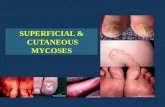
Superficial and cutaneous mycoses
-
Upload
dr-vrk-womens-medical-college -
Category
Education
-
view
1.407 -
download
1
description
Transcript of Superficial and cutaneous mycoses

Superficial Mycoses
Dr. Pendru Raghunath Reddy

SUPERFICIAL MYCOSES The superficial mycoses are usually confined to the outermost
layer of skin, hair, mucosa and do not invade living tissues

Superficial mycoses
• Do not elicit immune response• No discomfort • Cosmetic problems• Limited to stratum corneum

Superficial Mycoses
1. Pityriasis versicolor
2. Tinea nigra
3. Black piedra
4. White piedra

Pityriasis Versicolor
Caused by Malassezia furfur (Pityrosporum orbiculare) lipophilic yeast Found as a normal flora on the skin Rich in sebaceous glands Grows on media supplemented with fatty acids Exist in budding yeast,occasionally hyphal
Diseases : Pityriasis versicolor Pityriasis folliculitis Seborrhoeic dermatitis; Dandruff Systemic infection

Major clinical manifestations:
– Hyper- or hypopigmented of the skin
– Lesions are well-demarcated (white, pink or brownish)
– Fawn-colored macules are the most common presentation
Trunk and upper arms
Rarely on neck and face



Pityriasis folliculitis
follicular papules and pustules
back, chest and upper arms
sometimes the neck, seldom the face
Itchy and often appear after sun exposure

Pityriasis folliculitis

Seborrhoeic dermatitis
Changes in quantity and composition of sebum increase in wax esters shift from triglycerides to shorter fatty acid chains
Increase in alkalinity of skin
External local factors such as occlusion

Clinical manifestations:
Erythema and scaling in areas with a rich supply of sebaceous glands
scalp, face, eyebrows, ears and upper trunk
Lesions are covered with greasy scales
Itching is common in the scalp

14

Laboratory diagnosis
Specimen: Skin scrapings
Methods:
1. KOH preparation
2. Culture
KOH preparation
Both budding yeast cells and hyphae can be demonstrated
Shows characteristic ‘spaghetti and meatballs’ appearance

•Short fragments of hyphae•clusters of yeast• Spaghetti and meatballs appearance

Culture
M. furfur requires fatty acids for growth, hence is cultured on SDAwith a layer of olive oil
Colonies of M. furfur on Dixon's agar. A specialized isolation medium containing glycerol-mono-oleate

Management and Treatment:
1. Topical agent: imidazole (Ketoconazole shampoo)
2. Oral treatment : ketoconazole, itraconazole
3. Alternative: zinc pyrithione shampoo
• selenium sulfide lotion
• propylene glycol 50% in water twice daily

TINEA NIGRA
• Tinea nigra is an infection of keratinised layer of skin caused by Exophiala werneckii or Cladosporium werneckii
• C. werneckii is a dimorphic fungus that produces melanin

•palmar•brown•no scaling•no inflammation
A well-demarcated brown-black macular lesions which usually occur on the palmar aspects of hands and occasionally the plantar and other surfaces of the skin
Lesions are non-inflammatory and non-scaling

Laboratory diagnosis
KOH preparation
Microscopy of the KOH preparation of skin scrapings collected from the affected part
Typical darkly pigmented yeast-like cells and hyperfragmented hyphae are demonstrated

Culture
Initially colonies are mucoid, yeast-like and shiny black (young yeast)
Abundant aerial mycelia and become velvety, dark olivaceous in colour. (mature mould)

Management & Treatment
Sulfur soap, SSA, azoles
Topical treatment Whitfield's ointment (benzoic acid compound) Imidazole agent twice a day for 3-4 weeks
23

Black Piedra
• Black piedra is a superficial infection of the hair caused by Piedraia hortae, a dematiaceous fungus
Clinical Manifestations
Does not penetrate the hair follicle
presence of hard nodules found along the infected hair shaft
Nodules: hard, fusiform, firmly attached to hair shaft

Laboratory diagnosis
Demonstration of nodules containing asci with spindle shapedascospores in 10% KOH mount of the hair


Culture

Management and Treament
Shave or cut the hairs short
Terbinafine Dose: 250 mg a day for 6 weeks

White Piedra
• Infection of the hair caused by yeast-like organism Trichosporon beigelli
• Commonly found in South America, Central and Eastern Europe and Japan
• The hair of scalp, moustache, and beard are commonly affected
• The development of a soft, pasty, cream-colored growth along infected hair shaft characterizes the condition
• The initial growth occurs beneath the epidermis of hair• The infected hair shaft consists of mycelium that rapidly
fragments to arthroconidia

In this picture we see hair with white piedra (Trichosporon beigelii). Note that, when this module is compared with that seen in black piedra, it is not as discrete and lacks the dark coloration. Additionally, this fungus does not produce ascospores. When cultured on Sabouraud’s agar and incubated for 2-4 weeks at room temperature, this fungus produces a rough, membranous, white to light tan colony. Microscopically, the organism produces no characteristic spores.

Laboratory diagnosis
1. Direct Microscopy
Fragmented hyphae that develop into arthroconidia or produce blastoconidia in 10% KOH mount of hair

This is a 4-5 weeks old culture of Trichosporon beigelii grown on SDA agar at room temperature
2. Culture
Grown on SDA with cycloheximideWhite or yellowish to deep cream coloredSmooth, wrinkled, velvety, dull colonies with a mycelial fringe

Management and Treatment
Shave the hairs
Topical: imidazole agent









![superficial mycoses2 [Read-Only]iacld.ir/DL/workshop/superficialmycosesdrhashemi.pdf · Superficial MycosesSuperficial Mycoses PityriasisversicolorPityriasis versicolor Pityrosporosis](https://static.fdocuments.net/doc/165x107/5f0fe88d7e708231d4467c62/superficial-mycoses2-read-onlyiacldirdlworkshopsuperfi-superficial-mycosessuperficial.jpg)