The Bay Line - hfmamd.starchapter.com · certifications of which you may be unaware. All these...
Transcript of The Bay Line - hfmamd.starchapter.com · certifications of which you may be unaware. All these...
Officer’s CornerMichelle Brandt MedStar Health, Inc. Managed CareVP Physician, Ambulatory Contracting & Credentialing2015-2016 President Elect
In the January edition of the HFMA Chesa-peake Bay Line, James Case spoke about the role of HFMA in collaboration. Collaboration is critical for health care leaders in this ever changing and uncertain health care environ-ment. The Maryland Chapter has several pro-grams and events to provide opportunities for this essential collaboration through mem-ber forums, social events and community ser-vice projects.
In addition to the forums and top notch tech-nical sessions, the Maryland Chapter has been focusing more than ever on support-ing our membership with their leadership journey. I find the renewed commitment to leadership growth and development inspir-ing, and it is my hope that our sessions will also inspire you, our members. One of our newest leadership initiatives is the Women in Leadership series. Our first session in April of 2015 was a great success. During that session we engaged Content McLaughlin to describe her journey from putting herself through law school, being on the fast track to partner at a major law firm, and then later owning and leading her own successful law firm. Content inspired the group with her story, and provid-ed sound recommendations regarding how to overcome obstacles, leverage relationships, and mentor successfully. At the same session, we hosted a panel dis-cussion with an amazing line up of health care leaders across our industry: Donna Kin-zer, Executive Director, Health Services Cost Review Commission; Debi Kuchka-Craig, Cor-porate Vice President Managed Care, MedStar Health; Michelle Lee, Vice President Financial Reporting, UMMS; and Bonnie Phipps, Presi-dent & CEO, St. Agnes Hospital. These panel-
What’s Inside...Officer’s Corner 19 Ways Health Care Will Change in 2016 - Do you know your next steps? 2Save the Date for the Fall Institute 3Certification News 4Financial Arrangements: What’s Changed and what You Need to Know 5A Shift in Care: Protecting Access to Medicare Act 6Upcoming Education Events 7Crossword 7Committees 11Directors 12Sponsors 13
1
Vo
l 2015/2016, Issue 4, A
pril 2016
CThe hesapeake Bay Line
Continued on Page 8
2
Andrew Bachrodt, Managing PartnerKurt Salmon’s Health Care Group
Put Me in Coach:• Mandatory bundled pay-ments will force many provider organizations off of the value-based care sidelines and into the game in 2016. Some will win, most will struggle and many will fail—forcing provid-ers to put into place a true value-based care strategy built upon network scale and scope and the clinical and IT infrastructure to suc-cessfully manage value-based programs.
Penny Wise, Population Health Foolish:• Health system–employed primary care medical groups become the norm—and will continue to drain health system resources—whereas achieving real value under population health models remains elusive for many as health systems struggle to manage chronic patient populations and transitions into (and from) post-acute environments. Network develop-ment across the continuum as well as special-ist integration will be seen as equally critical, if not more so, as primary care.
Get with the In-Crowd:• Successful health sys-tems with regional strength will turn the ta-bles on payors and set the terms for narrow networks and direct-to-employer contracts to secure and grow share, manage appropriate utilization, and take more risk—and share—of the premium dollar.
There’s an App for That:• In population centers, health systems that embrace retail, digital and telemedicine platforms will realize big gains in brand value and set the stage for essential-ity to shift from physical assets to service and results.
I’ll Sit This Dance Out:• Population health is not for everyone or for every organization. The road to value-based care does not require everyone to do the “Hustle” when a simple “Waltz” will do. Listen to the music that is relevant in your market, and pick your dance partners wisely.
Back to the Future:• Provider merger and acquisition activity will continue to be strong in 2016 as providers continue to partner in an effort to achieve scale, es-pecially in response to the market tran-sition to value-based care. Federal and payor challenges to hospital asset and even virtual mergers will force many health systems to revisit vertical (payor and medical group) integration as an al-ternative foundation of their strategy.
Child’s Play:• Downward financial pressure means community hospitals will face the closure of their NICUs and smaller pedi-atric programs, and children’s hospitals will step in to either manage these units or create new capacity on their own campuses. Simultaneously, integrated health systems holding on to their pedi-atric platforms will look to freestanding children’s and academic medical centers for subspecialty support. Partnerships across key pediatric programs—and across state lines—will broaden research populations, and further advances in pe-diatric research will require a push for even greater collaboration in the future.
May–December Romance:• Hospitals will develop lasting, meaningful relation-ships with post-acute care providers, though the match-making will require kissing many frogs along the way.
Do the Math:• Health systems, newly rich with access to clinical data through in-vestments in EHRs and HIEs, will increas-ingly invest in data aggregation and predictive analytics—and be soundly disappointed with their efforts. Unleash-ing the power of big data is not core to most organizations, will be hugely ex-pensive and will require years of effort. It is one thing to do the math, and en-tirely another to act upon the results.
Vo
l 2015/2016, Issue 4, A
pril 2016
9 Ways Health Care Will Change in 2016 - Do you know your next steps?
4
Vo
l 2015/2016, Issue 4, A
pril 2016
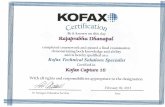
Certification News
Linker Mills, FHFMA, CRCRMaryland Chapter Certification Contact
I am proud to announce that we had four mem-bers pass the Certified Healthcare Financial Pro-fessional (CHFP) modules over the winter:
Desiree Axley, Director of Finance at MedStar •St. Mary’s Hospital
Koreen Muthiah, Vice President, Revenue Cy-•cle Management at Trident USA Health
Steve Oppitz, Manager, Financial Services at •MedStar Health
Katherine Turner, Manager Financial Planning •& Analysis at Anne Arundel Medical Center
We want to extend our congratulations to all these members on their great accomplishment!
The CHFP is the best known of the HFMA certi-fications, as it is the most comprehensive and the only one that can lead to the Fellow (FHFMA) designation. However, HFMA does offer specialty certifications of which you may be unaware. All these certifications cover specific areas of healthcare finance. The cost of these is $400 each for the on-line study material which leads to one comprehensive final. Once you pass the final, you are considered certified in that particu-lar focus area.
To maintain your certification with these, you will also have to retest ($100 and half the ques-tions of the original exam) every two years. This is compared to maintaining 60 continuing edu-cation hours every three years with the CHFP.
Certified Revenue Cycle Representative (CRCR): •Designed for those in the revenue cycle area, it deals with areas such as: Compliance, Pa-tient Access, Claims Processing, Account Reso-lution, and Cash Processing.
Certified Specialist Business Intelligence •(CSBI): Covers the concepts and uses of using healthcare data to create useful information that can drive decisions in healthcare organizations.
Certified Specialist Physician Practice •Management (CSPPM): Helps in the un-derstanding of the different topics and techniques needed to effectively man-age physician practices.
Certified Specialist Managed Care •(CSMC): Covers the different managed care models and the “nuts and bolts” of managed care and how they have been affected by healthcare reform.
Certified Specialist Accounting & Fi-•nance (CSAF): Provides an overview of healthcare accounting and finance and covers reports and statements unique to healthcare.
If you are interested in further information about any of these, please check out the HFMA website under the Education ban-ner.
A reminder that if your employer does not pay for the CHFP certification program, your Maryland HFMA chapter will reim-burse Maryland Chapter members once you become certified.
If you have any questions relating to certi-fication, please feel free to call me at 443-777-7949 or email me at [email protected].
Want to become a member or learn more about membership? Visit www.hfmamd.org or
contact Katie Eckert at [email protected].
5
By Susan Walberg, JD, MPA, CHC
There are always new laws, regulations, and changes in healthcare that keep us busy. One area that creates a lot of risk, however, is how we structure and manage financial arrange-ments, particularly those arrangements between referral sources. These arrangements can be be-tween hospitals and physicians, physician prac-tice groups and clinical laboratories, or anything else where you have referrals and money or oth-er benefits flowing back and forth. The purpose of this article is not to make you an expert on the details of fraud and abuse laws that apply to healthcare financial transactions, but rather to give you a few key points to keep in mind and to let you know of some recent changes that actu-ally make compliance easier.
In the Compliance world, we watch the govern-ment enforcement activities and the settlements that apply to healthcare organizations. The larg-est settlements, those multi-million dollar settle-ments, almost always involve a violation of Stark laws or the Anti-Kickback Statute, and include issues such as inappropriate payments to physi-cians or other referral sources. In some cases the organizations may have had an idea that they were pushing the envelope, but in other cases perhaps not. Because the Stark Law is a strict li-ability statute, you don’t need to have any intent for wrongdoing to get into trouble.
As a refresher, for anyone not familiar with the Stark Laws, Stark is also known as the physician self-referral statute. The basic premise is that physicians cannot refer Medicare or Medicaid patients to an entity where they or an immediate family member has a financial interest. Although ‘financial interest’ can encompass many arrange-ments, Stark does have a variety of exceptions, which is where your arrangements need to fall to find protection. The Anti-Kickback statute, on the other hand, is not limited to physician refer-rals, but does require that one purpose of a pay-ment is to induce referrals.
In either case, there are certain factors that will help keep you out of trouble. You will want to make sure your arrangement fits within a safe harbor or exception, and if you aren’t confident with this, you should definitely talk to your le-gal counsel. A few key points, however, to always keep in mind when giving or receiving anything of value from a potential referral source:
Fair market value. Whether it’s a lease •agreement, a Medical Directorship, or physician employment contract, you need to make sure the terms are within fair market value, and commercially rea-sonable. In other words, the arrangement would make sense even if there were no expectation of referrals. The rate is not the result of negotiation; it is objectively determined.
The terms are in no way based on vol-•ume or value of referrals. Your agreement should specifically state this, in addition to the fact that the fair market/commer-cially reasonable elements are met and documented.
The arrangement needs to be in writing, •signed by both parties. This has always meant that there needs to be a contract, particularly for any arrangement where you are paying a physician for anything.
This last point is where many organizations have gotten into trouble and have had to make self-disclosures to the government for ‘technical’ Stark violations when a con-tract had expired or payments were made to a physician without a contract. Such situations can arise for seemingly minor payments, like for continuing medical edu-cation. This year, in the 2016 Medicare Phy-sician Fee Schedule, CMS has made some ‘clarifications’ to the writing requirement under Stark that will actually make compli-ance easier.
In this Final Rule, published October 30, 2015, CMS revealed that arrangements do not need to be set forth in a single for-mal contract to comply with the ‘writing’ requirement under Stark. The revised lan-guage replaces the term ‘agreement’ with ‘arrangement’ and clarifies that, although a single written document memorializing the key aspects of the arrangement is the most straightforward means of establish-ing compliance, there may be situations where a collection of contemporaneous documents that evidence the terms and in-tent of the parties can suffice. In addition, not every document will need to bear the signature of one or both parties, although a signature for each party is required on at
Vo
l 2015/2016, Issue 4, A
pril 2016
Financial Arrangements: What’s Changed and what You Need to Know
Continued on Page 9
6
By Jessica Rosenberg,Associate with Lancaster Pollard [email protected]
The Protecting Access to Medicare Act (PAMA), like a lot of legislation, is based on a noble intention and is full of trade-offs, benefits and drawbacks. Overall, the Act aims to move the health care in-dustry toward one that pays for results as opposed to services. Getting there, of course, is the tricky part.
Since the PAMA was signed into law on April 1, 2014, it has been a source of con-versation among health care providers, lenders and beneficiaries. While there are many important components to this multifaceted legislation, this article will focus on the key components pertinent to senior living and health care provid-ers. Perhaps most noteworthy for pro-viders is the introduction of a value-based pay-ment system for skilled nursing facilities (SNFs) that is based on individual SNF performance on a hospital readmission measure.
In the spirit of transparency and clarity, the goal of PAMA is to further define the terms, expectations and limitations of the Medicare Act pertaining to Medicare providers, beneficiaries and legislative branches. When it was signed into law in 2014, one of the key provisions was a delay in any cuts in the Medicare reimbursement rate until 2015. These cuts were originally scheduled to go into effect April 1, 2014, and have traditionally been delayed each year for more than a decade. This time, the cuts went into effect with no legislation in sight to change that. Many groups, such as the American Medical Association (AMA), were dis-appointed in this aspect of PAMA and continue to push for a permanent fix to the Medicare cuts. It remains to be seen whether those efforts will prove to be fruitful. For now, PAMA is garnering attention not for the highly discussed Medicare cuts, rather for other provisions that are begin-ning implementation.
Paying for PerformanceOne of the core sections to come from the PAMA is section 215 which discusses the shift to a value-based purchasing (VBP) system. VBP is a demand side strategy to measure, report and reward ex-cellence in healthcare delivery. The transition to a VBP system typically occurs over many years with a transition period during which revenue decreases (Figure 1).
Beginning on Oct. 1, 2018, Medicare reim-bursement for SNFs will be tied to perfor-mance and quality of care rather than the traditional “fee-for-service” model. The VBP program looks at one quality measure de-fined by Health and Human Services (HHS) to determine the Medicare reimbursement that the facility will receive. High perform-ers will receive incentive payments and low performers will be subject to penalties. In order to create the incentive pool, SNF’s Medicare per-diem payments will be re-duced by 2%. Out of the money collected, 50-70% of it will be available for the incen-tive pool. Not all of the 2% reduction is go-ing back to SNFs, as it is also a means to save Medicare money, a projected $2 bil-lion over 10 years. Top performing SNFs will see most, if not all, of their 2% withhold re-turned through incentive payments, and possibly more. SNFs that perform in the middle level are expected to see a portion of their 2% withhold returned, while bot-tom performers will receive less than their withholding or nothing.
To quantify a SNF’s performance in the VBP program, HHS will use one of two quality measures: a hospital readmissions measure based of all causes and conditions, or a “re-source use” measure of “all-condition risk adjusted potentially preventable hospital readmissions” for SNFs. Initially, the VBP performance will be measured using the all-encompassing readmission measure,
A Shift in Care: Protecting Access to Medicare ActV
ol 2015/2016, Issu
e 4, Ap
ril 2016
Continued on Page 10Page 10
7
Date Event LocationFriday, April 22, 2016
Annual New HFMA Member Welcome & William J. Mooney Education Series
Maryland Hospital Association, 6820 Deerpath Road, Elkridge, MD 21075
Wednesday,April 27, 2016
Best Practice Initiatives for Managing Physician Practices
BWI Marriott
Thursday,April 28, 2016
Case Study: Building population health data infrastructure under New York payment reform (DSRIP)
Webinar
Note:
In addition to webinars hosted by the Maryland Chapter, the HFMA National organization spon-sors numerous complimentary webinars on a wide variety of current industry topics. The follow-ing is a link to the website if you are interested:http://www.hfma.org/Templates/UpcomingWebinars.aspx?id=613
Upcoming HFMA Education Events
ACCESSACCREDITATIONACUTE CAREAMBULATORY CAREANCILLARY SERVICESBALANCE BILLING BEHAVIORIAL HEALTHCARRIER
CARVE OUTCASE MIXCLINICCOST SHARINGDIAGNOSISHFMAMARGINDISCHARGE
FEE SCHEDULEGLOBAL BUDGETHEALTH POLICYMENTAL HEALTHNURSENETWORKPATIENT SAFETYPAYER
PROVIDERRATE REVIEWSPEND DOWNINDEMNITYDISABILITYOUTLIER
A C C R E D I T A T I O N X S S EN A M B U L A T O R Y C A R E R OU S M E N T A L H E A L T H O D DR E P C A R V E O U T H E A F G IS M A L I N D E M N I T Y H M L SE I T I D I S C H A R G E M L O AA X I N D I A G N O S I S A P B BS S E I N N G G F F O S R T R A IY E N C O S S Y R M Y Y D R G L LC L T A T E D E E A S O X C O B II U S R I R I R D E A T F G H U TL D A R A V M A R G I N C V B D YO L F E W E I V E R E T A R T G YP U E R E D I V O R P D F G Y E GH H T A S C O U T L I E R F S T FT C Y T E C O S T S H A R I N G RL S U S P E N D D O W N S D F G EA E B A L A N C E B I L L I N G SE E B E H A V I O R I A L H E A LH F M A E A N N I N S O C T T S T
Vo
l 2015/2016, Issue 4, A
pril 2016
Crossword
8
Vo
l 2015/2016, Issue 4, A
pril 2016
Officer’s CornerContinued from Page 1
Major General Linda Singh
Major General Linda Singh addressing the audience
Janice Burnett, EVP, CFO Bon Secours Health System, Inc.; Nora Hoban, Senior Vice President,
Policy & Analytics, MHA; Gwendolyn Skillern, Sr. Vice President & General Auditor, CareFirst BlueCross BlueShield; and Deana Stout, CFO,
MedStar Good Samaritan Hospital and MedStar Union Memorial Hospital.
ists answered tough questions about the reac-tion to women in the work place through the years and gave insightful and practical counsel regarding how women can help themselves and each other. Debi and Bonnie are also past HFMA National Chairs, so that provided a spe-cial bonus to attendees.
Given the feedback from our attendees at the first Women in Leadership session it was clear that we should continue with this leadership focus in future sessions. The Chapter’s second Women in Leadership session was held in Octo-ber of 2015 and we were honored to have Major General (Maj. Gen.) Linda Singh as our keynote speaker. Maj. Gen. Singh was born and raised in Maryland and is the first woman to be ap-pointed to the position of the Adjutant General for the Maryland National Guard. Two months into this role, Maj. Gen. Singh was tasked to lead Maryland’s Air and Army National Guard forces to restore peace during the Baltimore ri-ots. The rise of a women leader in the military is still rare today and Maj. Gen. Singh’s story of perseverance and determination was inspi-rational! Her compelling testimony to living a life, professionally and personally, focused on achievement left us reluctant for her time with us to end.
Following Maj. Gen. Singh we once again engaged a top notch panel of industry leaders: Janice Burnett, EVP, CFO Bon Secours Health System, Inc.; Nora Hoban, Senior Vice President, Policy & Analytics, MHA; Gwendolyn Skillern, Sr. Vice Presi-dent & General Auditor, CareFirst Blue-Cross BlueShield; and Deana Stout, CFO, MedStar Good Samaritan Hospital and MedStar Union Memorial Hospital. These industry leaders covered a vast array of topics and shared their wisdom, lessons learned, and valuable advice. Closing out our session for that day was a Toastmas-ters International speaker presenting the Importance of Communication in Lead-ership--a skill everyone can continue to improve in support of leadership devel-opment.
The Women in Leadership Commit-tee comprised of Jeanette Cross, Neusa Facenda, Mary Kim, and Traci LaValle (or as I call them, The Dream Team) are com-mitted to offering inspired, focused lead-ership sessions at least twice a year. We are already planning our next event for the evening of June 16th and we hope to see you there!
9
least one of the documents available to establish the arrangement.
Although these changes do certainly make the writing requirement easier, in theory, a contract is still the cleanest way to be sure. It isn’t clear yet how these changes will be interpreted by the government when they actually are investigat-ing a provider’s arrangements, and trying to pull together multiple pieces of documentation may be a burdensome exercise.
As financial arrangements continue to be a risk area, there are a couple things you should con-sider, just to minimize your exposure.
Conduct an audit of payments to physicians. •Tie the payments back to a contract, and if you can’t, then see what documentation you can locate to ‘prove’ the arrangement. This will give you a sense of your possible vulnerability,
and will help identify process weakness-es that can be corrected before you have an issue. If you do find major issues, talk to your legal counsel. It’s better to proactively manage these issues rather than having the government potentially handle it for you.
If you have previously disclosed a ‘tech-•nical’ Stark violation, and it’s still pend-ing, talk to your attorney. With these re-cent changes you may have some wiggle room.
The new rules have made Stark compli-ance easier, but it’s still important to know where your arrangements are at, and how well your documentation stacks up.
Vo
l 2015/2016, Issue 4, A
pril 2016
Visit us online at
for upcoming events, industry news and more!
www.hfmamd.org
Continued from Page 5
Financial Arrangements: What’s Changed and what You Need to Know
10
A Shift in Care: Protecting Access to Medicare Act
however, the PAMA requires that the more specific “resource use” measure be implemented as soon as possible. HHS will provide SNFs with confidential feedback on the initial results from both measures in 2016 and will publicly report data on both measures by Oct. 1, 2017. The proposed VBP rule will be pub-lished in 2018 and the first adjustments to a SNF’s payments will begin in 2019.
Ultimately, the VBP program should affect provid-ers, beneficiaries and lenders in a positive way. The programs afford health care providers the oppor-tunity to stand out from a quality of care, service and hospitality perspective by making global ini-tiatives to enhance their operations. This method-ology forces health care providers to refocus and reconsider their why statement (“why we are here and why are we doing this?”) Hospitals and other health programs were created to care for the sick by those who had a passion for helping others. Effectively implementing a VBP program within a health care organization returns to the original principals that guided the creation of health care in society today. Hospitals Feel the EffectsThe changes in the PAMA affect hospitals in a va-riety of ways. Typically, Medicare sets annual ben-eficiary payment limits for outpatient therapy ser-vices. The PAMA allowed the temporary expansion of the cap on outpatient therapy services provided in Hospital Outpatient Departments (HOPDs) if the therapy is deemed medically necessary. The exten-sion of the therapy cap was permanently extended by the Centers for Medicare & Medicaid Services (CMS) for Critical Access Hospitals (CAHs). From both an operational, beneficiary, and financial per-spective, this is key as it drives additional patients to hospitals to supplement Medicare revenue and it allows patients to receive higher quality care for longer time periods through what is likely to be a better therapy program.
Concentrating more on rural hospitals, Section 106 details plans to spend $100 million over 10 years, focusing on extending the Medicare-Dependent Hospital (MDH) program. Established in 1987, the MDH helps support small rural hospitals for which Medicare patients make up a majority of their inpa-tient days or discharges. To qualify as an MDH, the hospital must be located in a rural area, have 100 beds or less, not be classified as a sole community hospital, and have at least 60% of discharges or in-patient days covered by Medicare. These hospitals are able to receive the inpatient price per service
(PPS) rate plus three-quarters of the amount by which their costs per discharge exceed the (PPS) rate. For example: ABC hospital dis-charges Patient X who had a one night stay. Patient X had a PPS rate of $150. The cost to discharge Patient X is $300. The hospital will receive $262.50. This is determined by tak-ing the difference between the PPS rate and the discharge cost ($300-$150), multiplying it by .75 and adding it to the PPS rate which amounts to $112.50. This boost in rates is in-valuable to operators as it helps to bridge the gap between costly discharges and low PPS rates. Additionally, MDH will help de-crease expense margins and boost Medicare revenue. Section 212 has received a lot of attention due to its focus on technology and effect on monetary means of providers. HHS Secre-tary Sylvia Burwell delayed the adoption of ICD-10 as the standard code for medical data from Oct. 1, 2014 to Oct. 1, 2015. There was significant opposition regarding the delays in implementing the ICD-10 coding system. Many hospitals had incurred substantial fi-nancial obligations in implementing ICD-10. This delay ultimately slowed down the tran-sition to value-based payment in the health system.
A Clear ShiftThe PAMA, like a lot of legislation, has noble goals but is imperfect. While some sections in the PAMA are steering health care in the direction of realizing a true value-based pay-ment system, some components of the legis-lation such as the ICD-10 coding have slowed down this process. Overall, however, the trend is clear; health care is moving towards a pay-for-performance model and PAMA rep-resents a significant step in that direction.
Source: American Hospital Association, “Leg-islative Advisory, The Protecting Access to Medicare Act of 2014,” April 2014.
Vo
l 2015/2016, Issue 4, A
pril 2016
Continued from Page 6
11
Vo
l 2015/2016, Issue 4, A
pril 2016
The HFMA Maryland Chapter has many exciting committees that would welcome your participation. If you are interested, please contact one of the Committee Chairs below:
Committee Chairperson Email Address Annual Institute Ellen S. Milles
Tim [email protected]@baml.com
Certification Linker Mills [email protected]/Website Joshua Campbell [email protected] Service Megan Irwin [email protected] Katie Eckert [email protected] Donnell Henry [email protected] (Chapter Education) Brett McCone
Craig [email protected][email protected]
Webinar Jeanette Cross [email protected] Michael Myers
Michelle [email protected]@medstar.net
Social Brian Sims [email protected] Craig Masters
Scott [email protected]@stagnes.org
Volunteers Chuck Cronauer [email protected] Scott Furniss
Michael [email protected]@gbmc.org
Newsletter CommitteeMember Organization Email Address George Bayless GBMC Healthcare [email protected]
Tim Brooks Bank of America [email protected]
Nancy Creighton Peninsula Regional Medical Center [email protected]
Jeanette Cross Berkeley Research Group [email protected]
Kathryn Crostic UMMS [email protected]
Jennifer Douggherty UMMS [email protected]
Donnell Henry Kennedy Krieger Institute [email protected]
Lindsay Hurley Berkeley Research Group [email protected]
Don Kohlhafer Bank of America [email protected]
Scott Mitchell Grant Thornton [email protected]
Rachel Schaaf [email protected]
Kathleen Schippereit Berkeley Research Group [email protected]
Brian Sims MHA [email protected]
Vanessa Smith Bank of America [email protected]
Michael Whittington Berkeley Research Group [email protected]
Lucas Sater Berkeley Research Group [email protected]
India Suter Asset Strategy Consultants [email protected]
Megan Irwin UMMS [email protected]
Shirley Sutton St. Agnes Healthcare [email protected]
Caroline Znaniac Luna Healthcare Advisors [email protected]
12
PresidentMichael MyersGBMC Healthcare Inc.Phone: (443) 849-4328
Vice PresidentWilliam McConeMaryland Hospital AssociationPhone: (410) 949-8538
TreasurerJames CaseKpmg LlpPhone: (410) 949-8895
Director - Voting MemberJeanette CrossBerkeley Research GroupPhone: (443) 391-1042
Director - Voting MemberEllen MillesKennedy Krieger InstitutePhone: (443) 923-1807
Director - Non-voting MemberTraci La ValleMaryland Hospital AssociationPhone: (410) 379-6200
President-ElectMichelle BrandtMedStar HealthPhone: (410) 933-3015
SecretaryCraig MastersBon Secours Health System, Inc.Phone: (443) 367-2206
Director - Voting MemberTim BrooksBank Of AmericaPhone: (410) 547-4273
Director - Voting MemberMary KimMedstar HealthPhone: (410) 772-6591
Director - Voting MemberLinker MillsMedstar Franklin Square Medical CenterPhone: (443) 777-7949
Immediate Past President, Director - Non-voting MemberScott FurnissSt. Agnes HospitalPhone: (410) 368-3130
Board of Directors2015 - 2016
Let Yourself Be Heard!
Attention all members, sponsors and friends of the HFMA Maryland Chapter.
Have something to say to the Maryland Chapter members?
Itching to share your thoughts with others?
Then write an article for the Chesapeake Bay Line.
Send your articles for consideration to Donnell Henry, Newsletter Chair at [email protected]
Vo
l 2015/2016, Issue 4, A
pril 2016
We are very grateful to our sponsors who help the HFMA Maryland Chapter provide high qual-ity education programs and events. If you would like to partner with us and join this group of business leaders please contact Craig Masters at 443-367-2206 or [email protected] or visit our website at www.hfmamd.org to find out how. Thank you for your support.
The
HFMA Maryland Chapterc/o Laureen Nolker22 S. Greene St. - PP7Baltimore, MD 21201
Healthcare Financial Management Association
Chesapeake Bay Line