Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
-
Upload
marcelliawharsono -
Category
Documents
-
view
214 -
download
0
Transcript of Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf

7/23/2019 Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
http://slidepdf.com/reader/full/stewart-prevalence-of-migraine-ha-in-the-us-jama-1992pdf 1/6
Prevalence of Migraine Headachein the United States
Relation to Age, Income, Race, and OtherSociodemographic Factors
Walter F. Stewart, PhD, MPH; Richard B. Lipton, MD; David D. Celentano, ScD; Michael L. Reed, PhD
Objective.\p=m-\Todescribe the magnitude and distribution of the public healthproblem posed by migraine in the United States by examining migraine prevalence,attack frequency, and attack-related disability by gender, age, race, household in-
come, geographic region, and urban vs rural residence.
Design.\p=m-\In1989, a self-administered questionnaire was sent to a sample of15000 households. A designated member of each household initially respondedto the
questionnaire. Each household member with severe headache was asked
to respond to detailed questions about symptoms, frequency, and severity ofheadaches.
Setting.\p=m-\Asample of households selected from a panel to be representativeof the US population in terms of age, gender, household size, and geographic area.
Participants.\p=m-\Aftera single mailing, 20468 subjects (63.4% response rate)between 12 and 80 years of age responded to the survey. Respondents and non\x=req-\
respondents did not differ by gender, household income, region of the country, or
urban vs rural status. Whites and the elderly were more likely to respond. Migraineheadache cases were identified on the basis of reported symptoms using estab-
lished diagnostic criteria.
Results.\p=m-\17.6% of females and 5.7% of males were found to have one or more
migraine headaches per year. The prevalence of migraine varied considerably byage and was highest in both men and women between the ages of 35 to 45 years.
Migraine prevalence was strongly associated with household income; prevalencein the lowest income group (<$10 000) was more than 60% higher than in the two
highest income groups (\m=ge\$30000).The proportion of migraine sufferers who ex-
perienced moderate to severe disability was not related to gender, age, income,urban vs rural residence, or region of the country. In contrast, the frequency ofheadaches was lower in higher-income groups. Attack frequency was inverselyrelated to disability.
Conclusions.\p=m-\Aprojection to the US population suggests that 8.7 million fe-males and 2.6 million males suffer from migraine headache with moderate to severe
disability. Of these, 3.4 million females and 1.1 million males experience one or
more attacks per month. Females between ages 30 to 49 years from lower-incomehouseholds are at especially high risk of having migraines and are more likely thanother groups to use emergency care services for their acute condition.
(JAMA. 1992;267:64-69)
WHILE migraine is a common disablingcondition,110 little is known about the
From the Departments of Epidemiology (Dr Stewart)and Health Policy and Management (Dr Celentano),The Johns Hopkins University, Baltimore, Md; t he De-
partment of Neurology, Albert Einstein College ofMedicine, New York, NY (Dr Lipton); and Glaxo Inc,Research Triangle Park, NC (Dr Reed).
Reprint requests to Department of Epidemiology,School of Hygiene and Public Health, The Johns Hop-kins University, 615 N Wolfe St, Baltimore, MD 21205
(Dr Stewart).
variation in migraine prevalence by age,income, race, urban vs rural living, andother sociodemographic variables
thought to be related to medical care
access and utilization. Previous studieshave often been limited to narrowly de¬fined populations. Moreover, estimatesof migraine prevalence have varied
widely, possibly in part because of dif¬ferences in sociodemographic featuresof the study samples and differences in
the definition of a migraine case. No
study has estimated the prevalence of
migraine in a representative sample ofthe US population.
In the present study, the magnitudeand distribution of the public health
problem posed by migraine in the United
States is described using data from a
nationwide sample of more than 20 000respondents. This survey is the first toestimate migraine prevalence by a num¬
ber of sociodemographic factors, includ¬ing race, income level, region of the coun¬
try, and urban vs rural residence, andto employ a case definition based on cri¬teria recommended by the InternationalHeadache Society (IHS).11 The surveycovers the broadest age range reportedto date, including subjects from 12 to 80
years. All regions of the United Statesare included. Information is providedthat identifies groups a t highest risk of
migraine and migraine-related disabil¬ity and that provides opportunities to
identify barriers to effective medicaltreatment.
METHODS
SampleHeadache histories were ascertained
through a questionnaire mailed to UShouseholds. A market research firm,National Family Opinion Ine (NFO),Toledo, Ohio, maintains a panel of200000 households nationwide formarketing, opinion, and other types
of surveys.Potential NFO panel households are
initially selected as a stratified proba¬bility sample to be representative of theUS population with regard to urban vs
rural residence, age of the head of the
household, household income, and size.Households are recruited by volunteer
response to an initial mailing. A follow-
up mailing is conducted to obtain a de¬tailed household census and demographicinformation. Recruited households are
randomly assigned to one of 40 blocks of5000 households each. Every 2 years
at Albert Einstein College of Medicine on December 29, 2009www.jama.comDownloaded from

7/23/2019 Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
http://slidepdf.com/reader/full/stewart-prevalence-of-migraine-ha-in-the-us-jama-1992pdf 2/6
updated household census and demo¬
graphic information is obtained. In ad¬dition, 30% of each sampling block is
replaced. Households that are persis¬tent nonresponders to periodic surveysare removed from the sampling frame.In general, the NFO sampling frame isskewed toward but not limited to upper-income white households.
SurveyIn 1989, a self-administered question¬naire was sent to a stratified random
sample of 15 000 NFO panel households(three sampling blocks). A designatedmember from each household respondedto the questionnaire by reporting thenumber of members in the householdand the number who suffer from severe
headache. The study is limited to self-defined severe headache because thisconstitutes the most significant health
problem from the sufferer's point ofview. The consequences of this designchoice are
explored in the "Comment"
section.Each household member with severe
headache was asked to complete the
questionnaire. Detailed questions were
asked about severe headaches, includ¬
ing specific accompanying symptoms andfrequency of and disability from severe
attacks. A total of 9507 (63.4%) of the15 000 households responded to a singlequestionnaire mailing, for a total basepopulation of 23611 individual house¬hold members. Subjects less than 12
years old (n = 3043) were excluded fromthe analysis because of concerns regard¬
ing ability to reliably respond to andinterpret questions. We report on re¬
sponses of the 20468 subjects between12 and 80 years of age. One hundred
respondents were excluded because gen¬der was not reported.Measures
Subjects were asked questions about
eight specific symptoms associated withheadache: nausea; vomiting; unilateralhead pain; pulsating/throbbing pain; sen¬
sitivity to light (photophobia); sensitiv¬
ity to sound (phonophobia); seeing shim¬mering lights, circles, other shapes, or
colors before the eyes before a headache(visual scotoma); and numbness of the
lips, tongue, fingers, or legs before theheadache pain. Cases met criteria con¬
sistent with the IHS definition for mi¬
graine.11 Specifically, migraine cases
were respondents with at least one se¬
vere headache in the last 12 months whodid not experience headache every dayand who had one of the following sets ofsymptoms with their severe headaches:(1) unilateral or pulsatile pain and eithernausea or vomiting or phonophobia with
photophobia or (2) visual or sensory aura
before the headache. Subjects who didnot meet these criteria were simply de¬fined as having severe headache.
Three levels of disability were defined:severe disability if headache requiredbed rest, moderate disability if head¬ache severely impaired working abilityor activity, and mild disability if head¬ache impaired working ability or activ¬
ity to some degree. Otherwise, subjectswere not considered to be disabled fromtheir reported severe headaches.
Response categories for the frequencyof severe headache were as follows: ev¬
ery day, two to six times per week, once
per week, one to three times per month,and one to 12 times per year. Subjectswith severe headache every day were
excluded as migraine cases.
AnalysisSex-specific prevalence estimates of
active severe migraine headache suffer¬ers were derived by age, race, urban vs
rural residence, household
income, and
region of the country. GLIM Poissonregression (log-linear models)12 was usedto model sex- and age-specific preva¬lence by income and to derive adjustedprevalence ratios. Preliminary analysisshowed that males and females differedsubstantially both in the absolute prev¬alence of migraine and by covariates.Data were therefore modeled separatelyby gender. Age was divided into thir¬teen 5-year categories (the first age cat¬
egory, 12 through 19 years, was an e x¬
ception) and modeled as a continuousvariable. Two race groups (blacks and
whites), three urban vs rural groups(population <50000, 50000 to 500000,and >500000), and five household in¬come groups (<$10000, $10000 to
$19999, $20000 to $29999, $30000 to$44 999, and >$45 000) were defined. Asa reference, $24897 was the medianhousehold income in the United Statesin 1986.13 Six regions of the United Stateswere defined: New England, Atlantic,North Central, South Central, Moun¬tain, and Pacific. Individuals with otherand unknown race were excluded when
estimating crude and adjusted preva¬lence ratios because the groups were
too small to derive stable estimates.The 2 test was used to determine
whether a single variable (race, age,income, etc) significantly improved thefit of the log-linear model to the data.14The degrees of freedom for each testwere equal to the number of categoriesfor that variable minus 1. Crude andadjusted prevalence ratios were derivedas the ratio of migraine prevalence inone category of a variable vs a referencecategory (eg, prevalence in the higher-income groups vs the lowest incomegroup).
Table 1.—Distribution of Total Population and
Respondents
VariableTotal,
No. Respondents,
No. (%)Sex
MF
RaceBlackWhiteOtherUnknown
Age, y
12-1718-2930-3940-4950-592=60
RegionMountainNew EnglandAtlanticNorth CentralSouth CentralPacific
Urban vs rural<50 0 00 (rural)50 00 0 to
500 000500 0 00 to
2 000 000>2 000 000
Household size123425
Household income, Í<10 00010 000 to 19 99920 00 0 to 29 99 930 000 to 44 999==45 000
Total
1551317 28 8
127130 618
598314
321567036997501238117063
17791813
10910798356894627
9379
6520
587211 030
36509258698368876023
45365964580974359057
32 801
9660 (62.3)10 808 (62.5)
618 (48.6)19 464 (63.6)
225 (37.6)161 (51.3)
1904 (59.2)3518 (52.5)3979 (56.9)3123 (62.3)2583 (67.8)5361 (75.9)
1133 (63.7)1147 (63.3)6737 (61.8)5296 (66.3)3345 (58.8)2810 (60.7)
5790 (61.7)
4041 (62.0)
3799 (64.7)6838 (62.0)
2462 (67.5)6407 (69.2)4155 (59.5)4095 (59.5)3349 (55.6)
2739 (60.4)3711 (62.2)3615 (62.2)4672 (62.8)5731 (63.3)
20 46 8 (62.4)
RESULTS
Response Rate
Characteristics of survey respon¬dents are displayed in Table 1. Over¬all, 63.4% of all households and 62.4%of the total population participated inthe mailed questionnaire survey. The
response rate did not differ by sex,urban vs rural residence, householdincome, or region of the country, withthe exception of a lower response rate(58.8%) in the South Central UnitedStates. By race, the response ratewas higher among whites (63.6%)than blacks (48.6%) and other race
groups (37.6%). By age, the responserate was
highest among the
elderly(75.9%) and lowest among adults 18to 29 years (52.5%). The age distribu¬tion of respondents is consistent withthe known lower response rate to sur¬
veys among more mobile popula¬tions.15 Smaller households were more
likely to respond than larger house¬holds, representing in part the agedistribution of respondents.Prevalence and
Sociodemographic Variation
Crude Estimates.—A total of 17.6%of females and 5.7% of males between 12
at Albert Einstein College of Medicine on December 29, 2009www.jama.comDownloaded from

7/23/2019 Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
http://slidepdf.com/reader/full/stewart-prevalence-of-migraine-ha-in-the-us-jama-1992pdf 3/6
Table 2.—Sex-Specific Prevalence of Migraine and Total Severe Headache by Race, Household Income,Urban vs Rural Community, and Region of the United States
Variable
Prevalence (No. of Subjects)
Migraine All Severe Headaches
RaceBlack 17.4 (67) 3.3 (8) 27.2 (2787) 13.8 (1273)White 17.6 (1803) 6.1 (561) 28.8 (209) 16.3 (39)Other 12.3 (10) 2.5 (2) 21.2 (18) 15.8 (12)
Unknown 15.9 (22) 4.7 (6) 31.9 (36) 12.5 (14)Household Income, $<10 000 20.8 (374) 7.4 (70) 34.7 (623) 19.7 (186)10 000 to 19 999 17.8 (368) 6.6 (108) 28.1 (582) 15.1 (248)20 000 to 29 999 17.9 (328) 5.9 (142) 27.4 (506) 14.9 (263)30 000 to 44 99 9 16.3 (367) 5.9 (142) 24.2 (548) 12.5 (302)Ï45 000 16.3 (465) 5.3 (153) 24.4 (691) 11.7 (339)
Urban vs rural<50 000 19.7 (615) 6.2 (165) 30.7 (962) 15.5 (412)50 000 to 500 0 00 17.6 (386) 5.8 (109) 26.9 (585) 13.3 (249)>500 00 0 16.4 (901) 6.0 (303) 25.5 (1403) 13.0 (667)
RegionNew England 17.5 (107) 4.9 (26) 25.2 (154) 12.3 (66)Mountain 19.5 (115) 7.0 (38) 27.2 (161) 13.3 (72)Atlantic 17.7 (637) 5.8 (188) 27.3 (983) 13.6 (427)North Central 22.6 (147) 5.6 (138) 27.0 (760) 13.3 (330)South Central 18.2 (317) 6.6 (100) 29.6 (516) 15.8 (253)Pacific 17.2 (249) 6.4 (87) 26.0 (376) 13.9 (190)
Total 17.6 (1902) 5.7 (577) 27.3 (2950) 13.9 (1338)
Table 3— Crude and Adjusted Sex-Specific Prevalence Ratios of Migraine by Race, Household Income,Urban vs Rural Community, and Region of the United States
Prevalence Ratio*
Variable95% Confidence 95% Confidence
Crude Adjusted! Limits Crude Adjustedf Limits
RaceWhite 1.00 1.00 1.00
Black 1.01 0.84 (0.65,1.08) 0.54 0.50 (0.25, 0.98)Household income, $
<10000 1.00 1.00
10 00 0 to 19 999 0.86 0.79 (0.68,0.91) 0.89 0.88 (0.65,1.21)20 00 0 to 29 99 9 0.86 (0.59, 0.80) (0.50, 0.93)30 00 0 to 44 99 9 (0.50, 0.63) 0.79 0.64 (0.48, 0.86)3=45 000 0.78 0.58 (0.50, 0.69) 0.71 0.56 (0.42, 0.76)
Urban vs rural>50 000 1.00 1.00 1.00 1.00
50 000 to 500 000 0.89 0.93 (0.81, 1.06) 0.94 0.99 (0.77, 1.27)>500 000 0.83 0.91 (0.81,1.01) 0.97 (0.87, 1.31)
RegionNew England 1.00 1.00 1.00 1.00
Mountain (0.82, 1.40) 1.34 1.28 (0.72,2.15)Atlantic 1.02 1.01 (0.82,1.24) 1.25 1.26 (0.83, 1.91)
North Central (0.85,1.30) 1.18 1.14 (0.74, 1.75)South Central 1 05 1.00 (0.80, 1.25) 1.31 1.27 (0.82, 1.98)Pacific 0.97 (0.78, 1.23) (0.76,2.16)
•Comparing subgroup with a reference group (with a designated prevalence ratio of 1.00).tAdjusted for age, race, income, urban vs rural community, and region of the United States.
and 80 years of age met the case defi¬nition for migraine headache (Table 2) .The crude prevalence estimate of mi¬
graine in black females is similar to thatin white females but is lower in blackmales than in white males. Migraineprevalence is lower in higher-income
groups and in females living in largermetropolitan areas.
While there is no striking regionalpattern, the prevalence of migraine ap¬pears to be high among both males andfemales living in the Mountain region.In contrast, with one exception, New
England has the lowest gender-specificprevalence of migraine.
Migraine accounts for 64.4% of all fe¬male severe headache sufferers and 43%of a ll male severe headache sufferers.The pattern of severe headache preva¬lence by sociodemographic factors was
similar to that observed for migraineprevalence (Table 2).
Adjusted Estimates.—Because a
number of covariates, including age,were found to be associated with eachother, GLIM Poisson regression was
used to adjust for possible confoundingwhen estimating prevalence by eachvariable. Among males, age ( 2 = 20.4,df=l, P<.001) and age squared( 2 = 57.4, df=l, P<.001) significantlyimproved the fit of the model to the
data, followed by income ( 2 =19.4,ri/=4,P<.001)andrace(x2 =4.4,d/=l,P<.05). Among females, age ( 2 = 62,df=l, P<.001), age squared ( 2 = 341,d/=l, P<.001), age cubed ( 2= 30.1,
df=l, P<.001), and income
( 2=
73.8,df=4, P<.001) each significantly im¬proved the fit of the model to the data.Race was not significant among females.Urban vs rural residence, region, andinteraction terms between income or
race and age did not significantly im¬
prove the fit of the log-linear model tothe data. The significant age squaredterm in these models indicates that mi¬
graine prevalence has a nonlinear rela¬tion with age. The significant age cubedterm for females primarily affects the
"sharpness" of the peak and the steep¬ness of the rise and decline in migraine
prevalence with age. All covariates, ex¬cept age cubed in males, were includedin the final model to derive adjustedprevalence ratios by race, income, ur¬
ban vs rural residence, and region andto derive sex- and age-specific preva¬lence estimates by income.
After adjusting for other covariates,the prevalence of migraine was not sig¬nificantly different between black andwhite females. The adjusted prevalencewas lower among black males than whitemales (Table 3). The difference was sta¬
tistically significant (P<.05).The
prevalenceratio of
migraine, com¬
paring higher-income groups with thelowest income group, decreased with
increasing household income (Table 3).A consistent trend was found amongboth males and females. After adjustingfor other covariates, the prevalence of
migraine among females in the two high¬est income groups ($30000 to $44999and s$45 000) was, on average, only 59%of the prevalence observed for the low¬est income group (<$10000), followedin order by prevalence ratios of 0.69 and0.79 in the $20 000 to $29 999 and $10 000to $19 999 income groups, respectively.
at Albert Einstein College of Medicine on December 29, 2009www.jama.comDownloaded from

7/23/2019 Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
http://slidepdf.com/reader/full/stewart-prevalence-of-migraine-ha-in-the-us-jama-1992pdf 4/6
0.4-
0.0-
- <$10000. $10000-$19999-$20000-$29999- >$30000
20
Females
- "
30 40- -
50 60 70 80
0.20-
0.15·
0.05-
0.0-
- <$10000
.
$10000-$19999
-$20000-$29999-$30000-$44999
-
>$45000
Males
20 —r-
30- -
40 —r-
50 —I-
60- -
70 —r
80
Age, y
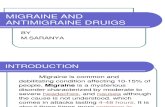
Age-specific prevalence of migraine by household Income among female and male respondents in a 1989national survey.
Males exhibited a similar pattern. Prev¬alence in the two highest income groupswas, on average, 59% (3=$45000) and64% ($30000 to $44999) of the preva¬lence in the lowest income group. Ur¬ban vs rural residence (population den¬
sity) was not significantly associatedwith migraine prevalence. Among fe¬
males, the prevalence ratios were lower
in urban vs rural
populations (Table 3),but the differences were not statisti¬
cally significant. Among males, no spe¬cific pattern emerged.
The sex- and age-specific prevalenceofmigraine by income group (in females,age-specific prevalence in the two high¬est income groups was similar andtherefore w as combined) is displayed inthe Figure. Among females, migraineprevalence increased sharply up to age40 years and declined monotonicallythereafter. The peak prevalence in thelowest income group was more than 40%compared with 22% in the highest in-
come group. The prevalence of migrainewas still relatively high for all income
groups, even at age 60 years in females.While a similar age-specific pattern was
found among males, it wa s not as strik¬
ing (note the difference in the preva¬lence scales in the Figure). Prevalence
slowly increased and decreased over a
broader age range. The highest age-
specific prevalence in males
(12% and
7% in the lowest and highest income
groups) occurred at a slightly youngerage than that found in females.
The age-specific sex ratio also varied
considerably by age, a reflection of the
contrasting age-specific prevalence pat¬terns among males and females. The
average prevalence sex ratio (averageof the age-specific ratios) was approxi¬mately 2.8. At age 12 years the ratiowas below 2.0, increasing sharply afterthis age and peaking at 3.3 between 40and 45 years. It is noteworthy that, even
after the age of menopause, the sex ra-
tio continues to be elevated above 2.0.While both females and males living
in the Mountain region of the UnitedStates exhibited a higher prevalence ofmigraine after adjusting for other co¬
variates, no region had a prevalence ofmigraine significantly different from thatof New England.
Frequency of Attacks and Disability
Female migraine sufferers reportedmore frequent attacks than their malecounterparts. Among those reportingsevere migraine headache in the last
year, approximately 59% (1158 of 1964)of females and 50% (303 of 611) of malesreported one or more severe headachesper month. In contrast, small genderdifferences were found among migrainesufferers in the occurrence of disability(Table 4). Among migraine sufferers,86% of females and 82% of males re¬
ported some disability from their se¬
vere headaches; 47% offemales and 43%of males
reported moderate
to severe
disability. Moderate to severe disabilityfrom headache was more common amongthose with fewer attacks per year (datanot shown). For example, among femaleswith one to 12 severe headaches peryear, 56.5% reported moderate to se¬
vere disability from their headache com¬
pared with 36.2% of females with one
severe headache per week.After adjusting for other covariates,
attack frequency decreased as house¬hold income increased for both malesand females (Table 4). On the otherhand, attack frequency was not associ¬
ated with race, urban vs rural resi¬dence, region of the country, or age.Similarly, moderate to severe disabilityamong migraine sufferers was not re¬
lated to race, income, urban vs rural res¬
idence, or region of the country in eitherfemales or males. It is noteworthy, how¬
ever, that black male migraine sufferers
reported more frequent severe head¬aches (prevalence ratio, 1.8) but less fre¬quent disability from their severe head¬aches (prevalence ratio, 0.57) than whitemales. Finally, the proportion ofmigrainesufferers who experience moderate to se¬
vere
disability does not
appear to changewith age. Thus, while the prevalence ofsevere migraine decreased with age, itappears that the proportion with disabil¬ity among those currently suffering from
migraine does not change with age.
COMMENT
Prevalence is a measure that reflectsboth the incidence of new cases and the
persistence of disease. Valid estimatesof prevalence are informative about the
public health toll and societal costs fromspecific diseases. We have provided de¬tailed descriptions of the age pattern of
at Albert Einstein College of Medicine on December 29, 2009www.jama.comDownloaded from

7/23/2019 Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
http://slidepdf.com/reader/full/stewart-prevalence-of-migraine-ha-in-the-us-jama-1992pdf 5/6
Table 4.—Adjusted Sex-Specific Prevalence Ratlos of Frequent and Moderate to Severe Disabling MigraineHeadaches by Race, Household Income, Urban vs Rural Community, and Region of the United States
Adjusted Prevalence Ratio*
Variable Frequent
Attacks DisabilityFrequentAttacks
RaceWhite 1.00 1.00 1.00 1.00
Black 1.00 1.83 0.58
Household income, $<10 000 1.00 1.00 1.00 1.00
10 000 to 19 999 0.91 0.74 0.97
20 000 to 29 999 0.93 0.78 1.09
30 000 to 44 999 0.94 0.99 0.60 1.02
a45 000 0.81 1.03 0.71 1.02
Urban vs rural<50 000 1.00 1.00 1.00
50 000 to 500 000 0.98 0.85 0.96
< 500 000 1.05 1.06
RegionNew England 1.00 1.00 1.00
Mountain 1.02 0.66 0.87 1.36
Atlantic 1.16 0.76 0.98 0.99
North Central 1.12 0.72 1.04 0.88
South Central 1.17 0.65 0.87 1.36Pacific 0.67 0.86
•Comparing subgroup with a reference group (with a designated prevalence ratio of 1.00), adjusted for age, race,income, urban vs rural community, and region of the United States.
migraine prevalence and examinedwhether migraine prevalence varies bya number of demographic factors.
The overall prevalence estimates of
migraine in our study, 17.6% in femalesand 5.7% in males, are lower than those
reported in most other studies.18 Thereare two possible reasons for the differ¬
ences. First, symptom histories wereobtained only from self-defined severe
headache sufferers. Migraineurs who ex¬
perience moderate pain and little or no
disability16 are likely to have been ex¬
cluded. Second, we employed a some¬
what strict case definition consistentwith that of the IHS.11 Our criteria dif¬fer with those of the IHS in that we didnot consider the lifetime number of pre¬vious attacks of migraine or headacheduration (3 to 72 hours). However, the
overwhelming majority of cases in our
study are likely to have met these cri¬teria. Finally, the rare cases of migraineattributable to organic disease could notbe excluded, and we did not employ theIHS criteria of increased headache se¬
verity on exertion.In previous population-based studies,
prevalence estimates18 of migraine havevaried widely and for this reason havebeen questioned.17 Overall, prevalencehas ranged from 5.3%5 to 19%2 in malesand from 11%S to 28%2 in females. Ourstudy suggests that the variation ob¬served among previous studies may beexplained in part by sociodemographicdifferences in the samples studied. For
example, most studies tend to focus on
younger age groups1·3,4,7,8 or only on fe¬males1,3,7 and therefore cannot be gen¬eralized to more broadly defined popu¬lations.
The prevalence of migraine peaks be¬tween 35 to 40 years, occurring slightlyearlier for males. Where sufficient datahave been available over a broad age
range,2,5·6 the prevalence of migraine de¬creases with age beginning in the 30sfor males and in the late 40s for females.
Migraine is reported to be two to fourtimes more common in females than inmales.19 Our data show that the genderratio varies considerably by age, rang¬ing from 2.0 to 3.3. Differences in the
age distribution between previous stud¬ies may account for the wide range in
gender ratios reported to date.The highest gender ratio in our study
was found between the ages of 30 to 45
years, the period of highest prevalencefor both females and males. The rise in
the gender ratio after the age of men-
arche, the peak near the age of meno¬
pause, and the decline in the genderratio thereafter suggest that hormonalfactors play a role in gender differencesin migraine prevalence. 18_2°However, the
gender ratio of 2.5 even after the age of70 years suggests that hormonal changesat menses and menopause do not fullyaccount for gender differences in mi¬
graine prevalence.After adjusting for other covariates,
blacks exhibited a lower prevalence ofmigraine than whites, particularlyamong males. Because blacks were less
likely to respond to our survey thanwhites, our sample may not be repre¬sentative of blacks in the United States.
Nonetheless, the difference by race isconsistent with a higher platelet level ofthe tyramine conjugating enzyme phe-nolsulfotransferase in blacks than inwhites.21 High levels of phenolsulfotrans-ferase may protect against migraine by
metabolizing suspected dietary triggers,including tyramine.The consistent trend of higher prev¬
alence in lower-income groups is con¬
trary to the commonly held belief thatmigraine is more prevalent among thoseof higher socioeconomic status. This be¬lief may arise from a tendency of mi¬
graine sufferers in higher socioeconomicgroups to consult a physician for care.22·23Although migraine may be more com¬
mon in individuals from higher-incomegroups in clinic-based series, in the gen¬eral population, migraine prevalence in¬creases as income decreases.
In the present study, the higher prev¬alence in lower-income groups may beexplained by a higher incidence of new
cases or a longer duration of time over
which cases suffer from attacks. Causaland medical care factors may governboth the incidence and duration of thiscondition. Diet, stress, and other fac¬tors associated with low income mayprecipitate migraine attacks. Alterna¬
tively, access to good health care maydecrease the duration of the illness andtherefore the prevalence among higher-income groups. In some individuals mi¬
graine may cause low income. That is,headache-related disability may seri¬ously disrupt function at work or school.The phenomenon of "downward" socio-economic drift has been described inother disabling conditions.24·25 In turn,occupational and social disruption mayexacerbate the migraine condition, cre¬
ating a downward spiral.Differences in reporting symptoms
may also account for the observed trendby income, resulting in misclassificationof a greater proportion of severe head¬ache sufferers as migraineurs in the low¬est income groups. While individuals
from lower-income households had a
higher overall prevalence of severe head¬ache, migraineurs accounted for a
smaller percentage of all severe head¬ache sufferers compared with respon¬dents from higher-income households.This finding is contrary to what wouldbe expected if severe headache is more
likely to be misclassified as migraine inlower-income groups.
The nonresponse rate of 37.6% is a
limitation of this survey. Migraineursmay have been more likely to respond,affecting both the overall prevalence es¬
timate of migraine and, possibly, dif-
at Albert Einstein College of Medicine on December 29, 2009www.jama.comDownloaded from

7/23/2019 Stewart - Prevalence of Migraine HA in the US -JAMA 1992.pdf
http://slidepdf.com/reader/full/stewart-prevalence-of-migraine-ha-in-the-us-jama-1992pdf 6/6
ferences by sociodemographic factors.While respondents and nonrespondentshad similar sociodemographic profilesby gender, income, urban vs rural liv¬
ing, and region of the country, differ¬ences were found by age and race.
Younger respondents are more mobileand are typically underrepresented in
population surveys compared with older
respondents. If migraineurs were sub¬
stantially more
likely to respond thannonmigraineurs we would have expectedfemales and young people to be over-
represented, patterns not observed inthe present study. These data suggestthat selection bias with regard to mi¬
graine status is not a significant factor.
Instead, more general factors that af¬fect survey response status account fordifferences between respondents andnonrespondents in our survey. However,
even if the prevalence ofmigraine amongnonrespondents were only 50% of theprevalence among respondents, an un¬
likely difference, the prevalence of mi¬graine in our study would be overesti¬mated by only 20%. Finally, it should benoted that our results are generalizableonly to those who self-report as havingsevere headache.
Using our prevalence estimates, we
have made projections of the number ofpeople in the United States who cur¬
rently suffer from migraine headacheand disabling migraine headache. Sex-and age-specific prevalence estimatesfor total migraine and moderate to se¬
vere disabling migraine from our na¬
tional survey were applied to 1989 sex-
and age-specific census estimates of theUS population. Projected estimates in¬dicate that there are 18 million females
and 5.6 million males currently suffer¬
ing from severe migraine headaches. Atotal of 8.7 million females and 2.6 mil¬lion males suffer from moderate to se¬
vere disabling headaches. Of these,3.4 million females and 1.1 million males
experience one or more attacks permonth.
Our study results highlight the needfor increased awareness of migraine on
the part of physicians. Meeting the chal¬lenge of caring for migraine sufferersrequires that physicians actively iden¬tify cases, educate patients to avoid trig¬ger factors, and prescribe medicationwhen appropriate.
This investigation was supported by US PublicHealth Service grants NS19381 and 5-T32 NSO-7153, awarded by the National Institute of Neuro¬logical Disorders and Stroke, Bethesda, Md, andby Glaxo Ine, Research Triangle Park, NC.
References
1. Markush RE, Karp HR, Heyman A, O'FallonWM. Epidemiologic study of migraine symptoms in
young women.
Neurology. 1975;25:430-435.2. Clarke GJR, Waters WE. Headache and mi-graine in a London general practice. In: WatersWE, ed. The Epidemiology ofMigraine. Bracknell\x=req-\Berkshire, England: Boehringer Ingelheim Ltd;1974:14-22.3. Moss G, Waters WE. Headache and migraine ina girl's grammar school. In: Waters WE, ed. TheEpidemiology of Migraine. Bracknell-Berkshire,England: Boehringer Ingelheim Ltd; 1974:49-58.4. Deubner DC. An epidemiologic study of migraineand headache in 10-20 year olds. Headache.1977;17:173-180.5. Schnarch DM, Hunter JE. Migraine incidence inclinical versus nonclinical populations. Psychoso-matics. 1980;21:314-319.6. D'Allesandro R, Benassi G, Lenzi PL, et al.Epidemiology of headache in the Republic o f SanMarino. J Neurol
Neurosurg Psychiatry.1988;51:21-27.7. Chen TC, Leviton A, Edelstein S, EllenbergJH. Migraine and other diseases in women of re-
productive age: the influence of smoking on ob-served associations. Arch Neurol. 1987;44:1024\x=req-\1028.8. Linet MS, Stewart WF, Celentano DD, ZieglerD, Sprecher M. An epidemiologic study of head-ache among adolescents and young adults. JAMA.
1989;261:2211-2216.9. Celentano DD, Linet MS, Stewart WF. Gender
differences in the experience of headache. Soc Sc iMed. 1990;30:1289-1295.10. Ziegler DK. Headache: public health problem.Neurol Clin. 1990;8:781-783.11. Headache Classification Committee of the In-ternational Headache Society. Classification anddiagnostic criteria for headache disorders, cranialneuralgias and facial pain. Cephalalgia. July1988;8(suppl 7):1-96.12. McCullugh P, Nelder JA. Generalized LinearModels. London, England: Chapman & Hall Ltd;1983:142.13. National Data Book and Guide to Sources:Statistical Abstract of the US. 108th ed. Washing-ton, DC: US Bureau of the Census; 1988.14. Breslow NE, Day NE. Statistical Methods inCancer Research, II: T he Design and Analysis ofCohort Studies. 1987;2:152.
15. Andersen
R, Kasper J, Frankel MR, et
al.Total Survey Error: Application to Improve HealthSurveys. San Francisco, Calif:Jossey-Bass Inc Pub-lishers; 1979.16. Celentano D, Stewart WF, Linet MS. The re-
lationship of headache symptoms with severity andduration of attacks. J Clin Epidemiol. 1990:43:983\x=req-\994.17. Bruyn GW. Epidemiology of migraine: a per-sonal view. Headache. 1983;23:127-133.
18. Kappius REK, Goolkasian P. Group and men-
strual phase effect in reported headaches among
college students. Headache. 1987;27:491-494.19. Johannes CG . Hormonal Factors in Relation-ship to Migraine Headache Attacks in YoungWomen. Baltimore, Md: The Johns Hopkins Uni-versity; 1989. Thesis.20. Silberstein SD, Merrian GR. Estrogens, prog-estins, and headache. Neurology. 1991;41:786-793.21. Anderson RJ, Jackson BL. Human platelet phe-nol sulfotransferase: stability of two forms of theenzyme with time and presence of racial difference.Clin Chim Acta. 1984;138:185-196.22. Waters WE. Community studies of the prev-alence of migraine. Headache. 1970;9:178-186.23. Lipton RB, Stewart WF, Celentano DD, ReedML. Diagnosing migraine: a comparison of symp-tom based, physician, and self diagnosis. Celphala-gia. November 1991;11:89-90.24. Liberatos P, Link BG, Kelsey JL . The mea-
surement of social class in epidemiology. Epide-miol Rev. 1988;10:87-121.25. Eaton WW, Day R, Kramer M. The use ofepidemiology for risk factor research in schizophre-nia: an overview in methodologic critique. In : Hand-book ofSchizophrenia-Nosology, Epidemiology andGenetics. New York, NY: Elsevier Science Pub-lishing Co Inc; 1988:169-204.
at Albert Einstein College of Medicine on December 29, 2009www.jama.comDownloaded from