Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25...
Transcript of Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25...
![Page 1: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/1.jpg)
Alcohol Misuse in Police Custody, 1.02 1st June 2016 Page 1 of 25
Standard Operating Procedure
Chest Pain and Cardiac Care in Police Custody
![Page 2: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/2.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25
For Completion by SOP Lead
Name of Responsible Committee , [Insert Date Ratified]
Issue Date Insert Date Issued (Change Version, Footers & Watermark)
Implementation Date
Review date Insert Agreed Review Date
Electronic location Insert G Drive Location
G4S is committed to ensuring that, as far as is reasonably practicable, the way we provide services to our detainees and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This SOP has been assessed accordingly
For Completion by SOP Author
Reference Number Reference xxxxx /SOP__ [Number provided by SOP Controller on Registration of SOP]
Version Draft – Version 1.01 [Draft version will be changed to Issued Version by the SOP Controller on approval]
Document Author(s) Stephen Dolphin
Document Reviewer(s)
![Page 3: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/3.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 3 of 25
CONTENTS 1. INTRODUCTION ........................................................................................................................................... 4
1.1 Chest pain ............................................................................................................................................ 42. PURPOSE ..................................................................................................................................................... 43. SCOPE .......................................................................................................................................................... 44. DUTIES AND RESPONSIBILITIES ............................................................................................................... 45. PROCESS ..................................................................................................................................................... 4
5.1 Incidence of chest pain ........................................................................................................................ 45.2 Causes of chest pain ............................................................................................................................ 55.3 Recommendations ............................................................................................................................... 7
6. Acute Coronary Syndrome (including myocardial infarction and unstable angina). ...................................... 86.1 Common signs and symptoms ............................................................................................................. 86.2 Treatment ............................................................................................................................................. 8
7. Stable Angina ................................................................................................................................................ 97.1 Common signs and symptoms: ............................................................................................................ 97.2 Treatment ............................................................................................................................................. 9
8. Pericarditis ................................................................................................................................................... 108.1 Common signs and symptoms ........................................................................................................... 108.2 Treatment ........................................................................................................................................... 10
9. Abdominal Aortic Aneurysm (Triple A) ......................................................................................................... 119.1 Common signs and symptoms ........................................................................................................... 119.2 Treatment ........................................................................................................................................... 11
10. Pulmonary embolism ................................................................................................................................... 1210.1 Common signs and symptoms ........................................................................................................... 1210.2 Treatment ........................................................................................................................................... 12
11. Pneumothorax ............................................................................................................................................. 1311.1 Common signs and symptoms ........................................................................................................... 1311.2 Treatment ........................................................................................................................................... 13
12. Musculo-skeletal .......................................................................................................................................... 1412.1 Common signs and symptoms ........................................................................................................... 1412.2 Treatment ........................................................................................................................................... 14
13. Gastric reflux ................................................................................................................................................ 1513.2 Common signs and symptoms ........................................................................................................... 1513.3 Treatment ........................................................................................................................................... 15
14. Hyperventilation ........................................................................................................................................... 1614.1 Common signs and symptoms ........................................................................................................... 1614.2 Treatment ........................................................................................................................................... 16
15. Drug use ...................................................................................................................................................... 1716. Cardiac Arrest .............................................................................................................................................. 18
16.1 Resuscitation ...................................................................................................................................... 1816.2 Stopping resuscitation ........................................................................................................................ 22
17. Medication Arrangements ............................................................................................................................ 2318. Reviews ....................................................................................................................................................... 2319. Advice to Detainee ....................................................................................................................................... 2320. Advice to Custody Staff ............................................................................................................................... 2321. TRAINING REQUIREMENTS ...................................................................................................................... 2422. REFERENCES AND ASSOCIATED DOCUMENTATION ........................................................................... 2423. VERSION HISTORY LOG ........................................................................................................................... 2424. CONFIRMATION OF SOP TRAINING RECORD ........................................................................................ 25
![Page 4: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/4.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 4 of 25
1. INTRODUCTION
1.1 Chest pain Chest pain is a common emergency in Police Custody. Myocardial infarction is, however, a rare event. Most chest pain comes from more mundane causes, such as anxiety and panic attacks and injury to the chest.
2. PURPOSE • To ensure full clinical and risk assessment of the physical and emotional needs of
detainees with chest pain and/or cardiac conditions. • • To enable the FME/HCP to provide clinically appropriate medical care, treatment,
education and psychological support to the detainee whilst detained in Police custody, and afterwards where appropriate, in accordance with NICE, HCPC and NMC guidelines and standards.
3. SCOPE
This SOP applies to all Health Care Professionals working in Police Custody.
4. DUTIES AND RESPONSIBILITIES All Healthcare Professionals undertaking medical assessments of detainees have a duty to take into account the effects of chest pain on the detainee. It is the responsibility of all Healthcare Professionals to advise Custody Staff of the possible effects of chest pain on the detainee.
5. PROCESS
5.1 Incidence of chest pain Chest pain is a common symptom found in detainees in Police custody and can be challenging to deal with due to the anxieties and preconceptions of, not only the detainee, but also the custody staff and sometimes the clinician. Chest pain has many causes. A recent survey from an A & E Department showed presentations of chest pain were finally diagnosed as below: Myocardial Infarction 20% Gastric Reflux 19% Ischaemic Heart Disease 15% No Diagnosis 10% Pulmonary 7% Musculo-skeletal 8% Ulcer/Gastritis 3% Malingering 2% Pericarditis 1% These figures were obtained from the general population presenting at A&E, including all ages and states of health. In the custody situation the typical detainees do not often include the very elderly and chronically sick detainees, but do often include those who are involved in violence and trauma, drug and alcohol use, hypertension, diabetes, and mental health problems, all of which can give rise to chest pain in various forms, so the incidence of MI and IHD will usually be less and the incidence of other causes will usually be more. However, this does not say that the detainees in custody will not have chest pain from a cardiac or pulmonary cause. It does happen, and if you make assumptions and do not carry out a full assessment, the consequences can be serious, both for the detainee and the clinician’s registration.
![Page 5: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/5.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 5 of 25
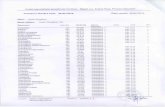
5.2 Causes of chest pain It is very easy to jump to conclusions as to the cause of chest pain, but careful examination and history-taking will usually differentiate between the serious and the not-so-serious and will guide the clinician towards the correct priorities and treatment for the optimum care of the detainee. The detainee must, first of all, be taken seriously. If they tell you of certain symptoms that suggest a relatively benign cause for the pain, it is important to keep an open mind and still ask the questions that will eliminate the serious causes. Potentially serious pathology may present with trivial symptoms and vice versa. For instance, a pneumothorax may present with just a sharp pain to one side of the chest, which could easily be dismissed as musculo-skeletal pain. Similarly, indigestion may mimic a minor myocardial infarction. Without proper investigation and treatment, serious repercussions could follow. Chest pains should not be treated as life-threatening “just in case”. Take a history and examine the detainee. Only then should you decide on the appropriate treatment.The need for speed can engender blinkered thinking, which must be avoided. If there is still doubt about the nature of the problem, first do no harm, and treat the signs and symptoms that you find. Inappropriate treatment can cause problems either way and the consequences of a wrong diagnosis can be devastating both for the detainee and for the clinician. A rational approach to the diagnosis of the cause of chest pain requires joined-up thinking on the part of the clinician, leading to a successful outcome to the call. The next page shows a table of the typical signs and symptoms of different causes of chest pain. It should be noted that the signs and symptoms shown are only typically representative of different causes of chest pain and are therefore only a guide. Each detainee must be individually examined to ensure correct diagnosis and treatment.
![Page 6: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/6.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 6 of 25
![Page 7: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/7.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 7 of 25
5.3 Recommendations These recommendations do not take the place of clinical judgment. Always examine your detainee thoroughly. Check if the chest pain may be cardiac. Consider:
• history of the pain • any cardiovascular risk factors • history of ischaemic heart disease and any previous treatment • previous investigations for chest pain
Check if any of the following symptoms of ischaemia are present. These may indicate an ACS:
• Pain in the chest and/or other areas (for example, the arms, back or jaw) lasting longer than 15 minutes.
• Chest pain with nausea and vomiting, marked sweating or breathlessness (or a combination of these), or with haemodynamic instability.
• New onset chest pain, or abrupt deterioration in stable angina, with recurrent pain occurring frequently with little or no exertion and often lasting longer than 15 minutes.
Central chest pain may not be the main symptom.
• Do not use response to glyceryl trinitrate (GTN) to make a diagnosis of ACS. • Do not assess symptoms of an ACS differently in men and women or among different
ethnic groups. • If the chest pain is non-cardiac, explain this to the person and investigate further.
Always examine the detainee thoroughly:
• Presenting complaint • History of presenting complaint • Past medical history • Drug history • Systems review –
Cardiovascular System, Respiratory System, Abdomen, and Central Nervous System. • Remember - Inspection, Palpation, Percussion, Auscultation.
![Page 8: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/8.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 8 of 25
6. Acute Coronary Syndrome (including myocardial infarction and unstable angina).
6.1 Common signs and symptoms 6.1.1 Pain
Pain begins rapidly but gradually, increasing steadily over a minute or two, usually beginning in the chest, behind the sternum. It is often described as a crushing, gripping or heavy pain, as though a great weight is on the chest or a tight band around the chest. The detainee will often clench their fist to their chest when describing the pain (Levine’s sign). The pain may be referred to other areas, such as the arms (this is due to the nerves for the arms coming from the same root as the heart during foetal development in the uterus). The pain may also radiate into the back and jaw. Pain in the referred areas without central chest pain is unlikely to be cardiac in origin, but not unknown. The pain of acute myocardial infarction classically lasts for more than 30 minutes, whereas angina pain usually subsides after five to ten minutes of rest. However, this is highly variable, with up to 20% of detainees, particularly the elderly, having no pain at all. Commonly, the pain is very severe, with the detainee sometimes fearing imminent death. The pain from angina is usually reduced by GTN, but the pain from infarction is not, but this can vary. Pain is perhaps the most important symptom of myocardial infarction as it causes the detainee to call for help.
6.1.2 Dyspnoea Reduction of blood supply to the lungs may cause dyspnoea, by simple lack of perfusion pressure and reduced gas exchange. Further, loss of left ventricular function will cause the symptoms of left ventricular failure, with its associated pulmonary oedema.
6.1.3 Auscultation There may be crepitations and wheezes and whistles in the lungs due to fluid accumulation in the lungs due to myocardial dysfunction. Heart sounds are generally normal, but there may be additional murmurs due to valve dysfunction. Pericardial effusion may dull the heart sounds.
6.1.4 Hypotension The loss of function of the myocardium can cause hypotension, but the fall in blood pressure is dependent on the size and location of the infarction and the ability of the body to compensate by sympathetic response. (Diabetics may have an altered presentation because of impaired autonomic response). A severe fall in blood pressure is the basic cause of cardiogenic shock, which will add to the difficulties of the heart as it struggles for adequate perfusion.
6.1.5 Pallor and sweating An adrenegic response from the sympathetic nervous system will produce profuse sweating, and hypotension will produce pale skin as blood is diverted to the major organs.
6.1.6 Pulse There may be bradycardia (<60bpm), tachycardia (>100bpm) or an irregular pulse, depending on the site and severity of the problem. Any of these can lead to a reduction in cardiac function and can be precursors to cardiac arrest. It should be noted that tachycardia is common in detainees in custody due to anxiety. However, tahcycardia with a cardiac cause is not usually amenable to reassurance.
6.1.7 ECG ECG changes are highly variable, ranging from "tombstone" ST elevation to no changes at all, with many different types of arrhythmia in between. It is beyond the scope of this SOP to cover ECG changes.
6.2 Treatment If acute coronary syndrome or myocardial infarction is suspected, immediately call for an ambulance. Stay with the detainee and provide reassurance until the ambulance arrives. Keep them at rest, sitting at 45 degrees and with their legs raised to reduce the work of breathing and help maintain the blood pressure. Have the AED and resus bag brought to you. If the detainee is in a collapsed state, attach the AED pads and be ready to begin CPR. The ambulance crew will be able to perform a 12-lead ECG which will further aid diagnosis and guide the correct course of treatment. They will carry the necessary equipment, analgesia, medication and oxygen to treat the detainee appropriately. Detainees with chest pain from a suspected cardiac cause need to be sent to A&E without delay.
![Page 9: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/9.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 9 of 25
7. Stable Angina Detainees with stable angina will usually be aware of their condition and will often carry their own Glyceryl Trinitrate (GTN) spray. If they have never experienced angina before, or do not carry their own spray, treat as unstable angina, as above. Angina is generally caused by spasm of the coronary arteries supplying the myocardium. GTN spray will generally relieve this spasm within a few minutes.
7.1 Common signs and symptoms: 7.1.1 Pain
The pain from angina is often very similar to ACS and MI. The pain and discomfort of angina feels like a dull, heavy or tight pain in the chest that can sometimes spread to the left arm, neck, jaw or back. The pain is usually triggered by physical activity or stress, typically only lasts for a few minutes and can be relieved by the use of GTN.
7.1.2 Dyspnoea Unstable angina can cause dyspnoea in the same way as ACS, but it is usually less marked.
7.1.3 Hypotension Unstable angina can cause hypotension in the same way as ACS, but it is usually less marked.
7.1.4 Pallor and sweating These usually occur with angina, for the same reasons as ACS.
7.1.5 Pulse The pulse rate is usually increased due to adrenergic response to pain and anxiety. However, marked bradycardia or tachycardia should prompt a strong suspicion of ACS and guide treatment.
7.1.6 ECG Myocardial ischaemia will generally cause widespread ST segment depression. This will only be found if an ambulance is called and an ECG is taken.
7.2 Treatment Suspected stable angina should be treated with a stat dose of 1 or 2 sprays of GTN under the tongue. (See PGD for inclusions and exclusions). If after 5 minutes this first dose only slightly reduces the pain or does not reduce it at all, a further dose should be given. This can be repeated once more, up to a total of three doses. If the detainee is still experiencing pain or signs and symptoms, an ambulance should be called and the detainee treated as for ACS. It should be noted that the Police have GTN spray available for PRN use. Any doses given by the Police prior to the clinician seeing the detainee should be taken into account when counting the number of doses.
![Page 10: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/10.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 10 of 25
8. Pericarditis Pericarditis is a relatively rare, but serious condition. It is an inflammation of the pericardial sac surrounding the heart and can have several causes. Infection by viruses and bacteria will often cause the signs and symptoms and normally include pyrexia. Post-infarction pericarditis often appears within 24 hours of a myocardial infarction, but this will not be a common presentation in custody. However, it may occur weeks or months following MI, so a careful history must be taken, as with all detainees.
8.1 Common signs and symptoms 8.1.1 Pain
Pain from pericarditis is generally sharp and pleuritic and usually occurs substernal or in the left precordium and often radiates to the base of the scapula. The pain is relieved by sitting up and bending forward and worsened by lying down or taking a deep breath. The pain may resemble that from ACS, but is differentiated by the pain changing on movement or changing body position. It is not relieved by GTN.
8.1.2 Dyspnoea The detainee with pericarditis will often have a dry cough. Cardiac tamponade will often cause dyspnoea due to hypotension and the inability of the heart to maintain perfusion to the organs.
8.1.3 Auscultation There may be a friction rub as the inflamed tissues around the heart develop a rougher surface and rub together. The sound is usually more marked on the left sternal border. There may be muffled heart sounds from percardial tamponade due to pericardial effusion.
8.1.4 Pallor and sweating There is usually profuse sweating and marked pallor, caused by hypoperfusion and adrenergic response.
8.1.5 Blood pressure There is often marked hypotension, and also increased jugular venous distension due to right heart failure and fluid overload.
8.2 Treatment Treat as for ACS. Immediately call for an ambulance. Stay with the detainee and provide reassurance until the ambulance arrives. Keep them at rest, sitting at 45 degrees and with their legs raised to reduce the work of breathing and help maintain the blood pressure. Have the AED and resus bag brought to you. Be ready to begin CPR.
![Page 11: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/11.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 11 of 25
9. Abdominal Aortic Aneurysm (Triple A)
9.1 Common signs and symptoms
• Unruptured - Often presenting as a pulsatile mass in the abdomen, with persistent mild to moderate abdominal and/or back pain.
• Ruptured - Pain is sudden and severe in the mid-abdomen. In men, this pain may radiate into the scrotum. Often described as tearing, or "being cut in half".
9.1.1 Dyspnoea Dyspnoea usually becomes severe as the sudden loss of blood pressure causes hypoperfusion of vital organs.
9.1.2 Blood pressure In the early stages the blood pressure may fall only slightly for the first ten minutes or so. There may be a difference of 10mmHg or more in the blood pressure in the left and right arms. In later stages, as the rupture advances, the lower legs may become cold to the touch due to lack of blood supply and the blood pressure will usually rapidly fall catastrophically, causing fainting, unconsciousness or cardiac arrest.
9.1.3 Pallor and sweating The detainee will usually be pale and have profuse sweating due to the effects of the pain and hypotension.
9.1.4 Abdominal examination There may be a pulsatile mass in the mid-abdomen (but this is normal in some detainees). The area may be locally tender and there may be some guarding.
9.2 Treatment Immediately call for an ambulance. Stay with the detainee and provide reassurance until the ambulance arrives. Keep them at rest, sitting at 45 degrees and with their legs raised to reduce the work of breathing and help maintain the blood pressure. Have the AED and resus bag brought to you. If the detainee is in a collapsed state, attach the AED pads and be ready to begin CPR.
![Page 12: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/12.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 12 of 25
10. Pulmonary embolism
10.1 Common signs and symptoms 10.1.1 Pain
There is usually a sharp, stabbing pain, (pleuritic pain), often localised but sometimes widespread. It is normally worse on inspiration.
10.1.2 Dyspnoea The level of dyspnoea will depend on the size of the area of lung affected, which depends on where the clot is located. Dyspnoea can develop suddenly or may come on slowly. The detainee will usually have a cough, which may sometimes produce haemoptysis (red-stained frothy mucus or sometimes frank blood). Severe cases can cause cyanosis of the lips and fingertips.
10.1.3 Blood pressure The blood pressure may fall, causing faintness, dizziness or unconsciousness.
10.1.4 Pallor and sweating This may occur if the blood pressure falls significantly and/or the oxygen saturation falls significantly.
10.1.5 Auscultation There may be an area of pleural friction rub, heard on deep inspiration. Pleural effusion may cause a decreased percussion note, due to the presence of fluid in the lung.
10.2 Treatment Immediately call for an ambulance. Stay with the detainee and provide reassurance until the ambulance arrives. Keep them at rest, sitting at 45 degrees and with their legs raised to reduce the work of breathing and help maintain the blood pressure. Have the AED and resus bag brought to you. Be ready to begin CPR.
![Page 13: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/13.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 13 of 25
11. Pneumothorax This is most often caused by trauma, but some detainees, notably young, tall and thin individuals, may have a spontaneous pneumothorax.
11.1 Common signs and symptoms 11.1.1 Pain
This usually sharp and stabbing pain which develops in one side of the chest. The pain is usually worse on inspiration.
11.1.2 Dyspnoea This can be mild, moderate or severe, depending on the size and stage of development of the pneumothorax. It is usually described as "can't get my breath".
11.1.3 Blood pressure There is usually little effect on blood pressure.
11.1.4 Pallor and sweating This may occur if the pneumothorax is large or well-developed, particularly if the pain is perceived as severe.
11.1.5 Auscultation There may be reduced breath sounds on the affected side, but this may be hard to detect. Percussion may produce hyper-resonance over the affected area.
11.2 Treatment Immediately call for an ambulance. Stay with the detainee and provide reassurance until the ambulance arrives. Keep them at rest, sitting at 45 degrees and with their legs raised to reduce the work of breathing and help maintain the blood pressure. Have the AED and resus bag brought to you. Cardiac arrest is unlikely, but possible.
![Page 14: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/14.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 14 of 25
12. Musculo-skeletal This is a common cause of chest pain in detainees and can usually be suspected after a clear history is taken.
12.1 Common signs and symptoms 12.1.1 Pain
Usually well-localised, with tenderness on palpation, especially over areas or bruising, abrasions or other wounds. Deep inspiration may locally exacerbate the pain. Rib fractures, whilst uncommon, may be detected by palpation of the ribs away from the affected area.
12.1.2 Dyspnoea This may just be a response to pain.
12.1.3 Blood pressure There is usually little effect on blood pressure.
12.1.4 Auscultation This is usually unremarkable.
12.2 Treatment If a fracture is suspected, or there is loss of function, the detainee will need to go to hospital for x-rays and further treatment. Whether they go to hospital in an ambulance or police car is a clinical judgement depending on the severity and site of the injury. Detainees that do not go to hospital will need adequate analgesia (see PGDs).
![Page 15: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/15.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 15 of 25
13. Gastric reflux 13.1.1 Causes
Hiatus hernia, obesity, pregnancy, heavy and/or fatty meals, certain foods, smoking, constipation, lying down,
13.2 Common signs and symptoms 13.2.1 Pain
Usually epigastric and often described as burning, often rising up to the upper chest and throat. The pain can be mild to severe. If the reflux reaches the throat, there may be hoarseness and a sore throat as the acid affects the larynx and oropharynx. This may also cause difficulty in breathing. The pain is often made worse by lying down or bending over.
13.3 Treatment A simple drink of water often reduces the symptoms. Give Lansoprazole 30mg daily for the duration of detention. Advise on suitable foods and lifestyle. If there is evidence of GI blood loss, unintentional weight loss, dysphagia, persistent vomiting or an upper abdominal mass (with no symptoms of Triple A), advise the detainee to see their GP on release and provide a letter detailing your findings for them to take to their GP.
![Page 16: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/16.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 16 of 25
14. Hyperventilation Emotion and panic attacks are a major cause of hyperventilation and chest pains in the stressful situation of custody. However, careful history-taking and examination must be undertaken to exclude other causes, such as head injury, stroke, respiratory disorders such as asthma and pneumonia, cardiovascular problems such as pulmonary embolisms, and adverse reactions to drugs.
14.1 Common signs and symptoms 14.1.1 Pain
The detainee will usually have a tightness across the upper chest and a general aching in the chest.
14.1.2 Dyspnoea This can seem severe, but there would normally be no other physical signs, such as pallor or cyanosis.
14.1.3 Nervous system There may be confusion and anxiety. The detainee is often unamenable to reason due to panic. They may have a dry mouth, light-headedness and muscle spasms in the hands and feet (carpo-pedal spasm). They will usually have tingling in the arms and around the mouth. They may feel weak.
14.2 Treatment This is mainly supportive. Remain calm and reassure the detainee that they are not going to die, and carry out a full examination, explaining all the steps and the results. Get the detainee to control their breathing, taking long, slow breaths. Get them to purse their lips. Pinch one nostril and get the detainee to breathe only through their nose. Get the detainee to breathe abdominally without moving their chest. If a full and thorough examination reveals no underlying cause of the hyperventilation other than anxiety, ask the detainee to hold a paper bag over their mouth and nose for about 5-10 breaths, then take it away and ask the detainee to breathe normally or with pursed lips as above. If the above treatments do not resolve the issue after about 30 minutes, consider sending the detainee to hospital for a thorough examination and possible anxiolytic medication. It should be noted that Diazepam, whilst effective for short-term treatment of severe anxiety, is not indicated for this condition in the G4S PGD and authorisation must be sought from an FME for this use.
![Page 17: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/17.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 17 of 25
15. Drug use Many drugs can cause chest pains and cardiac problems. These are mainly due to heightened emotional states and adrenergic effects. Ecstasy, LSD, amphetamines, crystal meth, cannabis (particularly skunk), "legal highs" and many other illegal drugs can cause panic attacks, palpitations, paranoia and psychosis, all leading to chest pain and their effects should be treated symptomatically. However, cocaine use, particularly in regular high-use or naive users, can cause cocaine toxicity, with severe hypertension, chest pain or seizures. This is thought to be due to its effects on cardiac conduction due to its sympathomimetic properties, leading to tachycardia and a lowered ventricular fibrillation threshold. Cocaine is one of the most commonly reported substances in drug-related presentations to emergency departments, and is frequently implicated in drug-related deaths. Fatal cardiac arrhythmias can arise. There is also a risk of myocardial infarction, panic and anxiety, mental problems and psychosis, all leading to chest pain. Any detainee with chest pains and/or severe hypertension and admitting to, or suspected of, the use of cocaine should be sent immediately to hospital by ambulance. Stay with the detainee until the ambulance arrives and have the AED and resus bag brought to you.
![Page 18: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/18.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 18 of 25
16. Cardiac Arrest The following changes in the basic life support (BLS) guidelines have been made to reflect the importance placed on chest compression, particularly good quality compressions, and to attempt to reduce the number and duration of pauses during chest compression:
• When obtaining help, ask for an automated external defibrillator (AED), if one is available.
• Compress the chest to a depth of 5-6 cm and at a rate of 100-120 min.
• Do not stop to check the victim or discontinue CPR unless the victim starts to show
signs of regaining consciousness, such as coughing, opening his eyes, speaking, or moving purposefully AND starts to breathe normally.
• There is increased emphasis on the importance of minimal interruption in high-quality
chest compressions throughout any ALS intervention: chest compressions are paused briefly only to enable specific planned interventions.
• Checking pulse and breathing - HCPs accustomed to CPR should check for a pulse and
breathing for no more than 10 seconds. Those not accustomed to CPR should just check for breathing.
• In the first few minutes after cardiac arrest, a victim may be barely breathing, or taking
infrequent, noisy, gasps. This is often termed agonal breathing and must not be confused with normal breathing.
• Look, listen, and feel for no more than 10s to determine if the victim is breathing
normally. If you have any doubt whether breathing is normal, act as if it is not normal.
• Absent muscle tone after seizures may indicate asystolic cardiac arrest.
16.1 Resuscitation If it appears that a detainee is in cardiac arrest
• Immediately begin Basic Life Support Algorithm
• Get custody staff to call 999 for an ambulance
• Get help from at least one member of custody staff – preferably two
• Have the AED and resus bag brought to you
• When the AED arrives, follow the AED Algorithm
• When the ambulance crew arrive, begin the Advanced Life Support Algorithm
![Page 19: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/19.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 19 of 25
Adult Basic Life Support
Unresponsive and not breathing normally
30 Chest compressions
Call 999 and ask for an ambulance
2 Rescue breaths
As soon as AED arrivesswitch it on and follow
instructions
Continue CPR 30:2
![Page 20: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/20.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 20 of 25
Adult Advanced Life Support
Unresponsive and not breathing normally
Call resuscitation team
CPR 30:2Attach defibrillator/monitor
Minimise interruptions
Shockable(VF/Pulseless VT)
1 ShockMinimise interruptions
Immediately resumeCPR for 2 min
Minimise interruptions
Return of spontaneous circulation
Immediate post cardiac arrest treatment
Use ABCDE approach Aim for SpO2 of 94-98% Aim for normal PaCO2 12-lead ECG Treat precipitating cause Targeted temperature
management
Non-shockable(PEA/Asystole)
Immediately resumeCPR for 2 min
Minimise interruptions
During CPR Ensure high quality chest compressions Minimise interruptions to compressions Give oxygen Use waveform capnography Continuous compressions when
advanced airway in place Vascular access (intravenous or
intraosseous) Give adrenaline every 3-5 min Give amiodarone after 3 shocks
Treat Reversible Causes Hypoxia Hypovolaemia Hypo-/hyperkalaemia/metabolic Hypothermia
Thrombosis - coronary or pulmonary
Tension pneumothorax Tamponade – cardiac Toxins
Assess rhythm
Consider Ultrasound imaging Mechanical chest
compressions to facilitate transfer/treatment
Coronary angiography and percutaneous coronary intervention
Extracorporeal CPR
![Page 21: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/21.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 21 of 25
Traumatic Cardiac Arrest Treatment Algorithm
Cardiac arrest
Continue CPR
Likely medical cause?
Follow ALS algorithmPenetrating trauma to chest/epigastrium?
Start CPR
Consider termination of resuscitation
Treat reversible causes(Use 4Hs & 4Ts approach)
Hypovolaemia
Hypoxia
Tension pneumothorax
Tamponade – cardiac
Control external bleeding Splint pelvis/fractures IV/IO fluid/blood
Basic/advanced airway management Give oxygen
Decompress chest (thoracostomy)
Consider thoracotomy
Prehospital
In hospital
Immediate transfer to appropriate hospital
Immediate transfer to operating theatre/interventional radiology if indicated
yesno
Consider immediate thoracotomy
yesno
yes no
Spontaneous circulation?
Trauma patient
Peri-arrest
![Page 22: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/22.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 22 of 25
16.2 Stopping resuscitation Guidelines from the Joint Royal Colleges Ambulance Service Liaison Committee (2006), advise that ambulance clinicians may stop resuscitation if all of the following criteria are met:
• 15 min or more has passed since the onset of collapse. • No bystander CPR was given before arrival of the ambulance. • There is no suspicion of drowning, hypothermia, poisoning/overdose, or pregnancy. • Asystole is present for more than 30 s on the ECG monitor screen.
Pre-hospital resuscitation attempts are also generally discontinued if the rhythm remains asystole despite 20 min of advanced life support (ALS) except in cases of drowning and hypothermia. In custody, it is not expected that all these criteria will often be met, so it will be usual for a detainee in cardiac arrest to be transported to hospital with ongoing ALS. However, if resuscitation attempts are halted, the Death in Custody procedures must be followed. These will be led by the Police and every assistance must be given.
![Page 23: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/23.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 23 of 25
17. Medication Arrangements
• Obtain medication from detainee’s property for inspection. If medication is boxed and labelled for the detainee, proceed as usual (see medications SOP)
• If medication is not boxed and labelled for the detainee,
check suitability of medications with GP (in hours) or FME (out of hours) or SCR (all times). If suitable, proceed as usual (see medications SOP). If not suitable, obtain advice from GP or FME
• If detainee says that they are currently taking a medication and it is not in their property
If the medication is obtainable from home or its current location, arrange for the police to collect it and proceed as usual (see medications SOP).
• If the medication is not obtainable from home or its current location check with GP (in hours) or FME (out of hours) and if required, obtain a prescription to be faxed direct to a local pharmacy. Arrange for the police to collect the medication and then proceed as usual (see medication SOP)
18. Reviews Detainees with chest pain will not normally require reviews, unless there are specific concerns.
19. Advice to Detainee • Detainee is to be advised of any medication arrangements and the reasons for the
arrangements, as they may differ from their home arrangements. • Detainee is to be advised to alert Custody Staff of any problems at an early stage. • Detainee is to be given advice on the ongoing management of their condition after they
leave custody.
20. Advice to Custody Staff • Custody Staff are to be advised of medication arrangements, review times, and signs
and symptoms to look for, e.g. further chest pain, breathlessness, pallor and sweating.
![Page 24: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/24.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 24 of 25
21. TRAINING REQUIREMENTS The contents of this SOP should be included in the Induction Training for all Health Care Professionals that work in Police Custody. The trainee should record the successful completion of this part of the Induction Course and this record should be kept in their personnel file. Knowledge of this SOP should be re-assessed during annual appraisals.
22. REFERENCES AND ASSOCIATED DOCUMENTATION
• Resuscitation Council Guidelines (2015) • NICE Guidelines – Chest pain of recent onset CG95 (2010) • FFLM Guidance - Health care of detainees in police stations • NMC Code of Professional Conduct for Nurses • HCPC Code of Professional Conduct for Paramedics
23. VERSION HISTORY LOG This area should detail the version history for this document. It should detail the key elements of the changes to the versions.
Version Date Implemented Details of Significant Changes 1.01 01/06/2016 Original draft 1.02 01/06/2016 Resus Guidelines 2015 incorporated
![Page 25: Standard Operating Procedure · Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 2 of 25 For Completion by SOP Lead Name of Responsible Committee , [Insert Date Ratified]](https://reader033.fdocuments.net/reader033/viewer/2022041821/5e5e5768d2a68b7bf178e50e/html5/thumbnails/25.jpg)
Chest Pain in Police Custody SOP 1.02 1st June 2016 Page 25 of 25
24. CONFIRMATION OF SOP TRAINING RECORD
A copy of this record may be kept in your personal training file to confirm your training in a specific SOP.
SOP Details: To be completed by the SOP Controller
Title of SOP
Reference Number Insert SOP Reference Number. xxxxxxx
Version Insert Version
Issue Date Insert Date Issued
Implementation Date Insert Agreed Date for Implementation.
Personnel Details
Name
Job Title & Research Role
Date of Training
Nature of Training Self Directed/Delivered by etc
Records of any meetings to clarify details in SOP
Signatures
I confirm that I have read and consider myself to be sufficiently trained in the above Standard Operating Procedure with regards to my individual roles and responsibilities Signature of Trainee ………………………………………………………… Date ………………………
I confirm training in the above SOP was delivered as recorded above and that the trainee may be considered sufficiently trained in their roles and responsibilities Signature of Trainer …………………………………………………………… Date ……………………… .