The TIMI Trials
Transcript of The TIMI Trials
-
DOCUMENT SIZE: 17.3125 x 11 4C PROCESS (SPINE 0.3125)
TIMI Study Group
10th Edition
YEARS301984 2014
The TIMI Trials
Office Level 1 | 350 Longwood Avenue | Boston, MA 02115 | T: 617.278.0145 | F: 617.734.7329 | www.timi.org
TH
E TIM
I TR
IALS 19
84
- 2014
Office Level 1 | 350 Longwood Avenue | Boston, MA 02115 | T: 617.278.0145 | F: 617.734.7329 | www.timi.org
904040_Cover.indd 1 11/7/14 11:37 AM
-
DOCUMENT SIZE: 17.3125 x 11 4C PROCESS (SPINE 0.3125)
Marc S. Sabatine, MD, MPH is the Chairman of the TIMI Study Group, a Senior Cardiologist at Brigham and Womens Hospital,
Professor of Medicine at Harvard Medical School. He has led multiple large-scale, international, randomized controlled trials of novel cardiovascular pharmacotherapies. Dr. Sabatine has also pioneered multimarker approaches to risk stratification and has several NIH grants supporting the application of proteomics and metabolomics for discovery of novel biomarkers. He has a long-standing interest in pharmacogenetics and has led key studies on the impact of genetic polymorphisms on the pharmacologic and clinical response to antiplatelet therapy. Dr. Sabatine has published extensively in these fields with seminal papers in the New England Journal of Medicine, JAMA, and the Lancet. He has mentored numerous fellows who have gone on to faculty
appointments as physician-scientists at major academic cardiovascular divisions.
Eugene Braunwald, M.D., the founding chairman of the TIMI Study Group, is a preeminent researcher, physician, and educator, and has truly improved health care for people around the world. According to Joseph B. Martin, M.D., former Dean of the Faculty of Medicine at Harvard Medical School, Dr. Braunwalds bench to bedside approach to the limitations of myocardial infarct size is perhaps the greatest single example of an individual whose scientific research has led to dramatic translational benefits to improve patient care. Dr. Braunwalds direct contributions as a clinical investigator have
improved the prognosis and quality of life for patients with cardiovascular disease. In addition, through his role as the standard-bearer for academic excellence, his trainees augment and multiply his positive influence on biomedical research, education, and patient care.
and a
a
The TIMI Study Group The TIMI Study Group is the oldest cardiovascular Academic Research Organization in the United States. Since its inception in 1984, the principal goal of the TIMI Study Group has been to conduct high quality clinical trials that enhance the care of patients suffering from cardiovascular disease and its risk factors. Based at Brigham and Womens Hospital and Harvard Medical School, TIMI has completed over 50 clinical trials, ranging from phase 1 first-in-man studies to large-scale, registration pathway phase 3 trials examining clinical cardiovascular outcomes. Correspondingly, these trials have ranged in size from less than 30 to more than 25,000 subjects and have relied on a network of over 8000 investigators at over 4000 sites in 52 countries around the world. The interventions studied include antithrombotic, lipid-modifying, anti-ischemic, anti-arrhythmic, anti-inflammatory, anti-diabetic, and anti-obesity agents as well as percutaneous coronary intervention. In addition, the TIMI Study Group has used its growing database of approximately 400,000 subjects and their clinical findings, electrocardiograms, angiograms, biomarkers, and genotypes to enhance the understanding of cardiovascular disease and its risk factors. The results from TIMI trials have led to over 500 papers in top tier medical journals including the New England Journal of Medicine, Lancet, and JAMA, and TIMI papers are cited close to 4000 times a year. The data from TIMI trials have led to regulatory approval of multiple new medications or new indications for medications and have served as the evidence base for many class I recommendations in American and European practice guidelines. An important corollary goal has been to train the next generation of clinical investigators. TIMI is especially proud of these trainees who have assumed leadership positions in leading institutions around the world.
904040_Cover.indd 2 11/7/14 11:37 AM
-
TIMI TRIALS10TH EDITION, 1984 2014
Chairman: Marc S. Sabatine, MD, MPHDirector of Operations: Suzanne E. Morin
904040_Text.indd 1 11/7/14 11:48 AM
-
904040_Text.indd 2 11/7/14 11:48 AM
-
Table of ContentsListing of TIMI Trials ..................................................................................................................................... 6
TIMI Lessons 2014 ........................................................................................................................................ 8
1. Acute Reperfusion Therapy in STEMI .................................................................................................. 1
1.1 Fibrin-specific Lytics in STEMI ........................................................................................... 10
1.2 Pre-hospital Thrombolytic Therapy in STEMI ................................................................... 1
2. Antithrombotic Therapy in Vascular Disease ...................................................................................... 12
2.1 Antiplatelet Therapy ......................................................................................................... 12
2.2 Anticoagulant Therapy ...................................................................................................... 21
2.3 Other Means to Reduce Ischemic Outcomes ................................................................... 25
3. Risk Factor Modification ...................................................................................................................... 28
3.1 Intensive Lipid-lowering Therapy with Statins after ACS .................................................. 28
3.2 PCSK9 Inhibition ................................................................................................................ 29
3.3 Anti-diabetic Drugs ........................................................................................................... 30
4. Prevention of Stroke in AF ................................................................................................................... 31
5. Personalized Medicine ......................................................................................................................... 32
5.1 Clinical Risk Scores ............................................................................................................ 32
5.2 Angiographic Scores .......................................................................................................... 34
5.3 Biomarkers for Risk Stratification & Predicting Treatment Benefits ................................ 35
5.4 Pharmacogenetics ............................................................................................................. 38
Ongoing Trials............................................................................................................................................. 42
Recently Completed Trials ......................................................................................................................... 48
Completed Trials ........................................................................................................................................ 66
TIMI Bibliography ....................................................................................................................................... 91
904040_Text.indd 3 11/7/14 11:48 AM
-
TRIAL NAMETIMI 1
TIMI 2A
TIMI 2B
TIMI 3A
TIMI 3B
TIMI 3 Registry
TIMI 4
TIMI 5
TIMI 6
TIMI 7
TIMI 8
TIMI 9A/B
TIMI 9 Registry
TIMI 10A
TIMI 10B
ASSENT 1 (TIMI 10C)
TIMI 11A
TIMI 11B
TIMI 12
TIMI 14
TIMI 15A
TIMI 15B
OPUS-TIMI 16
InTIME 2-TIMI 17
TACTICS-TIMI 18
ER-TIMI 19
INTEGRITI (TIMI 20)
A2Z (TIMI 21)
PROVE IT-TIMI 22
ENTIRE-TIMI 23
FASTER (TIMI 24)
ExTRACT-TIMI 25
JUMBO-TIMI 26
PROXIMATE-TIMI 27
CLARITY-TIMI 28
ADVANCE MI (TIMI 29)
PROTECT-TIMI 30
TIMI TRIALS 2014INDICATION COMPARISON
STEMI tPA vs. SK
STEMI Immediate vs. Delayed Angioplasty
STEMI Invasive vs. Conservative Strategy / Immediate vs. Delayed Metoprolol
UA/NSTEMI Thrombolysis vs. Placebo
UA/NSTEMI Thrombolysis vs. Placebo / Invasive vs. Conservative Strategy
UA/NSTEMI Natural History Study
STEMI tPA vs. APSAC vs. Combination
STEMI Hirudin vs. Heparin in conjunction with tPA
STEMI Hirudin vs. Heparin in conjunction with SK
UA Hirulog Dose Ranging
UA/NSTEMI Hirulog vs. Heparin
STEMI Hirudin vs. Heparin in conjunction with thrombolytic
STEMI Natural History Study
STEMI TNK Dose ranging
STEMI TNK vs tPA (Angiographic)
STEMI TNK Dose Ranging
UA/NSTEMI Enoxaparin Dose Ranging
UA/NSTEMI Enoxaparin vs Heparin
Post-ACS Oral GP IIb/IIIa inhibitor Dose Ranging
STEMI Abciximab +/- low dose tPA/SK
ACS IV GP IIb/IIIa inhibitor Dose Ranging
ACS
ACS Oral GP IIb/IIIa inhibitor vs. Placebo
STEMI nPA vs. tPA
UA/NSTEMI Invasive vs. Conservative Therapy with Tirofiban
STEMI Early rPA vs Standard Therapy
STEMI Eptifibatide +/- TNK-tPA (Angiographic)
ACS Tirofiban + (Enoxaparin vs Heparin) / Simvastatin Early vs. Late
Post-ACS Pravastatin vs. Atorvastatin / Gatifloxacin vs. Placebo
STEMI Abciximab +/- TNK / Enoxaparin vs. Heparin (Angiographic)
STEMI Tirofiban +/- TNK (Angiographic)
STEMI Enoxaparin vs. Heparin in conjunction with Thrombolytic
PCI Prasugrel vs. Clopidogrel Dose Ranging
Stable CAD
STEMI Clopidogrel vs. Placebo with Thrombolytic
STEMI Facilitated PCI (Eptifibatide + TNK) vs.Direct PCI (Eptifibatide + Placebo)/ Enoxaparin vs. Heparin
PCI Bivalirudin vs. Heparin + Eptifibatide
904040_Text.indd 4 11/7/14 11:48 AM
-
COMPARISON
Tissue Factor/fVIIa inhibitor (rNAPc2) vs. Placebo
Ticagrelor vs. Clopidogrel
ED vs. Catheterization Lab initiated Eptifibatide with Primary PCI
Novel markers of ischemia during ETT
Ranolazine vs. Placebo
PARP inhibitor in STEMI
Prasugrel vs. Clopidogrel in PCI for ACS
Early eptifibatide vs. placebo before PCI
Simvastatin vs. Vytorin
Ticagrelor vs. Clopidogrel
Dose-Ranging Study of Otamixaban
Aliskiren Valsartan vs. Placebo to Reduce NT-proBNP
Prasugrel vs. Clopidogrel to Inhibit Platelet Aggregation
Degree of Platelet Inhibition and Bleeding in CABG Patients
Dose-Ranging Study of Rivaroxaban vs. Placebo
Intracoronary Eptifibatide vs. Placebo in PCI
Edoxaban (Oral Xa inhibitor) vs. Warfarin
Intracoronary Fibrinolytic vs. Placebo
Vorapaxar (Thrombin receptor antagonist) vs. Placebo
Rivaroxaban (Oral Xa inhibitor) vs. Placebo
Darapladib (Selective Lp-PLA2 inhibitor) vs. Placebo
Saxagliptin (DPP-4 inhibitor) vs. Placebo for CVD Pre-vention
Ticagrelor vs. Placebo
Anacetrapib vs. Placebo
Dose-Ranging Study of Clopidogrel in Reduced- Function CYP2C19 Carriers
Dose-Ranging Study of AMG145 (PCSK9 inhibitor) vs. Placebo
Dapagliflozin (SGLT2 inhibitor) vs. Placebo
Evolocumap (PCSK9 inhibiitor) vs. Placebo in combination with a statin
Losmapimod (p38 MAPK inhibitor) vs. Placebo
Lorcaserin (serotonin receptor agonist 5HT2CR) vs. Placebo
TRIAL NAME INDICATIONTIMI 31 STEMI
ANTHEM-TIMI 32 UA/NSTEMI
DISPERSE2-TIMI 33 UA/NSTEMI
TITAN-TIMI 34 STEMI
PROMPT-TIMI 35 Stable CAD
MERLIN-TIMI 36 UA/NSTEMI
TIMI-37A STEMI
TRITON-TIMI 38 PCI in ACS
EARLY ACS (TIMI 39) UA/NSTEMI
IMPROVE IT (TIMI 40) * Post-ACS
PLATO ACS
SEPIA-ACS1-TIMI 42 UA/NSTEMI
AVANT GARDE-TIMI 43 Post-ACS
PRINCIPLE-TIMI 44 PCI
VERIFY NOW-TIMI 45 CABG
ATLAS ACS-TIMI 46 Post-ACS
IC TITAN-TIMI 47 PCI
ENGAGE AF-TIMI 48 Atrial Fibrillation
ICE-T-TIMI 49 STEMI
TRA 2 P-TIMI 50 Stable Atherosclerosis
ATLAS ACS 2-TIMI 51 Post-ACS
SOLID-TIMI 52 Post-ACS
SAVOR-TIMI 53++ Diabetes
PEGASUS-TIMI 54* Stable Post-MI
REVEAL-TIMI 55+++* Stable Atherosclerosis
ELEVATE-TIMI 56 Stable CAD
LAPLACE-TIMI 57 Hypercholesterolemia
* Ongoing
+ In conjunction with Uppsala Clinical Research Center, Sweden++ In conjunction with Hadassah Medical Organization, Israel +++ In conjunction with Oxford University,United Kingdom(ACS = Acute Coronary Syndrome, CAD = Coronary Artery Disease, CVD = Cardiovascular Disease, ETT = exercise tolerance test, LMWH = Low Molecular Weight Heparin, NSTEMI = Non-ST- elevation myocardial infarction, PCI = Percutaneous Coronary Intervention, STEMI = ST-elevation myocardial infarction, UA = unstable angina)
DECLARE-TIMI 58++* Diabetes
FOURIER (TIMI 59)* Stable Atherosclerosis
LATITUDE-TIMI 60* ACS
CAMELLIA-TIMI 61* Obesity
904040_Text.indd 5 11/7/14 11:48 AM
-
904040_Text.indd 6 11/7/14 11:48 AM
-
904040_Text.indd 7 11/7/14 11:48 AM
-
904040_Text.indd 8 11/7/14 11:48 AM
-
10
Fibrin-Specific Lytics in STEMI Tissue plasminogen activator (tPA) improves reperfusion and clinical outcomes when compared to other thrombolytics in STEMI.
1. ACUTE REPERFUSION THERAPY IN STEMI1.1 Fibrin-specific Lytics in STEMI
6270
3143
Reperfusion ofoccluded arteries
Patency at90 minutes
0
20
40
60
80
% o
f Pat
ient
s t-PASK
*P
-
11
Pre-Hospital Thrombolytic Therapy in STEMI A strategy of pre-hospital administration of thrombolytic therapy reduces time to reperfusion.
AmbulanceArrival
ED Arrival In-hospital Lytic
CONTROLGROUPN = 598
STUDYGROUPN = 309
62 min (47 62 min (47 -- 85)85)
Data = median times (Q1 - Q3)
TIME SAVED
31 min p < 0.0001*
*Adjusted for any effect of site and interaction
rPA Bolus
31 min (24 - 37)
Morrow DA, J Am Coll Cardiol 2002; 40:71 -77
ERER--TIMI 19TIMI 19
ER-TIMI 19 enrolled 315 patients with STEMI. Pre-hospital administration of rPA was found to be feasible and reduced time-to-lytic time by 31 minutes.
1.2 Pre-Hospital Thrombolytic Therapy in STEMI
904040_Text.indd 10 11/7/14 11:48 AM
-
12
2.1.1 Clopidogrel in Thrombolysis for STEMI Clopidogrel improves both angiographic and clinical outcomes in patients receiving thrombolytic therapy in STEMI.
2. ANTITHROMBOTIC THERAPY IN VASCULAR DISEASE
2.1 Antiplatelet Therapy
CV Death, MI,RI Urg Revasc
daysP
erce
ntag
e w
ith e
ndpo
int (
%)
05
1015
0 5 10 15 20 25 30
Placebo
Clopidogrel
Odds Ratio 0.80(95% CI 0.65-0.97)
P=0.026
20%20%20%
Sabatine MS, N Engl J Med 2005; 352:1179 -89
In CLARITY-TIMI 28, the addition of clopidogrel to fibrinolytic therapy also significantly reduced the odds of major cardiovascular events by 20% at 30 days.
In CLARITY-TIMI 28, subjects who were pre-treated with clopidogrel prior to PCI had a significant 46% reduction in the risk of cardiac events after PCI after adjusting for baseline differences. Of note, the benefit of pre-treatment appeared early and continued to persist over time.
Occluded Artery (or D/MI thru Angio/HD)
15.0
21.7
0
5
10
15
20
25
Occ
lude
d Ar
tery
or D
eath
/MI
(%)
PlaceboClopidogrel
n=1752 n=1739
36%Odds Reduction
36%Odds Reduction
CLARITY-TIMI 28 enrolled 3491 patients (
-
13
2.1.2 Prasugrel in ACS
More potent platelet inhibition with prasugrel significantly improves clinical outcomes in patients with ACS undergoing PCI as compared to clopidogrel, but with an increased risk of bleeding.
TRITON-TIMI 38 randomized 13,608 patients with ACS undergoing PCI to prasugrel or clopidogrel. Prasugrel significantly reduced the risk of death, MI or stroke by 19% (Absolute Risk Reduction [ARR] of 2.2%; Number Needed to Treat [NNT] = 46). Although bleeding rates were low, prasugrel significantly increased the risk of TIMI major bleeding by 32% (Absolute Risk Elevation [ARE] = 0.6%; Number Needed to Harm [NNH] = 167.
In TRITON-TIMI 38, subjects randomized to prasugrel had a significant 52% reduction in the risk of stent thrombosis compared to clopidogrel. This benefit was seen for both drug-eluting and bare-metal stents.
In the setting of ACS, prasugrel significantly reduces the risk of stent thrombosis by 52% compared to a 300mg loading dose and 75mg maintenance dose of clopidogrel.
904040_Text.indd 12 11/7/14 11:48 AM
-
14
Prasugrel reduced major adverse cardiovascular events in STEMI patients.
In the 3534 participants presenting with STEMI, the treatment with prasugrel resulted in a 32% reduction in cardiovascular death, non-fatal myocardial infarction or non-fatal stroke at 30 days (HR 0.68, 0.54-0.87; p=0.0017) compared to placebo, with continued effect to 15 months. Other secondary endpoints, including cardiovascular death, myocardial infarction and stent thrombosis were significant reduced with prasugrel compared to clopidogrel in STEMI patients.
904040_Text.indd 13 11/7/14 11:48 AM
-
15
In TRITON-TIMI 38, 4,529 patients were on a PPI at randomization and no association existed between PPI use and the risk of the CV events for patients treated with clopidogrel or prasugrel. These findings do not support the need to avoid concomitant use of PPIs, when clinically indicated, in patients receiving clopidogrel or prasugrel.
Diabetic patients appeared to derive particular benefit from prasugrel over clopidogrel in the setting of ACS.
There is concern PPIs can interfere with thienopyridine biotransformation by cytochrome P450, which is a two-step oxidation process for clopidogrel and a single oxidation step for prasugrel. In TRITON-TIMI 38, PPI treatment did not affect the clinical outcome of patients given either thienopyridine affirming patients can safely be treated with a PPI and thienopyridine.
0
5
10
15
0 30 60 90 180 270 360 450
HR 0.81(0.73-0.90)P=0.0004
Prasugrel
Clopidogrel
Days
Endp
oint
(%)
12.1
9.9
HR 1.32(1.03-1.68)
P=0.03
Prasugrel
Clopidogrel1.82.4
1o EP: CV Death / MI / Stroke
TIMI MajorNonCABG Bleeds
Wiviott SD, N Engl J Med 2007; 357:2001-15
TRITONTRITON--TIMI 38TIMI 38
904040_Text.indd 14 11/7/14 11:48 AM
-
16
In PLATO, ticagrelor was superior to clopidogrel for reducing cardiovascular events in invasively managed ACS patients without an increase in total major bleeding.
2.1.3 Ticagrelor is Superior to High-Dose Clopidogrel in Invasively Managed Patients with ACS More potent, early, and reversible platelet inhibition with ticagrelor significantly improves clinical outcomes in patients with ACS as compared to 300-600mg loading dose and 75mg maintenance dose of clopidogrel, without an increased risk of total major bleeding.
904040_Text.indd 15 11/7/14 11:48 AM
-
Giugliano et al. NEJM 2009;360:2176-90
N = 4722N = 4684
OR 0.89 (0.79, 1.01)P = 0.072
N = 4684 N = 4722
OR 1.75 (1.43, 2.13)P < 0.001
OR 0.92 (0.80, 1.06)P = 0.23
N = 4643 N = 4686
10.0%12.3%
3.4%
9.3%11.2%
5.7%
0%
5%
10%
15%
D/MI/RI UR/TBOat 96h D/MI at 30d
TIMI Major/MinorBleeding at 120h
Delayed ProvisionalEarly Routine
ResultsEARLY ACS (TIMI 39)EARLY ACS (TIMI 39)
Giugliano RP et al. NEJM 2009;360:2176-90
D = Death; MI = Myocardial Infarction; RI UR = Recurrent Ischemia leading to Urgent Revascularization; TBO = Thrombotic Bailout with bolus therapy Opposite to initial study-group assignment
EARLY ACS (TIMI 39) randomized 9,492high risk NSTE-ACS patients to early, routine or delayed, provisional administration of eptifibatide. Early use was not associated with improved outcomes as compared with provisional use and led to significantly higher rates of major bleeding.
17
2.1.4 Routine versus Provisional GP IIb/IIIa Inhibition in NSTE-ACS A strategy of dealyed, provisional eptifibatide yields similar ischemic outcomes and less bleeding compared with early, routine use in patients with NSTE-ACS.
904040_Text.indd 16 11/7/14 1:29 PM
-
18
TRA 2 P-TIMI 50 randomized 26,449 patients who had a history of myocardial infarction, ischemic stroke, or peripheral arterial disease to vorapaxar or placebo. Vorapaxar significantly reduced the risk of death, MI or stroke by 13% (Absolute Risk Reduction [ARR] of 1.2%, but significantly increased the risk of moderate or severe bleeding by 66% (Absolute Risk Elevation [ARE] = 1.7%).
Morrow et al. NEJM 2012; 366: 1404-13.
2.1.5 Vorapaxar in Vascular Disease
The addition of vorapaxar, a PAR-1 inhibitor, to standard background anti-thrombotic therapy reduces the risk of cardiovascular death or ischemic events in patients with coronary artery disease, peripheral artery disease, or cerebrovascular disease. Vorapaxar increased bleeding particularly in patients with prior stroke.
904040_Text.indd 17 11/7/14 11:48 AM
-
19
Scirica BM et al. Lancet 2012; 380:1317-24.
The addition of vorapaxar to standard background anti-thrombotic therapy reduces the risk of cardiovascular death or ischemic events in patients with prior MI.
TRA 2 P-TIMI 50 included 17,779 patients with prior MI among whom the addition of vorapaxar, as compared to placebo, significantly reduced the risk of death, MI or stroke by 20% (Absolute Risk Reduction [ARR] of 1.6%, but significantly increased the risk of moderate or severe bleeding by 61% (Absolute Risk Elevation [ARE] = 1.3%). The benefit of vorapaxar was consistent across thienopyridine use, prior PCI status, and qualifying event. Notably, the benefit of intensified antiplatelet therapy with vorapaxar in patients with prior MI was evident early and persisted beyond 1 year.
904040_Text.indd 18 11/7/14 11:48 AM
-
20
TRA 2 P-TIMI 50 included 3,767 patients enrolled based on a history of symptomatic peripheral arterial disease (PAD), defined as claudication and an ankle-brachial index
-
21
2.2.1 Enoxaparin in NSTE-ACS - Enoxaparin improves outcomes compared to unfractionated heparin in patients with non-ST-elevation ACS.
2.2.2 Enoxaparin for Conservative Management of NSTE-ACS -Enoxaparin was superior to unfractionated heparin when evaluated in early conservative management of NSTE-ACS
2.2 Anticoagulant Therapy
Antman EM, Circulation 1999; 100:1593-01
TIMI 11BTIMI 11B
22446688
101012121414161618182020
00 22 44 66 88 1010 1212 1414
P=0.029RRR 15 %
UFHUFHENOXENOX
16.7 %16.7 %
14.2 %14.2 %%
Days
14.5 %14.5 %
12.4 %12.4 %
P=0.048RRR 15 %
Death, MI or Urgent Revascularization at 14 DaysTIMI 11B randomized 3,910 patients with NSTE-ACS to UFH or enoxaparin. Enoxaparin significantly reduced the risk of death, MI or urgent revascularization at both 8 and 14 days.
In A to Z, 3987 patients with NSTE-ACS receiving aspirin and tirofiban were randomized to enoxaparin or unfractionated heparin. The rate of death, Myocardial infarction and refractory ischemia was significantly reduced with enoxparin Compared to unfractinated heparin (HR 0.88, 0.71-1.08). There was a trend towards greater benefit from enoxaparin in those managed with an early conservative as compared to early invasive strategy.
Blazing et al. JAMA 2004: 292: 1; 55.
904040_Text.indd 20 11/7/14 11:48 AM
-
22
ExTRACTExTRACT--TIMI 25TIMI 25
12.09.9
UFH UFH
ENOX ENOX
14.511.7
Days Days
%% RR = 0.83p = 0.000003
RR = 0.81p = 0.000001
Primary Endpoint:Death or MI
Main Secondary Endpoint:Death, MI or Urgent Revasc
Antman EM, N Engl J Med 2006; 354:1477-88
ExTRACT-TIMI 25 randomized 20,506 patients with STEMI receiving fibrinolytic therapy to enoxaparin through hospitalization or UFH for 48 hours. Enoxaparin significantly reduced the risk of death or MI by 17% (left panel) and reduced the risk of death, MI or urgent revascularization by 19% (right panel) by 30 days follow-up.
2.2.3 Enoxaparin in Thrombolysis for STEMI A strategy of enoxaparin through index hospitalization is superior to unfractionated heparin for 48 hours in patients receiving thrombolytic therapy for STEMI.
904040_Text.indd 21 11/7/14 11:48 AM
-
23
A meta-analysis that included data from 16 trials involving 33958 patients, of whom 2422 experienced MACE and 1406 had a major bleed found an increase in the risk of MACE with bivalirudin as compared to heparin-based regimens (risk ratio 109, 95% CI 101 117; p=00204). This was largely driven by increases in myocardial infarction (112, 103 123) and also by ischemia-driven revascularization (116, 0997 134) with no effect on mortality (099, 082 118). Bivalirudin increased the risk of stent thrombosis (risk ratio 138, 95% CI 109 174; p=00074), which was primarily due to an increase in acute cases in ST-segment elevation myocardial infarction (427, 228 800; p
-
24
ATLAS-ACS 2 TIMI 51 randomized 15,526 patients with a recent acute coronary syndrome to low dose rivaroxaban (5mg BID), very low dose rivaroxaban (2.5mg BID), or placebo. Overall, rivaroxaban significantly reduced the rate of cardiovascular death, MI, or stroke by 16% (Absolute Risk Reduction [ARR] of 1.8%) but significantly increased the risk of major bleeding not related to CABG and intracranial hemorrhage. Very low dose rivaroxaban (2.5mg BID) significantly reduced the rate of cardiovascular death and all-cause death.
Mega JL et al. NEJM 2012; 366: 9-19.
2.2.5 Rivaroxaban Improves Outcomes in Patients Stabilized Post-ACS The addition of low-dose rivaroxaban, an oral factor Xa inhibitor, to background antiplatelet therapy reduced the risk of cardiovascular death or ischemic events in patients stabilized after an ACS. Very low-dose rivaroxaban (2.5mg twice daily) also significantly reduced the risk of cardiovascular and all-cause death.
904040_Text.indd 23 11/7/14 11:48 AM
-
25
2.3.1 Beta-Blockade in STEMI - Early administration of intravenous beta-blockers reduces the risk of reinfarction or recurrent ischemia in stable patients with STEMI.
2.3 Other Means to Reduce Ischemic Outcomes
TACTICSTACTICS--TIMI 18TIMI 18
0 1 2 3 4 5 6Time (months)
0
4
8
12
16
20
% P
atie
nts
0 1 2 3 4 5 6Time (months)
0
4
8
12
16
20
% P
atie
nts
CONSINV
O.R 0.7895% CI (0.62, 0.97)
p=0.025
19.4%
15.9%
Death, MI, Rehosp for ACS at 6 Months
Cannon CP, N Engl J Med 2001; 344:1879-87
TACTICS-TIMI 18 randomized 2,220 patients with UA or NSTEMI to an early invasive strategy (routine cardiac catheterization
-
26
High risk women derive greater benefit from invasive strategy in NSTE-ACS.
Women are more likely to have non-obstructive CAD at catheterization.
Early invasive strategy in women: Although some studies suggested that women may not benefit from an invasive strategy, metanalysis indicated that women with high-risk features, such as elevated biomarkers of necrosis, derive comparable benefit from an invasive strategy in NSTE-ACS as men. In contrast, women without high-risk predictors should undergo further risk stratification before cardiac catheterization in NSTE-ACS.
Sex differences in the prevalence of CAD at catheterization: In a meta-analysis of randomized trials that compared an invasive versus conservative strategy in patients with NSTE-ACS, it was demonstrated that women are significantly less likely to have obstructive CAD at catheterization. In contrast, men are significantly more likely to have 3 vessel or left main disease.
904040_Text.indd 25 11/7/14 11:48 AM
-
27
2.3.3 Ranolazine
Ranolazine reduces recurrent ischemia after NSTE-ACS, but does not significantly change the risk of death or recurrent MI.
Ranolazine significantly reduced the risk of arrhythmias after NSTE-ACS. Ventricular ectopy lasting at least 4 beats in patients with NSTE-ACS is independently associated with increased risk of SCD even in the modern era of widespread use of reperfusion, revascularization, and contemporary medical therapy.
Morrow DA, JAMA 2007; 297:1775 -83
Secondary Endpoint:Recurrent Ischemia (%)
Days from Randomization
Ranolazine 13.9%*(N=3,279)
Placebo 16.1%*(N=3,281)
0 180 360 540
HR 0.87 (95% CI 0.76 to 0.99)P =0.030
0
5
10
15
20
CV Death, MI, or Recurrent Ischemia (%)
0
10
20
30
0 180 360 540
Days from Randomization
HR 0.92 (95% CI 0.83 to 1.02)P = 0.11
Ranolazine 21.8%*(N=3,279)
Placebo 23.5%*(N=3,281)
HR 0.92 (95% CI 0.83 to 1.02)P = 0.11
Ranolazine 21.8%*(N=3,279)
Placebo 23.5%*(N=3,281)
*KM cumulative incidence (%) at 12 months
Morrow DA, JAMA 2007; 297:1775 -83
MERLINMERLIN --TIMI 36TIMI 36
MERLIN-TIMI 36 randomized 6,560 patients with NSTE-ACS to the novel anti-ischemic agent ranolazine or placebo. Ranolazine did not significantly reduce the risk of the composite endpoint of CV death, MI or recurrent ischemia.
In MERLIN-TIMI 36, ranolazine significantly reduced the risk of recurrent ischemia by 13% compared to placebo (P=0.03), supporting its use as an anti-ischemic drug.
In MERLIN-TIMI 36, ranolazine significantly reduced the incidence of VT by 37%. In MERLIN-TIMI 36,
following NSTE-ACS was independently associated with risk of SCD.
SCD by length of longest episode of ventricular tachycardia
0
2
4
6
0 200 400Days from Randomization
No VT (n=2764)1.2%
(n=1978)1.4%
VT 4 -7 beats (n=1172)2.9%
VT >= 8 beats (n=431)
4.3%
Sudd
en C
ardi
ac D
eath
(%)
No. at RiskPlacebo 3184 3023 2647 1964 1167Ranolazine 3161 2994 2627 1951 1191
Triplets (VT=3 beats)
Risk vs. No Triplets or VTTriplets - HR* 1.1 (0.67-1.8), p=0.74VT 4-7bts - HR* 2.3 (1.5-3.7), p=8bts - HR* 2.8 (1.5-5.1), p=0.001
* Adjusted for TIMI Risk Score, Prior MI, Prior HF, CrCl, revasc during index hospitalization
Scirica BM, Circulation. 2010;122:455-462
904040_Text.indd 26 11/7/14 11:48 AM
-
28
After ACS, intensive lipid-lowering therapy with a high-potency statin significantly reduces the risk of adverse outcomes as compared to moderate-potency statin therapy.
The benefit of intensive lipid-lowering therapy appears early after ACS and persists over time.
3. RISK FACTOR MODIFICATION3.1 Intensive Lipid-lowering Therapy with Statins after ACS
The PROVE-IT TIMI 22 trial randomized 4162 patients to treatment with atorvastatin 80mg QD or pravastatin 40mg QD after ACS. Intensive lipid-lowering therapy with atorvastatin to a median LDL of 62 mg/dl significantly reduced the risk of the primary endpoint by 16% (P=0.005) and death, MI or urgent revascularization by 35% (P=0.0004, Figure).
In the PROVE-IT TIMI 22 trial, the benefit of atorvastatin 80mg compared to pravastatin 40mg appeared within the first month of starting therapy. At 30 days, atorvastatin 80mg significantly reduced the risk of death, MI or urgent revascularization by 33% (P=0.04, Figure).
904040_Text.indd 27 11/7/14 11:48 AM
-
29
Intensive lipid-lowering after ACS appears to be safe and efficacious even at very low achieved LDL concentrations.
In PROVE-IT TIMI 22, patients who achieved very low LDL concentrations appeared to derive as much benefit with intensive lipid-lowering therapy after ACS, as patients with higher achieved lipid values (left panel). There were no significant differences in safety parameters, including muscle, liver (right panel), or retinal abnormalities, ICH, or death, in the very low LDL group.
Administration of the PCSK9 inhibitor Evolocumab (AMG 145) reduced LDL-C by up to 66% in patients treated with statin.
3.2 PCSK9 Inhibition
The phase II dose-ranging LAPLACE-TIMI 57 trial randomized 631 stable hypercholesterolemic patients treated with statin to one of 6 doses of Evolocumab vs placebo administered subcutaneously every 2 or 4 weeks. Evolocumab reduced LDL-C at 12 weeks by 42-66% compared to placebo, in a dose-dependent fashion.
Giugliano RP et al. Lancet. 2012;380:2007-17
Wiviott SD, J Am Coll Cardiol 3005; 46:1411-16.
904040_Text.indd 28 11/7/14 11:48 AM
-
The DPP4 inhibitor saxagliptin neither increases nor decreases the risk of ischemic complications but increases risk of hospitalization for heart failure in patients at high cardiovascular risk.
3.3 Anti-Diabetic Drugs
SAVOR-TIMI 53 randomized 16,492 patients with T2DM and either established cardiovascular disease or multiple cardiovascular risk factors to saxagliptin or placebo, in addition to standard care. The primary safety objective of the trial was met, demonstrating that this novel agent known to effectively lowers A1c is not associated with increased cardiovascular ischemic events. There was, though, an unexpected 27% relative (0.8% absolute) increase in the risk of hospitalization for heart failure in patients treated with saxagliptin that was most evident in those patients with impaired renal function, history of prior heart failure, or elevated levels of natriuretic peptides.
30
904040_Text.indd 29 11/7/14 11:48 AM
-
31
4.1 Edoxaban in patients with Atrial Fibrillation - Two dose regimens of the once daily oral Factor Xa inhibitor edoxaban were non-inferior to well-managed warfarin while significantly reducing bleeding.
4. PREVENTION OF STROKE IN AF
The ENGAGE AF-TIMI 48 trial randomized 21,105 patients with AF at moderate to high risk of stroke to one of two dose regimens of once-daily edoxaban vs warfarin. Both dose regimens of edoxaban were non-inferior in the prevention of stroke or systemic embolism, with the higher dose regimen tending to be superior. Both dose regimens of edoxaban significantly reduced a variety of bleeding events, including major, intracranial, and fatal hemorrhage.
904040_Text.indd 30 11/7/14 11:48 AM
-
32
5.1.1 TIMI Risk Score for UA/NSTEMI The TIMI Risk Score for UA/NSTEMI is a simple prognostication scheme that categorizes a patients risk of death and ischemic events and provides a basis for therapeutic decision making.
5.1.2 TIMI Risk Score for STEMI The TIMI Risk Score for STEMI is a useful tool for helping to identify those individuals at increased risk of death after STEMI.
TIMI 11BTIMI 11B
4.7 8.313.2
19.926.2
40.9
0
10
20
30
40
50
0/1 2 3 4 5 6/7
TIMI Risk Score for UA/NSTEMI
Death, MI, Urgent Revascularization by TRS
Antman EM, JAMA 2000; 284:835-42
One Point for each of:Age > 65 y> 3 CAD RiskFactorsPrior Stenosis> 50 % ST deviation> 2 Anginalevents < 24 hASA in last 7 daysElevated Cardiac Markers
The TIMI Risk Score for UA/NSTEMI consists of a 7-point scale. As TIMI Risk Score increases, patients have a steep increase in the risk of adverse outcomes. The score was derived and validated in TIMI 11B and ESSENCE, but has since been validated in several trials including TIMI 3B, TACTICS-TIMI 18, MERLIN-TIMI 36, and CURE.
The TIMI Risk Score for STEMI consists of a 14-point scale based on history, exam and presentation. A higher TIMI Risk Score is associated with an increased risk of death. The score was derived in InTIME 2 and first validated in TIMI 9. The score has since been validated in several populations including TIMI 17, ExTRACT-TIMI 25, CLARITY-TIMI 28 and NRMI.
0.8 1.6 2.24.4
7.312.4
16.123.4
26.8
35.9
0
10
20
30
40
50
0 1 2 3 4 5 6 7 8 >8
TIMI 17TIMI 17
TIMI Risk Score for STEMI
Mortality at 30 d by STEMI TRS
Morrow DA, Circulation 2000; 102:2031-37
HistoricalAge 65-74 2pts
>75 3ptsDM/HTN/Angina 1ptExamSBP < 100 mmHg 3ptsHR > 100 bpm 2ptsKillip II IV 2ptsWeight < 67 kg 1 ptPresentationAnterior STE orLBBB 1 ptTime to Rx > 4hr 1pt------------------------------------Risk Score = Total (0-14)
5. PERSONALIZED MEDICINE5.1 Clinical Risk Scores
904040_Text.indd 31 11/7/14 11:48 AM
-
33
5.1.3 TIMI Risk Index A simple risk index based on characteristics that are easily assessed and captures most of the information from more complex tools, and is useful for risk stratification in patients with STEMI.
5.1.4 TIMI Bleeding Classification The TIMI Bleeding Classifications are widely used across clinical trials to grade severity of bleeding. Bleeding has been shown to be associated with an increased risk of adverse outcomes. The TIMI Bleeding Classifications have been expanded to include new definitions (shown at right).
Bleeding Requiring Medical Attention:Bleeding Requiring Medical Attention:Any overt sign bleeding that requires intervention (medical or surgical treatment), leads to hospitalization or prompting evaluation (unscheduled contact with a healthcare professional and diagnostic testing) and does not meet criteria for TIMI major or minor bleeding.
UpdatedUpdated
Instrumented Bleeding:Instrumented Bleeding:Any hemorrhage that occurs as a result of an invasive procedure.Spontaneous Bleeding:Spontaneous Bleeding:Any hemorrhage that is not the direct result of an invasive procedure (e.g. gingival bleeding, epistaxis, gastrointestinal bleeding).
TIMI 17TIMI 17
Simple Risk Score for STEMI
Morrow DA, Lancet 2001; 358:1571-75
SimpleRisk Score
Heart Rate x [Age/10]2SBP
Quartile Q1 Q2 Q3 Q4 Q5Range 30
30-day mortality by 43% for every 5 point in risk score
0.2 0.6 0.80.41.5 1.91.0
3.1 3.32.4
6.5 7.36.9
15.817.4
0
4
8
12
16
20
24
24 Hours In-hospital 30 Days
Q1 Q2 Q3 Q4 Q5
Mor
talit
y (%
)
The TIMI risk is calculated using a combination of patient heart rate, age and SBP at presentation. Every 5-point increase in score is associated with a 43% increase in 30-day mortality. The index was derived in InTIME 2 and validated in TIMI 9, ExTRACT-TIMI 25 and NRMI.
904040_Text.indd 32 11/7/14 11:48 AM
-
34
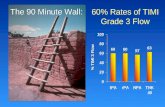
5.2.1 TIMI Flow Grade The TIMI Flow Grade is universally used to assess epicardial perfusion at angiography. A higher TIMI Flow Grade is strongly associated with increased survival.
5.2.2 TIMI Frame Count The TIMI Frame Count was established to enhance reproducibility of the angiographic assessment of coronary blood flow. As TIMI Frame Count increases, there is an increased risk of adverse clinical outcomes.
5.2 Angiographic Scores
TIMI 0TIMI 0 Complete occlusion
TIMI 1TIMI 1 Penetration of obstruction bycontrast but no distal perfusion
TIMI 2TIMI 2 Perfusion of entire arterybut delayed flow
TIMI 3TIMI 3 Full perfusion, normal flow
10.6
7
4.7
0
2
4
6
8
10
12
14
TIMI 0/1 TIMI 2 TIMI 3Flygenring BP, J Am Coll Cardiol 1991; 17:275A
Mortality at 42 Days
P < 0.005
TIMI Flow Grade
TIMI 1TIMI 1
TIMI Flow Grade is scored from 0-3 with TIMI Flow Grade 0 representing a complete occlusion and TIMI Flow Grade 3 representing normal perfusion (left). TIMI Flow Grade strongly predicts mortality (right) and has been validated in several trials.
8%16%
19% 22%22%
43%
0%
10%
20%
30%
40%
50%
60%
0
-
35
5.2.3 TIMI Myocardial Perfusion Grade The TIMI Myocardial Perfusion Grade assesses microvascular perfusion and is also associated with increased survival independent of TIMI Flow Grade.
5.3.1 Troponin in ACS Troponin is a powerful predictor of outcomes and is useful for helping to identify individuals who may benefit more from particular treatment strategies, including GP IIb/IIIa inhibitors and an early invasive strategy in NSTEMI.
0.7
2.9
5.44.7
7.5
0
2
4
6
8
10
12
Mor
talit
y (%
)
Epicardial TIMI Grade 3 FlowOverall Mortality: 3.7%
Epicardial TIMI Grade 2/1/0Overall Mortality: 7%
Myocardial Perfusion Grade 3
5 way p = 0.007
Myocardial Perfusion Grade 2
Myocardial Perfusion Grades 0/1
Myocardial Perfusion Grade 3
Myocardial Perfusion
Grades 2/1/0
TIMI 10BTIMI 10BMyocardial Perfusion Grade
Gibson CM, Circulation 1999; 99:1945-50
TIMI Myocardial Perfusion Grade is scored from 0-3 with TMPG 0 representing no apparent tissue-level perfusion and TMPG 3 indicating that blush begins to fade during washout. Regardless of TIMI Flow Grade, a lower TMPG was associated with an increased risk of death in TIMI 10B.
5.3 Biomarkers for Risk Stratification & Predicting Treatment Benefit
831 174 148 134 6750
Risk Ratio 1.0 1.8 3.5 3.9 6.2 7.8
0 to
-
36
5.3.2 Minor Elevations in Troponin in ACS Demonstration that even minor elevations in troponin are associated with an increased risk of adverse outcomes in patients with ACS.
5.3.3 Ultra-Sensitive Troponin Ultrasensitive assays for troponin reveal myocardial injury in nearly all patients with ACS and in some patients with provoked ischemia. The emergence of a new generation of troponin assays has the potential to lead to new clinical applications based on enhanced analytical performance at very low concentrations.
OR (p-value)
< 0.1 0.1 to
-
37
5.3.4 Multimarker Strategy in ACS A multimarker strategy that reflects complementary pathobiological axes of ACS can provide incremental information for risk stratification when compared to a single marker alone.
A simple multimarker strategy that categorizes patients based on the number of elevated biomarkers (troponin, BNP and CRP) at presentation. As the number of elevated biomarkers increases, there is a near doubling of mortality risk and cardiac events for each additional biomarker that is elevated. The score was derived in OPUS-TIMI 16 and first validated in TACTICS-TIMI 18.
5.3.5 BNP in ACS B-type natriuretic peptide (BNP) is a powerful predictor of risk of death after ACS.
Sabatine MS, Circulation 2002; 105:1760-63
1.0
2.1
3.2
4.5
0
1
2
3
4
5
0 1 2 3# of Elevated Markers
RR of D/MI/CHF at 6months
Assign patients 1 point for the presence of each elevated biomarker (TnI > 0.1 ng/ml, CRP > 1.5 mg/dl, BNP > 80 pg/ml).
1.00.2 0.5 2 51.00.2 0.5 2 5
OR & 95% CI for D/MI/CHF by 6 months
Age (per year)
Diabetes
Prior MI
Prior CHF
ST deviation
0 Biomarkers
1 Biomarker
2 Biomarkers
3 Biomarkers
TACTICSTACTICS--TIMI 18TIMI 18
In OPUS-TIMI 16, elevated levels of BNP were associated with an increased risk of death at 10 months. The unadjusted rate of death increased in a stepwise fashion among patients in increasing quartiles of baseline BNP levels (P< 0.001).
In the A2Z trial, patients with a BNP >80 pg/ml measured 4 months after ACS had a 3.4-fold increase in the risk of death or new heart failure through 2 years of follow-up (P
-
38
5.3.6 C-Reactive Protein After ACS When measured 30 days after ACS, high-sensitivity C-reactive protein (hsCRP) is a powerful predictor of outcomes, independent of achieved LDL concentration. Intensive statin therapy significantly reduces hsCRP and, in part, helps to attenuate the increased risk of death or MI seen with higher levels of hsCRP.
5.4.1 CYP2C19 Polymorphisms and Outcomes with Clopidogrel and Prasugrel Among patients on clopidogrel, carriers of a CYP2C19 reduced-function allele have diminished antiplatelet effect and an increased risk of events. These genetic polymorphisms do not affect the antiplatelet effect of prasugrel or result in an increased risk of events, which may explain in part the different pharmacological and clinical responses to the two medications.
In PROVE-IT TIMI 22, patients who have low hsCRP levels after statin therapy have better clinical outcomes than those with higher CRP levels, regardless of achieved LDL cholesterol. Atorvastatin 80mg significantly reduces hsCRP more than pravastatin 40mg (left) and may in part attenuate the higher risk of events with elevated hsCRP (right).
CYP2C19 is an isoform of cytochrome P450 and is involved in the metabolism of clopidogrel to its active metabolite. In ACS patients within TRITON-TIMI 38, carriers of a reduced-function allele who were treated with clopidogrel had a significant 53% increase in the risk of adverse events despite similar baseline characteristics. Carrier status of the CYP2C19 reduced-function allele had no significant clinical effect in those ACS patients treated with prasugrel.
5.4 Pharmacogenetics
Ridker P, N Engl J Med 2005; 352:20-28.
904040_Text.indd 37 11/7/14 11:48 AM
-
39
A Meta Analysis of CYP2C19 Reduced Function Polymorphisms and Outcomes -- Among patients on clopidogrel and who have undergone PCI, carriers of 1 or 2 CYP2C19 reduced-function allele(s) have diminished antiplatelet effect and an increased risk of major cardiovascular events.
5.4.2 Tailoring Clopidogrel Dosing Based on CYP2C19 Genotype Tripling the dose of clopidogrel among patients carrying 1 reduced function CYP2C19 allele achieves similar levels of platelet reactivity to that achieved by standard dose clopidogrel in non-carriers.
Mega JL et al. JAMA. 2010;304(16):1821-1830
Mega JL et al. JAMA 2011;306(20): 2221-8.
A meta-analysis of 9 studies evaluating CYP2C19 genotype and clinical outcomes in patients treated with clopidogrel and undergoing PCI demonstrates that carriers of reduced function allele(s) have a significantly increased risk of adverse CV events and stent thrombosis
The ELEVATE-TIMI 56 trial genotyped 333 patients with stable cardiovascular disease and randomized carriers of loss-of-function CYP2C19*2 alleles to 75, 150, 225, and 300mg of clopidogrel daily. Tripling the maintenance dose of clopidogrel to 225mg daily in stable heart disease patients carrying 1 reduced function allele achieved similar levels of platelet reactivity as achieved by standard dose clopidogrel in noncarriers.
904040_Text.indd 38 11/7/14 11:48 AM
-
Trials
904040_Text.indd 39 11/7/14 11:48 AM
-
904040_Text.indd 40 11/7/14 11:48 AM
-
ONGOING CLINICAL TRIALS
42
History of MI 1-3 yrs prior+ 1 additional atherothrombosis risk factor*N ~ 21,000
Ticagrelor90 mg bid Placebo
RANDOMIZEDOUBLE BLIND
Follow-up VisitsQ4 mos for 1st yr, then Q6 mos
Planned treatment with ASA 75 150 mg &
Standard background care
Primary Efficacy Endpoint: CV Death, MI, or StrokePrimary Safety Endpoint: TIMI Major Bleeding
* Age >65 yrs, diabetes, 2nd prior MI, multivesselCAD, or chronic non-end stage renal dysfunction
Min 12 mos and average 26 mos follow-upEvent-driven trial
Ticagrelor60 mg bid
Protocol DesignPEGASUS TIMI 54
IMPROVE IT -blind trial designed to assess the benefit of treating to LDL goals even lower than those targeted in PROVE IT-TIMI 22 with a combination of simvastatin and ezetimibe in patients stabilized after ACS.
(TIMI 40) is a randomized, double
PEGASUS TIMI 54 is a randomized, double-blind, placebo-controlled trial to assess the prevention of thrombotic events with ticagrelor on a background of aspirin therapy in patients with history of myocardial infarction.
904040_Text.indd 41 11/7/14 11:48 AM
-
ONGOING CLINICAL TRIALS
43
HPS3 / REVEAL TIMI 55 will assess the effect of Cholesteryl ester transfer protein (CETP) inhibition with anacetrapib 100 mg versus matching placebo on time to first major coronary event among 30,000 individuals with pre-existing vascular disease.
DECLARE-TIMI 58 is a superiority trial and designed to test the hypothesis that in patients with type 2 diabetes mellitus long-term treatment with dapagliflozin will reduce the incidence of the composite endpoint of cardiovascular death, myocardial infarction, or ischemic stroke.
904040_Text.indd 42 11/7/14 11:48 AM
-
ONGOING CLINICAL TRIALS
44
LATITUDE-TIMI 60 will assess whether losmapimod can safely reduce the risk of a subsequent cardiovascular event when started immediately after ACS.
FOURIER (TIMI 59) is a double-blind, randomized, placebo-controlled, multicenter study assessing the Impact of additional LDL-cholesterol reduction on major cardiovascular events when AMG 145 is used in combination with statin therapy in patients with clinically evident cardiovascular disease.
904040_Text.indd 43 11/7/14 11:48 AM
-
ONGOING CLINICAL TRIALS
45
CAMELLIA-TIMI 61 is a multicenter, randomized, double-blind, placebo-controlled, parallel-group study in overweight and obese subjects with CV disease and/or multiple CV risk factors.
904040_Text.indd 44 11/7/14 11:48 AM
-
Trials
904040_Text.indd 45 11/7/14 11:48 AM
-
904040_Text.indd 46 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
48
ENGAGE-AF-TIMI 48 is a randomized, double-blind trial to assess the efficacy and safety of edoxaban, an oral Factor Xa inhibitor, versus warfarin in preventing thromboembolic events in patients with moderate-high risk atrial fibrillation.
Giugliano RP et al. N Engl J Med 2013; 369: 2093-104
Giugliano RP et al. N Engl J Med 2013; 369: 2093-104
904040_Text.indd 47 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
49
Both dose regimens of edoxaban were non-inferior in the prevention of stroke or systemic embolism, with the higher dose regimen tending to be superior. Both dose regimens of edoxaban significantly reduced a variety of bleeding events, including major, intracranial, and fatal hemorrhage.
Giugliano RP et al. N Engl J Med 2013; 369: 2093-104
Giugliano RP et al. N Engl J Med 2013; 369: 2093-104
Both dose regimens of edoxaban were non-inferior in the prevention of stroke or systemic embolism, with the higher dose regimen tending to be superior. Both dose regimens of edoxaban significantly reduced a variety of bleeding events, including major, intracranial, and fatal hemorrhage. Both dose regimens of edoxaban reduced CV mortality.
904040_Text.indd 48 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
50
TRA 2 P-TIMI 50 a randomized, double-blind trial of vorapaxar, an oral PAR-1 receptor antagonist, versus placebo in 26,449 patients who had a history of myocardial infarction, ischemic stroke, or peripheral arterial disease.
Morrow DA et al. N Engl J Med 2013; 366:1404-13.
904040_Text.indd 49 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
51
Morrow DA et al. N Engl J Med 2013; 366:1404-13.
Morrow DA et al. N Engl J Med 2013; 366:1404-13.
904040_Text.indd 50 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
52
Morrow DA et al. N Engl J Med 2013; 366:1404-13.
Morrow DA et al. N Engl J Med 2013; 366:1404-13.
904040_Text.indd 51 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
53
Morrow DA et al. N Engl J Med 2013; 366:1404-13. TRA 2P-TIMI 50 investigated whether vorapaxar, a PAR-1 antagonist, reduces ischemic events when administered as long-term secondary prevention in stable patients with atherosclerotic disease. The overall trial showed a significant reduction in cardiovascular death, MI, or stroke (13% RRR, 1.2% ARR) but there was heterogeneity with respect to bleeding risk in that patients with a history of stroke/TIA had a disproportionate risk of bleeding including intracranial hemorrhage. Based on the TRA 2P-TIMI 50 results, vorapaxar was approved for use as long-term secondary prevention in the US for patients with a history of MI or PAD and no history of stroke or TIA.
904040_Text.indd 52 11/7/14 11:48 AM
-
54
RECENTLY COMPLETED TRIALS
Based on the findings in TRA 2P-TIMI 50, if 1000 appropriately selected patients were treated for three years, vorapaxar would prevent 10 myocardial infarctions, 4 strokes, and 4 cardiovascular deaths at the cost of 3 GUSTO severe bleeding events (including 2 intracranial hemorrhages).
904040_Text.indd 53 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
55
ATLAS ACS2 TIMI 51 was a randomized, double-blind trial of low-dose rivaroxaban, an oral factor Xa inhibitor, versus placebo in 15,526 patients with a recent acute coronary syndrome.
Mega JL et al. NEJM 2012; 366: 9-19.
Mega JL et al. NEJM 2012; 366: 9-19.
904040_Text.indd 54 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
56
The ATLAS ACS2 TIMI 51 trial demonstrates that in patients with a recent acute coronary syndrome, rivaroxaban significantly reduced the rate of death from cardiovascular causes, myocardial infarction, or stroke. Rivaroxaban significantly increased the risk of major bleeding and intracranial hemorrhage but not the risk of fatal bleeding.
Mega JL et al. NEJM 2012; 366: 9-19.
The ATLAS ACS2 TIMI 51 trial demonstrates that very low-dose rivaroxaban (2.5mg twice daily) significantly reduced the rate of cardiovascular death, MI, or stroke by 16% (Absolute Risk Reduction [ARR] of 1.8%), the rate of cardiovascular death by 34% (ARR of 1.4%) and all-cause death by 32% (ARR 1.6%).
Mega JL et al. NEJM 2012;366:9-19.
904040_Text.indd 55 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
57
SOLID TIMI 52 is a randomized, double-blind, placebo-controlled trial to assess the efficacy of darapladib, a novel Lp-PLA2 inhibitor, when added to standard of care in high-risk patients stabilized after ACS.
In high-risk patients stabilized after ACS, darapladib therapy did not reduce the primary endpoint of coronary heart disease death, myocardial infarction or urgent coronary revascularization (HR 1.00, 0.91-1.09; p=0.93).
JAMA. 2014;312:1006-1015.
JAMA. 2014;312:1006-1015.
904040_Text.indd 56 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
58
SAVOR TIMI 53 is a randomized, double-blind, placebo-controlled trial to assess the cardiovascular efficacy and safety of saxaglipitin, a DPP-4 inhibitor, when added to standard of care in patients with type 2 diabetes mellitus and either established cardiovascular disease or multiple cardiovascular risk factors.
The primary safety objective of the trial was met, demonstrating that this novel agent known to effectively lowers A1c is not associated with increased cardiovascular ischemic events.
904040_Text.indd 57 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
59
There was, though, an unexpected 27% relative (0.8% absolute) increase in the risk of hospitalization for heart failure in patients treated with saxagliptin that was most evident in those patients with impaired renal function, history of prior heart failure, or elevated levels of natriuretic peptides.
The ELEVATE-TIMI 56 trial was a randomized, double-blind trial of 333 patients with stable cardiovascular disease in which noncarriers of CYP2C19 reduced function alleles were treated with 75 and 150mg of clopidogrel while carriers were treated with 75, 150, 225, and 300mg of clopidogrel daily.
Mega JL et al. JAMA. 2011;306:2221-8.
904040_Text.indd 58 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
60
The ELEVATE-TIMI 56 trial demonstrates that dose escalation of clopidogrel from 75mg to 225mg daily progressively improves platelet inhib
The ELEVATE-TIMI 56 trial demonstrates that tripling the maintenance dose of clopidogrel to 225mg daily in stable heart disease patients carrying 1 reduced function allele achieved similar levels of platelet reactivity as achieved by standard dose clopidogrel in noncarriers.
Mega JL et al. JAMA. 2011;306:2221-8.
Mega JL et al. JAMA. 2011;306:2221-8.
904040_Text.indd 59 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
61
Giugliano RP et al. Lancet. 2012;380:2007-17
Giugliano RP et al. Lancet. 2012;380:2007-17
LAPLACE-TIMI 57 assessed whether 12 weeks of therapy with a novel injectable monoclonal antibody against PCSK9, given on a background of statin therapy, safely lowered LDL cholesterol in hypercholesterolemic subjects.
904040_Text.indd 60 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
62
Giugliano RP et al. Lancet. 2012;380:2007-17
In this phase II dose-ranging study, administration of the PCSK9 inhibitor evolocumab reduced LDL-C at 12 weeks by 42-66% compared to placebo, in a dose-dependent fashion. Several secondary lipid endpoints were significantly decreased with evolocumab, including ApoB. There was no concerning safety signal identified.
904040_Text.indd 61 11/7/14 11:48 AM
-
RECENTLY COMPLETED TRIALS
63
Giugliano RP et al. Lancet. 2012;380:2007-17
904040_Text.indd 62 11/7/14 11:48 AM
-
C Trials
904040_Text.indd 63 11/7/14 11:48 AM
-
904040_Text.indd 64 11/7/14 11:48 AM
-
IV Heparin
Baseline Angio
Patient with Acute ST Elevation MI Patient with Acute ST Elevation MI
-
IV t-PAHeparin, ASA Randomize
Acute MI < 4 hours onsetAcute MI < 4 hours onset
Conservative::Invasive:
TIMI IIBTIMI IIB Protocol Design
Pre-D/C ETT / RVG
Conservative::Cath if +ETT or
ischemia
Primary Endpoint:Death or MI
Follow-up 1 year
Invasive:Cath 18-48 hrs
Revasc if feasible
6 week ETT / RVG
PTCA or CABG to 1 Year
60
80
Invasive15
20
15.2%14.7%
Conservative
Death or MI to 1 Year
72.2%
TIMI IIBTIMI IIBConservative vs. Delayed Invasive
Management Strategy
TIMI Study Group, N Engl J Med 1989; 320:618-27 Williams DO, Circulation 1992; 85:533-42
0 7 14 21 28 35 42 52Weeks
0
20
40
Conservative
0 7 14 21 28 35 42 52Weeks
0
5
10
P=NS
Invasive
*P
-
TIMI IIIATIMI IIIA Primary Results
25
1920
25
30
15
20
25
30
20
25
30Measurable Improvement Substantial Improvement Measurable Worsening
0
5
10
15
tPA Placebo
15
5
0
5
10
15
tPA Placebo
31
0
5
10
15
tPA Placebo
P = 0.25 P = 0.003 P = 0.16
TIMI IIIA Investigators, Circulation 1993; 87:38-52
ASA, IV Heparin, Beta-blockers, Nitrates, Ca++ blockers
RandomizeEarly Invasive:
1473 Patients with Unstable Angina / NQWMI1473 Patients with Unstable Angina / NQWMI
Early
TIMI IIIBTIMI IIIB Protocol Design
ETT 6 weeks
yCath 18-48 h
PTCA/CABG prnConservative:
ST Holter, ETT Thallium Cath/PTCA if +ischemia
1o Endpoint Inv-Cons:Death, MI,Positive ETT - 6 weeks
Follow-up 1 yearCirculation 1994;89:1545-56
2x2 Factorial:2x2 Factorial:tt--PA vs. PlaceboPA vs. Placebo
1o Endpoint t-PA:Death, MI, Rec Isch,+ ETT, Thallium or ST Holter
TIMI IIIBTIMI IIIBtPA vs. Placebo in Non-ST Elevation ACS
Primary Results
54.2 55.5
50
60
70
80
8.8
6 28
10
12
0.55
0.5
0.6
0.7
0.8Composite Endpoint Death or MI ICH
TIMI IIIB Investigators, Circulation 1994; 89:1545-56
0
10
20
30
40
tPA Placebo
6.2
0
2
4
6
tPA Placebo
0.0040
0.1
0.2
0.3
0.4
tPA Placebo
P = NS P = 0.05 P = 0.05
Events at 42dEvents at 42d InvasiveInvasive ConservativeConservative pp valuevalueNo. Pts 740 733Death (%) 2.4 2.5 NSMI (%) 5.1 5.7 NS
TIMI IIIBTIMI IIIBEarly Invasive vs. Conservative Strategy
Primary Results
D/MI/+ETT (%) 16.2 18.1 NS
Rehosp Angina (%) 7.8 14.1
-
22.9
20
25
ST deviation >0.1 mV LBBB Tw change No ECG changes_
TIMI IIITIMI III RREGISTRYEGISTRYAdmission ECG as a prognostic indicator
Risk Stratification
Death or MI
2.6 3.6
11
0.8
6.6
1.63.7
6.8
1.63.7
8.2
In-Hospital 6 Weeks 1 Year0
5
10
15
Stone PH, JAMA 1996; 275:1104-12Cannon CP, J Am Coll Card 1997; 30:133-40
Pt. with AMI < 6 hrs
Heparin, ASA
tPA Combination APSAC
TIMI 4TIMI 4 Protocol Design
p
90 min Angio
18-36 hr AngioMIBI scan
RVG, MIBI scanFollow-up 6 wks, 1 yr
Unsatisfactory Outcome One Year Mortality
0.9
1
of P
ts)
TIMI 4TIMI 4Benefit of front-loaded tPA
Primary Results
52.456.760
80
nts
*P = 0.06
*
Cannon CP, J Am Coll Card 1994; 24:1602-10
0 30 60 90 120150180210240270300330 365Days from Randomization
0.7
0.8
Surv
ival
(% o
t-PAComb.APSAC
*p=0.07t-PA vs. APSAC
p=0.13t-PA vs. Comb.
42
0
20
40
tPA APSAC Comb.
% o
f Pat
ien
Pt. with AMI < 6 hrsPt. with AMI < 6 hrs
4 Ascending Hirudin Doses:
5000 U Bolus,1000 U/h IVAPTT 65 90 secs
TIMI 5TIMI 5 Protocol Design
Heparin Hirudin
ASA, tPA
Day 5-6: RVG, MIBI scan
Doses:0.15 B, 0.05 IV0.1 B, 0.1 IV0.3 B, 0.1 IV0.6 B, 0.2 IV
APTT 65-90 secs
F/U 6 Weeks, 1 yr
90 min angio
18-36 hr angioMIBI Scan
65
5760
80
6.7
6
9
62
4960
80
TIMI 5TIMI 5Hirudin vs. Heparin: Angiographic Results
Primary Results
TIMI 3 Flow at 90 TIMI 3 Flow at 90and 18-36 h Reocclusion
0
20
40
1.6
0
3
0
20
40
HeparinN = 84
HirudinN = 162
HeparinN = 79
HirudinN = 157
HeparinN = 60
HirudinN = 123
Cannon CP, J Am Coll Card 1994; 23:993-03
Pt. with AMI < 6 hrs
3 Ascending Hirudin Doses:
5000 U Bolus,1000 U/h IVAPTT 65 90
TIMI 6TIMI 6 Protocol Design
Heparin Hirudin
ASA SK
Day 5-6: RVG, MIBI scan
Doses:0.15 B, 0.05 IV0.3 B, 0.1 IV0.6 B, 0.2 IV
APTT 65-90 secs ASA, SK
F/U 6 Weeks
904040_Text.indd 68 11/7/14 11:48 AM
-
TIMI 6TIMI 6Heparin vs. Hirudin and stability of aPTT
Adjunctive Therapy
61.572.7 74.1
60
80
100
ith s
tabl
e A
PTT
APTT range 30 seconds*p < 0.001
25
0
20
40
Heparin 0.15/0.05 0.3/0.1 0.6/0.2
% o
f Pat
ient
s w
i
Hirudin Dose
Lee VL, Am J Cardiol 1995; 75:7-13
*
Randomize
Hirulog0.25 mg/kg/h
Patient with Unstable AnginaPatient with Unstable Angina
Hirulog0.5 mg/kg/h
Hirulog1.0 mg/kg/h
Hirulog0.02 mg/kg/h
TIMI 7TIMI 7 Protocol Design
ASA
30 Day Follow-up
TIMI 7TIMI 7Hirulog in Unstable Angina
Primary Results
10
12.5
10
12
14
16
18
% P
atie
nts)
Low Dose (0.02 mg/kg/hr)
Higher Doses (0.25-1.0
P = 0.009
3.2
5.2
0
24
6
810
Hospital Discharge Six Weeks
Dea
th o
r MI (
%
Fuchs J, Circulation 1995;92:727-33
P = 0.008
UA/NQMI < 24 hrsUA/NQMI < 24 hrs
ASAASA
TIMI 8TIMI 8 Protocol Design
Primary EndpointPrimary Endpoint: Death or MI: Death or MI
HirulogHirulog
FollowFollow--up: 30 daysup: 30 days
HeparinHeparin ((aPTT 50aPTT 50--70s)70s)
TIMI 8TIMI 8 Primary Results
9.2
12.3
10
12
14
OR (95 CI): 0.30 (0.06,1.53) 0.33 (0.08,1.30)
P Fisher Exact: 0.16 0.12
Antman E, Am Heart J 2002;143: 229-34
2.94.4
0
2
4
6
8
D/MI through day 14 D/MI through day 30
%
UFHBivalirudin
65 68 65 68
Pt. with AMI Pt. with AMI 80kg1300 u/h >80kg
HIRUDINHIRUDINBolus 0.6 mg/kgBolus 0.6 mg/kgInf 0.2 mg/kg/hInf 0.2 mg/kg/h
Major BleedingMajor Bleeding
96 H Rx96 H Rx
aPTT 60aPTT 60--90 s90 s
904040_Text.indd 69 11/7/14 11:48 AM
-
TIMI 9ATIMI 9A Results
6%
8%
10%
Non-ICH Major4.8
8.4p = .06
Major Bleeding by Treatment Group
Antman E, Circulation 1994;90:1624-30
0%
2%
4%
Heparin Hirudin
ICH4.8
6.6
1.8
2.8
2.0
p = .03
p = NS
N = 335 N = 335
Pt. with AMI < 12 hrsPt. with AMI < 12 hrs
Thrombolytic Therapy (accel tPA or SK)Thrombolytic Therapy (accel tPA or SK)
Protocol DesignTIMI 9BTIMI 9B
Sample Size =3000 pts (Power 90%, a .05, 25% Rx effect)
Death, MI, Death, MI, CHF/ShockCHF/Shock
30 days30 days
HEPARIN HEPARIN Bolus 5000 UBolus 5000 UInf 1000 U/hInf 1000 U/h
HIRUDINHIRUDINBolus 0.1 mg/kgBolus 0.1 mg/kgInf 0.1 mg/kg/h Inf 0.1 mg/kg/h
Major BleedingMajor Bleeding
96 H Rx
aPTT 55-85 s
88101012121414
UNSATISFACTORY OUTCOMEUNSATISFACTORY OUTCOME
%%
12.912.911.911.9
9.79.79.59.5
Primary Results
Hirudin vs. Heparin with tPA for MI
TIMI 9BTIMI 9B
00 55 1010 1515 2020 2525 30300022446688
HIRUDINHIRUDINHEPARINHEPARIN
DEATH + REINFARCTIONDEATH + REINFARCTION%%
PtsPts
Days post randomizationDays post randomization
p=NSp=NS
9 59 5
Antman E, Circulation 1996; 94:911-21
All Consecutive Patients with Acute STEMI/ LBBB enrolled at
20 Hospitals in US and CanadaIn 1994 N=840
TIMI 9TIMI 9 RegistryRegistry Protocol Design
Fibrinolysisn=505(60%)
Primary PCIn=76(9%)
No Reperfusionn=276(31%)
Cannon CP, Crit Path Cardiol 2002; 1:44-52
Use of reperfusion Rx in Patients presenting < 12 hours:65% 10% 25%
7 610.5
18.9
12
16
20
%
%3 way p
-
TIMI 10ATIMI 10ATIMI Flow Grade at 90 Minutes
Primary Results
60 64
80 40 66
42
2924
22
40
60
80
100
(%)
TIMI 3 TIMI 2
60
40
17
29
59 576
0
20
40
5 mg 7.5 mg 10 mg 15 mg 20 mg 30 mg 40 mg 50 mg
Patie
nts
Cannon CP, Circulation 1997; 95:351-56
TNK-tPA Dose
Randomize
TNK-tPA 30mg
Patient with Acute ST Elevation MI < 12 hours Patient with Acute ST Elevation MI < 12 hours
TNK-tPA 40mg
TNK-tPA 50mg*
t-PA100 mg
TIMI 10BTIMI 10B Protocol Design
ASA, IV Heparin
30 Day Follow-up
Angio 60, 75, 90 Mins
*Stopped early*Stopped earlyReplaced with 40 mgReplaced with 40 mg
TIMI 10BTIMI 10BTIMI Flow Grade at 90 Minutes
Primary Results
66
1922 16
22
60
80
100 TIMI 3 TIMI 2
77%77% 79%79%88%88%
82%82%
6355
63 66
0
20
40
60
tPA TNK 30 mg TNK 40 mg TNK 50 mg
Cannon CP, Circulation 1998; 98:2805-14
N = 311 304 146 76
Randomize
TNK-tPA 30
Patient with Acute ST Elevation MI < 12 hours Patient with Acute ST Elevation MI < 12 hours
TNK-tPA 40
TNK-tPA 50 *
ASSENT I (TIMI 10C)ASSENT I (TIMI 10C) Protocol Design
ASA, IV Heparin
30 Day Follow-up
30mg 40mg 50mg*
*Stopped early*Stopped earlyReplaced with 40 mgReplaced with 40 mg
1.5
1 0
1.5
ents
30 mg TNK, n=1,705 40 mg TNK, n=1,457 50 mg TNK, n=73
Primary Results
Incidence of Stroke at 30 Days
ASSENT I (TIMI 10C)ASSENT I (TIMI 10C)
0.5
1.0
0 0 0
0.94
0.62
Total Stroke ICH Ischemic Stroke
% o
f Pat
ie
Van de Werf F, Am Heart J 1999; 137:786-91
2.8
2.11.82.0
3.0
atie
nts
Pre Post
p = 0.046
p = 0.4
p = 0.01
ICH Pre/post Reduction in Heparin
Adjunctive TherapyTIMI 10 B /ASSENT I (TIMI 10C)TIMI 10 B /ASSENT I (TIMI 10C)
0.80.71.1
0.0
1.0
TNK 30 tPA Either
% o
f Pa p
Giugliano RP, Am Heart J 2001; 141:742-50
904040_Text.indd 71 11/7/14 11:48 AM
-
TIMI 11A Protocol Design
Dose 1N=320
IV BolusIV Bolus Wgt AdjWgt Adj Fixed DoseFixed Dose
30 mg1.25 mg/kg
Q 12 h (2-8d)< 65 kg > 65 kg
40 60
Hospital Phase Home RxDose-ranging trial of enoxaparin for patients with UA/NQMI
> 65 kgDose 2 N=309
N 320
30 mg
( )
1.0 mg/kgQ 12 h (2-8d)
40 mg 60 mgQ12 h
40 mg 60 mgQ12 h
Total Rx Period = 14 days
< 65 kg
InstrumentedSpontaneous
6.5%6
8
10
%
Primary Results
Incidence of Major Hemorrhage thru 14 days
TIMI 11A
N=3211.25 mg/kg
1.9%
T3BHep + Plac
N=735
3.2%
N=3091.0 mg/kg
0
2
4
Dose Tier 1 Dose Tier 2
%
TIMI 11A Investigators, J Am Coll Card 1997; 29:1474-82
Pt. with UA/NQMI < 24 h
Acute = Day 8UFH iv > 72 hUFH iv > 72 h
ASA
ENOX ivENOX iv--b,scb,sc
Protocol DesignTIMI 11B
Death, MI, Severe Rec Isch Requiring Urgent Revasc
Major Bleeding Serious AEs
Placebo scPlacebo sc ENOX scENOX scChronic = Day 43
12121414161618182020
UFHUFHENOXENOX 16.7 %16.7 %
14.2 %14.2 %%
14.5 %14.5 %
Primary Results
Death/MI/Urgent Revascularization at 14 Days
TIMI 11B
22446688
1010
00 22 44 66 88 1010 1212 1414
P=0.029RRR 15 %
Days
12.4 %12.4 %
P=0.048RRR 15 %
Antman E, Circulation 1999; 100:1593-01
Primary Results
Death/MI/Urgent Revascularization at 72 hours
TIMI 11B
56789
% P
ts
7.3 %
5.5 %
UFHENOX
Antman E, Circulation 1999; 100:1593-01
01234
0 8 16 24 32 40 48 56 64 72
%
Hours from Randomization
5.5 %RRR 23.8%
P=0.029Log rank
Sibrafiban3 mg bid
Sibrafiban5 mg qd
Sibrafiban5 mg bid
Sibrafiban10 mg qd
Protocol DesignTIMI 12TIMI 12Patients 1-7 days post-ACS
15 pts/dose
1o End Point:% Inhibition of ADP-induced Plt aggregation
Plt. Aggreg. / PK samples0, 2, 4, 6, 9, 24, 36 h
Follow-up visit Day 7Phone Contact Day 14, 21
Additional Doses:7 mg bid15 mg qd10 mg bid
Plt. Aggreg. / PK samples0, 2, 4, 6, 9, 24 h
Cannon CP, Circulation 1998; 97:340-49
904040_Text.indd 72 11/7/14 11:48 AM
-
3 mg bid3 mg bid5 mg bid5 mg bid7 mg bid7 mg bid10 mg bid10 mg bid
5050
7575
100100
ibiti
on (A
DP)
ibiti
on (A
DP)
D1D1 D28D28
Primary ResultsTIMI 12TIMI 12Inhibition of Platelet Aggregation by Dose Grp
00
2525
5050
00 66 1212 2424
Mea
n %
inh
Mea
n %
inh
00 66 1212 2424 3636Hours postHours post--dosedose
Cannon CP, Circulation 1998; 97:340-49
ST , lytic eligible, < 12 h
Group I Group II Group III Group IV
No Abciximab Abx: bolus 0.25 mg/kg inf 0.125 g/kg/min x 12 h
Protocol DesignTIMI 14TIMI 14
tPA < 100 mg dose tPA dose SK No lytic
Angio (90 min) , In Hospital Events, 30 day F/U
STD Heparin(70 U/kg ; 15 U/kg/h)
Low Dose Heparin(60 U/kg ; 7 U/kg/h)
vsGroup V
rPA 10+10UGroup VI
dose rPAvs
58 635749
6274
60
80
100
tient
s
60 Min 90 Min
Primary Results
Speed and Extent of Thrombolysis: TIMI 3 Flow
tPAtPA tPA + AbciximabtPA + Abciximab 2 Trend, p2 Trend, p < 0.002< 0.002
TIMI 14TIMI 14
45 4049
0
20
40
100 mg bolus bolus + 30 mininfusion
bolus + 60 mininfusion
% o
f Pat
Antman E, Circulation 1999; 99:2720-32
Normal Normal Flow Flow
cTFC < 28cTFC < 28
tPA 100 mg 36tPA 100 mg 36
tPA 50 (15b/35inf) + Abx tPA 50 (15b/35inf) + Abx 2828
SK + Abx 45SK + Abx 45
cTFCcTFCMedianMedian
P=0.005P=0.005
ents
ents 6060
707080809090
100100
Efficacy Results
TIMI Frame Count at 90 Min
TIMI 14TIMI 14
Abx 100Abx 100
% P
atie
% P
atie
010102020303040405050
0Corrected TIMI Frame Count
20 40 60 80 100
Antman E, Circulation 1999; 99:2720-32
100
120 0.80 ug/kg/min : N=130.60 ug/kg/min : N=120.50 ug/kg/min : N=200.40 ug/kg/min : N=34
Protocol Design/Primary ResultsTIMI 15ATIMI 15A
Mean Inhibition of Platelet Aggregation
various Doses
ACS within 0-48h
Safety and pharmacokinetics of various dosesof the IV GP IIb/IIIa inhibitor RPR 109891
0
20
40
60
80
1-4h 24h 48-96h Pre-stop 2-4h post 8-16hpost
17-24hpost
% IP
A
0.20 ug/kg/min : N=10
Giugliano RP, Am Heart J 2000; 140:81-93
various Doses
PK/PD at 0, 20m, 1-4hQD, pre-stop, 2-4h &
8-24h post stop
Clinical f/u at 14d
80
90
100
egat
ion placebo (n=24)
100/0.5 (n=52)100/0.4 (n=23)175 BID ( 14)
Percent Platelet Inhibition
TIMI 15BTIMI 15B
IV then oral
ACS within 0-72h
IV then oral
Safety and pharmacokinetics of the GP IIb/IIIa inhibitor RPR 109891 given IV and orally
Protocol Design/Primary Results
-10
0
10
20
30
40
50
60
70
80
1-3h end IV 2-4hpost
pre-dose
4h post 7-8hpost
pre-dose
% In
hibi
bitio
n of
Pla
tele
t Agg
re 175 BID (n=14)200 BID (n=12)150 TID (n=9)250 BID (n=9)300 BID (n=10)200 TID (n=5)
IV Infusion Day 7, Oral Day 28, Oral
RPR 109891(3 doses)
Treatment for 4 wks
IV then oralplacebo
Giugliano RP, Am Heart J 2000; 140:81-93
904040_Text.indd 73 11/7/14 11:48 AM
-
ASA 150-162 mg daily
Patient with Unstable Coronary Syndrome Rehosp,or Stroke
1520
r Per
cent
age
Composite Endpoint
34
5r P
erce
ntag
e
Mortality
ResultsOPUS OPUS -- TIMI 16TIMI 16
Time (days)0 50 100 150 200 250 300
05
101
Kapl
an-M
eie
Cannon CP, Circulation 2000; 102:149-56
Time (days)
0 50 100 150 200 250 300
01
23
Kapl
an-M
eie
placebo50-30mg50-50mg
placebo50-30mg50-50mg
ST Elev MI ST Elev MI
-
24.225
30
%)
CONS INV
Troponin T Substudy
Death, MI, Rehosp ACS at 6 Months
OR=0.55*p
-
Angiographic &ECG Results at 60 Minutes
62
5460
80
100Tenecteplase monotherapy
Eptifibatide (180/2/180) + 50% TNK (Dose Finding andDose Confirmation)
INTEGRITI INTEGRITI TIMI 20TIMI 20
40
13
4549
24
5452
0
20
40
% pts
N: 106 160
TFG 3 TrifectaComplete ST Res
TMPG 3
45 8153 89107 160
Giugliano RP, J Am Coll Cardiol 2003; 41:1251-60
Protocol Design
High Risk ACS (ST High Risk ACS (ST // or + Marker) Receiving Tirofiban or + Marker) Receiving Tirofiban
A Phase
If li i ll t bl d t l i k
Death, MI, refractory ischemiaat 7 days
Enoxaparin UF Heparin
A2Z A2Z TIMI 21TIMI 21
Z Phase
If clinically stable and not low-risk
Aggressive simvastatin Standard therapy
40 mg/day x 30 d 80 mg day thereafter
Placebo and diet x 4 monthssimvastatin 20 mg/day thereafter
1 year follow-up: CV death, MI, rehospitalization for ACS
Blazing JA, Am Heart J 2001; 142:211-17
Primary Endpoint Primary Endpoint -- Death, MI and Refractory IschemiaDeath, MI and Refractory Ischemia
Results A Phase
UFHEnoxaparin
s(%
)
8.4% (169 events)
9.4% (184 events)
8
10
12
A2Z A2Z TIMI 21TIMI 21
Blazing JA, JAMA 2004; 292:55-64Days From Randomization
Even
t Rat
es
7 Day
% ( )
HR 0.89 (0.72,1.09)prespecified non-inferiority margin met
0 10 20 300
2
4
6
Results Z Phase
15
20
e (%
)
Placebo/Simva 20Rate = 16.7%
HR 0.89, CI 0.76 - 1.04p = 0.14
Primary Endpoint Composite of Death, MI and Refractory IschemiaPrimary Endpoint Composite of Death, MI and Refractory Ischemia
A2Z A2Z TIMI 21TIMI 21
0 1 4 8 12 16 20 24Month from Randomization
0
5
10
KM
Rat
e
Simvastatin 40/80Rate = 14.4%
De Lemos J, JAMA 2004; 292:1307-16
PROVE IT PROVE IT -- TIMI 22TIMI 22 Protocol DesignPatients stabilized post ACS
-
Lipid Results
DEATH, NON-FATAL MI, OR URGENT REVASCULARIZATION
15
20
Pravastatin 40 mg16.7%
with
eve
nts
PROVE IT PROVE IT -- TIMI 22TIMI 22
Months of Follow-up0 6 12 18 24 30
0
5
10
RRR 25% P=0.0004
Atorvastatin 80 mg12.9%
Perc
ent p
atie
nts
Cannon CP, N Engl J Med 2004; 350:1495-04
Lipid Results
with
eve
nts
Pravastatin 40 mgH d R ti 0 67
4
5
DEATH, NON-FATAL MI, OR URGENT REVASCULARIZATIONAT 30 DAYS
PROVE IT PROVE IT -- TIMI 22TIMI 22
Days of Follow-up
Perc
ent p
atie
nts Pravastatin 40 mg
Atorvastatin 80 mg
Hazard Ratio =0.67p = 0.04
0 5 10 15 20 25 30
0
1
2
3
Cannon CP, N Engl J Med 2004; 350:1495-04
Lipid Results
Median C-reactive protein (hsCRP) levels by treatment
100
g/L)
Pravastatin 40mg (n=1873)Atorvastatin 80mg (n=1872)p=0.6
PROVE IT PROVE IT -- TIMI 22TIMI 22
Ridker PM, J Am Coll Cardiol 2005; 45:1644-48
1
10
Randomization 30 days 120 days Study end
Med
ian
hsC
RP
(mg
p
-
Results
50 51
0
20
40
60
80
100
UFH ENOX
75 78
140 275
60
80
100 FULL Dose TNK HALF Dose TNK+ Abx80
70 77 78
TIMI 2 Flow
TIMI 2 and 3 Flow at 60 minutes
ENTIRE ENTIRE TIMI 23TIMI 23
52 50 48 52
0
20
40
60
UFH ENOX UFH ENOXN = 73 141 67 134
% P
ts
Angio Evaluable Patients
TIMI 3 Flow
TIMI 2 Flow
Antman EM, Circulation 2002; 105:1642-49
ts
Results
3.1
8.2
3.1
1.8
0
4
8
12
UFH ENOX
11.3
4.9
P=0.01
15
20 FULL Dose TNK15.9 P=0.005
HALF Dose TNK + Abx
P=0.002
Death and MI at 30 days
ENTIRE ENTIRE TIMI 23TIMI 23
% P
All Treated Population
2.5 2.6 3.7
12.2
3.93.7
1.81.9
0
5
10
UFH ENOX UFH ENOX
P=0.0034.4
DeathMI
6.55.5
N = 82 160 77 164
Antman EM, Circulation 2002; 105:1642-49
ST Elevation ST Elevation MIMI < 6 h< 6 h
TNK-tPA 0.53 mg/kg Tirofiban bolus + infusion(10 to 15 g/kg) 0.15 g/kg/min
ASA
Protocol DesignFASTER FASTER -- TIMI 24TIMI 24
STD Heparin
Primary Endpoint Part A (Dose Finding): TIMI 3 Flow at 60 minPrimary Endpoint Part B (Dose Confirmation): ST segment resolution at 60 min
Low Dose Heparin
TNK-tPA dose
Ohman EM. International Symposium on Thrombolysis and Interventional Therapy in AMI. 2002
6.6 6
10
15 N=106 243 302
Urgent Revasc
10.4%* 11.9%* 11.9%*
Results
30 d Death, MI, Urgent Revasc
22 27 23
60
70
80
90
TIMI 3 TIMI 2
TIMI Flow at 60 min
FASTER FASTER -- TIMI 24TIMI 24
% P
ts1.9
2.9 3.6
4.74.9
4.7
5.7
0
5
10
TNK 50% TNK +Tirof
All TNK+Tirof
Death
MI
*Corrected for multiple events
58 57 59
0
10
20
30
40
50
60
TNK 50% TNK +Tirof
All TNK +Tirof
% P
ts
Ohman EM, Am Hear J 2005; 150:79-88
STEMI < 6 hLytic eligible
Lytic choice by MD(TNK, tPA, rPA, SK)
ENOX
Double-blind, double-dummy
ASA
UFH
EXTRACT EXTRACT TIMI 25TIMI 25Protocol Design
ENOX< 75 y: 30 mg IV bolus
SC 1.0 mg / kg q 12 h (Hosp DC)75 y: No bolus
SC 0.75 mg / kg q 12 h (Hosp DC)CrCl < 30: 1.0 mg / kg q 24 h
Day 301 Efficacy Endpoint: Death or Nonfatal MI
1 Safety Endpoint: TIMI Major Hemorrhage
UFH60 U / kg bolus (4000 U)
Inf 12 U / kg / h (1000 U / h)Duration: at least 48 hContd at MD discretion
Antman EM, Am Heart J 2005; 149:217-26
12.09.9
UFH UFH
ENOX
14.511.7
Primary Results
Primary Endpoint:Death or non-fatal re-MI by 30 days
Main Secondary Endpoint:Death, non-fatal re-MI,
urgent revascularization by 30 days
EXTRACT EXTRACT TIMI 25TIMI 25
ENOX ENOX
Days Days
%% RR = 0.83p = 0.000003
RR = 0.81p = 0.000001
Antman EM, N Engl J Med 2006; 354:1477-88
904040_Text.indd 78 11/7/14 11:48 AM
-
1123
1721
RRR (%)
206
SEX MaleFemale
1816All InteractionAll InteractionTestsTests
P = NSP = NS
1.52.3
1.93 5
ARD
2.01.5
1.92.9
AGE (years) < 75> 75
INFARCT AnteriorLOCATIONOther
DIABETES No DMDM
EXTRACT EXTRACT TIMI 25TIMI 25Results
0.5 1 2ENOX Better UFH BetterRelative Risk
21
1720
1318
2312
17P < 0.0001
3.5
1.93.5
2.1
1.62.2
2.61.5
DM
PRIOR MI No Prior MIPrior MI
FIBRINOLYTIC StreptokinaseFibrin-Specific
TIME TO RX < Median> Median
OVERALL 20,479
Antman EM, N Engl J Med 2006; 354:1477-88
Bleeding Endpoints (TIMI) 30 Days
3
4
5 UFHUFHENOXENOX
ents
ARD 0.7%RR 1.53
P 50%, Target in SVG or Art Conduit, EF < 30% or NYHA CHF II Bleeding Risks, Oral A/C, thienopyridine < 5 d, Rx with PPI
Protocol Design
Elective or Urgent PCI with intent to stent
ASA 325 mg
Parallel Randomization
JUMBO JUMBO TIMI 26TIMI 26
Maintenance Rx for 30 days
11oo endpoint:endpoint: Significant Bleeding (non CABG) bleeding through 30 daysSignificant Bleeding (non CABG) bleeding through 30 days
22oo endpoints:endpoints: Major bleeding (non CABG) through 30 daysMajor bleeding (non CABG) through 30 daysCV MACE through 30 daysCV MACE through 30 days
Significant bleeding + CV MACE through 30 daysSignificant bleeding + CV MACE through 30 days
Double-blindCS 747Low dose
(Load/Maintenance)
CS 747Low dose
(Load/Maintenance)
ClopidigrelLoading Dose 300 mg
Maint. Dose 75 mg
CS 747Intermed dose
(Load/Maintenance)
Results
2 0%3.0%
4.0%
5.0%
P= NSP = 0.77Dose RangingClop. vs Prasugrel
10 EP: Significant Non-CABG Bleeding 30 D
CLOPIDOGREL
Estim
ate
8%
10%
Time to MACEDeath, MI, CTVT, Stroke, and Recurrent Ischemia
JUMBO JUMBO TIMI 26TIMI 26
R/N
1.2%
2.0%1.5%1.7% 1.6%
0.0%
1.0%
2.0%
Clop Pras 40/7.5 60/10 60/15
3/254 11/650 3/199 4/200 4/251R/N
Prasugrel LD/MDTreatment Group
PRASUGREL
Kap
lan-
Mei
er E
0%
2%
4%
6%
Time since PCI (days)0 5 10 15 20 25 30 35
p = 0.26
Wiviott SD, Circulation 2005;111:3366-73
PROXIMATE PROXIMATE --TIMI 27TIMI 27 Protocol Design
cH36 BolusDose # 1
n = 7
Stable CADReceiving ASA
(n = 28)
f f
Membrane
Factor VIIaFactor VIIa
Factor Xanti-TF
PROXPROXimal imal IInhibition of coagulation using a nhibition of coagulation using a MMonclonal onclonal AAntibody to ntibody to TTissuissuee factor (Sunol cH36) factor (Sunol cH36) -- TIMI 27TIMI 27
Measured at multiple time points: cH36 levels Factor Xa activity Hgb/Hct PT/PTT/fibrinogen Platelet count Serum chemistries Human anti-chimeric ab
If no safety concerns, proceed to higher dose cH36 Bolus
Dose # 2n = 7
cH36 BolusDose # 3
n = 7
cH36 BolusDose # 4
n = 7
904040_Text.indd 79 11/7/14 11:48 AM
-
ResultsResults
Enrolled, NEnrolled, NMajor bleeding (pts)Major bleeding (pts)
0.0380
0.0640
0.0840
0.1070
0.3030
Dose Sunol cH36
PROXIMATE PROXIMATE --TIMI 27TIMI 27
Minor bleeding (pts)Minor bleeding (pts)SpontaneousSpontaneousProvokedProvokedAny minor*Any minor*
(Exact CI %)
1 (13)2 (25)2 (25)
(3, 65%)
2 (50)1 (25)3 (75)
(19, 99%)
2 (50)0
2 (50)(7, 93%)
6 (86)1 (14)6 (86)
(44,100%)
3 (100)1 (33)3 (100)
(29,100%)
*Provoked bleeds were those that occurred at the site of IV insertion or as the result of minor trauma; all others were classified as spontaneous.
Morrow DA, J Am Coll Cardiol 2005; 26:682-88
Fibrinolytic, ASA, Heparinrandomize
Double-blind, randomized, placebo-controlled trial in3491 patients, age 18-75 yrs with STEMI < 12 hours
CLARITY CLARITY TIMI 28TIMI 28Protocol Design
Clopidogrel300 mg + 75 mg qd
Coronary Angiogram(2-8 days)
Primary endpoint:Occludedartery (TIMI Flow Grade 0/1)or D/MI by timeof angio
Placebo StudyDrug
30-day clinical follow-up
Open-labelclopidogrelper MD in
both groups
Sabatine MS, Am Heart J 2005; 149:227-33
Occluded Artery (or D/MI thru Angio/HD)
15.0
21.7
20
25
eath
/MI
(%)
P=0 00000036P=0 00000036
Odds Ratio 0.64(95% CI 0.53-0.76)
Odds Ratio 0.64(95% CI 0.53-0.76)
36%Odds Reduction
36%Odds Reduction