Timeline - studentblogs.med.ed.ac.ukstudentblogs.med.ed.ac.uk/.../09/wordversionssc.docx · Web...
Transcript of Timeline - studentblogs.med.ed.ac.ukstudentblogs.med.ed.ac.uk/.../09/wordversionssc.docx · Web...
Modernising the treatment of Heart Failure: can anything “beat” an ACE inhibitor?
Heart failure (HF) is an increasingly common condition with around 900,000 patients in the UK currently diagnosed. Both the incidence and prevalence of HF increase with age, with an average age at diagnosis of 76 years. It is a complex syndrome with many causes and a poor prognosis, with as many as 30-40% of patients surviving less than a year from the time of diagnosis. (1)
There are currently a number of treatments available for HF, both pharmacological and mechanical, with ACE inhibitors (ACE-i) as the first-line treatment. In this research project we will explore the evidence base behind this and whether any current or emerging pharmacotherapies can rival the efficacy of ACE-i in the management of HF.
Aims & Objectives:
1. Introduce and define heart failure.
2. Explore the evidence base supporting the use of ACE-i as first line treatment in patients with heart failure.
3. Determine if there is a class effect or variability in effectiveness among different ACE-i .
4. Compare the evidence for commonly used ACE-i against that of beta-blockers and angiotensin receptor blockers.
5. Compare ACE-i to emerging drug therapy (LCZ696) in heart failure.
HEART FAILUREHeart Failure (HF) is defined as a condition in which cardiac output does not meet the metabolic demands of the body. Changes in cardiac function in HF result in decreased stroke volume and therefore a decrease in cardiac output. (2)
The Frank-Starling mechanism states that force of contraction increases with stretch of myocardial fibres. Therefore increasing preload subsequently increases the stroke volume. However in HF such as dilated cardiomyopathy, increased preload pressures in the ventricles can overstretch the cardiac fibres causing dilated ventricles and lower ejection fraction. (3)
(Figure 1. The Frank-Starling relationship showing the effect of HF on stroke volume and preload)
Reduced cardiac output activates the renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system (SNS), which in normal circumstances would aid cardiac function by increasing afterload and preload. However when ventricular function is impaired this results in a pathophysiological ‘vicious cycle’. (4)
HF is usually classified in terms of left ventricular ejection fraction (LVEF), calculated by dividing stroke volume by end-diastolic volume. (4) The two main types are:
Heart failure with reduced ejection fraction (HFwREF) – also known as systolic dysfunction – usually due to dilated ventricles that are unable to contract properly
Heart failure with preserved ejection fraction (HFwPEF) – also known as diastolic dysfunction – usually associated with impaired relaxation due to stiff ventricles (4)
(Figure 2. Types of heart failure. Image drawn by Joanna Moffatt)
Ejection fraction is an important consideration in HF because it indicates severity (the lower the LVEF the worse the prognosis) and also the majority of evidence for therapeutic intervention in those with HF is based on patients with systolic dysfunction. (4)
There are numerous causes of HF including both structural and functional abnormalities. Coronary artery disease is the most common cause of HFwREF but cardiomyopathy and myocarditis are also known precursors. Interestingly, HFwPEF tends to affect older female patients and has a different aetiology with chronic hypertension and atrial fibrillation most commonly implicated. (4)
Treatments:
Accurate aetiological diagnosis is crucial to guiding management of HF, as treatment of the underlying cause may prevent progression. Key pharmacotherapies recommended by NICE include ACE-i, angiotensin receptor blockers (ARBs), beta-blockers, aldosterone antagonists, vasodilators (eg hydralazine/nitrates) and digoxin. (1) The basis of most of these treatments is interruption of the RAAS and SNS in order to break the vicious cycle of HF. (2)
Mechanical treatments include implantable cardioverter-defibrillators (ICD) and cardiac resynchronisation therapy (CRT) used to maintain normal electrical conduction in the heart, and left ventricular assist devices (LVAD) – mechanical pumps which support cardiac function. (2)
The above therapies are recommended in those with HF according to the following flowchart (based on the ESC guidelines) (4):
(Figure 3. Normal ECG. A normal QRS complex is less than 120ms and represents ventricular contraction. Prolonged QRS duration suggests ventricular dyssynchrony. )
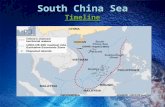
TIMELINEThis timeline displays major trials of treatments of HF since 1985 (6-35).
ACE-I VS ACE-ITable 1. Summary of key comparative trials on ACE-i therapy (8, 31, 7, 10, 30, 32).
ACE inhibitors (ACE-i) are a class of drugs given to HF or hypertension patients, which prevent the formation of the Angiotensin II hormone (Ang-II) from Angiotensin I (Ang-I). Ang-II constricts blood vessels, re-absorbs water in the kidneys, and stimulates Aldosterone secretion which encourages salt and water retention (increasing peripheral resistance and intravascular volume). By inhibiting the formation of Ang-II, blood vessels are relaxed and the intravascular volume is reduced, reducing strain on the heart.
NHS guidelines recommend the ACE-i Enalapril, Lisinopril and Ramipril as first-line treatment. (1) There are other ACE-i including Captopril and Perindopril used in international prescribing practice and clinical trials. Once the efficacy of ACE-i was established, investigations of different agents began to identify a “class effect”. Confirming if all the drugs in this class have similar effects on patients facilitates the use of the most cost effective agent. From a pharmaceutical perspective, identifying any benefits of one particular agent would be lucrative.
A recent meta-analysis conducted in 2014 demonstrated higher efficacy of Perindopril in patients with HF than Enalapril (36), however it is not as frequently prescribed. (37) This new finding has brought the “class effect” theory into question. There are pharmacokinetic and pharmacodynamic differences between the different ACE-i, including anti-inflammatory properties, lipophilicity, tissue-binding and bradykinin-site selectivity, which is especially high for perindopril. (38) The clinical relevance of these qualities is evaluated in clinical trials (Table 1).
ACE-i are categorised according to whether they are long or short-acting. Long-acting agents need less frequent dosing and have prolonged actions with stable cardiac unloading, suggesting greater therapeutic efficacy. Perindopril for example, has a very long duration of action, offering full-24-hour control of blood pressure. (38). Such agents are associated with more, although reversible, adverse effects on renal function than their short-acting counterparts. Study b) was a randomised controlled trial comparing long-acting Lisinopril versus shorter-acting Captopril (in addition to digoxin and diuretics) in a reasonable sample size of 189 patients with moderate-severe congestive HF, over 12 weeks. (7) The primary outcome was change in exercise duration, a poor measure of efficacy with many confounding factors. The study also investigated improvements in LVEF, a major determinant of patient survival in congestive HF and after recovery from myocardial infarction. (39) Lisinopril was associated with a statistically greater increase in exercise duration and also LVEF in patients with <35% function. Adverse experiences were comparable with a higher frequency of elevated blood urea nitrogen in those on Lisinopril (albeit reversible), but more rashes, nausea and dyspnoea with Captopril. The trial did
not specify the pharmacology behind Lisinopril’s superiority for improved LVEF but suggests a class-effect.
Study a) was a retrospective cohort study, therefore the results are less reliable than a randomized controlled trial in terms of blinding and observational bias. (31) It does, however, have the advantage of a large sample size (≥80% power in detecting a meaningful relative risk reduction), reducing the effect of random variability between groups. This study again showed a class effect among ACE inhibitors, with no significant benefit between Enalapril, Lisinopril and Ramipril in the combined endpoint of mortality and CHF readmission or those outcomes alone. The data could have been confounded by compliance, as there was no monitoring of dose administration. The study suggests that prescribing should be based on convenience and cost.
Decreased Ang-II by ACE-i prevents a number of adverse cardiovascular effects. Many studies demonstrated additional cardio-protective benefits in Perindopril compared to other ACE-i, which is a likely consequence of higher bradykinin binding-site selectivity (37):
(37, Table 1 demonstrating beneficial effects of ACE-i)
A 2005 Japanese randomised controlled trial d) displayed significantly improved cardiac sympathetic-nerve activity as well as left-ventricular performance using Perindopril compared to Enalapril, combined with a loop diuretic over a period of 6 months. (30) Outcomes were measured by brain natriuretic peptide levels and radioisotope scintigraphy which are useful prognostic indicators. The small sample (n=40) of patients who were admitted with a first episode of congestive HF and no past history makes it difficult to say whether the same results could be extrapolated to a larger and more diverse population. Medical examinations were assessed blindly, avoiding observer bias, and patients with previous myocardial infarction, dilated cardiomyopathy or valvular disease aetiologies were stratified. The results were consistent with a more recent study e) in 2008, with similar sample size however no stratification for aetiologies. (32) Both trials only investigated initial effects with a short follow up, and long term trials may be needed to evaluate left ventricular remodelling.
Trial c) compared first-dose response to ACE-i in the elderly and concluded that Perindopril confers better blood pressure stability after first dose. (10) Other notable results included similar maximum plasma ACE inhibition (after 8 hours) but both significantly greater inhibition after 24 hours and a small but significant slowing of the heart rate in Enalapril patients. The inclusion criteria of elderly, diuretic-treated, moderate-severe HF patients were chosen because of the higher risk of an adverse hypotensive response, although this limits the application of this study to a wider population. This trial was conducted with a small sample size, although efforts were taken to reduce the random effects of meals and posture on blood pressure. Similarly, White Coat hypertension is a possible confounding factor in this study. Another trial conducted in 2005 recorded a very similar difference in asymptomatic first-dose hypotension in a larger sample size of patients (n=239), as well as one episode of symptomatic hypotension in an Enalapril patient, adding to the consistency of the evidence base (40). The clinical relevance of this difference in blood pressure response is unknown, although it is a valuable starting point in refining the acute safety profile of different ACE-i, especially for those at risk of hypotension.
In conclusion, there is some evidence to show that Perindopril has added benefits in selected groups of patients, particularly the elderly, and this may be related to its pharmacological properties. However, its younger counterpart Ramipril has demonstrated similar tolerability and a reduced mortality in patients with HF. (37) There is compelling evidence for a degree of class effect amongst the commonly prescribed ACE inhibitors, however the safety of all agents cannot be assumed and extrapolated from these trials. On balance, the evidence base is not yet sufficient to justify change in clinical practice, and both cost and tolerability remain the major determinants of prescribing practice. (41)
ACE-I VS BETA BLOCKERTable 3. Summary of key trials comparing ACE-i and beta- blocker therapies (25, 27).
Increased levels of circulating catecholamines reflect increased sympathetic activity, one of the primary responses to fall in cardiac output occurring in chronic HF. (42) Catecholamines act on both alpha and beta adrenoreceptors throughout the body. Notably, the beta-1 adrenoreceptor is heavily present within the myocardium. New classes of highly selective beta adrenoreceptor antagonists, or beta blockers, have helped to minimise off target effects such as bronchospasm. This has enabled their usage within a larger patient population.
The mechanism of action of beta blockers is not fully understood, but it is suggested that they may increase LVEF, reduce myocardial remodeling, improve ventricular filling time and reduce end-systolic volume. (42) The RAAS is potentiated by chronic sympathetic activation leading to retention of water and salt, constriction of blood vessels, and increased ventricular preload and afterload. (43) Beta blockers suppress this increased sympathetic activity, therefore reducing RAAS activation.
European Society of Cardiology guidelines have stated beta blockers should only be introduced if patients remain symptomatic after ACE-i monotherapy at the maximum tolerated dose. (4) This is likely due to the timing of previous studies, as ACE-i were proven beneficial in this population prior to beta blockers. The evidence for beta blocker use is largely based on The Carvedilol and ACE-Inhibitor Remodelling Mild Heart Failure Evaluation Trial (CARMEN 2004) and The Cardiac Insufficiency Bisoprolol Study III (CIBIS-III 2005), which both aimed to challenge this status quo. In the CARMEN trial, Enalapril (ACE-i) monotherapy was compared with Carvedilol (non-selective beta blocker) monotherapy, with a third arm comparing both to combination therapy. This aimed to confirm that Enalapril monotherapy was the most effective first line treatment. The primary endpoint of CARMEN was change in left ventricular end-systolic volume (LVESV) index from baseline, which the study states is a good indicator of prognosis in patients with chronic HF.
The CARMEN study is a randomised, multi-centred double blinded trial, minimising potential bias. It offers novel information as it is the first large-scale direct comparison trial of a beta blocker versus an ACE-i on the effects of LV remodelling in patients with chronic HF. (25) Analysis was carried out twice by two independent, experienced and blinded echocardiographers
using standardised software and methods of analysis, thus reducing interpreter bias and error. Results showed that Enalapril monotherapy does not have any benefit in patients with mild to moderate HF in relation to change in LVESV index. A combination of Enalapril and Carvedilol was favoured, and remodelling was significantly evident after just six months of maintenance treatment. Carvedilol monotherapy provided a greater benefit than Enalapril alone, but was inferior to the combination. LVEF was one of the major secondary endpoints analysed, and both monotherapy with carvedilol and combination therapy significantly increased this. Increased LVEF due to Enalapril monotherapy was only apparent after 18 months.
However, in prior studies, for example SOLVD (1991), Enalapril was shown to have a greater benefit to patients with chronic HF. (8)The results of Enalapril taken from the CARMEN study should be interpreted with caution as two thirds of the patients were receiving ACE-i prior to the trial. Therefore its benefits may have been underestimated. Furthermore, the majority of participants were male and so gender distribution is not accurately represented. The source of funding for the trial was sponsorship from Roche, the manufacturer of Carvedilol. Their influence may have led to bias in the favour of this treatment.
The CIBIS-III study examined the timing of prescription of Enalapril vs Bisoprolol using monotherapy with bisoprolol (initial dose 1.25 mg once daily, target dose 10 mg once daily) or enalapril (initial dose 2.5 mg twice daily, target dose 10 mg twice daily) for 6 months, followed by their combination for up to 24 months. CIBIS-III studied the effect on mortality, morbidity and on attaining the maximum dose. The study was randomised and blinded with a study population older than 65, who correspond to NYHA class II or III and have a LVEF of less than 35%. Exclusion criteria included patients with previous strokes or myocardial infarction, had recently undergone coronary bypass surgery, had a heart rate of less than 60bpm and were not fitted with a pacemaker and all those with obstructive lung disease. This allows standardisation of the patients and the risk of developing an adverse event or requiring hospitalisation. Bisoprolol is a cardio-selective beta blocker and has few respiratory side effects; therefore it may be significant that patients with obstructive lung disease were excluded from the. (27)
Multivariable analysis was used to adjust for the 19 baseline variables. 59.6% reached the combined endpoint during the initial 6-month phase. There was no justification for the six month phase of monotherapy given within the trial, and these results would suggest the duration of monotherapy should be limited in a real world setting. The second conclusion drawn was that the target dose was more likely to be achieved in the drug prescribed first, regardless of which was initially given. The benefits of combination therapy were present regardless of the initial drug used. (44) The study is well designed and aims to reduce bias through blinding and confounding via multivariate analysis. However the small study size of 1010 patients gives rise to the influence of chance. With 68.2% of the study population being male the results may not be representative of all patient groups.
Beta blockers have a significant beneficial effect in the treatment of patients with chronic HF, especially in combination therapy with the ACE-i Enalapril. However, due to some limitations of the above trials the results obtained must be considered with caution, as it appears the full potential of Enalapril action was not realised due to poor patient selection.
There is sufficient evidence to advocate the introduction of combination therapy with an ACE Inhibitor, followed by a beta blocker at the earliest opportunity and at the maximum tolerated dose.
ACE-I VS ARBTable 4. Summary of key trials comparing ACE-i and ARB therapies. (12,16,20,23)
ARBs such as Losartan and Valsartan act by inhibiting the action of Ang-II on the heart, peripheral vasculature and kidney. In HF, they produce beneficial haemodynamic changes that are similar to the effects of ACE-i but are generally better tolerated. (2)
Multiple studies have shown that ACE-i reduce mortality of post-MI patients from HF, but have the tendency to incompletely suppress Ang-II with long-term therapy. ARBs offer an alternative approach to the inhibition of RAAS by blocking the biological effects of Ang-II more completely than ACE-i, therefore, theoretically offering clinical benefits beyond those of ACE-i for the treatment of HF. (45) These trials were therefore conducted to assess whether ARBs are a safe and effective alternative to ACE-i. (20,23)
After looking into several trials including ELITE and ELITE II, we decided to focus on the two biggest trials: OPTIMAAL and VALIANT. Both assessed all-cause mortality and morbidity as their primary outcome, using Captopril as the ACE-i, and Losartan and Valsartan as the ARB respectively. (20,23) Whilst these are robust endpoints to ensure drug safety, they do not study alternative clinical endpoints such as cardiovascular death, or HF specific outcomes such as an increase in LVEF, reduction in left ventricular end systolic volume, or an improvement in symptoms.
As seen in the table, both trials have relatively large sample sizes (20,23) which reduces chance effects and minimises the risk of a Type II error (failure to detect a true difference between treatments, due to an underpowered study). This would also ensure intervention and control groups are well matched at baseline. Both studies analysed results using intention-to-treat analysis (patients are analysed based on their initial group allocation regardless of whether they were allowed to cross over into an alternate treatment arm), giving a true and pragmatic representation of the clinical settings in the real patient population. (20,23)
OPTIMAAL was randomised with a computer generated allocation schedule to reduce selection bias and maintain the integrity of double-blindness. As the interventions differed in appearance and taste, each patient was given two drugs (one active, one placebo) to maintain the concealment of the active drug, thereby reducing performance and detection bias. (20)
VALIANT was also double-blinded and randomised with the use of an automated, interactive voice-response system. The study stated it had to unblind 105 patient details due to informed
consent concerns (23); this may lead to bias. However, it must be noted that VALIANT has a sample size of 14,808, thus 105 may not be significant enough to statistically influence findings.
Most patients in each trial completed the double-blind treatment period. Patients who discontinued were followed up in all studies and were usually included in the clinical outcome or safety analysis of each trial to reduce attrition bias. (20,23)
OPTIMAAL and VALIANT were both funded by drug companies invested in ARBs. Data management assistance was provided by the sponsor in OPTIMAAL (20), however, measures were taken to reduce possible bias. For example, it was explicitly stated that scientific conduct of the study and manuscript preparation were independent of the sponsor. (20) In VALIANT, all pre-specified end points were adjudicated by a clinical end point committee that was unaware of the treatment group assignments, and details of the double-blinding assignments were only accessible to the data and safety monitoring board and an independent drug-distribution group. (22) Bias was further reduced as data processing and site management were processed independently of the sponsor. (22) Whilst an awareness of sponsor influence must be noted, studies funded by pharmaceutical companies do not necessarily lead to biased studies, provided appropriate measures are taken.
OPTIMAAL and VALIANT were both relatively long trials, lasting 48 and 27.4 months respectively. (20,23) Long periods of follow-up help to increase the number of patients reaching the primary outcomes, and they are therefore more likely to find a significant difference in study populations should one exist. To avoid publication bias and to accurately assess the ARB class of drugs, inconclusive studies with unfavourable results should also be published. In line with this, VALIANT and OPTIMAAL showed evidence of ARB non-superiority and still recommend ACE-i as first line treatment. (20,23)
In conclusion, there were no significant differences between ARB and ACE-i in all-cause mortality and morbidity of HF patients in VALIANT and OPTIMAAL. However, ARBs were found to be superior over ACE-i with regards to adverse effects. In conclusion, ACE-i should be used as first-line treatment due to higher costs of ARBs. However, ARBs should be considered if patients are ACE-i intolerant. (20,23) Both the papers are considered to be robust, fairly investigated and accurately reported.
ACE-I VS ARBTable 4. Summary of key trials comparing ACE-i and ARB therapies. (12,16,20,23)
ARBs such as Losartan and Valsartan act by inhibiting the action of Ang-II on the heart, peripheral vasculature and kidney. In HF, they produce beneficial haemodynamic changes that are similar to the effects of ACE-i but are generally better tolerated. (2)
Multiple studies have shown that ACE-i reduce mortality of post-MI patients from HF, but have the tendency to incompletely suppress Ang-II with long-term therapy. ARBs offer an alternative approach to the inhibition of RAAS by blocking the biological effects of Ang-II more completely than ACE-i, therefore, theoretically offering clinical benefits beyond those of ACE-i for the treatment of HF. (45) These trials were therefore conducted to assess whether ARBs are a safe and effective alternative to ACE-i. (20,23)
After looking into several trials including ELITE and ELITE II, we decided to focus on the two biggest trials: OPTIMAAL and VALIANT. Both assessed all-cause mortality and morbidity as their primary outcome, using Captopril as the ACE-i, and Losartan and Valsartan as the ARB respectively. (20,23) Whilst these are robust endpoints to ensure drug safety, they do not study alternative clinical endpoints such as cardiovascular death, or HF specific outcomes such as an increase in LVEF, reduction in left ventricular end systolic volume, or an improvement in symptoms.
As seen in the table, both trials have relatively large sample sizes (20,23) which reduces chance effects and minimises the risk of a Type II error (failure to detect a true difference between treatments, due to an underpowered study). This would also ensure intervention and control groups are well matched at baseline. Both studies analysed results using intention-to-treat analysis (patients are analysed based on their initial group allocation regardless of whether they were allowed to cross over into an alternate treatment arm), giving a true and pragmatic representation of the clinical settings in the real patient population. (20,23)
OPTIMAAL was randomised with a computer generated allocation schedule to reduce selection bias and maintain the integrity of double-blindness. As the interventions differed in appearance and taste, each patient was given two drugs (one active, one placebo) to maintain the concealment of the active drug, thereby reducing performance and detection bias. (20)
VALIANT was also double-blinded and randomised with the use of an automated, interactive voice-response system. The study stated it had to unblind 105 patient details due to informed consent concerns (23); this may lead to bias. However, it must be noted that VALIANT has a sample size of 14,808, thus 105 may not be significant enough to statistically influence findings.
Most patients in each trial completed the double-blind treatment period. Patients who discontinued were followed up in all studies and were usually included in the clinical outcome or safety analysis of each trial to reduce attrition bias. (20,23)
OPTIMAAL and VALIANT were both funded by drug companies invested in ARBs. Data management assistance was provided by the sponsor in OPTIMAAL (20), however, measures were taken to reduce possible bias. For example, it was explicitly stated that scientific conduct of the study and manuscript preparation were independent of the sponsor. (20) In VALIANT, all pre-specified end points were adjudicated by a clinical end point committee that was unaware of the treatment group assignments, and details of the double-blinding assignments were only accessible to the data and safety monitoring board and an independent drug-distribution group. (22) Bias was further reduced as data processing and site management were processed
independently of the sponsor. (22) Whilst an awareness of sponsor influence must be noted, studies funded by pharmaceutical companies do not necessarily lead to biased studies, provided appropriate measures are taken.
OPTIMAAL and VALIANT were both relatively long trials, lasting 48 and 27.4 months respectively. (20,23) Long periods of follow-up help to increase the number of patients reaching the primary outcomes, and they are therefore more likely to find a significant difference in study populations should one exist. To avoid publication bias and to accurately assess the ARB class of drugs, inconclusive studies with unfavourable results should also be published. In line with this, VALIANT and OPTIMAAL showed evidence of ARB non-superiority and still recommend ACE-i as first line treatment. (20,23)
In conclusion, there were no significant differences between ARB and ACE-i in all-cause mortality and morbidity of HF patients in VALIANT and OPTIMAAL. However, ARBs were found to be superior over ACE-i with regards to adverse effects. In conclusion, ACE-i should be used as first-line treatment due to higher costs of ARBs. However, ARBs should be considered if patients are ACE-i intolerant. (20,23) Both the papers are considered to be robust, fairly investigated and accurately reported.
CONCLUSIONOur aim was to explore whether ACE-i are the most effective first-line treatment in patients with chronic HF. We looked at studies comparing ACE-i with beta blockers, with ARBs and with each other.
There are no studies which show significant variation in outcomes in patients using different types of ACE-i. This is an interesting finding, as it is known ACE-i vary widely in their pharmacokinetics and pharmacodynamics. However, in already hypotensive patients, perindropril was the safest.
In studies comparing ACE-i with beta blockers, both drugs were shown to be more effective when administered in combination. When used in monotherapy, one had no advantage over the other. Therefore, it was stated that beta blockers should be given in combination with ACE-i as soon as possible.
Studies comparing ACE-i and ARBs showed there were no significant differences in patient outcomes between the two classes of drugs. However, ARBs were found to have fewer adverse effects than ACE-i. It was concluded that ACE-i should be used as first-line treatment due to the higher costs of ARBs, but ARBs should be considered if patients are intolerant to ACE-is.
A trial on a new drug LCZ696 was recently published. It was considered to be a robust paper, with results indicating that LCZ696 showed superiority over ACE-i. However, as this is a
pioneer trial, it is important to ensure these results are accurate and repeatable in a larger patient population. Furthermore, long-term effects of the drug will not be recognised for some time.
Despite these papers having many strengths and providing evidence on which our practice can be changed, they did have weaknesses that cannot be ignored. Most papers used all-cause mortality as an endpoint, when a cardiac-related mortality may have been more relevant. Whilst this is important from the standpoint of overall drug safety and will help to identify ‘off target’ side effects, this has the potential to distract clinicians from more cardiovascular specific endpoints. Given that more women than men are affected by cardiovascular disease, it is clear that some studies were not using a representative sample of the patient population as majority of the subjects were male.
Furthermore, some of the trials were sponsored by manufacturers of the drugs involved. A certain level of bias may be present in the trials, particularly in those when the drug company was directly involved in data administration. However, whilst in an ideal world the pharmaceutical industry would have a very limited role in conducting such trials, it is important to recognise that without their funding, examining new treatments on such large scale would not be feasible due to economic constraints.
After thorough analysis of the papers mentioned, we conclude that ACE-i should remain as the first line treatment for chronic HF. However this could change in the future if further research on the new drug LCZ696 shows promising results. We believe future randomised controlled trials of LCZ696 should compare this treatment with the gold standard ACE-i, Ramipril, at its optimal dose of 10mg per day. This would combat many of the criticisms of this otherwise well conducted trial.
Throughout the course of this project, we as a group have developed and gained many skills. Teamwork was pivotal throughout, and we worked well to ensure that allocated tasks were completed efficiently and to a high standard. At the start of the project, the prospect of critically appraising academic papers was daunting to us all, but we have since developed and refined this skill. We have learnt that it is important not to take everything we read at face value. As medical students, it is essential to retain and develop these skills in our future clinical practice.
REFERENCES1. National Institute for Health and Care Excellence. Chronic Heart Failure: Management of
Chronic Heart Failure in Adults in Primary and Secondary Care. CG108. London: National Institute for Health and Care Excellence; 2010. http://www.nice.org.uk/guidance/cg108/resources/cg108-chronic-heart-failure-full-guideline3 (Website)
2. Newby DE, Grubb NR, Bradbury A. Cardiovascular Disease. In: Walker BR, Colledge NR, Ralston SH, & Penman ID, . Davidson’s principles and practice of medicine. 22nd ed. Edinburgh: Churchill Livingstone/Elsevier; 2014. p 546-553 (Textbook)
3. Kobirumaki-Shimozawa F, Inoue T, Shintani SA, Oyama K, Terui T, Minamisawa S, Ishiwata S, Fukuda N. Cardiac thin filament regulation and the Frank–Starling mechanism. J Physiol Sci. 2014; 64(4):221-232 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4070490/ (Review Article)
4. McMurray JJV, Adamopoulos S, Anker SD, et al. The European Society of Cardiology Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. The European Heart Journal. 2012; 33: 1787-1847 http://www.escardio.org/guidelines-surveys/esc-guidelines/guidelinesdocuments/guidelines-acute%20and%20chronic-hf-ft.pdf (Website)
5. Cohn JN,Archibald DG, Ziesche S, et al. Effect of Vasodilator Therapy on Mortality in Chronic Congestive Heart Failure. New England Journal of Medicine. 1986; 314(24):1547-52. http://www.nejm.org/doi/full/10.1056/NEJM198606123142404 (Primary Research Article)
6. Idänpään-Heikkilä U, Remes J, Hirvonen T, et al. Effects of Enalapril on Mortality in Severe Congestive Heart Failure. New England Journal of Medicine. 1987; 316:1429-1435. http://www.nejm.org/doi/full/10.1056/NEJM198706043162301 (Primary Research Article)
7. Giles TD, Katz R, Sullivan JM, Wolfson P, Haugland M, Kirlin P, Powers E, Rich S, Hackshaw B, Chiaramida A, et al. Short- and long-acting angiotensin-converting enzyme inhibitors: a randomized trial of lisinopril versus captopril in the treatment of congestive heart failure. The Multicenter Lisinopril-Captopril Congestive Heart Failure Study Group. J Am Coll Cardiol. 1989; 13(6):1240-7. http://www.ncbi.nlm.nih.gov/pubmed/2539403 (Primary Research Article)
8. Nicklas JM, Pitt B, Timmis G, et al. Effect of Enalapril on Survival in Patients with Reduced Left Ventricular Ejection Fractions and Congestive Heart Failure. New England Journal of Medicine. 1991; 325(5):293-302. http://www.nejm.org/doi/full/10.1056/NEJM199108013250501 (Primary Research Article)
9. Cohn JN, Johnson G, Ziesche S, et al. A Comparison of Enalapril with Hydralazine–Isosorbide Dinitrate in the Treatment of Chronic Congestive Heart Failure. New England Journal of Medicine. 1991; 325(5):303-310 http://www.nejm.org/doi/full/10.1056/NEJM199108013250502 (Primary Research Article)
10. MacFadyen R, Lees K, Reid J, et al. Differences in first dose response to angiotensin converting enzyme inhibition in congestive heart failure: a placebo controlled study. Heart. 1991; 66(3):206-211. http://heart.bmj.com/content/66/3/206.long (Primary Research Article)
11. Nicklas JM, Pitt B, Timmis G, et al. Effect of Enalapril on Mortality and the Development of Heart Failure in Asymptomatic Patients with Reduced Left Ventricular Ejection Fractions. New England Journal of Medicine. 1992; 327(10):685-691 http://www.nejm.org/doi/full/10.1056/NEJM199209033271003 (Primary Research Article)
12. Pitt B, Segal R, Martinez F, Meurers G, Cowley A, Thomas I et al. Randomised trial of losartan versus captopril in patients over 65 with heart failure (Evaluation of Losartan in the Elderly Study, ELITE). The Lancet. 1997; 349(9054):747-752. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(97)01187-2/fulltext (Primary Research Article)
13. Perry G, Brown E, Thornton R, et al. The Effect of Digoxin on Mortality and Morbidity in Patients with Heart Failure. New England Journal of Medicine. 1997; 336(8):525-533 http://www.nejm.org/doi/full/10.1056/NEJM199702203360801 (Primary Research Article)
14. Pitt B, Zannad F, Remme WJ, et al. The Effect of Spironolactone on Morbidity and Mortality in Patients with Severe Heart Failure. New England Journal of Medicine. 1999; 341(10):709-717. http://www.nejm.org/doi/full/10.1056/NEJM199909023411001 (Primary Research Article)
15. Hjalmarson Å, Goldstein S, Fagerberg B, et al. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in-Congestive Heart Failure (MERIT-HF). The Lancet. 1999;353(9169):2001-2007. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(99)04440-2/fulltext (Primary Research Article)
16. Pitt B, Poole-Wilson P, Segal R, Martinez F, Dickstein K, Camm A et al. Effect of losartan compared with captopril on mortality in patients with symptomatic heart failure: randomised trial—the Losartan Heart Failure Survival Study ELITE II. The Lancet. 2000; 355(9215):1582-1587. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(00)02213-3/fulltext (Primary Research Article)
17. Packer, M., Coats, A. J., Fowler, M. B, et al. Effect of Carvedilol on Survival in Severe Chronic Heart Failure. New England Journal of Medicine. 2001; 344(22): 1651-1658. http://www.nejm.org/doi/full/10.1056/NEJM200105313442201 (Primary Research Article)
18. Cohn JN, Tognoni G. A Randomized Trial of the Angiotensin-Receptor Blocker Valsartan in Chronic Heart Failure. New England Journal of Medicine. 2001; 345(23): 1667-1675. http://www.nejm.org/doi/full/10.1056/NEJMoa010713 (Primary Research Article)
19. Rose EA, Gelijns AC, Moskowitz AJ, et al. Long-Term Use of a Left Ventricular Assist Device for End-Stage Heart Failure. New England Journal of Medicine. 2001; 345(20): 1435-1443. http://www.nejm.org/doi/full/10.1056/NEJMoa012175 (Primary Research Article)
20. Dickstein K and Kjekshus J. Effects of losartan and captopril on mortality and morbidity in high-risk patients after acute myocardial infarction: the OPTIMAAL randomised trial. The Lancet. 2002; 360(9335):752-760. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(02)09895-1/fulltext (Primary Research Article)
21. McMurray JJ, Packer M, Desai AS, et al. Prophylactic Implantation of a Defibrillator in Patients with Myocardial Infarction and Reduced Ejection Fraction. New England Journal of Medicine. 2002; 346(12): 877-883. http://www.nejm.org/doi/full/10.1056/NEJMoa013474 (Primary Research Article)
22. Poole-Wilson P, Swedberg K, Cleland J, Di Lenarda A, Hanrath P, Komajda M et al. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. The Lancet. 2003; 362(9377):7-13. http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(03)13800-7/fulltext (Primary Research Article)
23. Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, Captopril, or Both in Myocardial Infarction Complicated by Heart Failure, Left Ventricular Dysfunction, or Both. New England Journal of Medicine. 2003; 349(20):1893-1906. http://www.nejm.org/doi/full/10.1056/NEJMoa032292 (Primary Research Article)
24. Pitt B, Remme W, Zannad F, et al. Eplerenone, a Selective Aldosterone Blocker, in Patients with Left Ventricular Dysfunction after Myocardial Infarction. New England Journal of Medicine. 2003; 348(14): 1309-1321. http://www.nejm.org/doi/full/10.1056/NEJMoa030207 (Primary Research Article)
25. Remme W, Riegger G, Hildebrandt P, Komajda M, Jaarsma W, Bobbio M et al. The Benefits of Early Combination Treatment of Carvedilol and an ACE-Inhibitor in Mild Heart Failure and Left Ventricular Systolic Dysfunction. The Carvedilol and ACE-Inhibitor Remodelling Mild Heart Failure Evaluation Trial (CARMEN). Cardiovascular Drugs and Therapy. 2004; 18(1):57-66. http://link.springer.com/article/10.1023%2FB%3ACARD.0000025756.32499.6f (Primary Research Article)
26. Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-Resynchronization Therapy with or without an Implantable Defibrillator in Advanced Chronic Heart Failure. New England Journal of Medicine. 2004; 350(21): 2140-2150. http://www.nejm.org/doi/full/10.1056/NEJMoa032423 (Primary Research Article)
27. Willenheimer R, van Veldhuisen DJ, Silke B, et al. Effect on Survival and Hospitalization of Initiating Treatment for Chronic Heart Failure With Bisoprolol Followed by Enalapril, as Compared With the Opposite Sequence: Results of the Randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation. 2005; 112(16):2426-2435. http://circ.ahajournals.org/content/112/16/2426.full (Primary Research Article)
28. Cleland JGF, Daubert JC, Erdmann E, et al. The Effect of Cardiac Resynchronization on Morbidity and Mortality in Heart Failure. New England Journal of Medicine. 2005; 352(15): 1539-1549. http://www.nejm.org/doi/full/10.1056/NEJMoa050496 (Primary Research Article)
29. Bardy GH, Lee K, Mark DB, et al. Amiodarone or an Implantable Cardioverter–Defibrillator for Congestive Heart Failure. New England Journal of Medicine. 2005; 352(3): 225-237. http://www.nejm.org/doi/full/10.1056/NEJMoa043399 (Primary Research Article)
30. Kasama S, Toyama T, Kumakura H, Takayama Y, Ichikawa S, Suzuki T, et al. Effects of perindopril on cardiac sympathetic nerve activity in patients with congestive heart failure: comparison with enalapril. European Journal of Nuclear Medicine and Molecular Imaging. 2005; 32(8):964-971. http://link.springer.com/article/10.1007/s00259-005-1786-z?no-access=true (Primary Research Article)
31. Tu K, Mamdani M, Kopp A, Lee D, et al. Comparison of angiotensin-converting enzyme inhibitors in the treatment of congestive heart failure. The American Journal of Cardiology. 2005; 95(2):283-286. http://www.sciencedirect.com/science/article/pii/S0002914904015437 (Primary Research Article)
32. Tsutamoto T, Tanaka T, Sakai H, Nishiyama K, Fujii M, Yamamoto T, et al. Beneficial Effect of Perindopril on Cardiac Sympathetic Nerve Activity and Brain Natriuretic Peptide in Patients With Chronic Heart Failure. Circulation Journal: official journal of the Japanese Circulation Society. 2008; 72(5):740-746. https://www.jstage.jst.go.jp/article/circj/72/5/72_5_740/_pdf (Primary Research Article)
33. Moss AJ, Hall WJ, Cannom DS, et al. Cardiac-Resynchronization Therapy for the Prevention of Heart-Failure Events. New England Journal of Medicine. 2009; 361(14): 1329-1338. http://www.nejm.org/doi/full/10.1056/NEJMoa0906431 (Primary Research Article)
34. Tang AS, Wells GA, Talajic M, et al. Cardiac-Resynchronization Therapy for Mild-to-Moderate Heart Failure. New England Journal of Medicine. 2010; 363(25): 2385-2395. http://www.nejm.org/doi/full/10.1056/NEJMoa1009540 (Primary Research Article)
35. McMurray JJ, Packer M, Desai AS, et al. Angiotensin–Neprilysin Inhibition versus Enalapril in Heart Failure. New England Journal of Medicine. 2014; 371(11): 993-1004. http://www.nejm.org/doi/full/10.1056/NEJMoa1409077 (Primary Research Article)
36. DiNicolantonio JJ, Hu T, Lavie CJ, O’Keefe JH, Bangalore S, et al. Perindopril vs Enalapril in Patients with Systolic Heart Failure: Systematic Review and Metaanalysis. The Ochsner Journal. 2014; 14(3): 350-358. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4171793/(Review Article)
37. Dinicolantonio JJ, Lavie CJ, O’Keefe JH, et al. Not all angiotensin-converting enzyme inhibitors are equal: focus on ramipril and perindopril. Postgraduate Medical Journal. 2013; 125(4):154-68. http://www.ncbi.nlm.nih.gov/pubmed/23933903(Comparative review article)
38. Straka RJ. Comparison of approved ACE inhibitors. ©2000. [cited 2014-11-21] Available from:http://www.courses.ahc.umn.edu/pharmacy/5822/Lectures/ACE-IChart12.12.00.pdf (Website)
39. White HD, Norris RM, Brown MA, Brandt PW, Whitlock RM, Wild CJ et al. Left ventricular end-systolic volume as the major determinant of survival after recovery from myocardial infarction. Circulation. 1987; 76:44-51. http://circ.ahajournals.org/content/76/1/44.full.pdf(Primary Research Article)
40. Vítovec J and Spinar J. First-dose hypotension after angiotensin-converting enzyme (ACE) inhibitors in chronic heart failure: a comparison of enalapril and perindopril. European Journal of Heart Failure. 2000 September; 2(3):299-304. http://onlinelibrary.wiley.com/doi/10.1016/S1388-9842(00)00095-7/full(Primary Research Article)
41. Brown MJ. A Rational Basis for Selection Among Drugs of the Same Class. Heart Journal. 2003; 89(6): 687-694. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1767704/ (Review Article)
42. Silke B. Beta-blockade in CHF: pathophysiological considerations. European Heart Journal Supplements. 2006; 8(Suppl C):C13-C18. http://eurheartjsupp.oxfordjournals.org/content/8/suppl_C/C13 (Comparative Review Article)
43. Sackner-Bernstein JD, Mancini DM. Rationale for treatment of patients with chronic heart failure with adrenergic blockade.JAMA. 1995; 274: 1462–1467 http://www.ncbi.nlm.nih.gov/pubmed/7474194 (Comparative Review Article)
44. Funck-Brentano C, van Veldhuisen DJ, van de Ven LL, Follath F, Goulder M, Willenheimer R. Influence of order and type of drug (bisoprolol vs. enalapril) on outcome and adverse events in patients with chronic heart failure: a post hoc analysis of the CIBIS-III trial. Eur J Heart Fail. 2011;13: 765–772. http://www.ncbi.nlm.nih.gov/pubmed/21551161 (Review Article)
45. Bissessor N and White H. Valsartan in the treatment of heart failure or left ventricular dysfunction after myocardial infarction. Vasc Health Risk Manag. 2007; 3(4): 425-430. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2291334/ (Primary Research Article)
46. Kostis JB, Packer M, Black HR, et al. Omapatrilat and enalapril in patients with hypertension: the Omapatrilat Cardiovascular Treatment vs. Enalapril (OCTAVE) trial. American Journal of Hypertension. 2004; 17(2):103-11. http://ajh.oxfordjournals.org/content/17/2/103 (Primary Research Article)
47. Marr RA, Guan H, Rockenstein E, et at. Neprilysin regulates amyloid Beta peptide levels. Journal of Molecular Neuroscience. 2004; 22(1-2):5-11. http://link.springer.com/article/10.1385/JMN:22:1-2:5 (Research Support Article)
CONTRIBUTIONS
All members did at least 1 weekly diary and critically appraised the hydralazine paper for the group critical appraisal.
Susannah Houston: She critically appraised a beta-blocker paper, did a mini critical appraisal presentation on CARMEN, wrote the ACEi vs beta-blocker page with Manveer and wrote the conclusion page with Chin.
Nazia Zahed: She critically appraised an ACEi paper and wrote the ACEi vs ACEi page with Alex. She did her presentation on LCZ696 and wrote the LCZ696 vs ACEi page with Abs.
Joanna Moffatt: She critically appraised a aldosterone antagonist paper, did her presentation on CIBIS, wrote the introduction/background pages, consolidated the tables in each section and drew images of the heart.
Elizabeth Page (Alex): She critically appraised a hydralazine paper, wrote the ACEi vs ACEi page with Nazia, presented the hydralazine paper and wrote the group critical appraisal on that same paper.
Abhijit Bajracharya (Abs): He critically appraised cardiac resynchronisation therapy and implantable cardioverter defibrillator papers, drew the timeline on excel, did his presentation on SOLVD and wrote the LCZ696 page with Nazia. He also referenced the timeline.
Faustina Davis: She filled in and submitted the ethics form on behalf of the group, critically appraised a digoxin paper, did her presentation on VALIANT, wrote up the ACEi vs ARB with Chin and wrote up the information search report.
Manveer Rahi: He critically appraised a left ventricular assist device paper, did his presentation on REMATCH, wrote the beta blockers vs ACEi page with Susannah, input the timeline into a prezi format and wrote the pathophysiology of HF in the background section.
Chin Yoxin: She critically appraised a ARB paper, did her presentation on OPTIMAAL, wrote the ACEi vs ARB page with Faustina, wrote the conclusion page with Susannah and wrote up the contribution page.
CRITICAL APPRAISALGroup Critical Appraisal
Aim:
To compare the efficacy of two vasodilators, enalapril and hydralazine/isosorbide-dinitrate in heart-failure patients also receiving digoxin and diuretic therapy (9)
Study design:
Randomized, double-blinded, multicentre clinical trial Parallel treatment groups – Hydralazine 300mg/ISDN 160mg daily Enalapril 20mg daily No placebo group due to ethical limitations of non-treatment
Study sample:
Population: n = 804 (Hydralazine/ISDN: n=401, Enalapril: n=403) Men aged 18-75 with chronic heart failure (defined as cardiothoracic ratio ≥0.55 on
radiography, diastolic LV internal diameter >2.7 cm per m2 of BSA on echocardiography, or EF < 0.45 by radionuclide scan, plus reduced exercise tolerance)
Excluded patients with MI or cardiac surgery within past 3 months, angina requiring therapy or limiting exercise, serious obstructive valvular disease, obstructive lung disease, other diseases likely to limit survival
Patient’s baseline characteristics between the groups appear similar although no P-values are provided. Potential confounders include duration of CHF and presence of hypertension AF, which are not well-matched
Statistical tests:
Significance level set at p=0.042 according to interim analyses Effect sizes expressed as relative reduction in mortality and relative risk ratios (and 95%
confidence-intervals) determined from life-table regression model Changes over time analysed at follow-up and mean changes from baseline in the two groups
compared with a t-test
Results:
Primary-outcome: mortality (cause of death was recorded) Secondary-outcomes: exercise testing with gas-exchange measurements, cardiothoracic ratio,
ejection-fraction, and plasma norepinephrine levels Mortality after 2 years significantly lower in enalapril group (P=0.016), due to reduction in
incidence of sudden-death (P=0.015) and premonitory worsening (P=0.032), but didn’t attain statistical significance for the rest of follow-up, overall (P=0.08) or for other types of cardiac death including pump-failure Cardiac deaths: Hydralazine/ISDN 137/401, Enalapril 112/403 All-cause death: Hydralazine/ISDN 153/401, Enalapril 132/403
Systolic BP reduction significantly better with enalapril after 13 weeks (no P-value given). O2-
consumption at peak exercise significantly higher in the hydralazine/ISDN group after 2 years (P=0.02). LVEF increased in both but faster in hydralazine/ISDN (significantly higher at 13 weeks, P=0.026). No significant difference was found for CT ratios and hospitalization rates
Bias:
Wide range of ejection-fractions (0.06-0.68) and ages (18-75) may confound results due to differing aetiologies of heart-failure and likelihood of survival
Selection bias: sample of heart-failure patients was unrepresentative as exclusion of vital groups like those above 75 years-old, women (~50% of patients, causing gender bias), suffering IHD, other common comorbidities and “diseases likely to limit survival” (a very vague criteria)
Small sample size may lead to chance findings, no power-calculation conducted to ensure the study had sufficient statistical power
Common presenting side-effects (e.g. cough for enalapril) could have impacted feasibility of blinding, producing researcher-bias
Non-compliance can make effectiveness of the treatment difficult to assess , P-value not given for the difference in adherence between the two treatment groups
Comments:
Appropriate design for addressing objectives, also attempted to replicate the clinical picture, like the intention-to-treat method. Classifying deaths according to cause was also important to properly address the aims
Mortality outcome for hydralazine/ISDN was consistent with VHEFT-i trial (5) Endpoints measured used reliable tools and appropriately addressed the aim. Methods were
well described (especially diagnostic criteria) and reproducible, however repeated checks during follow-up were not mentioned, reducing reliability of these measurements
P-values weren’t provided for all results, may have been useful in extrapolating data, and results of quality-of-life measured in a questionnaire were never presented
Conclusion:
Useful study on the long-term efficacy of hydralazine/ISDN and divergent effects of two vasodilators on different therapeutic endpoints. Also useful at the time for testing the new ACE-inhibitor class in NHYA mild-moderate patients. There are some flaws, in particular excluding important target populations reduces validity when extrapolating to the wider population
INFORMATION SEARCH REPORTResearch was needed to fill the gaps in our knowledge of HF and treatments. Textbooks, located using library services, were used to develop our knowledge of HF pathophysiology, while online databases and Google searches were utilized for scoping treatments. Using Medline, the PARADIGM timeline article found provided a good summary of the different HF treatments available to date. Having working knowledge of the treatments enabled us to shortlist 8 treatments to explore their evidence base further. Through a broad Google search we also came across a new drug for HF – LCZ696.
We included systematic reviews from various search modalities such as the Cochrane library and Google for background research. However, the project mainly utilised primary research papers, some of which were supplied by our tutor.
Focused searches for relevant clinical trials of the selected therapies were also done on databases such as Medline and Pubmed. Basic exclusion criterias included small sample sized, unblinded, and non-randomised studies. NICE guidelines for HF also aided focus of the research. Boolean functions such as ‘AND’, and limits such as ‘date published’ and ‘type of study’, in this case, ‘Randomised control trials’ were also used to narrow down the search and ensure that returned papers contained information that was relevant and up to date.
After deciding on papers to review, we used the ‘findit@edinburgh’ button to access the full text where possible. Some literatures were not available within the university subscription, which we overcame by working on library grounds and by asking for assistance from our tutor. ACE-i have a vast amount of research, mostly irrelevant, therefore the search was narrowed down using names of the specific ACE-i (eg. Enalapril) recommended for HF.
Week 1
This week we had our first meeting with our tutor, where we discussed our current knowledge surrounding heart failure and how it is treated. We concluded that we should do more research into treatment before deciding a direction or focus for our project. We also determined where were good places to look for information, how we could contact each other and what needed to be done before the next meeting: Manveer volunteered to set up a DropBox folder for our preliminary research, Faustina volunteered to fill out the Ethics form, and Alex will set up the initial website. We also set up a time for our next meeting.
Week 2
This week’s session was spent discussing what possible paths our project could take based on the research we did after our last meeting. We also drafted out an outline of points we wanted to include in our project Background (definition of heart failure, epidemiology and a timeline of treatments/management). At the end of the session we decided to focus on these 8 heart failure treatments:
Ace inhibitors – NaziaBeta blockers – SusannahAngiotensin receptor blockers – ChinAldosterone receptor antagonists – JoannaHydralazine – AlexDigoxin – Faustina
ICT and CRT-D – AbsVentricular assist devices – Manveer
Each member of the group was assigned to do further research into scientific papers (either meta-analysis or randomised, controlled trials) regarding their specific drug/treatment, to feedback to the group next week.
Week 3
This week, we had a group meeting without our tutor. We presented our individual findings for specific treatments from the trails we looked at during the week. Each member mentioned the pros and cons of possible problems/benefits of critically appraising those trials. We concluded that our project will be focusing on the pharmacological side of the treatment rather than the mechanical alternatives because of various flaws in the trials, for example the patients switching to mechanical treatment when the trials were comparing devices and drugs. Out of the various pharmacological treatments, some trials only focused on a certain population (e.g. Hydralazine with African American population) whereas drugs like ACE inhibitors are already a first line treatment, meaning that there must be strong evidence for it, making it difficult for us to critically appraise those trials. We came to a conclusion that we would focus our project on the new drug LCZ 696 as the trials are very recent and there are lots of trials with different levels of hierarchy. We also decided to post a paragraph on our group discussion page with our findings and references to the trial with a general conclusion of the various studies we looked at. This would make it easier for us to add the information on our project in a later stage.
Week 4
This week, we had a group meeting with our tutor. We briefly went through what we did last week and obtained feedback from our tutor. After discussing our options, we decided to focus our project on angiotensin converting enzyme inhibitors (ACEi), investigate a few types of ACEi and compare it with other types of drug therapy such as angiotensin receptor blockers (ARBs), beta-blockers and diuretics. We drafted out aims and objectives for our project, which still requires editing to make it more precise and clear:
1. Introduce and define heart failure. 2. An overview/timeline of current heart failure treatments. 3. Explore the evidence base supporting the use of ace inhibitors. 4. Investigate 2-3 (named) ace inhibitors. 5. Compare ace inhibitors to emerging drug therapy in heart failure.
We also set a deadline, 21/10/14, for ourselves to ensure that the progress of our project is on track.
Joanna: Rough draft on the introduction Abs: Timeline of management of heart failure Nazia and Alex: Compare different ACEi Susannah and Manveer: Compare beta-blockers with ACEi Chin and Faustina: Compare ARBs with ACEi
Two things were to be kept in mind whilst carrying out our individual tasks. Where possible, we should use enalapril, lisinopril, ramipril and perindropril as examples of ACEi. We should also keep note of the keywords and methods used to search for information, which would be used to write up the information search report next week.
Things to do next week:
Compare aldosterone and ACEi Compare diuretics and ACEi Compare LCZ696 and ACEi Write up the information search report
Week 5
Having decided to look at the evidence base comparing different ACE inhibitors, ACE inhibitors with ARBs and ACE inhibitors with beta blockers, we met with our tutor to discuss our progress with this. As well as comparing the different drug therapies we realised that it will be important to consider synergy between them. As we are covering quite a lot of information we decided the most succinct way to present each comparison would be using tables to demonstrate the key features of each trial followed by the critical appraisal. We met up later in the week without our tutor to work on this. We also decided which of us will present a critical appraisal of a trial informally to the group at our next meeting – Chin, Nazia, Alex and Joanna.
Week 6
For this week and next week we were to prepare and deliver a short presentation to the rest of the group in the format of a critical appraisal, of a paper relevant to our project. Nazia, Chin, Alex and Joanna gave presentations this meeting on LCZ69, OPTIMAAL, VHEFT 2 and CIBIS III trials respectively.
After the presentations we decided the LCZ696 trial published in the New England Journal was, as a well-conducted modern study, possibly too difficult to appraise for the group critical appraisal featuring on the website. We considered appraising the Hydralazine trial presented by Alex which was a more balanced study in terms of strengths and weaknesses.
For next week, Faustina, Susannah, Manveer and Abhijit were to present appraisals on their own papers. We also planned to start thinking about the website, deciding that in each pair we would compile a page on the ACE-inhibitor versus different therapies and trials. We were to think about what studies we wanted to include on our pages.
Week 7
Faustina, Susannah, Manveer and Abhijit delivered their presentations, critically appraising VALIANT, CARMEN, REMATCH and SOLVD trials respectively.
We scheduled a separate group meeting without our tutor before next week on Wednesday (05/11/14), in the group-study space of Hugh Robson Building where we would:
* Revise the project aims and objectives and add more depth.
* Start on the Wiki website. Everyone was to bring notes on relevant papers that we have critically appraised page on the ACE-inhibitor versus different therapies, aiming to write up as much as possible within the session and before next week’s formal meeting.
* In the meeting we began compiling our pages in pairs, deciding the rough format as
1) What the drugs we looked at did, with reference to physiology and mechanism of action
2) Picking the main studies and discussing why they were conducted, comparing the study methodology and results; commenting on results, bias, chance and confounding.
3) Providing a conclusion.
Before next week everyone in the group was to read through the hydralazine paper so that the group appraisal of the paper can be discussed next meeting and started.
Week 8
We met with our tutor to discuss our progress over the week; we had been working in pairs to construct the text for under the tables in each page of our website (ACE-I vs ACE-I, ACE-I vs
beta blockers and ACE-I vs ARBs). We agreed to email our drafts to our tutor for feedback over the next week.
As last week we decided to do our group critical appraisal on the hydralazine trial, this week we set a deadline of Friday to each think of as many strengths/weaknesses as we could, along with
any elements of bias, confounding and chance. These will be sent to Alex who will then construct the group critical appraisal.
Other roles assigned this week:
Conclusion: Susannah and Chin New drug (LCZ 969): Nazia and Abhijit Information search report: Faustina Wiki weekly diary: Susannah Group critical appraisal: Alex Pathophysiology of heart failure: Joanna (diagrams, eg. echo of normal vs. damaged heart)
and Manveer (text) Prezi: Manveer Timeline references: Abhijit
We also discussed which trials we had eliminated in our project and why. Our exclusion criteria was: small sample size, unblinded, non-randomised and non-pharmacological trials. We then decided to make two separate website pages for the introduction and background. It was decided that the introduction page would include the title and objectives, and that the background page would include what ACE inhibitors are, the pathophysiology and epidemiology of heart failure and a flowchart of the treatments used.
Week 9
This week we didn’t have the opportunity to meet with our tutor, however we all decided to meet and combine our contributions to the website. Chin was tasked with created a contributions page for the website. The group met again mid-week and here it was decided on how to standardise
and format the website. This was done by changing some abbreviations such as ACE-inhibitor to ACE-I across all pages. The referencing for each page was collated by Abhijit and added to the
website.