The Digestive System
-
Upload
api-26587879 -
Category
Documents
-
view
725 -
download
0
Transcript of The Digestive System

The Digestive SystemB. Pimentel, M.D.
University of Makati College of Nursing

Overview
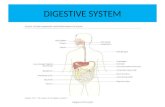
There are 2 major groups of organs in the digestive system:
Alimentary Canal - Organs thru which food actually passes (in order they are the: oral cavity, pharynx, esophagus, stomach, small intestine, and large intestine).
Accessory Organs - They assist in digestion, but no food actually passes through them. Includes the teeth, tongue, salivary glands, pancreas, liver, and gallbladder.

Overview

Functions
Ingestion Mastication Propulsion Mixing Secretion Digestion Absorption Elimination

The Abdominal Cavity
The majority of digestive organs are located Peritoneum
Visceral peritoneum Parietal peritoneum Peritoneal cavity Mesenteries
Retroperitonium Duodenum Pancreas Colon

The Abdominal Cavity

Histology
1. Mucosa - innermost tunic, consists of three layers. Mucosa epithelium, stratified squamous
epithelium Lamina propria, loose connective tissue. Muscularis mucosae, outer thin smooth
muscle.

Histology
2. Submucosa – thick connective tissue layer containing nerves blood vessels and small glands.
3. Muscularis – inner layer of circular smooth muscle and an outer layer of longitudinal smooth muscle. Exceptions superior esophagus has striated
muscle, and the stomach has three muscular layers.
4. Serosa or Adventitia – connective tissue.

Histology

Histology

Histology

The Oral Cavity
Boundaries Boundaries Anteriorly by the lipsAnteriorly by the lips Laterally by the cheeksLaterally by the cheeks Superiorly by the hard Superiorly by the hard
and soft palatesand soft palates Inferiorly by the tongueInferiorly by the tongue
Epithelial lining: non-Epithelial lining: non-keratinized stratified keratinized stratified squamous epitheliumsquamous epithelium

The Oral Cavity
STRUCTURE FUNCTION
Lips Mastication, speech, & entrance
Frenula Mucosal folds attach upper lip to alveolar process of the maxilla, and from the alveolar process of the mandible to lower lip.
Cheeks Mastication ,speech, & facial expression

Palate (hard & soft) Mastication, soft palate prevents food from entering nasal cavity.
Tongue Movement of food in mouth for mastication, swallowing, taste, speech.
Intrinsic muscles Flattening and elevating tongue for swallowing.
The Oral Cavity

Extrinsic muscles Protrude and retract, side to side, and shape change.
Teeth Mastication and speech
Incisors Cutting or nipping off food
Canines Tear and pierce
Premolars Grinding and crushing
Molars Grinding and crushing
The Oral Cavity

The Oral Cavity

The Oral Cavity

Salivary Glands
Structure Location
Parotid glands Just anterior to the ear, bilaterally.
Submandibular glands Inferior border of the posterior mandible
Sublingual glands Immediately below the mucus membrane in the floor of the mouth

Salivary Glands

Salivary Glands
Saliva Secretion rate 1 to 1.5L/day Salivary amylase – serous saliva breaks down apart
glucose molecules in starch and other polysaccharides into disaccharides.
Prevents bacterial infection together with lysozyme Mucin – proteoglycan that gives saliva a lubricating
quality. Stimulated primarily by the parasympathetics and less by
sympathetics.

Esophagus (Gross Anatomy)
Approx. 25 cm.
Between pharynx and stomach
Located in the mediastinum anterior to vertebrae and posterior to trachea.

Esophagus (Gross Anatomy)
Esophageal hiatus – opening in diaphragm and ends at stomach.
Upper esophageal and Lower esophageal sphincter – regulate the movement of materials into and out of esophagus.


Esophagus (Histology)
Mucosa stratified squamous epithelium with mucous glands that secret a thick lubricating mucus.
4 tunics: mucosa, submucosa, muscularis, and adventitia.

Deglutition

Deglutition

Stomach (Gross Anatomy)
Enlarged segment in left superior part of abdomen.
Gastroesophageal opening (cardiac) – opening of stomach from esophagus.
Cardiac region – located around the cardiac opening where food enters from the esophagus

Stomach (Gross Anatomy)
Fundus – left and superior to the cardiac region.
Body – largest part of stomach curves to the right forming the greater and lesser curvature. Greater curvature
lateral surface of the stomach anchors the greater omentum
Lesser Omentum medial surface anchors the lesser omentum

Stomach (Gross Anatomy)

Stomach (Gross Anatomy)
Pyloric region – region where body narrows
Pyloric opening - joins to the small intestine.
Pyloric sphincter – thick smooth muscle
surrounding the pyloric opening.

Stomach (Gross Anatomy)

Stomach (Histology)
Serosa – visceral peritoneum, outer most layer.
Muscularis – three layers,
longitudinal layer, circular layer, and an inner oblique layer.
Rugae – large folds of submucosa and mucosa, allows stomach to stretch.

Stomach (Histology)
Stomach is lined with simple columnar cells, with tube like gastric pits, which are openings for the gastric glands.
Surface mucous cells – produce mucus on the surface and lines the gastric pit.

Stomach (Histology)

Stomach (Histology)
Gastric gland cells Mucous neck cells – produce mucus.
Parietal cells – produce hydrochloric acid and intrinsic factor.
Chief cells – produce pepsinogen.
Endocrine cells –produce regulatory hormones.

Stomach Secretions
Chyme – food and stomach secretions mixed
SECRETION SOURCE FUNCTION
Mucus Surface and neck mucus cells .
Lubricates, protects
Intrinsic factor Parietal cells in gastric glands of the pyloric region.
Binds with and makes more readily absorbed in the ilium VITAMIN B12
Hydrochloric acid Parietal cells Low pH bactericidal, denature proteins, provides proper pH for pepsin.
Pepsinogen Chief cells Converts to pepsin, catalyzes the cleavage of peptide bonds in proteins.

Phase of Secretion

Phase of Secretion

Phase of Secretion

Functions of Gastrointestinal Hormones
Site of Production
Method of Stimulation
Secretory Effects Motility Effects
Gastrin
Stomach & duodenum
Distention, partially digested proteins, autonomic stim., alcohol & caffeine
Increases gastric secretions
Increased gastric emptying by increasing motility and relaxing pyloric sphincter.

Functions of Gastrointestinal Hormones
Secretin
Duodenum Acidity of chyme
Inhibits gastric secretions, stimulates pancreatic secretions, increases the rate of bile and increases intestinal secretions; mucus secretion
Decreases gastric motility
Site of Production
Method of Stimulation
Secretory EffectsMotility Effects

Functions of Gastrointestinal Hormones
Cholycystokinin
IntestinesFatty acids and other lipids
Slightly inhibits gastric secretions, stimulates pancreatic secretions, contraction of gall bladder, relaxation of hepatopancreatic ampular sphincter.
Decreases gastric motility
Site of Production
Method of Stimulation
Secretory EffectsMotility Effects

Gastric Inhibitory Polypeptide
Duodenum & Jejunum
Fatty acids and other lipids
Inhibits gastric secretions
Decreases gastric motility
Site of Production
Method of Stimulation
Secretory EffectsMotility Effects

Gastric Movements
Mixing of Stomach Contents
Gentle mixing waves which are peristalsis like contractions proceed from the body toward the pyloric sphincter. 80%
Peristaltic waves occur less frequently, significantly more powerful, force chyme near the periphery of the stomach toward the pyloric sphincter. 20%

Gastric Movements
Stomach Emptying
Fluids remain in the stomach approx. 1.5 to 2.5 hours, food approx. 3 to 4 hours.
Each peristaltic contraction is strong enough to force a small amount of chyme through the pyloric sphincter and into the duodenum, this is referred to as Pyloric Pump.

Gastric Movements
Regulation of stomach emptyingRegulation of stomach emptying
Hormonal – GastrinHormonal – Gastrin
CNS - distention of stomach wall and local CNS - distention of stomach wall and local reflexesreflexes
All promote increased in stomach emptying.All promote increased in stomach emptying.

Small Intestines
Consists of three parts: Duodenum Jejunum ilium
Length approx. 4.6 to 9 meters (14 to 29 feet). Site of greatest amount of digestion and
absorption. 8 to 8.5 liters of water enter the small intestine per
day.

Small Intestines (Duodenum)
Begins with a short superior end, which is where it exits the pylorus of the stomach, and ends in a sharp bend, where it joins the jejunum.
Major duodenal papilla & lesser duodenal papilla - two small mounds 2/3 of the down the descending part. At the major papilla the common bile duct and pancreatic duct join to form the hepatopancreatic ampular sphincter which empties into the duodenum.

Small Intestines (Duodenum)

Small Intestines (Duodenum)
Hepatopancreatic sphincter - regulates the opening of the ampular.
Internal surface has modifications which increase surface area about 600 fold.
Circular folds - mucosa and submucosa form a series of folds.
Villi- tiny fingerlike projections of the mucosa, simple columnar epithelium, contains blood capillary network and lacteals.

Small Intestines (Duodenum)

Small Intestines (Duodenum)

Small Intestines (Duodenum)
Microvilli - most of the cells of the surface of the villi have these numerous cytoplasmic projections to further increase surface area.
Brush border - the combined microvilli on the entire epithelial surface.

Small Intestines (Duodenum)

Small Intestines (Duodenum)

Small Intestines (Duodenum)
Cells Function
Absorptive Microvilli, produce digestive enzymes, absorb digested food
Goblet Produce a protective mucus
Granular cells Protect the intestinal epithelium from bacteria
Endocrine Produce regulatory hormones

Small Intestines (Jejunum & Ileum)
Similar in structure to duodenum, EXCEPT1. Gradual decrease in the size of the lumen.
2. Decrease in thickness of the intestinal wall
3. Number of circular folds decrease
4. Decrease in number of microvilli

Small Intestines (Jejunum & Ileum)
The duodenum and jejunum are major sites of nutrient absorption.
Lymph nodes called Peyer’s Patches are numerous in the mucosa and submucosa of the ileum.

Small Intestines (Jejunum & Ileum)

Small Intestines (Jejunum & Ileum)
Ileocecal junction – junction between the ileum and the large intestine.
Ileocecal sphincter – ring of smooth muscle.
Ileocecal valve – one way flow.

Small Intestines (Jejunum & Ileum)
Duodenal glands, intestinal glands, and goblet cells secrete large amounts of mucus.
Mucus provides most of the wall with protection from the acidic chyme, and digestive enzymes.

Small Intestines (Jejunum & Ileum)
Secretin & Cholycystokinin are released from the intestinal mucosa and stimulate pancreatic and hepatic secretions.
Enzymes of the intestinal mucosa are bound to the membranes of the absorptive cell microvilli

Small Intestines (Jejunum & Ileum)
1. Disaccharidase – breaks down disaccharides to monosaccharides.
2. Peptidase – hydrolyze the peptide bonds of amino acid chains.
3. Nucleases – break down nucleic acids.

Movements of the Small Intestine
Mixing and propulsion of chyme are the primary mechanical events.
Mechanical movement occurs due to segmental or peristaltic contractions of the smooth muscle wall, only propagated small distances.

Movements of the Small Intestine
Segmental contractions – mix intestinal contents.
Peristaltic contractions – propel the intestinal contents along the entire length of the intestine.
Wave of contraction can begin in the stomach.
Rate of movement 1cm/min

Movements of the Small Intestine
Regulation1. Distention of intestinal wall
2. Hypertonic or hypotonic solutions
3. pH of contents

Large Intestine
Extends from the ileocecal junction to the anus.Extends from the ileocecal junction to the anus. Consists of:Consists of:
CecumCecum ColonColon RectumRectum Anal canalAnal canal

Large Intestine

Large Intestine (Cecum)
Proximal end of the large intestine.
Extends approx. 6cm. Inferiorly past the ileocecal junction to form a blind sac.
Vermis Appendix – a small blind tube extending approx. 9cm from the blind sac. Contains many lymph nodes.

Large Intestine (Cecum)

Large Intestine (Colon)
Consists of four parts: Ascending colon Transverse colon Descending colon Sigmoid colon

Large Intestine (Colon)
The ascending colon The ascending colon travels up the right travels up the right side of the abdominal side of the abdominal cavity and turns cavity and turns medially (the right medially (the right colic flexure or colic flexure or hepatic flexure) and hepatic flexure) and travels across the travels across the abdominal cavity as abdominal cavity as the transverse colon. the transverse colon.

Large Intestine (Colon)
At the spleen the transverse colon turns downward (the left colic flexure or splenic flexure) and descends on the left side as the descending colon

Large Intestine (Colon)
Inferiorly, the decending colon enters the pelvis where it becomes the sigmoid colon

Large Intestine (Colon)
The last segment of the is the anal canal which begins where the rectum penetrates the muscles of the pelvic floor

Large Intestine (Colon)
The external opening is the anus. Controlling this exit are the internal anal sphincter (smooth muscle and involuntary) and the external anal sphincter (skeletal muscle and voluntary (to a point)).

Large Intestine (Colon)
The circular muscular layer of the colon is complete, but the longitudinal layer of muscle is incomplete
The mucosal lining consists of simple columnar epithelium.
Lining is not folded or villi, but has numerous straight tubules glands called crypts.

Large Intestine (Colon)
Crypts are similar to the glands of the small intestine, with absorptive, goblet, and granular cells.
The major difference is goblet cells are the predominate cell type while the others decrease in number.

Large Intestine (Rectum)
Straight muscular tube that begins at the termination of the sigmoid colon and ends at the anal canal
Simple columnar epithelium.
The muscular tunic is relatively thick compared to the rest of the digestive tract.

Large Intestine (Anal Canal)
Last 2 to 3cm of the digestive tract.
Begins at the inferior end of the rectum an ends at the anus.
The smooth muscle layer is even thicker than that of the rectum.

Large Intestine (Anal Canal)
Internal anal sphincter – superior end of anal canal.
External anal sphincter – skeletal muscle, inferior end of the canal.
Simple columnar to stratified squamous from superior to inferior anal canal.

Movement of the Large Intestines
Major secretory product, mucus. Mucus lubricates and helps fecal matter to stick
together
Peristaltic waves are largely responsible for moving chyme along the ascending colon.

Movement of the Large Intestines
Mass Movements – several strong contractions in the transverse and descending colon. This large contraction propels the colon contents a considerable distance toward the anus.

Movement of the Large Intestines
Defecation Reflex – local reflex distention of the rectal wall by feces, weak contractions of the rectum and relaxation of internal and external anal sphincters. Parasympathetic reflexes cause strong contractions of the rectum, normally responsible for most of defecation.

The Liver

The Liver
Largest gland in the body
Occupies most of the right hypochondriac and epigastric regions. Inferior to diaphragm, protected by ribs.

The Liver
Four lobes: Right lobe – largest Left lobe Caudate lobe –
posterior Quadrate lobe –
inferior to left lobe

The Liver

The Liver

The Liver
Falciform Ligament separates right and left lobes, suspends liver the liver from the diaphragm.
Porta hepatis – entrance for the hepatic artery and hepatic portal vein, and common hepatic duct.

The Liver
Bile leaves the liver through several bile ducts that form the left and right hepatic ducts which then combine to yield the common hepatic duct
The common hepatic duct will fuse with the cystic duct from the gallbladder to form the common bile duct which empties into the duodenum

The Liver

The Liver (Histology)
Each functional unit is called a liver lobule. Roughly hexagonal in shape.

The Liver (Histology)
Hepatocytes – liver cells, plates of hepatocytes are arranged around a central vein.

The Liver (Histology)
Portal triad – located at each of the six corners, three basic structures are always present. Hepatic artery Hepatic portal vein Bile duct

The Liver (Histology)

The Liver (Function)
Detoxification Production of bile
Fat emulsifier Yellow green alkaline solution Contains
Bile salts, Bile pigments, Cholesterol neutral fats , Phospholipids, Electrolytes

The Liver

The Gall Bladder
Storage of bile Concentration of bile. Thin walled, green, muscular sac. Located in a shallow fossae on the ventral surface
of the liver. Secretes bile by muscular wall contracting, bile
travels out the cystic duct and then flows to the common bile duct.

The Gall Bladder (Biliary Calculi)


The Pancreas
Lies deep to the stomach. Produces a broad spectrum of digestive enzymes.

The Pancreas
Has both exocrine and endocrine functions Pancreatic juice- exocrine product, drains via the
Main pancreatic duct. Acini – small clusters of secretory cells.
Secretions Pancreatic juice, Trypsinogen, Carboxypeptidase,
Chymotrypsin, Amylases, Lipases, Nucleases

The Pancreas

The Pancreas
Insulin and glucagon is secreted on its endocrine portion via patches of hormone-secreting cells known as Islets of Langerhans
Insulin and glucagon act in antagonistic fashion

The Pancreas



End