TB: Siriraj Internal Medicine Board Review 2018 · WHO Guideline 2016 Group of Drugs for...
Transcript of TB: Siriraj Internal Medicine Board Review 2018 · WHO Guideline 2016 Group of Drugs for...

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Nitipatana Chierakul
Division of Respiratory Disease and Tuberculosis,
Department of Medicine,
Siriraj medical School,
Bangkok, THAILAND
TB: Siriraj Internal Medicine Board Review
2018

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
TB-HIV 8 %

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Indicator Target (%)
Treatment coverage ≥ 90
Treatment success rate ≥ 90
Catastrophic costs due to TB in households 0
Initial WHO-recommended rapid diagnostic test ≥ 90
Latent TB infection treatment coverage ≥ 90
Contact investigation coverage ≥ 90
Drug-susceptibility testing (DST) coverage 100
Treatment coverage, new TB drugs ≥ 90
Documented HIV status among TB patients 100
Case fatality ratio (CFR) ≤ 5
Achievement for End-TB Strategy in 2025

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Conventional Diagnosis

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Options for Smear-negative PTB
Start anti-TB drugs if CXR reveal new cavity, adenopathy, or miliary pattern
Bronchoscopy CT scan if no suggestive CXR pattern and harbour risk of lung cancer
Otherwise, follow-up clinical symptoms and radiological findings every 3 months for 2 years
Also take risk for transmission and side effect of anti-TB drugs into consideration

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Consideration in AFB+
Tuberculosis (viable vs non-viable), especially in those considering treatment failure before starting empiric drug-resistant regimen by reviewing clinical, microbiological, and radiological responses
Non-tuberculous mycobacteria infection (colonization vsdisease)
Other organisms: Rhodococcus, Nocardia, Gordonia, Tsukamurella, Dietzia

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Mycobacterial Culture
Conventional culture and drug susceptibility testing (DST) has turnaround time (TAT) of 9-12 weeks for first-line drugs (FLD) and 12-16 weeks for second-line drugs (SLD)
Novel liquid culture can shorten TAT to 3-5 weeks for multidrug-resistant TB (MDR-TB) and 4-9 weeks for extensively drug-resistant TB (XDR-TB)
jjmicrobiol.com
www.bd.com

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Indication for Initial Culture & DST
Previous TB treatment for more than 1 month, especially treatment failure, regardless of smear status
HIV co-infection, especially CD4 < 200 cells/µL
Recent closely contact with MDR-TB case
Every new case in place where initial incidence of MDR-TB > 3%
Optional• Smear-negative pulmonary or extrapulmonary TB
where definite diagnosis is vital
• Deep-seated specimens: bronchoalveolar lavage fluid, CSF, joint fluid, pericardial effusion, percutaneous tissue aspiration or biopsy

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Tuberculin Skin test (TST) Indirect evidence of infection, not
an active disease, interpretation should be based on clinical probability
Quality of tuberculin and technique are vital
Essential tool for childhood TB
Confounded by BCG vaccination, immune status, non-tuberculous mycobacteria (NTM) infection
The more positive, the more likelihood of TB infection, however, in THAILAND 30% of adult with other pulmonary
diseases had TST > 15 mm
10% of adult with active pulmonary TB had TST < 10 mm

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
WHO Policy Statement 2011
IGRAs
Interferon-gamma Release Assays

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Category II regimen (2SHRZE/1HRZE/5HRE) should no longer be used
and rapid DST should be conducted to inform the choice of regimen

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
First-line Anti-TB Drugs
Dose Adverse reactions Remarks
H 300 mg/d
5/mg/kg/d
(BW < 30 kg)
Rash, hepatitis, neuritis Pyridoxine 50-100
mg/d in those at
risk, acne
R 10 mg/kg/d
Maximum 600
Rash, hepatitis, immune
dysregulation, drug
interaction
Potent enzyme
inducer, body fluid
discoloration, acne
Z 25 mg/kg/d
Maximum 2,000
Rash, hepatitis,
hyperuricemia
Dose adjustment
for low GFR
E 15 mg/kg/d Rash, retrobulbar neuritis,
hyperuricemia
Dose adjustment
for low GFR
S 15 mg/kg/d Ototoxicity, nephrotoxicity At least 5 times a
week
Ofx 400 mg/d CNS toxicity, tendinitis Avoid in children

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
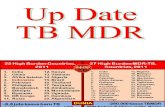
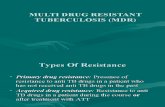
WHO Guideline 2016
Group of Drugs for rifampicin-resistant-TB and MDR-TB Treatment
Empiric MDR-TB regimen
1A, 1B, 2C, 1D1
6-8 Km Lfx Eto Cs Z (E or PAS)
+
12-14 Lfx Eto Cs ± Z (E or PAS)
Shorter MDR-TB regimen
4-6 Km Mfx Pto Cfz Z Hhigh E +
5 Mfx Cfz Z E

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Cutaneous Reaction to Anti-TB Drugs
Severity Skin lesion Systemic
symptomsManagement
MildMaculopapular,
transient-
Reassure,
antihistamine
Moderate Persistent +Stop, steroid,
rechallenge
SevereExtensive, mucosal
involvement+
Admit, stop,
steroid,
desensitize

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Anti-TB Drug-induced Liver Injury (DILI)
Risk Factors
Advanced age
Alcoholism
Previous significant liver abnormalities
HBV, HCV, and HIV infection
Malnutrition
Concomitant potential hepatotoxic drugs:
antiepileptics, methotrexate

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Antituberculosis-DILI
Inform the patients before prescription
Avoid alcohol and hepatotoxic agents
Baseline LFTs for those harbour risks
• Normal or near normal: repeat if symptomatic or every 2-4 weeks during the first 8 weeks
• Abnormal: close observe, repeat if symptomatic or 1-2/week during the first 2 weeks and then every 2 weeks during the intensive phase
Always aware for confounding viral hepatitis

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Antituberculosis-DILI
Elevation of ALT > 3 times with symptoms or 5 times without, ¾ occurs in first 2 months
Weigh between disease severity and degree of liver impairment, consider discontinue or replace less hepatotoxic agents (ethambutol, quinolones, aminoglycosides)
Drug challenging with low-dose or full-dose (R H Z) every 3 days after ALT < 2 times, rechecking if symptoms recur, the last drug added should be stopped
Up to ¾ of those with no pre-existing liver abnormality can resume HRZE
Rechallenge with Z may be hazardous in those with prolonged or severe hepatotoxicity
Alternative regimens: 6RZE, 2SHRE/6HR, 2HRE/7HR, 2 HZE/10HE, 2SHE/10HE, 2SOfxE/16OfxE
Close follow-up in case suspected of TB hepatitis

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Treatment Adjustment in CKD Patients
Isoniazid and rifampicin can be used safely regardless of GFR
Aminoglycosides should not be used
Quinolones require dose adjustment in advanced case
Adjust ethambutol to 10 mg/kg/d in stage 2 and 7.5 mg/kg/d in stage 3 with close monitoring for visual impairment, avoid in those stage 4
Pyrazinamide should be use at dose 10 mg/kg/d in those stage 3-4
In those on regular hemodialysis, prescribe ethambutol and pyrazinamide in usual dose, thrice weekly administered after dialysis

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
TB-HIV Treatment
ART should be started in all TB patients living with HIV regardless of their CD4 count
TB treatment should be initiated first, followed by ART as soon as possible within the first 8 weeks of TB treatment
Those withCD4 count < 50 cells/µL should receive ART within the first 2 weeks of initiating TB treatment
In patients receiving TB-HIV co-treatment (drug-
susceptible pulmonary TB), a 6-month standard
treatment regimen is recommended over an
extended treatment for 8 months or more

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Paradoxical Response (Non-HIV)PTB (AFB+) with Mediastinal TB Lymphadenopathy
Fever with right pleuritic chest pain 2 weeks after anti-TB

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
TB-associated Immune Restoration
Inflammatory Syndrome (IRIS)
Definite TB diagnosis was made before starting ARV
Initial response to TB treatment of more than 2 weeks
before ARV initiation
Alternative explanations must be excluded
Drug resistance TB
Poor adherence to treatment
Another opportunistic infection or neoplasm, particularly in those with smear-negative PTB or EPTB
Drug toxicity or reaction

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Treatment after Interruption
Non-compliance or temporary regimens for severe ADR
Re-numbering after successful re-introduction
At least 80% of prescribed dose can lead to no significant change in outcome (98% cure rate with 2%relapse rate for 2 HRZE / 4 HR)
Continue 2 weeks allowance during intensive phase
4 weeks allowance during maintenance phase
Otherwise re-number, except if 4 months has passed with symptoms and CXR are markedly improved and become negative smear

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Adjunctive Corticosteroids
In patients with tuberculous meningitis, an
initial adjuvant corticosteroid therapy with
dexamethasone or prednisolone tapered over
6-8 weeks should be used regardless of the
severity of meningitis
In patients with tuberculous pericarditis, an
initial adjuvant corticosteroid therapy may be
used for preventing constrictive pericarditis

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Treatment Adherence
Ensure health education and counseling on the
disease and treatment adherence
Community-based or home-based directly
observed treatment (DOT) is recommended over
health facility-based DOT or unsupervised
treatment, DOT administered by trained lay
providers or health-care worker may be considered
Video observed treatment (VOT) can replace DOT
when the video communication technology is
available and can be appropriately organized and
operated by health-care providers and patients

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Resuming Social Function
Abolishment or nearly absence of cough
Smear conversion or significantly decreased
Well ventilated space, no highly susceptible person (small children, older age, immunosuppressed)
Less infectivity after treatment for at least 2 weeks
Long travel and elective surgery should be postponed until sputum smears are negative

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Disease Monitoring Cough, fever, appetite, weight, organ
symptoms
Sputum smears every 2 weeks in intensive phase, and every 4 weeks in maintenance phase
CXR at the end of intensive phase in those initial smear-negative, and at the end of treatment regardless of smear status
Organ examination, imaging, and inflammatory biomarker such as C-reactive protein (CRP) for extrapulmonary TB

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Action for Those with Unfavorable Responses Smear +
Persistent + after M2: check for compliance and control of of co-morbidities
If clinical not improved and stable or worsening CXR
Available initial DST: adjust accordingly
NA initial DST, step down with close clinical FU if
Persistent + after M3, send DST
Persistent + after M4, Xpert TB/RIF, empiric MDR-TB regimen if test+
Smear – If smears convert to positive after M2
carefully consider for action as persistent+ after M4

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Hemoptysis after Treatment
• Cause• Relapse TB
• Infected bronchiectasis
• Mycetoma (aspergilloma)
• Scar tumor
• Rasmussen’s aneurysm
• Repeat consecutive
sputum smears, treat
infected bronchiectasis,
avoid quinolones
• Alert for lung cancer in
those harbored risk
• Aspergillus precipitin or
sputum fungal cultures for
mycetoma

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Thailand Renown
for Tuberculosis

เช่ียวชาญศาสตร์สรรพ์ ยดึม่ันคุณธรรม ชีน้ าสังคม
Suggested Readings
นิธิพฒัน์ เจียรกลุ. วณัโรค. ใน : ต ำรำอำยรุศำสตรท์ัว่ไป. นิธิพฒัน์ เจียรกลุ(บรรณำธิกำร). กรงุเทพมหำนคร, ภำพพิมพ ์2556; 286-295
World Health Organization
Treatment of tuberculosis: guidelines, 4th ed.
WHO/HTM/TB/2009.420
Companion handbook to the WHO guidelines for the
programmatic management of drug-resistant tuberculosis
WHO/HTM/TB/2014.11
The End TB Strategy
WHO/HTM/TB/2015.30
Global Tuberculosis Report 2017
WHO/HTM/TB/2017.23