TB Case Presentations - Rutgers Universityglobaltb.njms.rutgers.edu/downloads/courses/2011/Wang TB...
-
Upload
trinhtuyen -
Category
Documents
-
view
214 -
download
0
Transcript of TB Case Presentations - Rutgers Universityglobaltb.njms.rutgers.edu/downloads/courses/2011/Wang TB...

1
ShuShu--Hua Wang, MD, MPH&TMHua Wang, MD, MPH&TMAssistant Professor of MedicineAssistant Professor of Medicine
The Ohio State UniversityThe Ohio State University
TB Case PresentationsTB Case Presentations
Case Presentation (ACase Presentation (A--1)1)
Patient history 17-year-old Hispanic male No significant past medical history 8 week history of cough Associated with:
– Pleuritic retrosternal chest pain (CP) – Dyspnea on excertion (DOE) – Fever, night sweats, chills – 10-12 lb. weight loss
Any other questions????Any other questions????
Case Presentation (ACase Presentation (A--2)2)
2 weeks ago seen at free clinic New diagnosis of HIV: CD4: 41, Viral load:
199,000 TST: Non-reactive, 0mm No other significant past medical historyNo other significant past medical history No medicationsNo medications Social history:Social history:
–– 11stst sexual encounter age 15, last unprotected sexual encounter age 15, last unprotected sex 4mo ago, all sexual partners malesex 4mo ago, all sexual partners male
–– No incarcerations/homelessness/known TB No incarcerations/homelessness/known TB contacts contacts
Case Presentation (ACase Presentation (A--3) 3)
LabsLabs CBC WNLCBC WNL Chem WNLChem WNL LDH: 243LDH: 243 ABG: WNLABG: WNLCXRCXR No infiltrateNo infiltrate L hilar fullnessL hilar fullness
Physical ExamPhysical ExamVS: VS: Temp: 39.4Temp: 39.4˚̊ BP: 110/60 BP: 110/60 P: P: 108108 RR: 26RR: 26 97% RA97% RA

2
Case Presentation (ACase Presentation (A--4)4)QuestionQuestion
True or False ?True or False ?Patient does not have pulmonary TB because TST Patient does not have pulmonary TB because TST
is negative and CXR does not have an infiltrate? is negative and CXR does not have an infiltrate?
Case Presentation (ACase Presentation (A--5)5)AnswerAnswer
HIV infected persons may have normal CXR and HIV infected persons may have normal CXR and still have TB. still have TB.
Hilar adenopathy is suggestive of TBHilar adenopathy is suggestive of TB Active TB patients can be TST negative. Active TB patients can be TST negative.
–– HIV (+) or HIV (HIV (+) or HIV (--). ).
AFB sputum smear and culture should be AFB sputum smear and culture should be obtained obtained
Patient admitted to the hospitalPatient admitted to the hospital Negative pressure room (AII)Negative pressure room (AII) Sputum smear and culture X 3Sputum smear and culture X 3 Result: AFB smear negative X 3 Result: AFB smear negative X 3 Question Question –– Is there another test that can Is there another test that can
be ordered to help you with the diagnosis?be ordered to help you with the diagnosis?
Case Presentation (ACase Presentation (A--6)6)Hospital courseHospital course
Specimen collection and processing
AFB Smear MGIT (Liquid medium, automated system)
Agar PlateM H 711
No GrowthIncubate for 6 weeks
Case Presentation (ACase Presentation (A--7)7)Answer: YesAnswer: Yes
NAAT Positive GrowthNo Growth
Incubate for 4 weeks
NAAT: Nucleic acid amplification testMycobacterium tuberculosis Direct Test (MTD) or Amplicor

3
Nucleic Acid Amplification (NAA) TestsNucleic Acid Amplification (NAA) TestsMycobacterial TB Direct Test (MTD) Mycobacterial TB Direct Test (MTD)
Direct, rapid, detection of Direct, rapid, detection of Mycobacterium Mycobacterium tuberculosistuberculosis complex (rRNA)complex (rRNA)–– Patients suspected of TBPatients suspected of TB–– Takes about 4 to 5 hoursTakes about 4 to 5 hours–– Approved for respiratory specimens onlyApproved for respiratory specimens only Smear positive and smear negativeSmear positive and smear negative
–– NonNon--respiratory specimen (validated by labs) respiratory specimen (validated by labs) –– Can detect fewer than 10 organismsCan detect fewer than 10 organisms–– Does not distinguish live vs dead organism Does not distinguish live vs dead organism
MMWR July 7, 2000
CDC Guidelines CDC Guidelines -- 20092009Nucleic Acid Amplification Test Nucleic Acid Amplification Test
Collect specimen for AFB, culture, & NAA Collect specimen for AFB, culture, & NAA Interpret results with AFB smear Interpret results with AFB smear
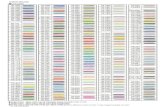
NAA AFB Recommend
+ + Start treatment. PPV >95% NAA in AFB+ cases
+ - Repeat NAA test. Presume TB if >=2 NAA (+)
- + Presume nontuberculous mycobacteria (NTM)
- - •Use clinical judgment.
•NAA sensitivity 50-80% in detection AFB (-) Culture (+) pulmonary TB
MMWR 2009
Case Presentation (ACase Presentation (A--8)8)Hospital Course: Hospital Course:
Treated empirically with Treated empirically with levofloxacinlevofloxacin: symptoms : symptoms improvedimprovedWorking diagnosis on dischargeWorking diagnosis on discharge
–– mediastinal lymphadenopathy, r/o lymphoma mediastinal lymphadenopathy, r/o lymphoma vs. mycobacterial disease vs. mycobacterial disease
Discharged with levofloxacin, PCP and MAC Discharged with levofloxacin, PCP and MAC prophylaxisprophylaxis
Case Presentation (ACase Presentation (A--9) 9)
Seen in HIV clinic 1 week after hospital Seen in HIV clinic 1 week after hospital dischargedischarge
Fever, chills, and cough recurred Fever, chills, and cough recurred Sputum AFB culture: still pendingSputum AFB culture: still pending Concerned the patient may have TBConcerned the patient may have TB Your health department has lost $$ TB Your health department has lost $$ TB
funding and you are short on staff for funding and you are short on staff for DOTDOT

4
Case Presentation (ACase Presentation (A--10) 10) Question Question
Which initial regimen would you start?Which initial regimen would you start?
a.a. INH, Rifampin, EMB, and PZA (daily)INH, Rifampin, EMB, and PZA (daily)
b.b. INH, Rifampin, EMB, and PZA (BIW)INH, Rifampin, EMB, and PZA (BIW)
c.c. Refill Levofloxacin Refill Levofloxacin –– he got better on it!he got better on it!
d.d. Has LTBI and can treat with INH and Has LTBI and can treat with INH and Rifapentine (once weekly)Rifapentine (once weekly)
e.e. Wait for culture to be positive before startingWait for culture to be positive before starting
TB Treatment TB Treatment -- CultureCulture--Positive TBPositive TB
Initial Phase
(Rated: AI in HIV-negative, AII in HIV-positive patients)
2 months - INH, RIF, PZA, EMB daily (56 doses, 8 weeks)
- INH, RIF, PZA, EMB 5x/wk (40 doses, 8 weeks)
• Do NOT use twice-weekly therapy for HIV + with low CD4 < 100 cells/mm33
•• Avoid use of Rifapentine for HIVAvoid use of Rifapentine for HIV--TB CoTB Co--infectedinfected
MMWR 2003 / 52(RR11);1-77
Case Presentation (ACase Presentation (A--11)11)
Day 20Day 20 AFB culture AFB culture -- positive for positive for M. tuberculosisM. tuberculosis All isolates: All isolates: panpan--susceptible to first line drugssusceptible to first line drugs
Day 25Day 25 -- Enlarging lymph nodeEnlarging lymph nodeAdmitted Admitted Axillary lymph node biopsyAxillary lymph node biopsy Continued on TB medications Continued on TB medications Symptoms improved Symptoms improved DischargedDischarged
Case Presentation (ACase Presentation (A--12)12)Acid Fast Smear of Axillary Lymph NodeAcid Fast Smear of Axillary Lymph Node

5
Day 60 Day 60 -- HIV Clinic HIV Clinic HIV viral load 199,000HIV viral load 199,000 HAART initiated:HAART initiated:
–– Triple nucleoside regimenTriple nucleoside regimen–– d4T, 3TC, abacavir d4T, 3TC, abacavir
Traveled to Puerto Rico for 2 weeks to visit familyTraveled to Puerto Rico for 2 weeks to visit family
Case Presentation (ACase Presentation (A--13)13) Case Presentation (ACase Presentation (A--14)14)
Day 99 Day 99 Presented to ER 39 days Presented to ER 39 days
after starting HAARTafter starting HAARTCC: Increasing SOB & CC: Increasing SOB &
diaphoresisdiaphoresis
Vitals: Vitals: T 104.3T 104.3°°FFRR 40 BP 84/52RR 40 BP 84/52Physical exam: Physical exam: Distended neck veinsDistended neck veinsDecrease heart tonesDecrease heart tones
PA VIEWS OF THE CHEST:Increasing Cardiothoracic Ratio & Superior Mediastinal Widening
Initial admission = 42% 2 months later = 51 %
Case Presentation (ACase Presentation (A--15)15)
Initial Diagnosis 2 months later
Interval Development of Large Pericardial Effusion
Case Presentation (ACase Presentation (A--16)16)

6
Pericardial Biopsy -Thickened Pericardium with Acute and Chronic Hemorrhagic Inflammation
Pericardial biopsy and fluid were all negative
Case Presentation (ACase Presentation (A--17)17)
Slide courtesy of Dr Jonathon Rock and OSUMC Clinical Pathology
Slide courtesy of Dr Jonathon Rock and OSUMC Clinical Pathology
QuestionQuestion
Which of the following is the most likely Which of the following is the most likely explanation for his current symptoms?explanation for his current symptoms?
a.a. He has developed multiHe has developed multi--drug resistant TBdrug resistant TBb.b. He has developed PCP He has developed PCP ((Pneumocystis jiroveci )
c.c. He is experiencing side effects to his antiHe is experiencing side effects to his anti--TB medicationTB medication
d.d. He has developed a He has developed a ““paradoxical reactionparadoxical reaction””to his antito his anti--TB and HAARTTB and HAART
Case Presentation (ACase Presentation (A--18)18)

7
Immune Restoration Inflammatory SyndromeImmune Restoration Inflammatory Syndrome
Occurs in 8Occurs in 8--43% of co43% of co--infectedinfected Most patients have advanced HIV diseaseMost patients have advanced HIV disease
–– median CD4 count of 35 cells/ mmmedian CD4 count of 35 cells/ mm3 3
–– median viral load > 500,000 copies/mlmedian viral load > 500,000 copies/ml–– Usually severe TB disease with high pathogen burdenUsually severe TB disease with high pathogen burden
Median 15 days after starting ARV therapy (<30 d) Median 15 days after starting ARV therapy (<30 d) –– Most within 90 days of starting TB RxMost within 90 days of starting TB Rx
Diagnosis of exclusion: Diagnosis of exclusion: –– Differential diagnosis include:Differential diagnosis include: Treatment failure, adherence, drug toxicity, new Treatment failure, adherence, drug toxicity, new
infectioninfection Management of reactions:Management of reactions:
–– NSAIDS if mild, NSAIDS if mild, –– Prednisone if severe Prednisone if severe
Slide courtesy of Dr Michael Para
Response to Corticosteroids: Response to Corticosteroids: Resolution of Pericardial EffusionResolution of Pericardial Effusion
Day - 1 Day + 8Day of Corticosteroids
Case Presentation (ACase Presentation (A--20)20)
Response to Corticosteroids: Response to Corticosteroids: Resolution of Pericardial EffusionResolution of Pericardial Effusion
Day - 1 Day + 17Day of Corticosteroids
Case Presentation (ACase Presentation (A--21)21) Key Points: HIVKey Points: HIV--TB CoTB Co--infectioninfection
HIV and TB enhance each otherHIV and TB enhance each other’’s s pathogenicitypathogenicity, , resulting in dual epidemicresulting in dual epidemic–– All TB patients should be tested for HIV and HIV patients All TB patients should be tested for HIV and HIV patients
checked for TBchecked for TB
LTBI progression to TB is a significant riskLTBI progression to TB is a significant risk Diagnosis is more difficult Diagnosis is more difficult
–– Symptoms may be minimal, atypical or absentSymptoms may be minimal, atypical or absent–– Presentations are often unusualPresentations are often unusual
Treatment of TB and HIV is more complicatedTreatment of TB and HIV is more complicated–– Drug toxicities/interactions are frequent, drug resistanceDrug toxicities/interactions are frequent, drug resistance
IRIS may mimic treatment failure or new infectionIRIS may mimic treatment failure or new infection

8
Case Presentation (BCase Presentation (B--1)1)
41 year old man presents to the ER at Charity 41 year old man presents to the ER at Charity with headache for 3 dayswith headache for 3 days
No relief with over the counter acetaminophenNo relief with over the counter acetaminophen Nausea, mild neck stiffnessNausea, mild neck stiffness No vomiting, no blurry vision, no mental status No vomiting, no blurry vision, no mental status
changes or problems speaking no shortness of changes or problems speaking no shortness of breath, no coughbreath, no cough
PMH: Sexual transmitted infectionsPMH: Sexual transmitted infections Social History: No tobacco, alcohol, or illicit drug Social History: No tobacco, alcohol, or illicit drug
useuse
Case Presentation (BCase Presentation (B--2) 2) Physical Examination (PE)Physical Examination (PE) AF, VSS (Afebrile, vital signs stable)AF, VSS (Afebrile, vital signs stable) PE: WNL (within normal limits)PE: WNL (within normal limits) A&O X 3 (alert and oriented) cognition is normalA&O X 3 (alert and oriented) cognition is normal Cranial nerves: II Cranial nerves: II -- XII grossly intactXII grossly intact Fundoscopy: mildly blurry disc marginsFundoscopy: mildly blurry disc margins, no , no
venous pulse appreciatedvenous pulse appreciated Motor: 5/5 strength upper and lower extremitiesMotor: 5/5 strength upper and lower extremities Sensory: intactSensory: intact Cereballar function: intactCereballar function: intact DTRDTR’’s: 2+ bilaterallys: 2+ bilaterally
Case Presentation (BCase Presentation (B--3) 3) LaboratoryLaboratory WBC: 4.1 WBC: 4.1
–– SS7373 BB44 LL1212 MM1010 EE11
Hgb: 13.8Hgb: 13.8 Hct: 41Hct: 41 Plt: 246Plt: 246
Chemistry WNLChemistry WNLBilateral reticulonodular pattern with upper zone predominance. Differential diagnosis includes infectious process (TB is a consideration)versus neoplastic process. Bilateral hilar predominance.
CXR

9
Case Presentation (BCase Presentation (B--4) 4) CT MRICT MRI
Cerebellar vermian mass (1.8 cm) with associated vasogenic edema
Cerebellar mass lesion with two predominant ring enhancing components.
Differential diagnosis:Immunocompetent: hemangioblastoma, astrocytoma, met malignancyImmunocompromise: toxoplasmosis, lymphoma
Case Presentation (BCase Presentation (B--5) 5) Chest CT Chest CT
Micro nodular opacities
Nodularity with architectural distortion
HIV: ReactiveCD4: 152, 25.3%, ratio 0.5TST: Negative
Case Presentation (BCase Presentation (B--6) 6) Hospital Course Hospital Course -- Microbiology resultsMicrobiology results
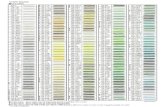
TestTest SmearSmear CultureCulture
Sputum AFB x 4Sputum AFB x 4 Smear negativeSmear negative
AFB Blood CXAFB Blood CX
BAL AFB x2BAL AFB x2 Smear negativeSmear negative
Case Presentation (BCase Presentation (B--7) 7) Hospital Course Hospital Course -- Microbiology resultsMicrobiology results
TestTest SmearSmear CultureCultureSputum AFB x 4Sputum AFB x 4 Smear negativeSmear negative
AFB Blood CXAFB Blood CX
BAL AFB x2BAL AFB x2 Smear negativeSmear negative
Brain BiopsyBrain Biopsy Pus on gram stains.Pus on gram stains.No organismsNo organisms
Brain Biopsy:Brain Biopsy:viral, fungal, and viral, fungal, and bacterial cultures bacterial cultures
NegativeNegative
Brain swabBrain swab Numerous AFB seenNumerous AFB seen
Brain swab cultureBrain swab culture NegativeNegative

10
Case Presentation (BCase Presentation (B--8) 8) Hospital Course Hospital Course -- Microbiology resultsMicrobiology results
TestTest SmearSmear CultureCultureSputum AFB x 4Sputum AFB x 4 Smear negativeSmear negative + + MtbMtbAFB Blood CXAFB Blood CX + + MtbMtbBAL AFB x2BAL AFB x2 Smear negativeSmear negative + + MtbMtbBrain BiopsyBrain Biopsy Pus on gram stains.Pus on gram stains.
No organismsNo organismsBrain Biopsy:Brain Biopsy:viral, fungal, and viral, fungal, and bacterial cultures bacterial cultures
NegativeNegative
Brain swabBrain swab Numerous AFB seenNumerous AFB seen + + MtbMtbBrain swab cultureBrain swab culture NegativeNegative
Case Presentation (CCase Presentation (C--1)1)
40 years old, HIV (+), 2 months pregnant40 years old, HIV (+), 2 months pregnant Boyfriend just diagnosed with active pulmonary TB Boyfriend just diagnosed with active pulmonary TB She does not have any symptoms of active TBShe does not have any symptoms of active TB
QuestionsQuestionsAppropriate management would include:Appropriate management would include:
A. A tuberculin skin test A. A tuberculin skin test -- (on a pregnant woman)?(on a pregnant woman)? B. An anergy panel? B. An anergy panel? C. A chest xC. A chest x--ray ray –– (wait until after first trimester)? (wait until after first trimester)? D. Treatment for LTBI?D. Treatment for LTBI?
Case Presentation (CCase Presentation (C--2)2)
A. Skin testing on pregnant or nursing woman is safeA. Skin testing on pregnant or nursing woman is safe
B. Anergy testing no longer routinely recommendedB. Anergy testing no longer routinely recommended•• Cannot r/o diagnosis based on negative skin test Cannot r/o diagnosis based on negative skin test –– Overwhelming TB disease, severe or febrile illness, viral infecOverwhelming TB disease, severe or febrile illness, viral infectiontion–– LiveLive--virus vaccinations (MMR)virus vaccinations (MMR)
C. C. CXR CXR -- Shielding consistent with safety guidelines Shielding consistent with safety guidelines even during first trimester of pregnancyeven during first trimester of pregnancy
D. HIV infected persons and children D. HIV infected persons and children <<4 years old exposed to 4 years old exposed to an infectious case of TB, should be treated with INH after an infectious case of TB, should be treated with INH after active TB has been r/oactive TB has been r/o
Case Presentation (CCase Presentation (C--3)3)
Skin test results Skin test results -- positive at 5mm positive at 5mm No symptoms and CXR is normalNo symptoms and CXR is normal
Appropriate management would include Appropriate management would include which of the following regimens?which of the following regimens?
a.a. 2 months of PZA and Rifampin2 months of PZA and Rifampinb.b. 4 months of Rifamycin4 months of Rifamycinc.c. 6 months of INH6 months of INHd.d. 9 months of INH9 months of INH

11
Case Presentation (CCase Presentation (C--4)4)Answer: dAnswer: d Treatment of latent TB infection for Treatment of latent TB infection for HIV HIV
positive and negativepositive and negative is the sameis the same Recommend 9 months of INHRecommend 9 months of INH Acceptable alternative Acceptable alternative
–– 4 months of Rifampin4 months of Rifampin–– 6 months INH6 months INH
PZA and RIF is no longer recommended due PZA and RIF is no longer recommended due to hepatotoxicity to hepatotoxicity
MMWR Morb Mortal Wkly Rep 2003 Aug 8;52(31):735-9 Update: adverse event data and revised ATS and CDC recommendations against the use of RIF and PZA for treatment of LTBI-United States, 2003.