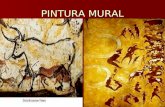
PINTURA MURAL. MURAL EGÍPCIO MURAL CRETENSE PADRÃO GREGO X ROMANO.
The Blood–Brain Barrier - CSHL Pcshperspectives.cshlp.org/content/7/1/a020412.full.pdf · Mural...
Transcript of The Blood–Brain Barrier - CSHL Pcshperspectives.cshlp.org/content/7/1/a020412.full.pdf · Mural...

The Blood–Brain Barrier
Richard Daneman1 and Alexandre Prat2
1Departments of Neuroscience and Pharmacology, University of California, San Diego, San Diego,California 92093
2Department of Neuroscience, Universite de Montreal, Montreal, Quebec H2X 0A9, Canada
Correspondence: [email protected]
Blood vessels are critical to deliver oxygen and nutrients to all of the tissues and organsthroughout the body. The blood vessels that vascularize the central nervous system (CNS)possess unique properties, termed the blood–brain barrier, which allow these vessels totightly regulate the movement of ions, molecules, and cells between the blood and thebrain. This precise control of CNS homeostasis allows for proper neuronal function andalso protects the neural tissue from toxins and pathogens, and alterations of these barrierproperties are an important component of pathology and progression of different neurolog-ical diseases. The physiological barrier is coordinated by a series of physical, transport, andmetabolic properties possessed by the endothelial cells (ECs) that form the walls of the bloodvessels, and these properties are regulated by interactions with different vascular, immune,and neural cells. Understanding how these different cell populations interact to regulate thebarrier properties is essential for understanding how the brain functions during health anddisease.
Blood vessels convey blood from the heart toeach tissue and organ throughout the body,
which is essential to deliver oxygen and nutri-ents to the tissues, remove carbon dioxide andmetabolic waste from tissues, convey hormonalsignaling among tissues, as well as mediate theinteraction of the peripheral immune systemwith each tissue. The vascular tree is comprisedof arteries and arterioles, which deliver bloodto the tissues, the capillary bed, which is essen-tial for gas and nutrient exchange within tissues,and venules and veins, which drain blood fromtissues. Each segment has different propertiesdepending on where they are in the vasculartree as well as which organ they vascularize. Inparticular, the microvasculature, made up of
the capillaries and postcapillary venules, hasdifferent properties to meet the unique require-ments of the tissue they vascularize.
There are three main structural classes ofcapillaries. Continuous nonfenestrated capillar-ies of the skin and lung are joined together bycellular junctions, have a complete basementmembrane (BM), and lack fenestra (pores) intheir plasma membrane. Continuous fenestrat-ed vessels of the intestinal villi and endocrineglands have a similar continuous structure butcontain diaphragmed fenestra throughout theirmembrane. Discontinuous capillaries in the liv-er have large gaps throughout the cell and havean incomplete BM. These classes of capillariesdiffer greatly in their regulation of movement of
Editors: Ben A. Barres, Marc R. Freeman, and Beth Stevens
Additional Perspectives on Glia available at www.cshperspectives.org
Copyright # 2015 Cold Spring Harbor Laboratory Press; all rights reserved; doi: 10.1101/cshperspect.a020412
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
1
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

solutes between the blood and the tissues, withcontinuous fenestrated capillaries being themost restrictive, and discontinuous being theleast restrictive (Aird 2007a,b).
The blood–brain barrier (BBB) is a termused to describe the unique properties of themicrovasculature of the central nervous system(CNS). CNS vessels are continuous nonfenes-trated vessels, but also contain a series of addi-tional properties that allow them to tightly reg-ulate the movement of molecules, ions, and cellsbetween the blood and the CNS (Zlokovic 2008;Daneman 2012). This heavily restricting barriercapacity allows BBB ECs to tightly regulate CNShomeostasis, which is critical to allow for properneuronal function, as well as protect the CNSfrom toxins, pathogens, inflammation, injury,and disease. The restrictive nature of the BBBprovides an obstacle for drug delivery to theCNS, and, thus, major efforts have been madeto generate methods to modulate or bypass theBBB for delivery of therapeutics (Larsen et al.2014). Loss of some, or most, of these barrierproperties during neurological diseases includ-ing stroke, multiple sclerosis (MS), brain trau-mas, and neurodegenerative disorders, is amajor component of the pathology and progres-sion of these diseases (Zlokovic 2008; Daneman2012). BBB dysfunction can lead to ion dysreg-ulation, altered signaling homeostasis, as well asthe entry of immune cells and molecules intothe CNS, processes that lead to neuronal dys-function and degeneration.
CELLS OF THE BBB
Blood vessels are made up of two main cell types:ECs that form the walls of the blood vessels, andmural cells that sit on the ablumenal surface ofthe EC layer. The properties of the BBB are large-ly manifested within the ECs, but are inducedand maintained by critical interactions withmural cells, immune cells, glial cells, and neuralcells, which interact in the neurovascular unit(Fig. 1).
Endothelial Cells
Endothelial cells (ECs) are mesodermally de-rived modified simple squamous epithelial cells
that form the walls of blood vessels. The diam-eter of large arteries and veins can be made upof dozens of ECs, whereas the smallest capillaryis formed by a single EC folding onto itself toform the lumen of the vessel (Aird 2007a,b).These CNS microvascular ECs are extremelythin cells that are 39% less thick than muscleECs, with a distance of less than a quarter of amicron separating the lumenal from the paren-chymal surface (Coomber and Stewart 1985).
CNS ECs have unique properties comparedwith ECs in other tissues that allow them totightly regulate the movement of ions, mole-cules, and cells between the blood and the brain.CNS ECs are held together by tight junctions(TJs), which greatly limit the paracellular flux ofsolutes (Reese and Karnovsky 1967; Brightmanand Reese 1969; Westergaard and Brightman1973). CNS ECs undergo extremely low ratesof transcytosis as compared with peripheralECs, which greatly restricts the vesicle-mediatedtranscellular movement of solutes (Coomberand Stewart 1985). This tight paracellular andtranscellular barrier creates a polarized cell withdistinct lumenal and ablumenal membranecompartments such that movement betweenthe blood and the brain can be tightly controlledthrough regulated cellular transport properties(Betz and Goldstein 1978; Betz et al. 1980).
There are two main categories of transport-ers expressed by CNS ECs. The first are effluxtransporters, which are polarized to the lumenalsurface and transport a wide variety of lipophil-ic molecules that could otherwise diffuse acrossthe cell membrane, toward the blood (Cordon-Cardo et al. 1989; Thiebaut et al. 1989; Loscherand Potschka 2005). The second are highly spe-cific nutrient transporters that facilitate thetransport of specific nutrients across the BBBinto the CNS, as well as removal of specific wasteproducts from the CNS into the blood (Mitta-palli et al. 2010). CNS ECs contain higheramounts of mitochondria compared to otherECs (Oldendorf et al. 1977), which is thoughtto be critical to generate ATP to drive the iongradients critical for transport functions. CNSECs also express an extremely low level of leu-kocyte adhesion molecules (LAMs), as com-pared with ECs in other tissues greatly limiting
R. Daneman and A. Prat
2 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

the amount of immune cells that enter the CNS(Henninger et al. 1997; Aird 2007a; Danemanet al. 2010a). In addition, there is thought to bedifferential vascular metabolism in CNS ECsgenerating a barrier by altering the physicalproperties of molecules, which can change theirreactivity, solubility, and transport properties.The combination of physical barrier properties(TJs, low transcytosis), molecular barrier prop-erties (efflux transporters, specific metabolism,low LAMs), as well as specific transporters todeliver required nutrients, allows the ECs totightly regulate CNS homeostasis.
A major question remains whether the BBBin different regions of the brain possess uniqueproperties required for the function of the localneural circuitry. For instance, localized trans-port of specific nutrients could be importantfor the development or functions of specificsubclasses of neurons. Although most regions
of the CNS are vascularized by capillaries thatcontain BBB properties, specific nuclei adjacentto the third and fourth ventricles, including thesubfornical organ, area postrema, pineal gland,and median eminence, contain vessels that havea much greater passive permeability (Ufnal andSkrzypecki 2014). The capillaries of these cir-cumventricular organs are continuous fenes-trated vessels, with a high permeability to sol-utes. This high permeability is important forthe functions of these nuclei, which either senseblood solute concentrations or secrete mole-cules into the blood.
Mural Cells
Mural cells include vascular smooth musclecells that surround the large vessels and peri-cytes, which incompletely cover the endotheli-al walls of the microvasculature. Pericytes (PCs)
AE
B
D E F
A CAE
EC
EC
PC
TJ
PC
TJ
AEEC
PC
Figure 1. Components of the BBB. (A) Vascular cast of a spinal cord showing density of the CNS vascularnetwork. (B) Electron micrograph (EM) of a cross section of a CNS vessel depicting a relationship amongendothelial cells (ECs), pericytes (PCs), and astrocytes. (C) Magnified EM of ECs depicting a relationshipamong ECs (with tight junctions [TJ]), PCs, basement membranes (BMs), and astrocyte endfeet (AE).(D) Schematic representation of the cell types within the neurovascular unit. (E) Immunofluorescencemicrograph depicting relationship of PCs (red) with ECs (green). (F) Micrograph depicting relationshipof astrocytes (red-labeled with GFAP-cre; Rosa-tdTomato) with blood vessels (unstained). Astrocytes extendprocesses that ensheath the blood vessels, such that the outline of the blood vessels can be visualized by theendfeet of these processes (courtesy of Matthew Boisvert and Nicola Allen).
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 3
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

are cells that sit on the ablumenal surface of themicrovascular endothelial tube, and are embed-ded in the vascular BM (Sims 1986). A difficultyin studying PCs is the lack of a specific markerthat is expressed uniquely by PCs, and, thus,these cells are often confused with other cellsthat sit in the perivascular space (Armuliket al. 2011). Currently, the most widely acceptedmolecular identifier of CNS PCs is positive re-activity to both PDGFR-b and NG2; but othermarkers, including Anpep (CD13), desmin,Rgs5, Abcc9, Kcnj8, Dlk, and Zic1, have allbeen used to identify PCs, with none being per-fect identifiers of this cell type (Armulik et al.2011). Pericytes extend long cellular processesalong the ablumenal surface of the endotheliumthat can often span several EC bodies. Thesecells contain contractile proteins, and have theability to contract to control the diameter of thecapillary (Peppiatt et al. 2006; Hall et al. 2014).Although these cells line the endothelial tube,most of the cell body and processes do not touchthe endothelium, but are separated by the BMthey are embedded within. The processes doform cellular adhesions with the endotheliumat discrete points, described as peg-and-socketjunctions, and are mediated by the adhesionmolecule N-cadherin (Gerhardt et al. 2000).In addition, other pericyte-endothelial cellularadhesions have been identified including adhe-sion plaques, gap junctions, and tight junctions(Courtoy and Boyles 1983; Cuevas et al. 1984;Larson et al. 1987; Diaz-Flores et al. 2009).
CNS PCs have been shown to have uniqueproperties compared to PCs in other tissues.CNS PCs are derived from the neural crest, incontrast with PCs in many peripheral tissues,which are derived from the mesoderm (Majesky2007). In addition, CNS microvasculatures havethe highest CNS PCs coverage of any tissue, withan endothelial:pericyte ratio estimated between1:1 and 3:1, whereas the muscle has a ratio of100:1 (Shepro and Morel 1993). Pericytes playimportant roles in regulating angiogenesis, dep-osition of extracellular matrix, wound healing,regulating immune cell infiltration, and regula-tion of blood flow in response to neural activity,and reports suggest that they also can be multi-potent stem cells of the CNS (Armulik et al.
2011). In addition, these cells have been shownto be important for regulating the formation ofthe BBB during development, as well as main-taining its function in adulthood and aging (Ar-mulik et al. 2010; Daneman et al. 2010b). Oneof the major questions in pericyte biology iswhether there are different subsets of PCs thatmay have different functions. Owing to the lackof defining markers, it remains unclear whetherall of the different functions attributed to PCsare performed by all of the same cells, by differ-ent subsets of PCs, or even by nonpericyte cellsthat sit adjacent to the vasculature. The iden-tification of new PC-specific markers, as well asthe potential identification of markers of sub-sets of PCs will aid in clearing up these issues.
Basement Membrane
The vascular tube is surrounded by two BMs,the inner vascular BM and the outer parenchy-mal BM, also called the vascular glia limitansperivascularis (Del Zoppo et al. 2006; Sorokin2010). The vascular BM is an extracellular ma-trix secreted by the ECs and PCs, whereas theparenchymal BM is primarily secreted by astro-cytic processes that extend toward the vascula-ture. These BMs are comprised of different se-creted molecules including type IV collagens,laminin, nidogen, heparin sulfate proteogly-cans, and other glycoproteins. The vascular andparenchymal BMs have a different composition,for instance, the former is made up of lamininsa4 and a5, whereas the latter contains lamininsa1 anda2 (Wu et al. 2009; Sorokin 2010). TheseBMs provide an anchor for many signaling pro-cesses at the vasculature, but also provide anadditional barrier for molecules and cells tocross before accessing the neural tissue. Disrup-tion of these BMs by matrix matalloproteinasesis an important component of BBB dysfunctionand leukocyte infiltration that is observed inmany different neurological disorders.
Astrocytes
Astrocytes are a major glial cell type, which ex-tend polarized cellular processes that ensheatheither neuronal processes or blood vessels (Ab-bott et al. 2006). The endfeet of the basal process
R. Daneman and A. Prat
4 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

almost completely ensheath the vascular tube,and contain a discrete array of proteins includ-ing dystroclycan, dystrophin, and aquaporin 4.The dysroglycan–dystrophin complex is im-portant to link the endfeet cytoskeleton to theBM by binding agrin (Noell et al. 2011; Wolburget al. 2011). This linkage coordinates aquaporin4 into orthogonal arrays of particles, which iscritical for regulating water homesostasis in theCNS. Astrocytes provide a cellular link betweenthe neuronal circuitry and blood vessels. Thisneurovascular coupling enables astrocytes to re-lay signals that regulate blood flow in responseto neuronal activity (Attwell et al. 2010; Gordonet al. 2011). This includes regulating the con-traction/dilation of vascular smooth musclecells surrounding arterioles as well as PCs sur-rounding capillaries. Astrocytes have been iden-tified as important mediators of BBB formationand function because of the ability of purifiedastrocytes to induce barrier properties in non-CNS blood vessels in transplantation studies(Janzer and Raff 1987), as well as induce barrierproperties in cultured ECs in in vitro cocultureparadigms (Abbott et al. 2006). One issue withthese studies is that the astrocytes are oftencultured from neonatal rodent brains and gothrough many rounds of cell division, suggest-ing that these studies are analyzing progenitorcells as opposed to mature astrocytes. Recentdata analyzing the BBB in dissected rodent em-bryos suggest that the BBB is formed beforeastrocyte generation and ensheathment of thevasculature (Daneman et al. 2010b), and, thus,these cells do not play a role in the initial induc-tion of the BBB. The identification of astrocyte-secreted factors that do regulate BBB functionsuggests that mature astrocytes modulate andmaintain the barrier once it is formed.
Immune Cells
CNS blood vessels interact with different im-mune cell populations both within the bloodas well as within the CNS. The two main cellpopulations within the CNS are perivascularmacrophages and microglial cells. Perivascularmacrophages are monocyte lineage cells thatsit on the ablumenal side of the vascular tube
commonly found in the Virchow–Robin space,a small fluid filled canal that lines the ablume-nal surface of the veins and arteries that enter/leave the CNS (Hickey and Kimura 1988; Polflietet al. 2001). These cells are derived from blood-borne progenitors, and chimera experimentssuggest that they are able to cross the BBB andcan be 80% replaced within 3 mo (Unger et al.1993; Vass et al. 1993; Williams et al. 2001).These cells provide a first line of innate immu-nity by phagocytosing cellular debris. Microgli-al cells are resident CNS parenchymal immunecells that are derived from progenitors in theyolk sac and enter the brain during embryonicdevelopment (Ginhoux et al. 2010). These cellsare involved in regulating neuronal develop-ment, innate immune response, and woundhealing, and can act as antigen-presenting cellsin adaptive immunity (Streit et al. 2005; Ajamiet al. 2007). In addition, different blood-borneimmune cell populations, including neutro-phils, T cells, and macrophages, can interactwith CNS vessels when activated and arethought to regulate BBB properties in responseto infection, injury, and disease by releasingreactive oxygen species that can increase vascu-lar permeability (Persidsky et al. 1999; Hudsonet al. 2005). Identifying the mechanisms bywhich both the immune cells and the BBB be-come “activated” to interact may be importantin deciphering the mechanisms by which theBBB is disrupted during different neurologicaldiseases.
MOLECULES OF THE BBB
The discovery of molecules expressed by CNSECs has led to the identification of importantstructural and transport components of theBBB (Fig. 2) (Li et al. 2001, 2002; Enerson andDrewes 2006; Cayrol et al. 2008; Daneman et al.2009, 2010a; Ohtsuki et al. 2014). Recently, theuse of large-scale genomic and proteomic ex-perimental approaches has provided greater de-tail and understanding of the molecular biol-ogy of the BBB. Use of acutely purifiedmicrovascular fragments, acutely purified ECs,and cultured ECs combined with microarrarytechnology, RNA sequencing, and mass spec-
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 5
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

troscopy proteomic analysis have enabled large-scale gene expression comparisons of CNS ECswith neural cells as well as ECs from other tis-sues. In particular, comparison of the moleculardifferences between CNS ECs and ECs fromnonneural tissues has provided an understand-ing of the unique molecular composition of theBBB.
Tight Junctions
CNS ECs are held together by TJs, which create ahigh-resistance paracellular barrier to moleculesand ions, polarizing the luminal and ablumenalcompartments. Most of what is known aboutTJs is from work on ECs, which have identifiedthat these cellular adhesions are formed on theapical part of the lateral membrane by homo-typic and heterotypic interactions of transmem-brane molecules that are linked to the cytoskel-eton through interactions with cytoplasmicadaptors. The strength of the junctions variesgreatly depending on the tissue in which theyare found, and work in cell culture suggeststhat they have a size-selective permeability touncharged molecules of up to 4 nm, and thenlow permeability to larger molecules (Van Itallieand Anderson 2006; Van Itallie et al. 2008). Thissuggests that the TJs form a 4-nm pore and thatlarger molecules would pass through disconti-nuities in the junctions.
The transmembrane molecules includeclaudins, occludins, and JAMs (Furuse 2010).
Claudins are a class of more than 25 differentfamily members that are tetraspanins charac-terized by a W-GLW-C-C domain in the firstextracellular loop (Gupta and Ryan 2010). Evi-dence in vitro suggests that claudins are es-sential for the paracellular barrier formation.Expression of claudins is sufficient to form TJstrands in fibroblasts, and disruption of clau-dins decreases the paracellular barrier proper-ties of canine kidney cells (Furuse et al. 1998,2001; Van Itallie et al. 2001; Amasheh et al. 2005;Hou et al. 2006). Work with chimeric claudinshas shown that amino acid residues in the firstextracellular loop define the size and charge se-lectivity of the pore within the cellular junc-tion, and, thus, the composition of the claudinswithin a given cell can determine the permeabil-ity of the paracellular barrier (Colegio et al.2003). Different claudin family members areexpressed by different epithelial barriers indifferent tissues, and mouse knockouts haveshown that specific family members are essen-tial for specific barriers (cldn 1 epidermal bar-rier, cldn 16 kidney epithelia, cldn11 CNS my-elin, cldn 19 peripheral myelin), many of whichhave been associated with human disease (Gowet al. 1999; Furuse et al. 2002; Hadj-Rabia et al.2004; Knohl and Scheinman 2004; Miyamotoet al. 2005; Hampson et al. 2008). Claudin-5has been shown to be highly expressed by CNSECs, and mice that lack claudin-5 have a size-selective leak of the BBB (Morita et al. 1999;Nitta et al. 2003). In addition, other claudins,
Astrocyte
Endothelial cell
Basal lamina
Blood
CNS Parenchyma
Pericyte
N-cadherin
Pgp
VE-cadherinTfr
TfrLat 1Mct 1glut1
CD31Ocln
BCRP Mrp
Jacop
Cldn5
Cldn12
Catenins
Jacop
ZO-2
ZO-1
ZO-1ZO
-2
Figure 2. Schematic representation of molecules of the BBB. CNS, central nervous system; VEcad, VE cadherin.
R. Daneman and A. Prat
6 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

including cldn12 and cldn3, have been identi-fied at the BBB (Nitta et al. 2003; Liebner et al.2008; Daneman et al. 2010a).
Occludin is a tetraspanin expressed by epi-thelial cells and CNS ECs, an in vitro cultureexperiment disrupting occludin homotypic in-teractions suggest that it is important for theresistance of the barrier (Balda et al. 1996; Mc-Carthy et al. 1996; Wong and Gumbiner 1997).Occludin is highly enriched in CNS ECs com-pared with ECs in nonneural tissues, indicatingthat it may be an important component of thebarrier. Occludin-deficient mice, however, areshown to have a normal high-resistance epithe-lial barrier and a functioning BBB. These micedo have calcification of the CNS suggesting thatperhaps occludin specifically regulates calciumflux across the BBB (Saitou et al 2000). JAMs areimmunoglobulin superfamily members thatform homotypic interactions at tight junctionsin epithelial cells and ECs. JAMs have beenshown to regulate leukocyte extravasation as wellas paracellular permeability (Martin-Paduraet al. 1998; Johnson-Leger et al. 2002; Ludwiget al. 2005). In particular, JAM4 has been iden-tified at the BBB in mice (Daneman et al.2010a). Recently, it has been shown that uniquemolecular components are required to seal theparacellular barrier at the contact points of threecells. These tricellular junctional complexes aremade up of lipolysis-stimulated receptor (LSR),which is required to localize marveld2 to tricel-lular adhesions (Masuda et al. 2011). It remainsunclear what the nature of the size/charge-se-lective pore is formed by the specific composi-tion tight junction proteins expressed by CNSECs, and whether the permeability of this poreis static or whether it is dynamically altered inresponse to neuronal activity.
The transmembrane adhesion complexesare linked to the cytoskeleton through a seriesof cytoplasmic adaptors including ZO-1, ZO-2,Cingulin, Jacop, MAGIs, and MPPs (Van Itallieand Anderson 2013). In addition, the TJs inter-act with basal adherens junctions (AJs), whichconnect all ECs and are made up of vascularendothelial (VE)-cadherin and platelet EC ad-hesion molecules (PECAM)1, and are linkedto the cytoskeleton by catenins. Interestingly,
many of the TJ proteins identified, includingcldn5, cldn12, ZO-1, and ZO2, appear to beexpressed by ECs in all tissues. Thus, a majorquestion is why only CNS ECs form this tightbarrier and not ECs in other tissues. Transcrip-tional analysis comparing CNS ECs with pe-ripheral ECs suggests that several cytoplasmicadaptors, including jacop and MPP7, as wellas tricellular TJ molecules, LSR and marveld2(Daneman et al. 2010a), are enriched at the BBBsuggesting that these molecules may be criticalfor this barrier formation.
Transporters
CNS ECs are highly polarized cells that havedistinct lumenal and ablumenal compartments.The low permeability of the paracellular junc-tions allows the transport properties of the cellsto control the movement of ions and moleculesbetween the blood and the brain. There are twomain types of transporters expressed by CNSECs: efflux transporters and nutrient trans-porters. Current work to elucidate the full arrayof transporters and their substrates is highlysought after both to understand the externalrequirements for brain metabolism and func-tion, but also to identify targets to aid in drugdelivery across the BBB.
Efflux transporters, including Mdr1, BCRP,and MRPs, use the hydrolysis of ATP to trans-port their substrates up their concentrationgradient (Ha et al. 2007). Many of these trans-porters are localized to the lumenal surface andtransport a wide array of substrates into theblood compartment. This wide substrate diver-sity allows these transporters to provide a bar-rier to many small lipophilic molecules, whichwould otherwise passively diffuse through theEC membrane. Mdr1, also called P-glycopro-tein, has been widely studied in this context,and knockout mice show an increase in a widevariety of small lipophilic drugs entering thebrain, as well as endogenous molecules (Schin-kel et al. 1994, 1995, 1996). Up-regulation ofMdr1 has also been associated with drug-resis-tant epilepsy and tumors (Potschka et al. 2001;Abbott et al. 2002). An important avenue ofresearch uses structural modeling to predict
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 7
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

substrates of these efflux transporters to developtherapeutics that can avoid efflux and, thus,gain entry to the CNS. In addition, developinginhibitors of these efflux transporters is an on-going research avenue to aid in delivery of smallmolecule compounds to the CNS. Interestingly,not much is known about the endogenous mol-ecules that are effluxed by these transporters,how this is important to regulate brain func-tion, and whether inhibitors would alter thetissue distribution of important endogenousmolecules.
Nutrient transporters facilitate the move-ment of specific nutrients down their concen-tration gradient. CNS ECs express a wide varietyof these transporters to deliver very specific nu-trients across the physical barrier of the CNSECs into the CNS parenchyma. Many of thesebelong to the solute carrier class of facilitatedtransporters, including slc2a1 (glucose), slc16a1(lactate, pyruvate), slc7a1 (cationic amino ac-ids), and slc7a5 (neutral amino acids, L-DOPA)(Zlokovic 2008; Daneman 2012). Slc2a1, alsocalled glut1, has been largely studied for itsrole in providing the CNS with glucose. Expres-sion of this transporter is highly enriched inCNS ECs compared with ECs in nonneural tis-sues, and it facilitates the transport of glucosedown its concentration gradient from the bloodinto the brain (Cornford et al. 1994). In hu-mans, Glut1 deficiency leads to an epilepticsyndrome that is treated by being fed a high-ketone diet (De Vivo et al. 1991, 2002). In ad-dition, CNS ECs express a variety of differentreceptor-mediated transport systems, includingthe transferrin receptor (transferrin/iron), Ager(amyloid), and low-density receptor-related li-poprotein (LRP)1/LRP8. Many of these trans-port systems are being targeted as Trojan horsesto aid in drug delivery to the CNS. Althoughmost of these transporters provide nutrientsfrom the blood to the brain (slc2a1, slc16a1,slc7a5, Tfr), several are also important for re-moving waste products from the brain (Ager). Acomplete characterization of BBB transporters,their substrates, and their direction of transportis critical to determine the external nutrient re-quirements of the CNS and how the BBB me-diates the interaction between the blood and theCNS. Recently, systemic proteins have been im-
plicated in regulating neurogenesis differentlyin youth and during aging (Villeda et al. 2011,2014; Katsimpardi et al. 2014); however, it re-mains unclear whether this is because of specifictransport, localized permeability of the BBB, ornonspecific passive movement of small amountsof systemic factors.
Transcytosis
In CNS ECs, the rate of transcytosis is dramat-ically lower than in ECs in nonneural tissues butis up-regulated as a major component of BBBdysfunction during injury and disease. Trans-cytosis through ECs is mediated through caveo-lin-based vesicle trafficking. Caveolin-1 is ex-pressed by all ECs and is up-regulated at theBBB following traumatic brain injury (Liu et al.2010; Zhao et al. 2011; Gu et al. 2012). Plasma-lemma vesicle-associated protein (PLVAP) ex-pression is enriched in peripheral ECs com-pared with CNS ECs, and has been implicatedin vesicle trafficking, formation of fenestra, andleukocyte extravasation in these “leaky” vascu-lar beds. This molecule is also up-regulated inCNS ECs in a variety of diseases in which there isBBB leakage (Shue et al. 2008; Keuschnigg et al.2009). Therefore, lack of PLVAP in healthy CNSECs appears to be important for limiting per-meability.
Leukocyte Adhesion Molecules (LAMs)
In the healthy CNS, there is an extremely lowlevel of immune surveillance, with an almostcomplete lack of neutrophils and lymphocyteswithin the parenchyma. Entry of a leukocytefrom the blood into a tissue is a multiple-stepprocess that includes rolling adhesion, firm ad-hesion, and extravasation. This requires a se-ries of different leukocyte adhesion molecules,including selectins (E-selectin, P-selectin) forrolling adhesion and immunoglobulin familymembers for firm adhesion (Huang et al. 2006;Aird 2007b). The expression of these adhesionmolecules is much lower in CNS ECs than inperipheral ECs but is elevated during neuroin-flammatory diseases, such as stroke and MS(Henninger et al. 1997; Huang et al. 2006; En-gelhardt 2008; Daneman et al. 2010a). Interest-
R. Daneman and A. Prat
8 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

ingly, different subsets of inflammatory cells areobserved infiltrating the CNS in different diseas-es. For instance, in MS, there is infiltration ofT cells, B cells, neutrophils, and macrophagesat sites of active lesions, whereas in stroke, thereare neutrophil and macrophage infiltrates butlymphocytes are largely excluded. An importantquestion is whether each cell has a differentmechanism for crossing the BBB, and whetherthe discrimination is done at the level of theactivated BBB or the activated immune cell.
Other Components of the BBB
Large-scale genomic and proteomic approacheshave identified signaling cascades that areturned on in CNS ECs. In particular, Wnt/b-catenin signaling through Lef1, as well as Sonichedgehog signaling through Gli have beenshown to be important for regulating the for-mation and function of the BBB (Liebner et al.2008; Stenman et al. 2008; Daneman et al. 2009;Alvarez et al. 2011a). In addition, vascular me-tabolism has been implicated in regulating bar-rier properties of CNS vasculature by metabo-lizing potential toxins or altering the propertiesof molecules (Fig. 1). Specific enzymes, includ-ing carbonic anhydrase IV and g-glutamyltranspeptidase, have been identified as enrichedin CNS vessels compared with vessels from non-neural tissues (Orlowski et al. 1974; Ghandouret al. 1992).
Large-scale genomic and proteomic ap-proaches have provided invaluable resources inunderstanding the gene expression of the BBB,but work still needs to be done to identify whichof these BBB-enriched genes are important foreach aspect of the BBB, whether there is hetero-geneity of these genes at different segments ofthe vascular tree and in different brain regions,and whether the expression and function ofeach protein is dynamically regulated by neuro-nal function, stress, or diet. In addition, workexpanding beyond genomics is aimed at identi-fying the proteomics, miRNAs, noncodingRNAs, lipids, metabolomics, epigenetics, andother regulatory steps that are important forBBB formation and function.
REGULATION OF THE BBB FORMATIONAND HOMEOSTASIS
Although key properties of the BBB are mani-fested within the ECs, important transplanta-tion studies have shown that they are regulatedby interactions with the microenvironment ofthe CNS (Stewart and Wiley 1981; Janzer andRaff 1987). The BBB is not one physiology, but aseries of physiological properties that eitherneed to be induced (TJs, transporters, metabol-ic enzymes) or inhibited (transcytosis, LAMs)in CNS ECs. Recent work has dissected the cel-lular and molecular mechanisms that regulatethis process, and have identified that it is a com-plex process of induction and maintenance sig-naling interactions among CNS ECs and PCs,astrocytes, and immune cells.
Regulation of Barrier Properties duringAngiogenesis
Recent work in genetic mouse models hasshown that there is a unique angiogenic pro-gram driving vessel formation in the CNS reg-ulated by Wnt/b-catenin that also inducesspecific barrier properties in CNS ECs (Liebneret al. 2008; Stenman et al. 2008; Daneman et al.2009). Comparative microarray analysis hasidentified that effectors of Wnt/b-catenin sig-naling, including Lef1, Apcdd1, and tnfrsf19, areenriched CNS ECs compared to ECs in periph-eral organs (Daneman et al. 2009, 2010a). Trans-genic reporter mice have confirmed that Wnt/b-catenin signaling is activated in CNS ECs dur-ing embryonic angiogenesis (Liebner et al. 2008;Stenman et al. 2008; Daneman et al. 2009). Dif-ferent Wnt ligands are secreted by neural stemcells and neural progenitors in spatially distinctregions, notably Wnt7a and Wnt7b in ventralregions and Wnt1, Wnt3, Wnt 3a, and Wnt4in dorsal regions (Stenman et al. 2008; Dane-man et al. 2009). Disruption of Wnt signalingin all ECs by conditional depletion of b-cateninleads to widespread CNS angiogenic defectswith overtly normal blood vessel formation inperipheral tissues. These defects include a thick-ening of the vascular plexus, which contains en-dothelial progenitors, a loss of capillary beds,
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 9
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

and the formation of hemorrhagic vascular mal-formations, which together suggest that Wnt is amigration signal driving vessels into the CNS(Stenman et al. 2008; Daneman et al. 2009).These phenotypes were also observed followingdeletion of neural Wnts (Wnt7a/7b), demon-strating that the CNS angiogenic program re-quires Wnt as well as b-catenin. This CNS-specific angiogenic program was also shown toinduce the expression of nutrient transporters,such as glut1, as well as the specific tight junc-tion molecules like claudin-3 (Liebner et al.2008; Stenman et al. 2008; Daneman et al.2009). Taken together, these data suggest thatspecific properties of the BBB are induced asvessels invade the CNS by a unique angiogenicprogram. Different Wnt ligands and Fzd recep-tors are expressed in spatially distinct regionsand appear to be important for the regulationof CNS angiogenesis and BBB formation inthose regions. One interesting receptor/ligandpair is Norrin/Fzd4, which is required for theformation of the retinal vasculature. Norrin is atransforming growth factor (TGF)-b familymember with no homology with Wnt ligands,which is able to activate Fzd4 and induce canon-ical Wnt signaling. Loss of Norrin or Fzd4 pro-duces major retinal vascular defects including areduction in endothelial proliferation, vascularmalformations, crossing of arteries and veins, aloss of venous fate, and leakiness of the blood–retinal barrier (Xu et al. 2004; Ye et al. 2010;Wang et al. 2012). Fzd4 mutants also have re-gional-specific BBB defects in the cerebellum,spinal cord, olfactory bulb but not the cortex,striatum, or hypothalamus. The more wide-spread phenotype of Fzd4 mutants suggeststhat it may also be activated by other ligands.Use of genetic mosaics has shown that Fzd4is required cell-autonomously for sealing theBBB, and the Fzd4-deficient ECs have a loss ofclaudin-5 and an increase in PLVAP (Wang et al.2012). Interestingly, deletion of Fz4 in adultsleads up-regulation of PLVAP, loss of claudin-5,and leakage of the BBB, whereas reintroductionof Norrin to Norrin-deficient retinas leads tosealing of BBB properties (Wang et al. 2012).These data suggest that canonical Wnt signalingis not only required for BBB induction, but
that also for maintenance of the BBB phenotypein adults, when the ligands are glial derived.
Regulation of the BBB by Pericytes
Analysis of mouse mutants in PDGFBB-PDGFR-b signaling has identified an importantrole for PCs in regulating BBB formation andfunction (Armulik et al. 2010; Daneman et al.2010b). These mutant mouse models includePdgfb null and Pdgfrb null mice that completelylack CNS PCs and die at birth, as well as extra-cellular matrix (ECM)-retention motif muta-tions to Pdgfb or hypomorphic alleles of Pdgfrbin which mice have fewer PCs than their wild-type littermates. Analysis of the BBB in Pdgfrbnull mice during embryogenesis revealed a leakyBBB, demonstrating that PCs are required toregulate the formation of the BBB. In particular,lack of PCs leads to an increase in the rate oftranscytosis and an increase in the expression ofLAMs resulting in CNS-immune infiltration(Armulik et al. 2010; Daneman et al. 2010b).Further use of mice with Pdgfrb hypomorphicalleles, which have varying numbers of CNSPCs, showed that the total number is importantfor the relative permeability of the vessels (Ar-mulik et al. 2010; Daneman et al. 2010b). Ad-ditionally, work done in adult mice with ECM-retention motif mutations to Pdgfb that containfewer PCs has identified that PCs are requiredduring adulthood to regulate BBB homeostasis,and particularly do so by inhibiting transcytosis(Armulik et al. 2010). Microarray analysis com-paring the transcriptional profile of CNS ECswith pdgfrb mutant mice and wild-type micesuggest minimal changes in the expression ofgenes involved in BBB-specific properties, suchas tight junctions, nutrient transport, or effluxtransport, but an increase in the expressionof genes involved in peripheral EC-specific“leaky” properties, including transcytosis(PLVAP) and leukocyte adhesion (Icam1, Al-cam) (Daneman et al. 2010b). Taken together,these data suggest that PCs are not involved inthe induction of BBB-specific properties (TJs,transporters), but play an important role in theinhibition of properties normally associated withleaky peripheral vessels (transcytosis, LAMs).
R. Daneman and A. Prat
10 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

Regulation of the BBB by Astrocytes
The persistence of a functional BBB through-out adulthood is maintained and regulated bynumerous factors unique to the micronicheof the neurovascular unit (NVU) (Abbott etal. 2006). Astrocyte–BBB–EC interactions areknown to regulate EC morphology, angiogene-sis, and to influence the phenotype of the barrierunder physiological and pathological condi-tions (Prat et al. 2001).
Astrocytes are known to produce factorsthat modulate endothelial functioning dur-ing development and adulthood. One of thesepathways is the Hedgehog (Hh) signaling cas-cade known to be involved in embryonic mor-phogenesis, neuronal guidance, and angiogen-esis. Astrocytes secrete Sonic Hh (SHh) (Wanget al. 2008), and BBB ECs express the Hh recep-tor Patched-1, the signal transducer Smooth-ened (Smo), as well as transcription factorsof the Gli family. Interestingly, transendothelialelectrical resistance (TEER) and permeabilityexperiments showed that activation of the Hhpathway induced expression of junctional pro-teins and promoted a BBB phenotype. In ad-dition, mice genetically engineered to lose thesignal transducer Smo on ECs had a significantincrease in BBB permeability that correlatedwith a decrease in junctional protein expres-sion and disturbed BMs (Alvarez et al. 2011a,2013), supporting the concept that the Hhpathway has a significant influence on BBBfunction.
Astrocytes also secrete angiogenic factorsthat promote vascular growth, such as vascularendothelial growth factor (VEGF). During de-velopment, VEGF is required for the formation,remodeling, and survival of embryonic bloodvessels. During early embryogenesis, radial gliacells seem to be the source of VEGF neededfor vascular development, although ECs havebeen described to promote cell-autonomousactivation of the VEGF signaling (Lee et al.2007). Although VEGF is a factor mostly knownto promote angiogenesis during development,in adulthood, VEGF decreases the stability of theBBB during inflammatory conditions (Argawet al. 2009, 2012).
Perivascular cells, including astrocytes, se-crete angiopoietins (Ang1), which participatein the complex process of BBB differentia-tion by promoting angiogenesis and inducinga time-dependent decrease in endothelial per-meability. This occurs through the up-regula-tion of junctional protein expression (Prat et al.2001). In contrast, Ang-2 is known to partic-ipate in the early phases of BBB breakdownduring injury and disease (Nourhaghighi et al.2003). Interestingly, when factors known tocompromise BBB function, such as VEGF, arecoexpressed with Ang1, the barrier integrity isenhanced and neuroprotective properties areinduced (Shen et al. 2011).
Astrocytes also produce the angiotensin-converting enzyme-1 (ACE-1), which convertsangiotensin I into angiotensin II and acts ontype 1 angiotensin receptors (AT1) expressedby BBB ECs. Angiotensin II induces tighten-ing of vessels, and, in the CNS, activation ofAT1 restricts BBB permeability and stabilizesjunctional protein function by promoting theirrecruitment into lipid rafts. Angiotensinogen(AGT)-deficient mice have an aberrant expres-sion of occludin at the BBB, suggesting thatastrocyte-secreted angiotensin II promotes TJformation (Wosik et al. 2007).
TGF-b is a pleiomorphic cytokine involvedin cell growth, differentiation, morphogene-sis, apoptosis, and immunomodulation. In theCNS, TGF-b is neuroprotective, and in vitrostudies have shown its capacity to induce Mdr1activity and to reduce BBB permeability (Dohguet al. 2004). TGF-b is secreted by astrocytesand CNS-ECs, and TGF-b known to down-regulate the extent of leukocyte transmigra-tion across the endothelium. However, the over-whelming pleomorphic roles of TGF-b do notcurrently allow a conclusion on the exact role ofastrocyte-derived TGF-b in BBB physiology.
Retinoic acid (RA) can be secreted by radialglial cells, and recent findings suggest that RA isalso secreted by astrocytes, and its receptor, RA-receptor b (RAR-b), is expressed in the devel-oping vasculature. RAR-b activation increasesTEER, which correlated with enhanced expres-sion of VE-cadherin, P-gp, and ZO-1. In vivo,pharmacologic modulation of RAR-b resulted
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 11
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

in a perturbed BBB (Mizee et al. 2013). Inter-estingly, RA is known to regulate the Hh, Wnt,and FGF pathways (Halilagic et al. 2007; Pa-schaki et al. 2012), which implies that RA secre-tion by radial glial cells could be a master up-stream regulator of BBB development.
Convergence of Signaling Events at the BBB
It is clear that the BBB is regulated by a complexset of cellular signaling mechanisms that regu-late both the induction of barrier properties dur-ing initial angiogenesis into the CNS, as well asthe maintenance of barrier properties in adults.Neural stem cells appear to be the key cell typeinvolved in the early differentiation of the ECsinto BBB ECs, and then PCs and astrocytes pro-vide further cues modulating the different bar-rier properties of these CNS ECs. The number ofdistinct factors that are known to impact on BBBpermeability highlights the diversity of the CNSinputs needed to generate this physiological bar-rier. This also emphasizes the redundancy ofmolecular signals affecting BBB formation andstability, and the need for future work to identifyhow each of these signals are coordinated to reg-ulate different aspects of the BBB. These signalscan, however, be integrated into a general con-cept (Prat et al. 2001). Key signaling pathwaysand transcription factors have either barrier-promoting properties (Wnt, Hh, Sox-18, nrf-2, ERG, Nkx2-1, and SP3/YY1) or barrier-dis-rupting effects (NF-kB, Snail, FoxO1, PKC, andeNOS). Within the signaling pathways promot-ing BBB functioning, Wnt and Hh seem to bedominant and to cooperate in driving a BBBphenotype. Wnt ligand binding to Frizzled/LRP5/6 activates b-catenin, which leads to theexpression and targeting of the junctional pro-teins claudin-3 and p120 to the cell membrane(Liebner et al. 2008; Hong et al. 2010). b-Cate-nin also down-regulates the activity of Snail,which has a negative effect on the stability ofp120/VE-cadherin complexes and on the ex-pression of TJ molecules occludin and clau-din-5. Loss of the Wnt coreceptor Lrp5 causesdown-regulation of claudin-5 expression (Chenet al. 2011). The Hh signaling pathway appearsto drive the transcription and expression of
junctional proteins, but also dampens inflam-matory responses on CNS-ECs. Activation ofGli-1 by the Hh ligands or wnt signaling are re-ported to activate Sox-18 (Alvarez et al. 2011a),which control claudin-5 expression (Fontijnet al. 2008). Wnt and Hh activation also inducethe expression of NR2F2, a transcription factorthat promotes Ang-1 expression, inducing junc-tional protein expression through tie-2. NR2F2also down-regulates expression of Ang-2, a fac-tor known to decrease junctional protein expres-sion. In a similar way, activation of the nrf-2pathway by oxidative stress activates antioxidantresponse elements (ARE), which are known tostabilize ZO-1, occludin, and claudin-5 expres-sion (Fan et al. 2013). In addition, nrf-2 protectsECs during injury by supressing the expressionof inflammatory genes (Chen et al. 2006). In thissense, signaling pathways and transcription fac-tors supporting barrier function also tend topromote anti-inflammatory responses.
One of the major issues when analyzing pre-vious work is that many different measures havebeen used to quantify BBB function when ana-lyzing the effect of genetic orenvironmental per-turbations on the barrier, making it difficult tocompare and contrast different studies. Further-more, in many cases, only a small number ofmeasures are used to examine BBB function,whether a single molecular tracer or analysis ofa small set of molecular markers. The BBB is nota single entity, but a series of different propertiespossessed by the CNS ECs and regulated by in-teractions with different neural, vascular, andimmune cells; thus, a more exhaustive approachto understanding how different pathways regu-late each aspect of the BBB is required to fullyunderstand this barrier. Thus, future work needsto identify whether each of these signaling path-ways regulate all aspects of the BBB, or whetherdifferent properties of the BBB are induced andregulated by different pathways, and, if so, howdo each of these pathways coordinate to regulatethe BBB, allowing proper neuronal function.New genetic tools allow for manipulation ofgenes and pathways both in development andin adulthood and, thus, will be able to determinewhether the pathways are required for induc-tion during development, maintenance during
R. Daneman and A. Prat
12 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

adulthood, and/or disruption during disease.Furthermore, new intravital imaging techniquesin live awake-behaving animals will enable theunderstanding of how plastic the BBB is andwhether different properties of the BBB can bedynamically regulated in response to neuronalactivity, diet, infection, or other environmentalstimuli.
DYSFUNCTION OF THE BBB IN CNSDISORDERS
Disruption of the BBB is observed in manydifferent neurological disorders including MS,stroke, Alzheimer’s disease (AD), epilepsy, andtraumatic brain injuries. Functional imaging ofhuman patients and analysis of postmortembrain samples has identified the pathologicalbreakdown of the barrier in different neurolog-ical diseases. In addition, work with animalmodels of disease and with cell culture BBBmodels has enabled the identification of someof the molecular mechanisms that cause changesto the BBB. This dysfunction can include alter-ations in many different properties of the BBBincluding TJs, transporters, transcytosis, andLAM expression. This breakdown can lead toedema, disruption of ionic homeostasis, alteredsignaling, and immune infiltration that can leadto neuronal dysregulation and, ultimately, de-generation. Although BBB dysfunction is oftensecondary to the primary insult in these diseas-es, in some cases, it has been a suggested cause,including MS, epilepsy, and AD (Fig. 3).
MS and Related Disorders
In most CNS pathologies, the BBB is affectedas a result of the inflammation, injury, or de-generative processes specific to the pathology.However, in only a few diseases, the BBB is spe-cifically targeted by the pathogenic process orby the disease determinants. Neuromyelitis op-tica (NMO) and MS are among these diseases.Astrocytes are generally not regarded as a pri-mary target of the immune system in MS,although BBB disruption and alterations in as-trocyte physiology are hallmarks of MS patho-genesis. The etiology of MS remains elusive, but
it is clear that multiple factors are involved indisease development, including environmentaland genetic factors. Nevertheless, MS is a T-cell-mediated disease in which CD4 T-helper (Th)cells of the Th17 and Th1 phenotype play a fun-damental role in its pathogenesis. B cells are alsoessential in MS immunopathogenesis, as anti-bodies produced within the CNS are a funda-mental feature of the disease (i.e., oligoclonalbands) and as B-cell-directed therapies providestrong protection against lesion formation. It isclear that during immune cell infiltration andlesion formation, BBB function becomes com-promised (Larochelle et al. 2011), which is char-acterized by vascular leakage associated with al-terations of junctional proteins. Analysis of MStissue shows that abnormalities in the expres-sion of junctional proteins coincide with peri-vascular astrogliosis, and such changes are de-tected in very early stages of lesion formation(Prat et al. 2001). This has been, in part, ex-plored by Luo et al. (2008) when inducing activeexperimental autoimmune encephalomyelitis(EAE) in mice expressing luciferase under thecontrol of GFAP. Despite showing clinical signsonly at day 11, increases in bioluminescence as-sociated with GFAP expression could be detect-ed in the brain of these animals as early as 3 dpostinduction suggesting that astrocytes are ac-tivated in the very early stages of EAE and in theabsence of clinical signs of the disease.
Besides its primary neuroprotective func-tion, the BBB has also been shown to activelypromote neuroinflammation by orchestratingimmune responses during CNS-targeted auto-immune aggression. BBB ECs are an importantsource of proinflammatory chemokines CCL2(Biernacki et al. 2001; Kebir et al. 2007), CCL5,and CXCL10, which are required for lympho-cyte and monocyte recruitment to the CNS(Prat et al. 2001). Immune cell infiltration intothe CNS correlates with production of pro-inflammatory mediators, such as interleukin(IL)-17, IL-22, granulocyte macrophage colo-ny–stimulating factor (GM-CSF), interferon(IFN)-g, and tumor necrosis factor (TNF)(Alvarez et al. 2011b). These cytokines havebeen implicated in the modulation of EC func-tion by up-regulating the expression of pro-
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 13
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

inflammatory mediators and by affecting theexpression of junctional proteins and, thus,compromising BBB permeability. Last, BBBECs express intercellular adhesion molecule(ICAM)-1, ICAM-2, vascular CAM (VCAM)-1, activated leukocyte CAM (ALCAM), melano-ma CAM (MCAM), and Ninjurin-1, which me-diate, at least in part, the adhesion process andtransmigration of leukocytes and leukocyte sub-types to the CNS (Cayrol et al. 2008; Dodelet-Devillers et al. 2009; Greenwood et al. 2011).Thus, although the BBB protects against CNS-directed inflammation by restricting immunecell access to the brain, it can also regulate thelocal inflammatory response by expressing pro-inflammatory molecules that promote the re-cruitment of peripheral immune cells into theCNS.
Following migration across ECs, leukocytescross the endothelial BM and, subsequently, theparenchymal BM to get access into the CNS.The composition of the endothelial BM canregulate the extent of perivascular infiltrationas large amounts of leukocytes are detected invessels expressing laminin 411 and low levels of511, whereas in the absence of 411, laminin 511is ubiquitously expressed and associates withlow-T-cell infiltration and milder disease. InEAE and MS, immune cell infiltrates are in great
part contained to the perivascular space, andthe process of leukocyte migration across theparenchymal BM and astrocyte endfeet appearsto be more tightly controlled than the diapede-sis across ECs (Engelhardt and Sorokin 2009).In EAE, CD4þ T-cell infiltration across the pa-renchymal BM is not laminin dependent, butrather requires focal activation of and matrixmetalloproteinases (MMP)-2 and MMP-9 toselectively cleave dystroglycan, affecting the BMstability and integrity (Agrawal et al. 2006). In-terestingly, parenchymal BM components andother ECM-binding receptors on the astrocyteendfeet remain unaffected, indicating the ex-istence of specific and specialized protectivemechanisms under the control of astrocytesand possibly other cells within the NVU (Engel-hardt and Sorokin 2009). Thus, further under-standing is needed in terms of astrocyte involve-ment in supporting or inhibiting the activationand migration of immune cells as well as therepair of the affected BBB/NVU during MS/EAE and other CNS disorders.
Reactive astrocytes can also be the source offactors that will negatively affect barrier func-tion at the NVU. In MS and EAE, VEGF-A isexpressed by reactive astrocytes, and in vitro/in vivo studies show its capacity to induceBBB breakdown by disrupting claudin-5 and
GliLef1
SHH
MMPs
MMP
ROS
Astrocytes
Agt
AQ4
FZD
RBCs
Endothelial cells
Immune cells
Health Disease
Wnt
Wnt
Pericyte
AQ4
PDGF-BBPDGFR-β
Ptch Smo
β-Catenin
VEGF
Selectin ICAM
Neuralprogenitor
Figure 3. Schematic representation of signaling regulating the blood–brain barrier in health and disease. ICAM,intercellular adhesion molecule; MMP, matrix metalloproteinase; ROS, reactive oxygen species.
R. Daneman and A. Prat
14 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

occludin expression and promote immune cellinfiltration to the CNS. Additional studies pro-pose that IL-1 production by microglia inducesVEGF-A up-regulation. VEGF-A is releasedfrom the astrocytes and binding to its receptorVEGFR2 on BBB-ECs activates eNOS-depen-dant down-regulation of the junctional proteinsclaudin-5 and occludin that leads to BBB break-down.
Although reactive astrocytes can produceBBB-promoting (i.e., Hh) or BBB-disrupting(i.e., VEGF) factors, they can also lose ordown-regulate factors that have the capacity topromote barrier function. In this regard, astro-cytes produce AGT (which is cleaved into an-giotensin II), and analysis of MS tissues showedthat expression of AGT in astrocytes and occlu-din in ECs is decreased in MS lesions whencompared to normal appearing white matter.This pattern correlates with the down-regulatedexpression of AGT detected in astrocytes stim-ulated in vitro with IFN-g and TNF-a. Inter-estingly, nonimmunized (non-EAE) AGT-defi-cient mice have compromised BBB function,which correlates with decreased and disruptedexpression of occludin. Therefore, local inflam-matory mediators present in perivascular cuffscan also negatively impact on the capacity ofreactive astrocytes to promote BBB functionby down-regulating their production of BBB-promoting factors (Wosik et al. 2007).
NMO is also an immune-mediated diseaseof the CNS affecting predominantly the spinalcord and the optic nerves. In NMO, the produc-tion of anti-AQP4 IgG antibodies affects thefunction of the astrocyte water channel AQP4directly affecting BBB function. Binding of anti-AQP4 antibodies to their target results in theactivation of complement-dependent cytotoxiccell damage that leads to the loss of AQP4,GFAP, and the excitatory amino-acid transport-er 2 (EAAT2). In addition, the BBB damage isassociated with focal areas of perivascular im-mune cell infiltration and demyelination, par-ticularly granulocytes, and eosinophils that de-granulate in the perivascular space causing localdamage that includes astrocyte injury. Althougholigodendrocytes are affected as a result of thepathophysiological changes, the exact mecha-
nism(s) leading to oligodendrocyte and neuro-nal damage remains to be determined.
Modulation of the BBB following Hypoxia/Ischemia and in Stroke
In vivo and in vitro stroke models have shownthat cerebral vascular permeability increasesin a time- and hypoxia-dependent manner.This leads to a subsequent increase in cerebraledema; however, the processes involved in thehypoxia-induced BBB permeability are notcompletely understood. Work in animal modelsof stroke has identified that there is a biphasicleakage of the BBB, with an early opening with-in hours following hypoxia/ischemia, followedby a refractory phase and then a second openingthe next day (Kuroiwa et al. 1985; Huang et al.1999). In addition, analysis in transgenic mod-els has identified that there are stepwise alter-ations in the BBB, with an increase in trans-cytosis observed first followed by alterations inthe TJs (Knowland et al. 2014). There are alsoimportant changes in ion channel and effluxtransporter expression and activity.
Focal cerebral ischemia damages elementsof the BBB and induces inflammatory processesthat alter the relationships of ECs, ECM, andastroglial cells. This results in profound changesin the microvascular permeability barrier. Focalincreases in permeability to fibrinogen, IgG,and other large proteins are detected within afew hours following middle cerebral artery oc-clusion (MCAO). Conversely, and surprisingly,hypoxic conditions induce expression of ZO-1in vitro and claudin-5 and occludin in vivo. Theexact functional consequences of these up-reg-ulations are not clear. Nevertheless, levels of EC-expressed integrins a1b1, a3b1, and a6b1 de-crease rapidly after MCAO and MMPs are acti-vated on ischemic insult, which induces basallamina remodeling, and also chemokine activa-tion. Finally, dystroglycan, expressed by astro-cyte, disappears after MCAO, a phenomenonresponsible for detachment of astrocyte endfeetand perivascular edema. These studies suggestthat adhesive interactions between the endothe-lium and the ECM contribute to the acute vas-cular remodeling seen in stroke.
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 15
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

Molecular Alterations of theTight Junctions
Clinically, strokes are known to cause an in-crease in vasogenic edema, which can be attrib-uted to an increase in BBB permeability. Recentin vitro studies have begun to elucidate themolecular changes leading to increases in BBBpermeability. In studies by Mark and Davis(2002) and Witt et al. (2008), an increase inactin protein levels and actin stress fibers wasobserved following hypoxic insult, whereashypoxia alone had no effect on protein expres-sion of the TJs, occludin, claudin-1, or ZO-1/2.Following hypoxia, reoxygenation increases ex-pression of occludin, claudin-1, and ZO-1/2.Changes in the cellular localization of the TJproteins occludin and ZO-1/2 following hyp-oxic insult were confirmed with dynamic con-focal microscopy recordings. Interestingly, thesechanges were reversible and returned to controllevels on reoxygenation.
Changes in junctional structure formationor stability are now known to involve up-regu-lation in vascular endothelial growth factor(VEGF), and inhibition of VEGF attenuatesthe hypoxia-induced increase in BBB perme-ability (Fischer et al. 2002; Schoch et al. 2002).In addition, hypoxia increases nitric oxide(NO) release by ECs and inhibition of NO syn-thase reduces the effect of hypoxia on cell per-meability. Although the exact mechanisms in-volved in the VEGF- and NO-mediated changesin EC permeability are still being investigated,some reports have shown that NO may directlymodify the TJ proteins by nitrosylation or nitro-sation.
MMPs and the BBB
MMPs are zinc-dependent proteases that havethe ability to degrade fibronectin and laminins.As the basal lamina is composed of collagen,fibronectin, laminin, and heparin sulfate, andserves as an important scaffold for brain ECs,MMPs have been considered as obvious initia-tors of BBB disruption. Following ischemia/re-perfusion, MMPs have been shown to be up-regulated in the brain (Lenglet et al. 2014), either
through proinflammatory cytokine pathways(via NF-kB) or through activation of HIF-1aand furin, which convert pro-MT-MMP intoactivated MT-MMP. More specifically, it hasbeen shown that MMP-9, MMP-3, and MMP-2 levels were increased following ischemia/re-perfusion, correlating with the increase in su-crose diffusion across the BBB. Additionally, in-hibition of MMP with pharmacological agentsor use of MMP knockout animals reduced BBBdisruption (Rosenberg et al. 1998). It remainsunclear whether MMP-mediated BBB disrup-tion occurs at the level of the basal lamina, orat the level of the TJ and AJ, as these junctionalproteins were also shown to be substrates ofMMPs.
Modulation of Channels and Transporters
Ion channels and transporters are key compo-nents of the BBB, which maintain cerebral phys-iological and metabolic homeostasis. As one ofthe major consequences of stroke is the forma-tion of cerebral vasogenic and cytotoxic edema,understanding the effect of stroke on the func-tion of channels and transporters at the BBBcould identify important therapeutic targets.
During ischemic stroke, there is an impor-tant release of glutamate from neurons that bindto N-methyl-D-aspartate (NMDA) receptors.This excess NMDA receptor activation is large-ly responsible for cytotoxic edema of neurons(Sharp et al. 2003). Studies have shown that BBBECs also express both NMDA and metabotropicglutamate receptors (Krizbai et al. 1998; Sharpet al. 2003). Circulating inflammatory media-tors have also been shown to stimulate a releaseof glutamate, which disrupts the BBB viametabotropic receptors (Collard et al. 2002).Interestingly, in vitro studies showed thatNMDA receptor activation reduces BBB integ-rity, whereas activation of metabotropic recep-tors increased BBB electrical resistance suggest-ing a tightening of the BBB.
The activity of exchangers and transporters,such as the Naþ/Hþ exchanger (NHE), Naþ/Kþ ATPase, and Naþ/Kþ/Cl2 cotransporter,contribute to maintaining ion balance at theBBB and in the brain in general. During stroke,
R. Daneman and A. Prat
16 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

osmotic and ion balance are altered, leading toactivation of ion transporters and exchangers.
Regulation of the BBB in AD
Dysfunction of cerebral vascular ECs and leu-kocyte transmigration across the BBB probablyparticipate in the development of AD, Parkin-son’s disease (PD), and other neurodegenera-tive diseases. As multidrug resistance functionat the level of the BBB decreases with age, de-creased clearance of neurotoxic compounds andincreased oxidative stress in the brain increasesthe risk of neurodegenerative pathology.
Arterial spin labeling magnetic resonanceimaging (MRI), functional blood-oxygen-lev-el-dependent (BOLD)-MRI, fluorodeoxyglu-cose-positron emission tomography (FDG-PET), and single-photon emission computer-ized tomography (SPECT) studies in humansshow that cerebral blood flow is significantlyreduced first in mild cognitive impairment andthen in AD. Amyloid b is transported from theblood to the brain by the receptor for advancedglycation endproducts (RAGE), which is ex-pressed on BBB-ECs. Conversely, both solubleLRP and ApoE are cell-surface Ab chaperonesthat associate with clearance receptors and pro-mote extrusion of Ab from the brain back intothe blood through the BBB. In AD, these clear-ance pathways seem to be altered, which is hy-pothesized to lead to accumulation of solubleAb in the perivascular space and the formationof toxic oligomeric Ab. Ab deposition in thevascular smooth muscle cell layer and Abplaque formation around vessels of AD patientshas been well documented, and participate inthe pathology of cerebral amyloid angiopathy,an entity strongly linked to AD. Soluble amyloidb is also known to stimulate the transmigrationof monocytes, to enhance tau pathology, to in-duce secretion of proinflammatory cytokines(TNF and IL-6) and chemokines, to activateMT1-MMP, the activator of MMP-2, to stimu-late production of MMP-9, and to activate pro-duction of reactive oxygen species (ROS) wheninjected by microdialysis in vivo. Patients withAD have also been reported to have focal vascu-lar defects in the CNS, such as vascular “regres-
sion,” reduced capillary density, accumulationof collagen, perlecan in the basal lamina, re-duced mitochondrial content, and loss of TJand AJ proteins. These might well be causedby Ab accumulation and BBB dysfunction, al-though it has not been proven.
Summary
In addition, BBB disruption has been observedin a series of other neurological diseases includ-ing amyotrophic lateral sclerosis (ALS), epilep-sy, edema, brain traumas, PD, as well as systemicdiseases, such as liver failure (Daneman 2012).A major question remains whether there is acommon mechanism for BBB disruption dur-ing all different diseases, or whether the dys-function in each disease results from differentcellular and molecular mechanisms. Several dif-ferent signaling pathways have been shown to beimportant for BBB disruption across multiplepathologies including VEGF, reactive oxygenspecies, TNF-a, and MMP-mediated disrup-tion of TJs and ECM, but it remains unknownhow different triggers may engage these path-ways, and how different outcomes can be ob-served in different diseases. As with studyingBBB formation, one of the major issues whenanalyzing studies of BBB dysfunction is thateach study uses different measures of the BBB,thus making it difficult to compare the dysfunc-tion during the disease. What is clear is thatdisruption of the BBB in many of these diseasesappears to be multimodal, with increasing ves-icle trafficking, disruption of tight junctionstrands, and alterations of endothelial transportand metabolic processes. What remains unclearis how each of these processes interacts witheach other. For instance, an increase in trans-cytosis precedes TJ disruption following stroke,but it is not clear whether this increased vesicletrafficking actually leads to the removal of junc-tion proteins and transporters from the cell sur-face. Furthermore, it remains unclear what thecellular signaling events that coordinate theseprocesses are. Is the BBB disruption a result ofa loss of pericyte and astrocyte signals includ-ing Wnt, SHH, and others, or is it because ofreception of disruption signals from neural or
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 17
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

immune cells? In the future, a more exhaustiveanalysis of the BBB at different stages of eachdisease as well as large-scale “omics” analysis ofchanges to the BBB in each disease will clarifythis important question.
It is clear that there is BBB dysfunction inmany different neurological diseases in a widevariety of species, and, thus, this is an evolution-ary conserved important feature of these diseas-es. A critical question moving forward is to un-derstand what aspects of this BBB dysfunctionare healing and what aspects are pathological.Like any inflammatory event, a small amountis likely helpful in clearing debris, fighting path-ogens, and aiding in wound healing, whereas alarge amount can be debilitating causing tissuedysfunction and degeneration. Thus, under-standing the molecular mechanisms regulatingBBB breakdown and developing methods to ap-propriately modulate this process will be criticalin developing therapeutics to aid in the repairprocess of these diseases.
CONCLUSIONS
The BBB is an important cellular barrier thattightly controls the microenvironment of theCNS to allow for proper neuronal function.This barrier is an extremely important factorto consider when determining treatments fordifferent neurological diseases, both becausedisruption of the BBB can lead to severe pathol-ogy observed in many different diseases, but alsobecause crossing the BBB is an essential consid-eration in the development of CNS-acting ther-apeutics. Recent work has identified many mol-ecules required for BBB function as well as manyof the cellular and molecular signaling eventsthat regulate the formation of the BBB duringdevelopment, its function in adulthood, andits response to injury and disease (Fig. 2). Al-though much progress has been made, manyquestions still remain. Are all of the differentproperties of the BBB regulated by the samepathways or different pathways? How are differ-ent signaling pathways coordinated to regulatedifferent aspects of the BBB? Which pathwaysinduce properties of the BBB during develop-ment, and which are required throughout life
for maintenance of the barrier? How dynamicis the BBB? Are different BBB properties, includ-ing the transport and tight junctions, dynami-cally regulated in response to neural activity?How do alterations in the BBB affect neuronalactivity, brain function, and behavior? Arethere localized specialties of the BBB that regu-late regional neuronal development or func-tion? What leads to loss of BBB properties dur-ing neurological disease, a loss of maintenancesignals or the presence of disruption signals?Understanding these questions will allow forthe development of therapeutics to modulatethe BBB both to restore its function during neu-rological disease and to develop methods to by-pass the BBB for drug delivery (Fig. 3).
REFERENCES
Abbott NJ, Khan EU, Rollinson CM, Reichel A, Janigro D,Dombrowski SM, Dobbie MS, Begley DJ. 2002. Drugresistance in epilepsy: The role of the blood–brain bar-rier. Novartis Found Symp 243: 38–47; discussion 47–53,180–185.
Abbott NJ, Ronnback L, Hansson E. 2006. Astrocyte–endo-thelial interactions at the blood–brain barrier. Nat RevNeurosci 7: 41–53.
Agrawal S, Anderson P, Durbeej M, van Rooijen N, Ivars F,Opdenakker G, Sorokin LM. 2006. Dystroglycan is selec-tively cleaved at the parenchymal basement membraneat sites of leukocyte extravasation in experimental auto-immune encephalomyelitis. J Exp Med 203: 1007–1019.
Aird WC. 2007a. Phenotypic heterogeneity of the endothe-lium: II. Representative vascular beds. Circ Res 100: 174–190.
Aird WC. 2007b. Phenotypic heterogeneity of the endothe-lium: I. Structure, function, and mechanisms. Circ Res100: 158–173.
Ajami B, Bennett JL, Krieger C, Tetzlaff W, Rossi FM. 2007.Local self-renewal can sustain CNS microglia mainte-nance and function throughout adult life. Nat Neurosci10: 1538–1543.
Alvarez JI, Dodelet-Devillers A, Kebir H, Ifergan I, Fabre PJ,Terouz S, Sabbagh M, Wosik K, Bourbonniere L, BernardM, et al. 2011a. The Hedgehog pathway promotesblood–brain barrier integrity and CNS immune quies-cence. Science 334: 1727–1731.
Alvarez JI, Cayrol R, Prat A. 2011b. Disruption of centralnervous system barriers in multiple sclerosis. BiochimBiophys Acta 1812: 252–264.
Alvarez JI, Katayama T, Prat A. 2013. Glial influence on theblood brain barrier. Glia 61: 1939–1958.
Amasheh S, Schmidt T, Mahn M, Florian P, Mankertz J,Tavalali S, Gitter AH, Schulzke JD, Fromm M. 2005.Contribution of claudin-5 to barrier properties in tightjunctions of epithelial cells. Cell Tissue Res 321: 89–96.
R. Daneman and A. Prat
18 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

Argaw AT, Gurfein BT, Zhang Y, Zameer A, John GR. 2009.VEGF-mediated disruption of endothelial CLN-5 pro-motes blood–brain barrier breakdown. Proc Natl AcadSci 106: 1977–1982.
Argaw AT, Asp L, Zhang J, Navrazhina K, Pham T, MarianiJN, Mahase S, Dutta DJ, Seto J, Kramer EG, et al. 2012.Astrocyte-derived VEGF-A drives blood–brain barrierdisruption in CNS inflammatory disease. J Clin Invest122: 2454–2468.
Armulik A, Genove G, Mae M, Nisancioglu MH, Wallgard E,Niaudet C, He L, Norlin J, Lindblom P, Strittmatter K, etal. 2010. Pericytes regulate the blood–brain barrier. Na-ture 468: 557–561.
Armulik A, Genove G, Betsholtz C. 2011. Pericytes: Devel-opmental, physiological, and pathological perspectives,problems, and promises. Dev Cell 21: 193–215.
Attwell D, Buchan AM, Charpak S, Lauritzen M, MacvicarBA, Newman EA. 2010. Glial and neuronal control ofbrain blood flow. Nature 468: 232–243.
Balda MS, Whitney JA, Flores C, Gonzalez S, Cereijido M,Matter K. 1996. Functional dissociation of paracellularpermeability and transepithelial electrical resistance anddisruption of the apical-basolateral intramembrane dif-fusion barrier by expression of a mutant tight junctionmembrane protein. J Cell Biol 134: 1031–1049.
Betz AL, Goldstein GW. 1978. Polarity of the blood–brainbarrier: Neutral amino acid transport into isolated braincapillaries. Science 202: 225–227.
Betz AL, Firth JA, Goldstein GW. 1980. Polarity of theblood–brain barrier: Distribution of enzymes betweenthe luminal and antiluminal membranes of brain capil-lary endothelial cells. Brain Res 192: 17–28.
Biernacki K, Prat A, Blain M, Antel JP. 2001. Regulation ofTh1 and Th2 lymphocyte migration by human adultbrain endothelial cells. J Neuropathol Exp Neurol 60:1127–1136.
Brightman MW, Reese TS. 1969. Junctions between inti-mately apposed cell membranes in the vertebrate brain.J Cell Biol 40: 648–677.
Cayrol R, Wosik K, Berard JL, Dodelet-Devillers A, Ifergan I,Kebir H, Haqqani AS, Kreymborg K, Krug S, MoumdjianR, et al. 2008. Activated leukocyte cell adhesion moleculepromotes leukocyte trafficking into the central nervoussystem. Nat Immunol 9: 137–145.
Chen XL, Dodd G, Thomas S, Zhang X, Wasserman MA,Rovin BH, Kunsch C. 2006. Activation of Nrf2/AREpathway protects endothelial cells from oxidant injuryand inhibits inflammatory gene expression. Am J PhysiolHeart Circ Physiol 290: H1862–H1870.
Chen J, Stahl A, Krah NM, Seaward MR, Dennison RJ, Sa-pieha P, Hua J, Hatton CJ, Juan AM, Aderman CM, et al.2011. Wnt signaling mediates pathological vasculargrowth in proliferative retinopathy. Circulation 124:1871–1881.
Colegio OR, Van Itallie C, Rahner C, Anderson JM. 2003.Claudin extracellular domains determine paracellularcharge selectivity and resistance but not tight junctionfibril architecture. Am J Physiol Cell Physiol 284: C1346–C1354.
Collard CD, Park KA, Montalto MC, Alapati S, Buras JA,Stahl GL, Colgan SP. 2002. Neutrophil-derived glutamate
regulates vascular endothelial barrier function. J BiolChem 277: 14801–14811.
Conway EM, Carmeliet P. 2004. The diversity of endothelialcells: A challenge for therapeutic angiogenesis. GenomeBiol 5: 207.
Coomber BL, Stewart PA. 1985. Morphometric analysis ofCNS microvascular endothelium. Microvasc Res 30: 99–115.
Cordon-Cardo C, O’Brien JP, Casals D, Rittman-Grauer L,Biedler JL, Melamed MR, Bertino JR. 1989. Multidrug-resistance gene (P-glycoprotein) is expressed by endothe-lial cells at blood–brain barrier sites. Proc Natl Acad Sci86: 695–698.
Cornford EM, Hyman S, Swartz BE. 1994. The human brainGLUT1 glucose transporter: Ultrastructural localizationto the blood–brain barrier endothelia. J Cereb Blood FlowMetab 14: 106–112.
Courtoy PJ, Boyles J. 1983. Fibronectin in the microvascu-lature: Localization in the pericyte-endothelial intersti-tium. J Ultrastruct Res 83: 258–273.
Cuevas P, Gutierrez-Diaz JA, Reimers D, Dujovny M, DiazFG, Ausman JI. 1984. Pericyte endothelial gap junctionsin human cerebral capillaries. Anat Embryol (Berl) 170:155–159.
Daneman R. 2012. The blood–brain barrier in health anddisease. Ann Neurol 72: 648–672.
Daneman R, Agalliu D, Zhou L, Kuhnert F, Kuo CJ, BarresBA. 2009. Wnt/b-catenin signaling is required for CNS,but not non-CNS, angiogenesis. Proc Natl Acad Sci 106:641–646.
Daneman R, Zhou L, Agalliu D, Cahoy JD, Kaushal A, BarresBA. 2010a. The mouse blood–brain barrier transcrip-tome: A new resource for understanding the develop-ment and function of brain endothelial cells. PLoS ONE5: e13741.
Daneman R, Zhou L, Kebede AA, Barres BA. 2010b. Peri-cytes are required for blood–brain barrier integrity dur-ing embryogenesis. Nature 468: 562–566.
Del Zoppo GJ, Milner R, Mabuchi T, Hung S, Wang X,Koziol JA. 2006. Vascular matrix adhesion and theblood–brain barrier. Biochem Soc Trans 34: 1261–1266.
De Vivo DC, Trifiletti RR, Jacobson RI, Ronen GM, Beh-mand RA, Harik SI. 1991. Defective glucose transportacross the blood–brain barrier as a cause of persistenthypoglycorrhachia, seizures, and developmental delay.N Engl J Med 325: 703–709.
De Vivo DC, Leary L, Wang D. 2002. Glucose transporter 1deficiency syndrome and other glycolytic defects. J ChildNeurol 17: 3S15–3S23; discussion 3S24–3S25.
Diaz-Flores L, Gutierrez R, Madrid JF, Varela H, Valladares F,Acosta E, Martın-Vasallo P, Dıaz-Flores L Jr. 2009. Peri-cytes. Morphofunction, interactions and pathology in aquiescent and activated mesenchymal cell niche. HistolHistopathol 24: 909–969.
Dodelet-Devillers A, Cayrol R, van Horssen J, Haqqani AS,de Vries HE, Engelhardt B, Greenwood J, Prat A. 2009.Functions of lipid raft membrane microdomains at theblood–brain barrier. J Mol Med (Berl) 87: 765–774.
Dohgu S, Yamauchi A, Takata F, Naito M, Tsuruo T, HiguchiS, Sawada Y, Kataoka Y. 2004. Transforming growth fac-tor-b1 upregulates the tight junction and P-glycoprotein
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 19
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

of brain microvascular endothelial cells. Cell Mol Neuro-biol 24: 491–497.
Enerson BE, Drewes LR. 2006. The rat blood–brain barriertranscriptome. J Cereb Blood Flow Metab 26: 959–973.
Engelhardt B. 2008. Immune cell entry into the central ner-vous system: Involvement of adhesion molecules andchemokines. J Neurol Sci 274: 23–26.
Engelhardt B, Sorokin L. 2009. The blood–brain and theblood–cerebrospinal fluid barriers: Function and dys-function. Semin Immunopathol 31: 497–511.
Fan X, Staitieh BS, Jensen JS, Mould KJ, Greenberg JA, JoshiPC, Koval M, Guidot DM. 2013. Activating the Nrf2-mediated antioxidant response element restores barrierfunction in the alveolar epithelium of HIV-1 transgenicrats. Am J Physiol Lung Cell Mol Physiol 305: L267–L277.
Fischer S, Wobben M, Marti HH, Renz D, Schaper W. 2002.Hypoxia-induced hyperpermeability in brain microves-sel endothelial cells involves VEGF-mediated changes inthe expression of zonula occludens-1. Microvasc Res 63:70–80.
Fischer S, Wiesnet M, Marti HH, Renz D, Schaper W. 2004.Simultaneous activation of several second messengers inhypoxia-induced hyperpermeability of brain derived en-dothelial cells. J Cell Physiol 198: 359–369.
Fontijn RD, Volger OL, Fledderus JO, Reijerkerk A, de VriesHE, Horrevoets AJ. 2008. SOX-18 controls endothelial-specific claudin-5 gene expression and barrier function.Am J Physiol Heart Circ Physiol 294: H891–H900.
Furuse M. 2010. Molecular basis of the core structure oftight junctions. Cold Spring Harb Perspect Biol 2:a002907.
Furuse M, Sasaki H, Fujimoto K, Tsukita S. 1998. A singlegene product, claudin-1 or -2, reconstitutes tight junc-tion strands and recruits occludin in fibroblasts. J CellBiol 143: 391–401.
Furuse M, Furuse K, Sasaki H, Tsukita S. 2001. Conversionof zonulae occludentes from tight to leaky strand type byintroducing claudin-2 into Madin-Darby canine kidney Icells. J Cell Biol 153: 263–272.
Furuse M, Hata M, Furuse K, Yoshida Y, Haratake A, Sugi-tani Y, Noda T, Kubo A, Tsukita S. 2002. Claudin-basedtight junctions are crucial for the mammalian epidermalbarrier: A lesson from claudin-1-deficient mice. J CellBiol 156: 1099–111.
Gerhardt H, Wolburg H, Redies C. 2000. N-cadherin medi-ates pericytic–endothelial interaction during brain an-giogenesis in the chicken. Dev Dyn 218: 472–479.
Ghandour MS, Langley OK, Zhu XL, Waheed A, Sly WS.1992. Carbonic anhydrase IVon brain capillary endothe-lial cells: A marker associated with the blood–brain bar-rier. Proc Natl Acad Sci 89: 6823–6827.
Ginhoux F, Greter M, Leboeuf M, Nandi S, See P, Gokhan S,Mehler MF, Conway SJ, Ng LG, Stanley ER, et al. 2010.Fate mapping analysis reveals that adult microglia derivefrom primitive macrophages. Science 330: 841–845.
Gordon GR, Howarth C, MacVicar BA. 2011. Bidirectionalcontrol of arteriole diameter by astrocytes. Exp Physiol96: 393–399.
Gow A, Southwood CM, Li JS, Pariali M, Riordan GP, BrodieSE, Danias J, Bronstein JM, Kachar B, Lazzarini RA. 1999.
CNS myelin and sertoli cell tight junction strands areabsent in Osp/claudin-11 null mice. Cell 99: 649–659.
Greenwood J, Heasman SJ, Alvarez JI, Prat A, Lyck R, En-gelhardt B. 2011. Review: Leucocyte-endothelial cellcrosstalk at the blood–brain barrier: A prerequisite forsuccessful immune cell entry to the brain. NeuropatholAppl Neurobiol 37: 24–39.
Gu Y, Zheng G, Xu M, Li Y, Chen X, Zhu W, Tong Y, ChungSK, Liu KJ, Shen J. 2012. Caveolin-1 regulates nitric ox-ide-mediated matrix metalloproteinases activity andblood–brain barrier permeability in focal cerebral ische-mia and reperfusion injury. J Neurochem 120: 147–156.
Gupta IR, Ryan AK. 2010. Claudins: Unlocking the code totight junction function during embryogenesis and in dis-ease. Clin Genet 77: 314–325.
Ha SN, Hochman J, Sheridan RP. 2007. Mini review onmolecular modeling of P-glycoprotein (Pgp). Curr TopMed Chem 7: 1525–1529.
Hadj-Rabia S, Baala L, Vabres P, Hamel-Teillac D, JacqueminE, Fabre M, Lyonnet S, De Prost Y, Munnich A, Had-chouel M, et al. 2004. Claudin-1 gene mutations in neo-natal sclerosing cholangitis associated with ichthyosis: Atight junction disease. Gastroenterology 127: 1386–1390.
Halilagic A, Ribes V, Ghyselinck NB, Zile MH, Dolle P,Studer M. 2007. Retinoids control anterior and dorsalproperties in the developing forebrain. Dev Biol 303:362–375.
Hall CN, Reynell C, Gesslein B, Hamilton NB, Mishra A,Sutherland BA, O’Farrell FM, Buchan AM, Lauritzen M,Attwell D. 2014. Capillary pericytes regulate cerebralblood flow in health and disease. Nature 508: 55–60.
Hampson G, Konrad MA, Scoble J. 2008. Familial hypo-magnesaemia with hypercalciuria and nephrocalcinosis(FHHNC): Compound heterozygous mutation in theclaudin 16 (CLDN16) gene. BMC Nephrol 9: 12.
Henninger DD, Panes J, Eppihimer M, Russell J, GerritsenM, Anderson DC, Granger DN. 1997. Cytokine-inducedVCAM-1 and ICAM-1 expression in different organs ofthe mouse. J Immunol 158: 1825–1832.
Hickey WF, Kimura H. 1988. Perivascular microglial cells ofthe CNS are bone marrow-derived and present antigen invivo. Science 239: 290–292.
Hong JY, Park JI, Cho K, Gu D, Ji H, Artandi SE, McCrea PD.2010. Shared molecular mechanisms regulate multiplecatenin proteins: Canonical Wnt signals and componentsmodulate p120–catenin isoform-1 and additional p120subfamily members. J Cell Sci 123: 4351–4365.
Hou J, Gomes AS, Paul DL, Goodenough DA. 2006. Study ofclaudin function by RNA interference. J Biol Chem 281:36117–36123.
Huang ZG, Xue D, Preston E, Karbalai H, Buchan AM. 1999.Biphasic opening of the blood–brain barrier followingtransient focal ischemia: Effects of hypothermia. Can JNeurol Sci 26: 298–304.
Huang J, Upadhyay UM, Tamargo RJ. 2006. Inflammationin stroke and focal cerebral ischemia. Surg Neurol 66:232–245.
Hudson LC, Bragg DC, Tompkins MB, Meeker RB. 2005.Astrocytes and microglia differentially regulate traffick-ing of lymphocyte subsets across brain endothelial cells.Brain Res 1058: 148–160.
R. Daneman and A. Prat
20 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

Janzer RC, Raff MC. 1987. Astrocytes induce blood–brainbarrier properties in endothelial cells. Nature 325: 253–257.
Johnson-Leger CA, Aurrand-Lions M, Beltraminelli N, FaselN, Imhof BA. 2002. Junctional adhesion molecule-2(JAM-2) promotes lymphocyte transendothelial migra-tion. Blood 100: 2479–2486.
Katsimpardi L, Litterman NK, Schein PA, Miller CM, Lof-fredo FS, Wojtkiewicz GR, Chen JW, Lee RT, Wagers AJ,Rubin LL. 2014. Vascular and neurogenic rejuvenation ofthe aging mouse brain by young systemic factors. Science344: 630–634.
Kebir H, Kreymborg K, Ifergan I, Dodelet-Devillers A,Cayrol R, Bernard M, Giuliani F, Arbour N, Becher B,Prat A. 2007. Human TH17 lymphocytes promoteblood–brain barrier disruption and central nervous sys-tem inflammation. Nat Med 13: 1173–1175.
Keuschnigg J, Henttinen T, Auvinen K, Karikoski M, SalmiM, Jalkanen S. 2009. The prototype endothelial markerPAL-E is a leukocyte trafficking molecule. Blood 114:478–484.
Knohl SJ, Scheinman SJ. 2004. Inherited hypercalciuric syn-dromes: Dent’s disease (CLC-5) and familial hypomag-nesemia with hypercalciuria (paracellin-1). Semin Neph-rol 24: 55–60.
Knowland D, Arac A, Sekiguchi KJ, Hsu M, Lutz SE, PerrinoJ, Steinberg GK, Barres BA, Nimmerjahn A, Agalliu D.2014. Stepwise recruitment of transcellular and paracel-lular pathways underlies blood–brain barrier breakdownin stroke. Neuron 82: 603–617.
Krizbai IA, Deli MA, Pestenacz A, Siklos L, Szabo CA, And-ras I, Joo F. 1998. Expression of glutamate receptors oncultured cerebral endothelial cells. J Neurosci Res 54:814–819.
Kuroiwa T, Ting P, Martinez H, Klatzo I. 1985. The biphasicopening of the blood–brain barrier to proteins followingtemporary middle cerebral artery occlusion. Acta Neuro-pathol 68: 122–129.
Larochelle C, Alvarez JI, Prat A. 2011. How do immune cellsovercome the blood–brain barrier in multiple sclerosis?FEBS Lett 585: 3770–3780.
Larsen JM, Martin DR, Byrne ME. 2014. Recent advances indelivery through the blood–brain barrier. Curr Top MedChem 14: 1148–1160.
Larson DM, Carson MP, Haudenschild CC. 1987. Junctionaltransfer of small molecules in cultured bovine brain mi-crovascular endothelial cells and pericytes. Microvasc Res34: 184–199.
Lee S, Chen TT, Barber CL, Jordan MC, Murdock J, Desai S,Ferrara N, Nagy A, Roos KP, Iruela-Arispe ML. 2007.Autocrine VEGF signaling is required for vascular ho-meostasis. Cell 130: 691–703.
Lenglet S, Montecucco F, Mach F, Schaller K, Gasche Y,Copin JC. 2014. Analysis of the expression of nine secret-ed matrix metalloproteinases and their endogenous in-hibitors in the brain of mice subjected to ischaemicstroke. Thromb Haemost 112: 363–378.
Li JY, Boado RJ, Pardridge WM. 2001. Blood–brain barriergenomics. J Cereb Blood Flow Metab 21: 61–68.
Li JY, Boado RJ, Pardridge WM. 2002. Rat blood–brainbarrier genomics: II. J Cereb Blood Flow Metab 22:1319–1326.
Liebner S, Corada M, Bangsow T, Babbage J, Taddei A, Czu-palla CJ, Reis M, Felici A, Wolburg H, Fruttiger M, et al.2008. Wnt/b-catenin signaling controls development ofthe blood–brain barrier. J Cell Biol 183: 409–417.
Liu LB, Xue YX, Liu YH. 2010. Bradykinin increases thepermeability of the blood-tumor barrier by the caveo-lae-mediated transcellular pathway. J Neurooncol 99:187–194.
Loscher W, Potschka H. 2005. Blood–brain barrier activeefflux transporters: ATP-binding cassette gene family.NeuroRx 2: 86–98.
Ludwig RJ, Zollner TM, Santoso S, Hardt K, Gille J, Baatz H,Johann PS, Pfeffer J, Radeke HH, Schon MP, et al. 2005.Junctional adhesion molecules (JAM)-B and -C contrib-ute to leukocyte extravasation to the skin and mediatecutaneous inflammation. J Invest Dermatol 125: 969–976.
Luo J, Ho P, Steinman L, Wyss-Coray T. 2008. Biolumines-cence in vivo imaging of autoimmune encephalomyelitispredicts disease. J Neuroinflammation 5: 6.
Majesky MW. 2007. Developmental basis of vascularsmooth muscle diversity. Arterioscler Thromb Vasc Biol27: 1248–1258.
Mark KS, Davis TP. 2002. Cerebral microvascular changes inpermeability and tight junctions induced by hypoxia-re-oxygenation. Am J Physiol Heart Circ Physiol 282:H1485–H1494.
Martin-Padura I, Lostaglio S, Schneemann M, Williams L,Romano M, Fruscella P, Panzeri C, Stoppacciaro A, RucoL, Villa A, et al. 1998. Junctional adhesion molecule, anovel member of the immunoglobulin superfamily thatdistributes at intercellular junctions and modulatesmonocyte transmigration. J Cell Biol 142: 117–127.
Masuda S, Oda Y, Sasaki H, Ikenouchi J, Higashi T, AkashiM, Nishi E, Furuse M. 2011. LSR defines cell corners fortricellular tight junction formation in epithelial cells. JCell Sci 124: 548–555.
McCarthy KM, Skare IB, Stankewich MC, Furuse M, TsukitaS, Rogers RA, Lynch RD, Schneeberger EE. 1996. Occlu-din is a functional component of the tight junction. J CellSci 109: 2287–2298.
Mittapalli RK, Manda VK, Adkins CE, Geldenhuys WJ,Lockman PR. 2010. Exploiting nutrient transporters atthe blood–brain barrier to improve brain distribution ofsmall molecules. Ther Deliv 1: 775–784.
Miyamoto T, Morita K, Takemoto D, Takeuchi K, Kitano Y,Miyakawa T, Nakayama K, Okamura Y, Sasaki H, MiyachiY, et al. 2005. Tight junctions in Schwann cells of periph-eral myelinated axons: A lesson from claudin-19-defi-cient mice. J Cell Biol 169: 527–538.
Mizee MR, Wooldrik D, Lakeman KA, van het Hof B, Drex-hage JA, Geerts D, Bugiani M, Aronica E, Mebius RE, PratA, et al. 2013. Retinoic acid induces blood–brain barrierdevelopment. J Neurosci 33: 1660–1671.
Morita K, Sasaki H, Furuse M, Tsukita S. 1999. Endothelialclaudin: Claudin-5/TMVCF constitutes tight junctionstrands in endothelial cells. J Cell Biol 147: 185–194.
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 21
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

Murakami M, Nguyen LT, Zhuang ZW, Moodie KL, Carme-liet P, Stan RV, Simons M. 2008. The FGF system has a keyrole in regulating vascular integrity. J Clin Invest 118:3355–3366.
Nitta T, Hata M, Gotoh S, Seo Y, Sasaki H, Hashimoto N,Furuse M, Tsukita S. 2003. Size-selective loosening of theblood–brain barrier in claudin-5-deficient mice. J CellBiol 161: 653–660.
Noell S, Wolburg-Buchholz K, Mack AF, Beedle AM, Satz JS,Campbell KP, Wolburg H, Fallier-Becker P. 2011. Evi-dence for a role of dystroglycan regulating the membranearchitecture of astroglial endfeet. Eur J Neurosci 33:2179–2186.
Nourhaghighi N, Teichert-Kuliszewska K, Davis J, StewartDJ, Nag S. 2003. Altered expression of angiopoietins dur-ing blood–brain barrier breakdown and angiogenesis.Lab Invest 83: 1211–1222.
Ohtsuki S, Hirayama M, Ito S, Uchida Y, Tachikawa M,Terasaki T. 2014. Quantitative targeted proteomics forunderstanding the blood–brain barrier: Towards phar-macoproteomics. Expert Rev Proteomics 11: 303–313.
Oldendorf WH, Cornford ME, Brown WJ. 1977. The largeapparent work capability of the blood–brain barrier: Astudy of the mitochondrial content of capillary endothe-lial cells in brain and other tissues of the rat. Ann Neurol 1:409–417.
Orlowski M, Sessa G, Green JP. 1974. g-Glutamyl transpep-tidase in brain capillaries: Possible site of a blood–brainbarrier for amino acids. Science 184: 66–68.
Paschaki M, Lin SC, Wong RL, Finnell RH, Dolle P, Nieder-reither K. 2012. Retinoic acid-dependent signaling path-ways and lineage events in the developing mouse spinalcord. PLoS ONE 7: e32447.
Peppiatt CM, Howarth C, Mobbs P, Attwell D. 2006. Bidirec-tional control of CNS capillary diameter by pericytes.Nature 443: 700–704.
Persidsky Y, Ghorpade A, Rasmussen J, Limoges J, Liu XJ,Stins M, Fiala M, Way D, Kim KS, Witte MH, et al. 1999.Microglial and astrocyte chemokines regulate monocytemigration through the blood–brain barrier in humanimmunodeficiency virus-1 encephalitis. Am J Pathol155: 1599–1611.
Polfliet MM, Zwijnenburg PJ, van Furth AM, van der Poll T,Dopp EA, Renardel de Lavalette C, van Kesteren-Hen-drikx EM, van Rooijen N, Dijkstra CD, van den Berg TK.2001. Meningeal and perivascular macrophages of thecentral nervous system play a protective role during bac-terial meningitis. J Immunol 167: 4644–4650.
Potschka H, Fedrowitz M, Loscher W. 2001. P-glycoproteinand multidrug resistance-associated protein are involvedin the regulation of extracellular levels of the major anti-epileptic drug carbamazepine in the brain. Neuroreport12: 3557–3560.
Prat A, Biernacki K, Wosik K, Antel JP. 2001. Glial cell in-fluence on the human blood–brain barrier. Glia 36:145–155.
Reese TS, Karnovsky MJ. 1967. Fine structural localizationof a blood–brain barrier to exogenous peroxidase. J CellBiol 34: 207–217.
Reuss B, Dono R, Unsicker K. 2003. Functions of fibroblastgrowth factor (FGF)-2 and FGF-5 in astroglial differen-
tiation and blood–brain barrier permeability: Evidencefrom mouse mutants. J Neurosci 23: 6404–6412.
Rosenberg GA, Estrada EY, Dencoff JE. 1998. Matrix metal-loproteinases and TIMPs are associated with blood–brain barrier opening after reperfusion in rat brain. Stroke29: 2189–2195.
Saitou M, Furuse M, Sasaki H, Schulzke JD, Fromm M,Takano H, Noda T, Tsukita S. 2000. Complex phenotypeof mice lacking occludin, a component of tight junctionstrands. Mol Biol Cell 11: 4131–4142.
Schinkel AH, Smit JJ, van Tellingen O, Beijnen JH, WagenaarE, van Deemter L, Mol CA, van der Valk MA, Robanus-Maandag EC, te Riele HP, et al. 1994. Disruption of themouse mdr1a P-glycoprotein gene leads to a deficiencyin the blood–brain barrier and to increased sensitivityto drugs. Cell 77: 491–502.
Schinkel AH, Wagenaar E, van Deemter L, Mol CA, Borst P.1995. Absence of the mdr1a P-Glycoprotein in mice af-fects tissue distribution and pharmacokinetics of dexa-methasone, digoxin, and cyclosporin A. J Clin Invest 96:1698–1705.
Schinkel AH, Wagenaar E, Mol CA, van Deemter L. 1996. P-glycoprotein in the blood–brain barrier of mice influ-ences the brain penetration and pharmacological activityof many drugs. J Clin Invest 97: 2517–2524.
Schoch HJ, Fischer S, Marti HH. 2002. Hypoxia-inducedvascular endothelial growth factor expression causes vas-cular leakage in the brain. Brain 125: 2549–2557.
Sharp CD, Hines I, Houghton J, Warren A, Jackson TH IV,Jawahar A, Nanda A, Elrod JW, Long A, Chi A, et al. 2003.Glutamate causes a loss in human cerebral endothelialbarrier integrity through activation of NMDA receptor.Am J Physiol Heart Circ Physiol 285: H2592–H2598.
Shen F, Walker EJ, Jiang L, Degos V, Li J, Sun B, Heriyanto F,Young WL, Su H. 2011. Coexpression of angiopoietin-1with VEGF increases the structural integrity of theblood–brain barrier and reduces atrophy volume. J CerebBlood Flow Metab 31: 2343–2351.
Shepro D, Morel NM. 1993. Pericyte physiology. FASEB J 7:1031–1038.
Shue EH, Carson-Walter EB, Liu Y, Winans BN, Ali ZS,Chen J, Walter KA. 2008. Plasmalemmal vesicle associat-ed protein-1 (PV-1) is a marker of blood–brain barrierdisruption in rodent models. BMC Neurosci 9: 29.
Sims DE. 1986. The pericyte—A review. Tissue Cell 18: 153–174.
Sorokin L. 2010. The impact of the extracellular matrix oninflammation. Nat Rev Immunol 10: 712–723.
Stenman JM, Rajagopal J, Carroll TJ, Ishibashi M, McMa-hon J, McMahon AP. 2008. Canonical Wnt signaling reg-ulates organ-specific assembly and differentiation of CNSvasculature. Science 322: 1247–1250.
Stewart PA, Wiley MJ. 1981. Developing nervous tissue in-duces formation of blood–brain barrier characteristics ininvading endothelial cells: A study using quail–chicktransplantation chimeras. Dev Biol 84: 183–192.
Streit WJ, Conde JR, Fendrick SE, Flanary BE, Mariani CL.2005. Role of microglia in the central nervous system’simmune response. Neurol Res 27: 685–691.
Thiebaut F, Tsuruo T, Hamada H, Gottesman MM, Pastan I,Willingham MC. 1989. Immunohistochemical localiza-
R. Daneman and A. Prat
22 Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

tion in normal tissues of different epitopes in the multi-drug transport protein P170: Evidence for localization inbrain capillaries and crossreactivity of one antibody witha muscle protein. J Histochem Cytochem 37: 159–164.
Ufnal M, Skrzypecki J. 2014. Blood borne hormones in across-talk between peripheral and brain mechanisms reg-ulating blood pressure, the role of circumventricular or-gans. Neuropeptides 48: 65–73.
Unger ER, Sung JH, Manivel JC, Chenggis ML, Blazar BR,Krivit W. 1993. Male donor-derived cells in the brains offemale sex-mismatched bone marrow transplant recipi-ents: A Y-chromosome specific in situ hybridizationstudy. J Neuropathol Exp Neurol 52: 460–470.
Van Itallie CM, Anderson JM. 2006. Claudins and epithelialparacellular transport. Annu Rev Physiol 68: 403–429.
Van Itallie CM, Anderson JM. 2013. Claudin interactions inand out of the tight junction. Tissue Barriers 1: e25247.
Van Itallie C, Rahner C, Anderson JM. 2001. Regulated ex-pression of claudin-4 decreases paracellular conductancethrough a selective decrease in sodium permeability. JClin Invest 107: 1319–1327.
Van Itallie CM, Holmes J, Bridges A, Gookin JL, CoccaroMR, Proctor W, Colegio OR, Anderson JM. 2008. Thedensity of small tight junction pores varies among celltypes and is increased by expression of claudin-2. J CellSci 121: 298–305.
Vass K, Hickey WF, Schmidt RE, Lassmann H. 1993. Bonemarrow-derived elements in the peripheral nervous sys-tem. An immunohistochemical and ultrastructural inves-tigation in chimeric rats. Lab Invest 69: 275–282.
Villeda SA, Luo J, Mosher KI, Zou B, Britschgi M, Bieri G,Stan TM, Fainberg N, Ding Z, Eggel A, et al. 2011. Theageing systemic milieu negatively regulates neurogenesisand cognitive function. Nature 477: 90–94.
Villeda SA, Plambeck KE, Middeldorp J, Castellano JM,Mosher KI, Luo J, Smith LK, Bieri G, Lin K, Berdnik D,et al. 2014. Young blood reverses age-related impairmentsin cognitive function and synaptic plasticity in mice. NatMed 20: 659–663.
Wang Y, Imitola J, Rasmussen S, O’Connor KC, KhourySJ. 2008. Paradoxical dysregulation of the neural stemcell pathway Sonic Hedgehog-Gli1 in autoimmune en-cephalomyelitis and multiple sclerosis. Ann Neurol 64:417–427.
Wang Y, Rattner A, Zhou Y, Williams J, Smallwood PM,Nathans J. 2012. Norrin/Frizzled4 signaling in retinalvascular development and blood brain barrier plasticity.Cell 151: 1332–1344.
Westergaard E, Brightman MW. 1973. Transport of proteinsacross normal cerebral arterioles. J Comp Neurol 152: 17–44.
Williams K, Alvarez X, Lackner AA. 2001. Central nervoussystem perivascular cells are immunoregulatory cells thatconnect the CNS with the peripheral immune system.Glia 36: 156–164.
Witt KA, Mark KS, Sandoval KE, Davis TP. 2008. Reoxy-genation stress on blood–brain barrier paracellularpermeability and edema in the rat. Microvasc Res 75:91–96.
Wolburg H, Wolburg-Buchholz K, Fallier-Becker P, Noell S,Mack AF. 2011. Structure and functions of aquaporin-4-based orthogonal arrays of particles. Int Rev Cell Mol Biol287: 1–41.
Wong V, Gumbiner BM. 1997. A synthetic peptide corre-sponding to the extracellular domain of occludin per-turbs the tight junction permeability barrier. J Cell Biol136: 399–409.
Wosik K, Cayrol R, Dodelet-Devillers A, Berthelet F, Ber-nard M, Moumdjian R, Bouthillier A, Reudelhuber TL,Prat A. 2007. Angiotensin II controls occludin functionand is required for blood brain barrier maintenance:Relevance to multiple sclerosis. J Neurosci 27: 9032–9042.
Wu C, Ivars F, Anderson P, Hallmann R, Vestweber D, Nils-son P, Robenek H, Tryggvason K, Song J, Korpos E, et al.2009. Endothelial basement membrane laminina5 selec-tively inhibits T lymphocyte extravasation into the brain.Nat Med 15: 519–527.
Xu Q, Wang Y, Dabdoub A, Smallwood PM, Williams J,Woods C, Kelley MW, Jiang L, Tasman W, Zhang K, etal. 2004. Vascular development in the retina and innerear: Control by Norrin and Frizzled-4, a high-affinityligand-receptor pair. Cell 116: 883–895.
Ye X, Wang Y, Nathans J. 2010. The Norrin/Frizzled4 sig-naling pathway in retinal vascular development and dis-ease. Trends Mol Med 16: 417–425.
Yuan SY. 2002. Protein kinase signaling in the modulationof microvascular permeability. Vascul Pharmacol 39:213–223.
Zhao LN, Yang ZH, Liu YH, Ying HQ, Zhang H, Xue YX.2011. Vascular endothelial growth factor increases per-meability of the blood–tumor barrier via caveolae-me-diated transcellular pathway. J Mol Neurosci 44: 122–129.
Zlokovic BV. 2008. The blood–brain barrier in health andchronic neurodegenerative disorders. Neuron 57: 178–201.
The Blood–Brain Barrier
Cite this article as Cold Spring Harb Perspect Biol 2015;7:a020412 23
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from

2015; doi: 10.1101/cshperspect.a020412Cold Spring Harb Perspect Biol Richard Daneman and Alexandre Prat
Brain Barrier−The Blood
Subject Collection Glia
MaintenanceThe Nodes of Ranvier: Molecular Assembly and
Matthew N. Rasband and Elior Peles
Oligodendrocyte Development and PlasticityDwight E. Bergles and William D. Richardson
Microglia in Health and DiseaseRichard M. Ransohoff and Joseph El Khoury Support
Oligodendrocytes: Myelination and Axonal
Mikael Simons and Klaus-Armin NaveThe Astrocyte: Powerhouse and Recycling Center
Bruno Weber and L. Felipe Barros Central Nervous System GliaDrosophila
Marc R. Freeman
Development and PlasticityMicroglia Function in Central Nervous System
Dorothy P. Schafer and Beth StevensSynapse: Adaptable, Multitasking Glial CellsPerisynaptic Schwann Cells at the Neuromuscular
Chien-Ping Ko and Richard Robitaille
the Central Nervous SystemOligodendrocyte Development and Myelination in Transcriptional and Epigenetic Regulation of
Ben Emery and Q. Richard Lu
and EliminationAstrocytes Control Synapse Formation, Function,
Won-Suk Chung, Nicola J. Allen and Cagla Eroglu
ControversiesOrigin of Microglia: Current Concepts and Past
Florent Ginhoux and Marco Prinz
Schwann Cell MyelinationJames L. Salzer
Remyelination−−Glia Disease and RepairRobin J.M. Franklin and Steven A. Goldman Repair
Schwann Cells: Development and Role in Nerve
LloydKristján R. Jessen, Rhona Mirsky and Alison C.
Astrocytes in Neurodegenerative DiseaseHemali Phatnani and Tom Maniatis
Perineurial GliaSarah Kucenas
http://cshperspectives.cshlp.org/cgi/collection/ For additional articles in this collection, see
Copyright © 2015 Cold Spring Harbor Laboratory Press; all rights reserved
on January 16, 2021 - Published by Cold Spring Harbor Laboratory Press http://cshperspectives.cshlp.org/Downloaded from