Statins Promote Interleukin-1β–Dependent Adipocyte Insulin ......3T3-L1 adipocyte lipolysis was...
Transcript of Statins Promote Interleukin-1β–Dependent Adipocyte Insulin ......3T3-L1 adipocyte lipolysis was...

Statins Promote Interleukin-1b–Dependent AdipocyteInsulin Resistance Through Lower Prenylation, NotCholesterolBrandyn D. Henriksbo,1 Akhilesh K. Tamrakar,2 Joshua Xu,1 Brittany M. Duggan,1 Joseph F. Cavallari,1
Jobanjit Phulka,1 Martin R. Stampfli,3 Ali A. Ashkar,3 and Jonathan D. Schertzer1
Diabetes 2019;68:1441–1448 | https://doi.org/10.2337/db18-0999
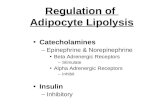
Statins lower cholesterol and adverse cardiovascularoutcomes, but this drug class increases diabetes risk.Statins are generally anti-inflammatory. However, statinscan promote inflammasome-mediated adipose tissueinflammation and insulin resistance through an uniden-tified immune effector. Statins lower mevalonate path-way intermediates beyond cholesterol, but it is unknownwhether lower cholesterol underpins statin-mediatedinsulin resistance. We sought to define the mevalonatepathway metabolites and immune effectors that propa-gate statin-induced adipose insulin resistance. We foundthat LDL cholesterol lowering was dispensable, butstatin-induced lowering of isoprenoids required for pro-tein prenylation triggered NLRP3/caspase-1 inflamma-some activation and interleukin-1b (IL-1b)–dependentinsulin resistance in adipose tissue. Multiple statins im-paired insulin action at the level of Akt/protein kinaseB signaling in mouse adipose tissue. Providing geranyl-geranyl isoprenoids or inhibiting caspase-1 preventedstatin-induced defects in insulin signaling. Atorvastatin(Lipitor) impaired insulin signaling in adipose tissue fromwild-type and IL-182/2 mice, but not IL-1b2/2 mice. Ator-vastatin decreased cell-autonomous insulin-stimulatedlipogenesis but did not alter lipolysis or glucose uptake in3T3-L1 adipocytes. Our results show that statin loweringof prenylation isoprenoids activates caspase-1/IL-1binflammasome responses that impair endocrine controlof adipocyte lipogenesis. This may allow the targeting ofcholesterol-independent statin side effects on adiposelipid handling without compromising the blood lipid/cholesterol-lowering effects of statins.
Statins lower blood cholesterol and reduce the risk ofadverse cardiovascular events, but these drugs can increaseblood glucose and risk of diabetes (1). Statins inhibitHMG-CoA reductase, lowering cholesterol biosynthesisand promoting hepatic cholesterol uptake. Statins havecholesterol-independent actions that depend on HMG-CoA inhibition but are often termed pleiotropic effects.Statin-mediated lowering of mevalonate pathway inter-mediates can alter immunity, independent of cholesterol(2). Inhibition of mevalonate synthesis reduces the iso-prenoid production required for protein prenylation,a posttranslational modification that occurs on hundredsof cellular proteins (3). Statin lowering of specific isopre-noids can limit farnesylation or geranylgeranylation (3).
Statin-mediated lowering of prenylation is generallyassociated with reduced inflammation, including lowerlevels of circulating interleukin-6 (IL-6) and tumor-necrosis factor-a (4). Statins paradoxically increase IL-1band IL-18, and reduced geranylgeranylation is sufficient toincrease IL-1b and IL-18 in monocytes (5). It is also knownthat statins increase caspase-1 activity in immune cells (6).Therefore, statins activate a caspase-1 inflammasome andIL-1b/IL-18 responses despite widespread anti-inflammatoryactions of this drug class. We previously characterized howan inflammasome contributes to the balance of theseimmune effects and endocrine control of metabolism.We found that the nucleotide-binding oligomerization(NOD)-like receptor family, pyrin-domain containing 3(NLRP3) contributes to statin-induced insulin resistancein adipose tissue (7). It was not known which metabolites
1Department of Biochemistry and Biomedical Sciences and Farncombe FamilyDigestive Health Research Institute, McMaster University, Hamilton, Ontario,Canada2Biochemistry Division, CSIR-Central Drug Research Institute, Lucknow, India3Department of Pathology and Molecular Medicine, McMaster ImmunologyResearch Centre, McMaster University, Hamilton, Ontario, Canada
Corresponding author: Jonathan D. Schertzer, [email protected]
Received 15 September 2018 and accepted 16 April 2019
This article contains Supplementary Data online at http://diabetes.diabetesjournals.org/lookup/suppl/doi:10.2337/db18-0999/-/DC1.
© 2019 by the American Diabetes Association. Readers may use this article aslong as the work is properly cited, the use is educational and not for profit, and thework is not altered. More information is available at http://www.diabetesjournals.org/content/license.
Diabetes Volume 68, July 2019 1441
METABOLISM

in the mevalonate pathway promote statin-induced insulinresistance. Statin-mediated inhibition of the cholesterolbiosynthesis pathway can influence immunity by alteringintermediates such as 25-hydroxycholesterol (25-HC),which has been directly linked to NLRP3 inflammasomeactivation in macrophages (8). Statins can actually pre-vent inflammasome assembly and attenuate caspase-1–mediated IL-1b secretion by acutely depleting endoplasmicreticulum–resident cholesterol in macrophages (9). Statinscan also attenuate NLRP3 activation and IL-1b releasewhen lipopolysaccharide (LPS)-primed monocytes are ac-tivated with cholesterol crystals, but the same data showthat statins alone increase active caspase-1 and IL-1bsecretion (10). Here, we tested whether prenylation orcholesterol underpinned statin-induced adipose insulinresistance.
It is unknown which inflammasome effector propagatesadipose insulin resistance as a result of statins. NLRP3/caspase-1 inflammasome regulation of IL-1b promotes in-sulin resistance in adipocytes and dysglycemia in rodents(11). Markers of NLRP3 inflammasome activation arehigher in patients with type 2 diabetes, and IL-1 receptorantagonism can improve glycemia (12,13). IL-1b is a goodcandidate to test for statin-mediated insulin resistance,but caspase-1 targets beyond IL-1b or IL-18 can linkNLRP3 inflammasome responses to metabolic defects ininsulin-responsive tissues (14,15).
We show that statin-induced adipocyte insulin resis-tance occurs through IL-1b and the lowering of isopre-noids required for prenylation, independent of changes incellular cholesterol or LDL-mediated pathways to insulinresistance. Statins cause cell-autonomous impairment ininsulin-stimulated adipocyte lipogenesis rather than glu-cose uptake or inhibition of lipolysis.
RESEARCH DESIGN AND METHODS
The McMaster University animal ethics review boardapproved all procedures. Male C57BL/6J mice werefrom The Jackson Laboratory (#000664). IL-1b2/2
mice were from Yoichiro Iwakura (University of Tokyo,Tokyo, Japan) and bred in-house. IL-182/2 mice werefrom A.A.A. Explants from mouse gonadal adiposedepots were exposed to statins, zoledronate, cholesterolderivatives, geranylgeranyl pyrophosphate (GGPP) orz-YVAD (18 h), LPS (final 4 h), or insulin (final10 min). Lysates were immunoblotted (16), and IL-1bwas quantified by ELISA (7). Adipocytes were separatedfrom the stromal vascular fraction (SVF) (17). 3T3-L1adipocytes and bone marrow–derived macrophages(BMDMs) were immunoblotted or analyzed by quantita-tive PCR (18).
3T3-L1 adipocyte lipolysis was determined as previ-ously described (18). Lipogenesis was measured in lipidsfrom adipose explants using [14C]U-glucose (2 mCi/mL)and 3T3-L1 adipocytes (1 mCi/mL)6 insulin (0.3 nmol/L)for the final 2 h (explants) or 1 h (3T3-L1). Glucose uptakewas measured using [3H]-2-deoxyglucose (16).
Each experimental replicate represents a single adiposeexplant or 3T3-L1 culture well. Statistical significance wasdetermined by ANOVA with Tukey post hoc test. Unpairedt tests were used to compare two conditions.
RESULTS
Mevalonate Pathway Inhibition Lowers Insulin-Stimulated Lipogenesis in Adipose TissueWe previously showed that NLRP3 was required for flu-vastatin to impair insulin-stimulated Ser473 phosphoryla-tion of Akt/phosphokinase B (PKB) in explanted mouseadipose tissue. Adipose tissue was primed with a dose ofLPS (2mg/mL, 4 h) that does not alter insulin signaling butallows investigation of inflammasome responses (7) (Fig.1A). The bisphosphonate zoledronate (1 and 5 mmol/L),which inhibits the mevalonate pathway distal to HMG-CoAreductase, lowered insulin-stimulated Ser473 phosphoryla-tion of Akt/PKB in LPS-primed explanted adipose tissue(Fig. 1A). Multiple statins impaired insulin signaling inadipose tissue, indicating a drug class effect on insulinsensitivity. We found that 1 mmol/L atorvastatin or1 mmol/L pravastatin (Fig. 1B and C) but 0.1 mmol/Lcerivastatin decreased insulin-stimulated Ser473 phosphor-ylation of Akt/PKB in LPS-primed adipose explants (Fig.1D). Atorvastatin impaired insulin-stimulated lipogenesisin LPS-primed adipose explants (Fig. 1E). Compared withadipose explants from lean mice, explants from high-fat–fed obese mice had impaired insulin signaling where LPS,but not statin exposure, further decreased insulin action(Fig. 1F). These results show that inhibiting the mevalo-nate pathway at multiple steps or with multiple statinsimpaired insulin signaling wherein one functional outcomeis lower insulin-stimulated adipose tissue lipogenesis asa result of statin exposure.
Statin Lowering of Prenylation Inhibits Insulin Signalingin Adipose TissueWe next tested whether lowering cholesterol metabolitesor isoprenoids underpinned statin-mediated insulin re-sistance. We found that supplementation with LDL cho-lesterol (0.01 and 1 mg/mL) or free cholesterol (1 and20 mmol/L) did not cause a further reduction of (and didnot restore) statin-mediated lowering of Ser473 phosphor-ylation of Akt/PKB in LPS-primed adipose explants (Fig.2A and B). LDL cholesterol treatment alone (1 mg/mL)lowered insulin signaling independently of LPS priming orstatin treatment (Fig. 2A). Lower 25-HC can lead toactivation of caspase-1 and increase IL-1b in macro-phages (8). However, we found that supplementationof LPS-primed adipose explants with 25-HC (1 and20 mmol/L) did not cause a further reduction of (anddid not restore) impaired insulin signaling as a result ofatorvastatin (Fig. 2C). In contrast to all experiments usingcholesterol derivatives, supplementation of LPS-primedadipose explants with the isoprenoid GGPP at 50 mmol/L(but not 5 mmol/L) restored atorvastatin-induced suppres-sion of insulin-stimulated phosphorylation of Akt/PKB at
1442 Statins Impair Lipogenesis Through Prenylation Diabetes Volume 68, July 2019

Ser473 and Thr308 (Fig. 2D and E). Importantly, GGPPrestored insulin action as a result of statin exposure butnot LDL cholesterol (1 mg/mL) (Fig. 2A). These data showthat a statin-mediated reduction in a geranylgeranyl iso-prenoid is required for impaired insulin signaling, whichoccurs in-dependently of cholesterol or LDL-mediatedeffects on insulin action.
IL-1b Is Required for Statin-Induced Insulin ResistanceWe next tested whether caspase-1 regulation of IL-1b orIL-18 was involved in impaired insulin action in adiposetissue (Fig. 3A). Inhibition of caspase-1 with 1 or 10mmol/Lz-YVAD restored atorvastatin-mediated lowering of Ser473
phosphorylation of Akt/PKB in LPS-primed adiposeexplants stimulated with insulin (Fig. 3B). Atorvastatin,
Figure 1—Mevalonate pathway inhibition impairs insulin action in adipose tissue. Adipose tissue explants were from wild-type C57BL/6Jmice and treated with LPS (2 mg/mL for the final 4 h) where indicated. A–D: Representative immunoblots (top) and quantification (bottom) ofphosphorylated Akt (pAkt)/PKB (Ser473) from basal (i.e., no insulin) and insulin-stimulated (0.3 nmol/L) conditions after treatment of adiposetissue explants with vehicle (control) or zoledronate (1 or 5 mmol/L), atorvastatin (1 mmol/L), pravastatin (1 mmol/L), or cerivastatin (0.1 or1 mmol/L) for 18 h. E: Fold-change insulin-stimulated lipogenesis in adipose tissue explants treated with vehicle (control) or atorvastatin(1 mmol/L, 18 h) and LPS (2 mg/mL, final 4 h). F: Representative immunoblot (top) and quantification (bottom) of pAkt/PKB (Ser473) from basal(i.e., no insulin) and insulin-stimulated (0.3 nmol/L) conditions after treatment of adipose tissue explants from control diet–fed lean mice andhigh-fat–fed obese mice treated with atorvastatin (1 mmol/L, 18 h) and LPS (2 mg/mL, final 4 h). Each value from a given explant and mean6SEM is shown. The number above each experimental condition indicates the number of adipose tissue explants used in quantification.#Significantly different from control; *significantly different from lean control. Ator, atorvastatin; AU, arbitrary unit.
diabetes.diabetesjournals.org Henriksbo and Associates 1443

Figure 2—Isoprenoids, not cholesterol, mitigate statin-induced insulin resistance in adipose tissue. Adipose tissue explants were from wild-type C57BL/6J mice and treated with LPS (2 mg/mL for the final 4 h) where indicated. A–C: Representative immunoblots (top) andquantification (bottom) of basal (i.e., no insulin) and insulin-mediated phosphorylated Akt (pAkt) (Ser473) after treatment of adipose tissueexplants with vehicle (control) or atorvastatin (1 mmol/L, 18 h) with and without LDL cholesterol, free cholesterol, or 25-HC at the doseindicated. A: LDL cholesterol–treated explants were also treated in combination with GGPP (50 mmol/L, 22 h). D and E: Representativeimmunoblots (top) and quantification (bottom) of basal (i.e., no insulin) and insulin-mediated pAkt at Ser473 and Thr308 after treatment ofadipose tissue explants with atorvastatin (1 mmol/L, 18 h) plus supplementation with and without GGPP at the dose indicated. Each valuefrom a given explant and mean 6 SEM is shown. The number above each experimental condition indicates the number of adipose tissueexplants used in quantification. #Significantly different from control. Ator, atorvastatin; AU, arbitrary unit.
1444 Statins Impair Lipogenesis Through Prenylation Diabetes Volume 68, July 2019

Figure 3—Statins impair adipose insulin action through IL-1b. A: Schematic of the relationship among statins, prenylation, and theNLRP3/caspase-1 effector that could promote insulin resistance. Adipose tissue explants were treated with LPS (2 mg/mL for the final 4 h)where indicated. Explants derived from wild-type C57BL/6J or IL-1b2/2 or IL-182/2 mice as indicated. B: Representative immunoblots (top)and quantification (bottom) of basal (i.e., no insulin) and insulin-mediated phosphorylated Akt (pAkt) (Ser473) after treatment of adipose tissueexplants with vehicle (control) or atorvastatin (1 mmol/L) supplemented with or without the caspase-1 inhibitor z-YVAD at the dose indicated.C and D: Representative immunoblots (top) and quantification (bottom) of basal (i.e., no insulin) and insulin-mediated pAkt (Ser473) aftertreatment with either atorvastatin (1 mmol/L) or pravastatin (1 mmol/L) or cerivastatin (0.1 mmol/L) in adipose tissue explants derived fromIL-1b2/2 mice. E: Representative immunoblots (top) and quantification (bottom) of basal (i.e., no insulin) and insulin-mediated pAkt (Ser473)after treatment with atorvastatin (1 mmol/L) in adipose tissue explants derived from IL-182/2 mice. Each value from a given explant andmean 6 SEM is shown. The number above each experimental condition indicates the number of adipose tissue explants used inquantification. #Significantly different from control. ASC, apoptosis-associated speck-like protein containing CARD; Ator, atorvastatin;AU, arbitrary unit; Ceriv, cerivastatin; Prav, pravastatin.
diabetes.diabetesjournals.org Henriksbo and Associates 1445

Figure 4—Statin-mediated lowering of prenylation impairs adipocyte-autonomous lipid handling. A and B: Quantification of IL-1b by ELISAand transcript levels of NLRP3 and pyrin in adipocytes vs. the SVF from adipose tissue explants treated with atorvastatin (1 mmol/L, 18 h)and LPS (2 mg/mL for the final 4 h). C: Transcript levels of NLRP3 and pyrin in macrophages (BMDM), white adipose tissue (WAT), and3T3-L1 adipocytes treated with atorvastatin (10 mmol/L, 18 h), fluvastatin (10 mmol/L, 18 h), or LPS (0.2 or 2 mg/mL, 4 h). D: Cholesterolconcentration of 3T3-L1 adipocytes after treatment with atorvastatin (10 mmol/L) for 1, 3, and 22 h. E and F: Representativeimmunoblots (top) and quantification (bottom) of basal (i.e., no insulin) and insulin-mediated phosphorylated Akt (pAkt)/PKB(Ser473) after treatment of 3T3-L1 adipocytes with atorvastatin (10 mmol/L), LPS (2 mg/mL), and/or GGOH (25 mmol/L, 18 h) or farnesol(FOH) (25 mmol/L, 18 h). G: 3T3-L1 adipocytes were treated with atorvastatin (10 mmol/L, 18 h) and LPS (2 mg/mL, 4 h) with or withoutisoproterenol (Iso) (10 nmol/L, 5 h), and lipolysis was determined by glycerol release rate. H: 3T3-L1 adipocytes were exposed to
1446 Statins Impair Lipogenesis Through Prenylation Diabetes Volume 68, July 2019

pravastatin, or cerivastatin did not lower Ser473 phosphor-ylation of Akt/PKB in LPS-primed adipose explants derivedfrom IL-1b2/2 mice (Fig. 3C and D). Similar to wild-typemice, atorvastatin lowered Ser473 phosphorylation ofAkt/PKB in LPS-primed adipose explants derived fromIL-182/2 mice (Fig. 3E). Overall, these data show that statinsrequire caspase-1 and IL-1b to impair insulin signaling inadipose tissue.
Statin Lowering of Prenylation Impairs Adipocyte-Autonomous LipogenesisWe next sought to determine the contributions of adipo-cytes versus the immune cell-enriched SVF. When adiposetissue explants were LPS primed and treated with ator-vastatin, we found that both adipocytes and SVF hadhigher IL-1b (Fig. 4A). IL-1b was more abundant in theSVF compared with adipocytes (Fig. 4A). Previous researchin BMDM reported that statin-mediated lowering of iso-prenoids can also activate the pyrin inflammasome topromote IL-1b processing (19). The requirement for pyrinin macrophages contradicts our previous report whereinstatins engaged the NLRP3 inflammasome in adiposetissue (7). We assessed whether cell type was the un-derlying factor for this discrepancy. We found that tran-script levels of NLRP3 were increased with LPS treatmentin the adipocyte and SVF, although no increase in tran-scripts of pyrin could be detected (Fig. 4B). We found thattranscript levels of pyrin were detectable and augmentedby LPS priming in BMDMs and adipose tissue (containingthe SVF), but pyrin transcripts were not detectable in 3T3-L1 adipocytes (Fig. 4C). NLRP3 transcripts were present inBMDM, adipose tissue, and 3T3-L1 adipocytes, and NLRP3transcript levels were augmented by LPS priming in allthree cell/tissue types (Fig. 4C). This prompted us todetermine whether a cell-autonomous response under-pinned NLRP3 statin-induced adipocyte insulin resistance.
Cholesterol concentration in 3T3-L1 adipocytes did notchange during treatment with atorvastatin (Fig. 4D).Atorvastatin lowered insulin-stimulated Ser473 phosphor-ylation of Akt/PKB in 3T3-L1 adipocytes, and supple-mentation with the isoprenoid geranylgeraniol (GGOH)(25 mmol/L) restored this aspect of insulin signaling(Fig. 4E). Supplementation with farnesol did not restoreatorvastatin-mediated lowering of insulin-stimulated Ser473
phosphorylation of Akt/PKB in 3T3-L1 adipocytes (Fig.4F). We next sought to determine the functional conse-quences of these adipocyte-autonomous statin-mediatedresponses. Atorvastatin did not alter lipolysis (with orwithout isoproterenol) in 3T3-L1 adipocytes (Fig. 4G).
However, insulin-stimulated lipogenesis was decreasedby atorvastatin, an effect that was not observed when3T3-L1 adipocytes were supplemented with 25 mmol/LGGOH (Fig. 4H). Insulin-stimulated glucose uptake into3T3-L1 adipocytes was not changed by atorvastatin orGGOH (Fig. 4I). Overall, these data show that atorvastatinlowers insulin-stimulated adipocyte-autonomous lipogen-esis by lowering isoprenoids required for protein preny-lation but not farnesylation.
DISCUSSION
Statins lower cholesterol, risk of cardiovascular disease,and all-cause mortality, but this drug class can increaseblood glucose (1). The mechanisms linking statins andincreased risk of diabetes should be clarified becausewarning labels now include an increased risk of bloodglucose and diabetes (Health Canada, RA-16949). It isnot known whether statin-induced changes in glycemiaare related to cholesterol lowering. We sought to deter-mine whether statins impaired insulin action by loweringcholesterol or another mevalonate pathway metabolite.We found that LDL cholesterol and 25-HC were dispens-able for statin-mediated insulin resistance in adiposetissue. Cell type is a key determinant of how statins engagespecific inflammasomes. Others have shown that statinscan attenuate ligand-induced NLRP3 or pyrin inflamma-some responses in macrophages or monocytes (9,10,19).We show that isoprenoids required for protein prenylationwere sufficient to prevent statin-mediated defects in in-sulin signaling in adipocytes. This is important becausecoadministration of statin and isoprenoids may mitigateadipose tissue side effects but not interfere with lipid/cholesterol-lowering benefits of statins. Determination ofthe prenylated proteins that alter inflammasome activa-tion and insulin resistance is warranted. Targeting specificprenylation events may be superior to widespread reversalof isoprenoid lowering that could mitigate longevity andcardiac benefits of statins shown in Drosophila (20).
We show that statins impaired insulin-stimulated lipo-genesis in an adipocyte-autonomous manner, which wasprevented by supplementing isoprenoids required for pre-nylation. This is important because impaired insulin sig-naling does not always correlate with impaired insulinaction. Given that statins did not impair glucose uptake inadipocytes, our results are consistent with statins impair-ing selective and heterogeneous effects of insulin resis-tance that manifest in lipid metabolism (21).
We show that statin-induced insulin resistance is a drugclass effect. Cerivastatin was removed from the market
atorvastatin (10 mmol/L) supplemented with or without GGOH (25 mmol/L) for 18 h followed by the addition of [14C]-U-glucose(1 mCi/mL) 6 insulin (0.3 nmol/L) for 1 h, and lipogenesis was quantified using the radiolabeled lipid pool. I: Glucose uptake wasdetermined in 3T3-L1 adipocytes that were exposed to atorvastatin (10 mmol/L) and/or GGOH (25 mmol/L) for 18 h before the addition ofinsulin (0.3 nmol/L, 20 min) and [3H]-2-deoxyglucose (0.5 mCi/mL) uptake for 5 min. Data are mean 6 SEM. The number above eachexperimental condition indicates the number of adipose tissue explants or independent 3T3-L1 adipocyte cultures used in thequantification. n $ 5 replicates if not otherwise indicated. #Significantly different from control. Ator, atorvastatin; AU, arbitrary unit;DPM, disintegrations per minute; ND, not detected.
diabetes.diabetesjournals.org Henriksbo and Associates 1447

because of side effects. Our results show that cerivastatinwas the most potent statin in promoting adipose insulinresistance (and the most potent activator of IL-1b releasefrom BMDMs [data not shown]). IL-18 was dispensable forstatin-induced adipose insulin resistance. IL-1b was thekey mediator of statin-induced adipocyte insulin resis-tance, which ultimately impaired lipogenesis. IL-1b alonelowers insulin-stimulated lipogenesis in rodent and humanadipocytes (22). IL-1 receptor antagonism can improveglycemia, but the design of clinical trials using IL-1binhibition, such as the Canakinumab Anti-InflammatoryThrombosis Outcome Study (CANTOS) trial, does notnecessarily always reveal reduced diabetes incidence(13,23). Statins are pervasive in these clinical trials andshould be considered as a confounding variable. It is notclear why patients with familial hypercholesteremia onlifelong statins can have a low prevalence of type 2 diabetesas opposed to patients who are obese or with metabolicdisease in whom stains can increase the risk of type2 diabetes (24). Our results suggest that impaired adipo-cyte lipogenesis underpins the relationship between lipidsand glucose during statin treatment because higher bloodtriglycerides are a known risk factor predicting statin-induced diabetes (25). Our results appear relevant to statinintolerance and diminishing returns of increased statindose on triglyceride/lipid lowering. Statin engagement ofan NLRP3/caspase-1/IL-1b response may limit the effec-tiveness of statins to lower blood triglycerides independentof cholesterol lowering. Targeting NLRP3/caspase-1/IL-1bmay allow enhanced blood lipid lowering at a given statindose and/or mitigate side effects at a statin dose thatachieves lipid-lowering goals.
Funding. This work was supported by grants to J.D.S. from the CanadianInstitutes of Health Research (FDN-154295) and Hamilton Health Sciences NewInvestigator fund (NIF-16401). J.D.S. holds a Canada Research Chair in MetabolicInflammation.Duality of Interest. No potential conflicts of interest relevant to this articlewere reported.Author Contributions. B.D.H. researched the data, contributed to thediscussion, and edited the manuscript. B.D.H. and J.D.S. derived the hypothesisand wrote the manuscript. A.K.T., J.X., B.M.D., J.F.C., and J.P. researched thedata. M.R.S. and A.A.A. contributed to the discussion and provided mice. J.D.S. isthe guarantor of this work and, as such, had full access to all the data in the studyand takes responsibility for the integrity of the data and the accuracy of the dataanalysis.
References1. Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes:a collaborative meta-analysis of randomised statin trials. Lancet 2010;375:735–7422. Greenwood J, Steinman L, Zamvil SS. Statin therapy and autoimmunedisease: from protein prenylation to immunomodulation. Nat Rev Immunol 2006;6:358–3703. Sinensky M. Recent advances in the study of prenylated proteins. BiochimBiophys Acta 2000;1484:93–106
4. Rosenson RS, Tangney CC, Casey LC. Inhibition of proinflammatory cytokineproduction by pravastatin. Lancet 1999;353:983–9845. Mandey SHL, Kuijk LM, Frenkel J, Waterham HR. A role for geranylger-anylation in interleukin-1beta secretion. Arthritis Rheum 2006;54:3690–36956. Montero MT, Hernández O, Suárez Y, et al. Hydroxymethylglutaryl-coenzymeA reductase inhibition stimulates caspase-1 activity and Th1-cytokine release inperipheral blood mononuclear cells. Atherosclerosis 2000;153:303–3137. Henriksbo BD, Lau TC, Cavallari JF, et al. Fluvastatin causes NLRP3 in-flammasome-mediated adipose insulin resistance. Diabetes 2014;63:3742–37478. Reboldi A, Dang EV, McDonald JG, Liang G, Russell DW, Cyster JG. In-flammation. 25-Hydroxycholesterol suppresses interleukin-1-driven inflammationdownstream of type I interferon. Science 2014;345:679–6849. de la Roche M, Hamilton C, Mortensen R, Jeyaprakash AA, Ghosh S, AnandPK. Trafficking of cholesterol to the ER is required for NLRP3 inflammasomeactivation. J Cell Biol 2018;217:3560–357610. Boland AJ, Gangadharan N, Kavanagh P, et al. Simvastatin suppressesinterleukin Ib release in human peripheral blood mononuclear cells stimulatedwith cholesterol crystals. J Cardiovasc Pharmacol Ther 2018;23:509–51711. Vandanmagsar B, Youm YH, Ravussin A, et al. The NLRP3 inflammasomeinstigates obesity-induced inflammation and insulin resistance. Nat Med 2011;17:179–18812. Lee H-M, Kim JJ, Kim HJ, Shong M, Ku BJ, Jo EK. Upregulated NLRP3inflammasome activation in patients with type 2 diabetes. Diabetes 2013;62:194–20413. Larsen CM, Faulenbach M, Vaag A, et al. Interleukin-1-receptor antagonist intype 2 diabetes mellitus. N Engl J Med 2007;356:1517–152614. Murphy AJ, Kraakman MJ, Kammoun HL, et al. IL-18 production from theNLRP1 inflammasome prevents obesity and metabolic syndrome. Cell Metab2016;23:155–16415. McBride MJ, Foley KP, D’Souza DM, et al. The NLRP3 inflammasomecontributes to sarcopenia and lower muscle glycolytic potential in old mice. Am JPhysiol Endocrinol Metab 2017;313:E222–E23216. Schertzer JD, Tamrakar AK, Magalhães JG, et al. NOD1 activators link innateimmunity to insulin resistance. Diabetes 2011;60:2206–221517. Cavallari JF, Fullerton MD, Duggan BM, et al. Muramyl dipeptide-basedpostbiotics mitigate obesity-induced insulin resistance via IRF4. Cell Metab 2017;25:1063–1074.e318. Duggan BM, Foley KP, Henriksbo BD, Cavallari JF, Tamrakar AK, SchertzerJD. Tyrosine kinase inhibitors of Ripk2 attenuate bacterial cell wall-mediatedlipolysis, inflammation and dysglycemia. Sci Rep 2017;7:157819. Akula MK, Shi M, Jiang Z, et al. Control of the innate immune response by themevalonate pathway. Nat Immunol 2016;17:922–92920. Spindler SR, Li R, Dhahbi JM, et al. Statin treatment increases lifespan andimproves cardiac health in Drosophila by decreasing specific protein prenylation.PLoS One 2012;7:e3958121. Tonks KT, Ng Y, Miller S, et al. Impaired Akt phosphorylation in insulin-resistant human muscle is accompanied by selective and heterogeneousdownstream defects. Diabetologia 2013;56:875–88522. Lagathu C, Yvan-Charvet L, Bastard JP, et al. Long-term treatment withinterleukin-1b induces insulin resistance in murine and human adipocytes. Di-abetologia 2006;49:2162–217323. Everett BM, Donath MY, Pradhan AD, et al. Anti-inflammatory therapy withcanakinumab for the prevention and management of diabetes. J Am Coll Cardiol2018;71:2392–240124. Besseling J, Kastelein JJP, Defesche JC, Hutten BA, Hovingh GK. Associationbetween familial hypercholesterolemia and prevalence of type 2 diabetes mellitus.JAMA 2015;313:1029–103625. Sung K-C, Reaven G. Fasting plasma triglyceride concentration: a possibleapproach to identify increased risk of statin-induced type 2 diabetes. Diab Vasc DisRes 2015;12:373–376
1448 Statins Impair Lipogenesis Through Prenylation Diabetes Volume 68, July 2019