Treatment (2008), 541-547.
56. Mayrovitz, HN, DN Weingrad, S Davey:Local tissue water in at-risk and contralateralforearms of women with and without breastcancer treatment-related lymphedema.Lymphat. Res. Biol. 7 (2009), 153-158.
Harvey N. Mayrovitz, PhDCollege of Medical SciencesNova Southeastern University3200 S. University DriveFt. Lauderdale, Florida 33328Phone: 954-262-1313Fax: 954-262-1802Email: [email protected]
Permission granted for single print for individual use. Reproduction not permitted without permission of Journal LYMPHOLOGY.