Sperm impairments in adult vesper mice (Calomys laucha) caused by in utero exposure to bisphenol A
-
Upload
janice-vilela -
Category
Documents
-
view
11 -
download
0
description
Transcript of Sperm impairments in adult vesper mice (Calomys laucha) caused by in utero exposure to bisphenol A
-
ORIGINAL ARTICLE
Sperm impairments in adult vesper mice (Calomys laucha)caused by in utero exposure to bisphenol AJ. Vilela1, A. Hartmann1, E. F. Silva2, T. Cardoso1, C. D. Corcini1,2, A. S. Varela-Junior1, P. E. Martinez1
& E. P. Colares1
1 Instituto de Cie^ncias Biologicas, Universidade Federal do Rio Grande (FURG), Rio Grande, RS, Brazil;
2 ReproPel, Faculdade de Veterinaria, Campus Cap~ao do Le~ao, Universidade Federal de Pelotas (UFPel), Pelotas, RS, Brazil
Keywords
BisphenolCalomysendocrine disruptor
reproductionsemen
Correspondence
Janice Vilela, Programa de Pos-Graduac~aoem Cie^ncias Fisiologicas: Fisiologia Animal
Comparada - Instituto de Cie^ncias Biologicas,
Universidade Federal de Rio Grande. Av. Italia
km 8 Bairro Carreiros, Rio Grande,
RS 96203-900, Brazil.
Tel.: +55 (61) 8305 0527;
Fax: +55 (53) 3233 6848;
E-mail: [email protected]
Accepted: September 9, 2013
doi: 10.1111/and.12182
Summary
This study aimed to evaluate the effects of in utero administration of bisphenol A
(BPA) on semen parameters of vesper mice. Sixty female Calomys laucha were
divided into six groups and received by gavage during gestation the following sub-
stances: Water (negative control), Olive Oil (vehicle control), Diethylstilbestrol
(DES positive control 6.5 lg kg1 bw) and BPA (40, 80 and 200 lg kg1 bw).Male offspring were euthanised at 70 days of age, and sperm parameters were anal-
ysed. BPA reduced normal sperm morphology (water = 96.1 0.65;BPA200 = 96.8 2.3%), sperm membrane integrity (water = 88.8 1,65; BPA200 = 70.6 4,15%), sperm motility (water = 87.5 1.71; BPA200 = 51.3 9.9%) and in vitro penetration rates (water = 55.0 7.14; BPA200 = 7.47 2.96%), but it did not affect body weight, anogenital distance, sperm DNA integ-
rity and acrosome integrity. In conclusion, in utero exposure to BPA caused a
reduction in sperm parameters of adult C. laucha. Natural mating studies should
be conducted to verify the effects of BPA on fertility of the animals.
Introduction
It is well documented that several natural and man-made
chemicals interfere with the hormonal system of vertebrate
and invertebrate organisms (Pawlowski et al., 2004), acting
as endocrine disruptors both directly, by binding to
hormonal receptors, and indirectly, by modulating endoge-
nous hormone levels, by interfering with biochemical
processes associated with the production, availability or
metabolism of hormones, or also by the modulation of
receptors (Lagadic et al., 2007). One of them is bisphenol
A (BPA), a substance used in the production of
polycarbonate plastic and epoxy resins which are used in
manufacturing plastic containers, baby bottles and other
products (Geens et al., 2012). This chemical was found to
be an important endocrine disruptor that acts by mimick-
ing estrogens (Welshons et al., 2006), and it has been
detected in air, fresh and marine waters, soil and sediments
(Rodriguez-Mozaz et al., 2005; Vandenberg et al., 2007; Fu
& Kawamura, 2010; Flint et al., 2012; Huang et al., 2012).
Many studies have shown that mice perinatally exposed
to BPA present impaired fertility (Toyama & Yuasa, 2004;
Salian et al., 2009, 2011; LaRocca et al., 2011) as well as
increased anogenital distance and reduced prostate size
and epididymis weight (Gupta, 2000). Also, BPA has been
reported reducing sperm count in rats that ingested 25
and 100 ng kg1 (Al-Hiyasat et al., 2002); in humans,higher doses of urine BPA were related to lower sperm
concentration and motility and higher sperm DNA
damage (Meeker et al., 2010; Li et al., 2011).
While most of the studies of BPA effects aim to
extrapolate the results to human impacts, there are few
studies concerning its effects on wildlife (Nieminen et al.,
2002a,b). Evaluation of BPA exposure on mammals cur-
rently relies on data from laboratory studies on model
animals, such as mice and rats, and indicates many detri-
mental effects on rodents at high levels of BPA. However,
wildlife species may be exposed to chemicals at low doses
and thus act as bioindicators for the effects of endocrine
disruptors in natural ecosystems (Flint et al., 2012). The
vesper mouse (Calomys laucha, Waterhouse 1837) is a
small rodent found in South America (Reis et al., 2006)
and it is of epidemiological relevance as a reservoir of
Hantavirus and of protozoa pathogenic to humans (Mills
2013 Blackwell Verlag GmbH 1Andrologia 2013, xx, 18
-
et al., 1994). Its spermatozoon has a rounded head,
similar to that of no rodent mammals, and their small
size and rapid reproductive cycle are beneficial to experi-
mental studies (Lasserre et al., 2000). Moreover, this
species has some advantages over conventional rodents
for toxicological studies because of its genetic variability
and resistance to stressful agents (Vandenbergh, 2004).
While the main source for human exposure to BPA is
food and liquid storage containers, BPA is also released
into the environment through sewage treatment effluent
(via human-ingested BPA being eliminated through
sewage), landfill leachate (via hydrolysis of BPA from
plastics) and natural degradation of polycarbonate plastics
(Crain et al., 2007). As vesper mouse lives on coasts, in
pastures and along roadsides (Reis et al., 2006), this spe-
cies may be affected by environmental sources of BPA.
Since these animals still present wild characteristics, what
is observed in captivity may be similar to what happens
in wildlife. Therefore, this study aimed to verify the
effects of in utero exposure to BPA on sperm parameters
of adult Calomys laucha.
Materials and methods
Animal handling
Animals were from the vivarium of nonconventional
animals at the Federal University of Rio Grande (FURG),
Rio Grande do Sul, Brazil. Animal collection and
maintenance in captivity were approved by the Brazilian
Institute for Environmental Protection (IBAMA, permit
#14174-1). Animals used in this study were from F5 gen-
eration kept in the vivarium. Parental crosses were from
selected animals so as to prevent brothersister matings.The animals were individually housed in plastic boxes
(35 9 20 9 13 cm), kept in an environment with
controlled temperature (20.0 2.0 C) and photoperiod(LD 12:12, with light on at 6:00 a.m. and off at 6:00
p.m.), and received soy-free diet and water ad libitum.
Experimental design
Sixty female Calomys laucha from 50 to 70 days old were
kept with males to reproduce. As no alterations in vaginal
swab were observed, after 5 days, males were separated
and females were divided into six groups that received,
by gavage, the following treatments: (i) 100 ll of water(Negative control Water); (ii) 100 ll of olive oil(vehicle control); (iii) 6.5 lg kg1 body weight (bw) ofdiethylstilbestrol (DES - positive control); (iv) 40 lgkg1 bw of BPA (BPA40); (v) 80 lg kg1 bw of BPA(BPA80); (vi) 200 lg kg1 bw of BPA (BPA200). Thevehicle for administration of DES and BPA was 100 ll of
olive oil. The treatment was given daily from the day
males were separated from females until parturition. After
this period, treatment ceased and breastfeeding occurred
normally.
The current oral reference dose established by the US
Environmental Protection Agency is 50 lg kg1 day1 forconsumption of BPA without deleterious effects
(Vandenberg et al., 2007). For this study, therefore, the
lowest dose of BPA was lower than this reference dose, and
the highest dose was based on the lowest dose used in
another study conducted by our group (300 lg kg1 datanot published). The oestrogenic potency of DES is 1001000 times higher than BPA (vom Saal & Welshons, 2006),
so a lower dose of this substance was used.
Pups were counted, weighed and sexed at birth. Their
weight was gauged every 10 days until postnatal day
(PND) 50. Anogenital distance was measured at birth and
at PND 21. Males and females were euthanised by cervical
dislocation on PND 70, after reaching full maturation of
the reproductive tract. The procedures used for
experimentation and euthanasia of the animals followed
the recommendations of Brazilian law #6638 of May 8,
1979, and also those of the US National Institute of
Health guide for the use of laboratory animals (1996).
Chemical substances were purchased from Sigma
(St. Louis, MO, USA).
Semen analyses
Spermatozoa were collected after approaching the repro-
ductive system by laparotomy. The cauda of both epi-
didymes and part of the vas deferens were removed,
ruptured with a 12 g 9 40 mm needle and placed in a
35 mm Petri dish containing 200 ll of M2 medium withHEPES (M7167) (Corcini et al., 2012) for sperm dilution.
Sperm quality evaluations were done as described below
after incubation of samples for 10 min at 37 C in M2medium.
For sperm motility evaluation, an aliquot (10 ll) con-taining spermatozoa was placed between a slide and a cover
glass, and warmed at 37 C for further observation under aphase contrast optical microscope (Olympus BX 41-PH-III
America INC, S~ao Paulo, Brazil). Sperm motility was
reported as the average of three evaluations carried out by
a trained technician using optical microscopy at 2009
(Tayama et al., 2006) and expressed as percentage (0100%). Sperm morphology was determined after counting
200 cells using phase contrast microscopy at 10009 (Tay-
ama et al., 2006). Normal spermatozoa were counted, as
well as defects of distal droplet, detached head and tucked
tail. The number of sperm recovered from the epididymis
was counted in a Neubauer chamber by calculating the
concentration of spermatozoa per ml of medium.
2 2013 Blackwell Verlag GmbHAndrologia 2013, xx, 18
Sperm damage in mice by in utero exposure to BPA J. Vilela et al.
-
Sperm DNA integrity, mitochondrial functionality,
DNA integrity, sperm membrane integrity and acrosome
integrity were held in an epifluorescence microscope
(Olympus BX 51; America INC, S~ao Paulo, Brazil), with
5 ll of solution with sperm under coverslip (18 918 mm), evaluating 200 cells per sample. Results were
expressed in percentage of functional cells over total of
evaluated cells. Sperm DNA integrity was evaluated with
acridine orange gauge (Evenson & Jost, 2000). Sperm
membrane integrity and acrosome integrity were evalu-
ated at 4009 with 450520 nm filtre wavelength. Spermmembrane integrity was evaluated using carboxyfluoresce-
in diacetate and propidium iodide (Harrison & Vickers,
1990) and in each slide, 200 cells were counted and classi-
fied as follows: intact (green fluorescence) or not intact
(either red or simultaneous red and green fluorescence).
Acrosome integrity was evaluated using FITC-PNA, after
counting 200 cells in dry slides. Acrosomes were classified
as follows: intact, when the sperm cell presented red fluo-
rescence, the acrosome presented green fluorescence and
the cells conformation was normal; or not intact, when
the sperm cell presented red fluorescence but the acro-
some was not evident or presented abnormal conforma-
tion (Jimenez et al., 2003). Results were expressed as
percentage of intact acrosome. Mitochondrial functional-
ity was evaluated by fluorescent rhodamine 123 (Johnson
et al., 1980).
For the in vitro penetration (IVP) test, fresh oocytes were
collected from the ovarium of prepubertal gilts obtained
from a local abattoir. Oocytes were collected and pro-
cessed; thirty oocytes were used for each sample and the
test followed the protocol described by Corcini et al.
(2012). Briefly, a M2 medium containing HEPES, 0.4%
bovine serum albumin (A3311) and approximately
2 9 106 spermatozoa per ml was used. Gametes were incu-
bated in a water bath (37 C) for 2 h. Following incuba-tion, oocytes were collected, washed, stained with Hoescht
33 342 (10 lg ml1) for 15 min at 38 C and thenobserved under an epifluorescence microscope (4009 mag-
nification). Penetration rate (%) was calculated based on
the relationship between the number of penetrated oocytes
and the total number of oocytes per sample and per
treatment. For each male, the number of penetrated
oocytes and of spermatozoa per oocyte was counted.
Statistics
Statistical analysis was carried out using Statistica 7.0
software. Descriptive statistics were calculated for all eval-
uated sperm variables. The continuous variables were
tested for normal distribution with ShapiroWilk anddata were compared by the KruskalWallis H-test (Krus-kalWallis one-way analysis of variance by ranks) withmultiple comparisons of mean ranks for all groups (Siegel
& Castellan, 1988).
Results
Of all sixty females, 41 sired litters. Mean birth weight
was 1.6 0.1 g and there was no statistical differencebetween the groups. One animal from the BPA40 group
was born dead and without three limbs (Fig. 1). Two ani-
mals from the BPA80 group presented male genitals and
female reproductive tract. No statistical differences were
found for number of males and females and proportion
of genders per treatment, which was 15.6 1.9 malesand 15.3 2.3 females (proportion 1:1). Number ofpups per litter also presented no statistical differences
between the groups, with a mean of 3.8 0.31 femalesand 2.2 0.48 males. No statistical differences werefound for anogenital distance (AGD), which was
3.48 0.06 mm.Spermatozoa were collected and analysed from a total
of 71 males, 16 being from water group, 8 from olive oil,
13 from DES, 15 from BPA40, 11 from BPA80 and 8
from BPA200. Number of spermatozoa increased signifi-
cantly in the olive oil group in relation to all other
groups (P < 0.05). Values tended to be lower in DES andBPA groups (Fig. 2) in relation to vehicle group, despite
being statistically equal to water group.
Sperm DNA integrity and acrosome integrity are pre-
sented in Table 1. No statistical differences were found
(a) (b)
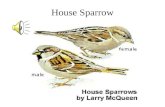
Fig. 1 Newborn Calomys laucha from bisphe-
nol A (BPA) 40 group without three limbs.
2013 Blackwell Verlag GmbH 3Andrologia 2013, xx, 18
J. Vilela et al. Sperm damage in mice by in utero exposure to BPA
-
for DNA integrity, but the values tended to drop in the
BPA200 group (P > 0.05). Acrosome integrity did notdiffer between vehicle group and treatment groups, but
values were significantly higher in the water group.
Normal sperm morphology was statistically reduced
only in the BPA200 group (P < 0.05). Although defectsof morphology did not present statistical differences
between groups, BPA200 showed higher values in distal
droplets and detached head, while DES and BPA200 pre-
sented more tucked tails than the other groups (Table 2).
Sperm mitochondrial integrity, motility and sperm
membrane integrity are presented in Table 3. Mitochon-
drial integrity was statistically equal in the water and
BPA40 groups and significantly lower (P < 0.05) in thevehicle, DES, BPA80 and BPA200 groups, which did not
differ statistically from each other. Sperm motility was
statistically reduced in BPA80 and BPA200 in relation to
the other groups and membrane integrity was signifi-
cantly reduced in BPA40 and BPA200 in relation to the
other groups (P < 0.05).
In vitro penetration rates were significantly reduced at
all BPA concentrations (Fig. 3). Number of penetrating
spermatozoa per oocyte was statistically lower only in the
BPA200 group (Fig. 4).
Discussion
Bisphenol A has shown conflicting responses in different
species and doses. It has been reported that litter size
remained consistent across BPA (50 and 1000 lg kg1)treatment groups and the vehicle (sesame oil) in mice,
but DES (5 lg kg1) decreased litter size both at birthand weaning (LaRocca et al., 2011). Studies have also
reported that in utero administration of doses of BPA
(0, 4 and 40 mg kg1 day1) through gavage had noeffects on growth and AGD of F1 rat offspring (Kobay-
ashi et al., 2002). Contrary to these observations, another
study reported that in utero administration of doses of
BPA (50 lg kg1 day1) through diet increased AGD inCD-1 mice offspring (Gupta, 2000). In this study, results
showed that in utero exposure to BPA and DES did not
affect litter size, weight of animals or the AGD. Discrep-
ancies between the results may be because of differences
Fig. 2 Number of spermatozoa for Calomys laucha exposed in utero
to water, olive oil, Diethylstilbestrol (DES) (6.5 lg kg1) and bisphenolA (BPA) (40, 80 and 200 lg kg1) (N = 71). Data expressed asMean SE. Values followed by different letters differ significantly byKruskalWallis test (P < 0.05).
Table 1 Sperm DNA integrity and acrosome integrity for Calomys
laucha exposed in utero to water, olive oil, Diethylstilbestrol (DES)
(6.5 lg kg1) and bisphenol A (BPA) (40, 80 and 200 lg kg1)(N = 71)
Treatment DNA Acrosome
Water 97.9 0.73a 89.6 2.24aOlive Oil 95.4 2.01a 50.0 2.38bDES 91.0 4.12a 43.6 4.08bBPA40 85.1 6.19a 48.1 3.29bBPA80 90.5 4.23a 48.7 2.52bBPA200 89.5 3.06a 49.2 2.71b
Results are expressed as Mean of percentage SE. Values followedby different letters in the same column differ significantly by Kruskal
Wallis test (P < 0.05).
Table 2 Sperm morphology for Calomys laucha exposed in utero to
water, olive oil, Diethylstilbestrol (DES) (6.5 lg kg1) and bisphenol A(BPA) (40, 80 and 200 lg kg1) (N = 71)
Treatment Normal
Distal
droplet
Detached
head
Tucked
Tail
Water 96.1 0.65a 1.1 0.38a 1.0 0.25a 2.0 0.59aOlive Oil 96.0 0.86a 1.8 0.89a 1.1 0.32a 0.9 0.49aDES 94.5 0.98a 1.3 0.42a 0.7 0.49a 4.0 0.96aBPA40 93.7 1.50a 1.5 0.61a 1.4 0.41a 3.4 1.64aBPA80 94.6 1.08a 1.1 0.30a 1.0 0.43a 3.9 1.12aBPA200 90.8 2.30b 3.8 1.01a 2.7 0.84a 4.4 2.93a
Data expressed as Mean of percentage SE. Values followed by dif-ferent letters in the same column differ significantly by KruskalWallis
test (P < 0.05).
Table 3 Sperm mitochondrial integrity (Mit). motility and membrane
integrity (Mem) for Calomys laucha exposed in utero to water, olive
oil, Diethylstilbestrol (DES) (6.5 lg kg1) and bisphenol A (BPA) (40,80 and 200 lg kg1) (N = 71)
Treatment Mit Motility Mem
Water 92.8 1.71a 87.5 1.71a 88.8 1.65aOlive Oil 35.2 6.24b 65.7 13.43a 77.2 3.63aDES 35.8 7.09b 78.8 2.27a 55.9 13.85aBPA40 61.8 9.20a 79.2 2.60a 65.5 5.09bBPA80 58.6 6.89b 61.8 7.11b 74.6 4.14aBPA200 56.1 7.20b 51.3 9.90b 70.6 4.15b
Data expressed as Mean of percentage SE. Values followed by dif-ferent letters differ significantly by Kruskal-Wallis test (P < 0.05).
4 2013 Blackwell Verlag GmbHAndrologia 2013, xx, 18
Sperm damage in mice by in utero exposure to BPA J. Vilela et al.
-
among species and route and vehicle of administration of
the substances.
It is known that in utero exposure of DES in women is
a cause of several anatomical and functional disorders of
the genital tract (Laurent et al., 1998). In this study,
although neither BPA nor DES affected AGD, it was
observed that only 3 females that received DES by gavage
sired a litter, while this number was much higher in the
other groups. The dose of 6.5 lg kg1 of DES given tothe females may have caused anatomical, functional or
hormonal disorders. To verify this hypothesis, uteri of all
the female breeders and their litters were collected for
future histological analyses.
Studies indicate that BPA exposure results in perma-
nent alterations in androgen-target tissues (Maffini et al.,
2006). Corroborating this hypothesis, an increase in pros-
tate duct volume (Timms et al., 2005), enlarged prostates
and decreased epididymal weight (Gupta, 2000) have
been previously reported in mice. In this study,
80 lg kg1 of BPA induced malformation of the repro-ductive system; additionally, 40 lg kg1 of BPA induced
limb malformation in one animal. Other studies have
reported teratogenic effects of BPA in Xenopus laevis
(Iwamuro et al., 2003) and early mice embryos in vitro
(Pei et al., 2003), but this study demonstrates that doses
lower than that accepted by the US Environmental
Protection Agency may cause death and malformation in
foetuses of rodents.
Sperm DNA integrity has been shown to reduce in a
doseresponse manner with urinary BPA in men (Meekeret al., 2010). It has also been reported that in utero expo-
sure to endocrine disruptors influences the embryonic
testis and causes epigenetic effects such as DNA methyla-
tion, resulting in abnormal germ-cell differentiation that
influences adult spermatogenic capacity and male fertility
in rats (Lenzi et al., 1996). The doses used in this study
did not affect sperm DNA, but BPA tended to reduce
DNA integrity, so it is possible that higher doses may
cause a significant decrease in this parameter.
The effect of olive oil on acrosome integrity, mitochon-
drial integrity and increasing number of sperm lead us to
question whether olive oil was the best vehicle for admin-
istration of BPA. Many genes involved in fatty acid
metabolism are regulated by a family of three members of
the nuclear peroxisome proliferator-activated receptors
(PPARs), which regulate glucose homeostasis, lipid
metabolism and inflammation. There is indication that
oleic, linoleic and palmitic acids, which are present in
the olive oil, are ligands of PPARs (revised by Kaput
& Rodriguez, 2004). Since most studies do not compare
vehicle treatment with negative control (water),
comparing only treatment with BPA and other oestrogenic
compounds and the vehicle used (Nagao et al., 1999;
Kobayashi et al., 2002; Toyama & Yuasa, 2004; Salian
et al., 2009; LaRocca et al., 2011), our study may provide
new information about the use of oily vehicles for
administration of BPA, which may in fact protect the
cells against the epigenetic effect of BPA. Moreover, in
spite of the improving effects of olive oil, BPA still caused
a reduction in sperm parameters, indicating its inhibiting
effect. Sperm morphological abnormalities have been
reported in rats prenatally exposed to BPA, which
presented cytoplasmic droplets in the mid-piece, principal
and head regions of the spermatozoa (Salian et al., 2009).
In this study, droplets were found in the distal region of
the cell. However, these abnormalities may not impair
C. laucha reproduction, since normal sperm morphology
of this species has been reported by Corcini et al. (2012)
to be equal to 90.2 6.6%, which is lower than theBPA200 group in this study. Sperm motility has also been
shown to decrease in rats perinatally exposed to BPA
(Salian et al., 2009), and lower motility related to urinary
BPA in a doseresponse manner in men has beenreported (Li et al., 2011). Corroborating these findings, in
Fig. 3 In vitro penetration (IVP) rates for Calomys laucha exposed in
utero to water, olive oil, Diethylstilbestrol (DES) (6.5 lg kg1) andbisphenol A (BPA) (40, 80 and 200 lg kg1) (N = 71). Data expressedas Mean of percentage SE. Values followed by different lettersdiffer significantly by KruskalWallis test (P < 0.05).
Fig. 4 Number of penetrating spermatozoa per oocyte for Calomys
laucha exposed in utero to water, olive oil, Diethylstilbestrol (DES)
(6.5 lg kg1) and bisphenol A (BPA) (40, 80 and 200 lg kg1)(N = 71). Data expressed as Mean SE. Values followed by differentletters differ significantly by KruskalWallis test (P < 0.05).
2013 Blackwell Verlag GmbH 5Andrologia 2013, xx, 18
J. Vilela et al. Sperm damage in mice by in utero exposure to BPA
-
this study, sperm motility was significantly decreased in
groups BPA80 and BPA200 in relation to water and olive
oil.
The effect of BPA on plasma membrane integrity is
demonstrated for the first time in this study. Our results
for the water group were similar to those found by Cor-
cini et al. (2012), who studied in vitro assays for vesper
mice sperm and reported normal membrane integrity as
88.7 9.6% for C. laucha.All the parameters discussed above may influence the
IVP test. The IVP test presents high specificity, detecting
sub-fertile males unable to sire a litter after natural mat-
ing by detecting those failing to penetrate swine oocytes
in vitro (Corcini et al., 2012). Since C. laucha sperm head
morphology is similar to that of other mammals (Lasserre
et al., 2000), it has been shown that porcine oocytes are
useful heterologous substrates for in vitro fertilisation
studies of this species (Lasserre et al., 2000; Corcini et al.,
2012). This is the first study of IVP rates related to BPA.
In this study, BPA significantly reduced penetration rates
at all doses given. However, the reason for this reduction
in IVP rates could not be determined. As heterologous
oocytes were used, it is possible that BPA affected an
important factor for the spermatozoa to penetrate the
oocyte that was not analysed in this study. Corcini et al.
(2012) found IVP rates for C. laucha equal to 39.8%,
which is lower than our control groups, but higher than
treatment groups. However, to confirm the reduction of
fertility by BPA and DES, natural mating studies need to
be performed.
The mechanisms of action of BPA are not fully under-
stood. The adverse effects of BPA on sperm parameters
may be due to a direct effect on the testes, acting as an
androgen receptor (AR) antagonist that interrupts normal
AR binding activity (Wetherill et al., 2007). Also, BPA
may alter spermatogenesis by disrupting the hypothala-
muspituitarytestes axis, altering the function of Leydigcells and reducing testosterone biosynthesis (Takao et al.,
2003).
This study shows that prenatal exposure to BPA causes
permanent alterations in semen quality of C. laucha,
while other studies show that effects of adult and perina-
tal administration of BPA are transitory (Nagao et al.,
1999; Kuwada et al., 2002; Toyama & Yuasa, 2004). The
differences between in utero and perinatal administration
of BPA may occur because in utero exposure to BPA
affects the developing testes, thus affecting germ cells,
while perinatal exposure affects the already formed organ.
Another important observation in this study is that
most of the parameters were affected only by the highest
dose of BPA. Thus, data suggest C. laucha is more resis-
tant to low doses of BPA than other rodents; this may be
because wild species present higher genetic variability,
making them more resistant to a series of infectious and
stressful agents.
In conclusion, it is shown for the first time in vivo that
low doses of BPA may cause malformation of foetuses.
In utero exposure to high doses of BPA permanently
reduced normal sperm morphology, sperm membrane
integrity, sperm motility and IVP rates of adult C. laucha
males. This species may act as a bioindicator of BPA pol-
lution in natural environments. Natural mating experi-
ments must be conducted to confirm whether these
alterations reduce the fertility of the animals.
Acknowledgements
We thank the ReproPel team from the University of Pelo-
tas for help with the semen analyses and CAPES (Coorde-
nac~ao de Aperfeicoamento de Pessoal de Nvel Superior,Braslia, DF, Brazil) for financial support.
References
Al-Hiyasat AS, Darmani H, Elbetieha AM (2002) Effects of
bisphenol A on adult male mouse fertility. Eur J Oral Sci
110:163167.
Corcini CD, Stephan MHL, Colares EP, Santos ECS, Varela
AS, Bongalhardo DC, Lucia T (2012) In vitro assays for
vesper mice (Calomys laucha) sperm using heterologous
substrates from nonrodent species. J Exp Zool A 317:96102.
Crain DA, Eriksen M, Iguchi T, Jobling S, Laufer H, LeBlanc
GA, Guillette LJ Jr (2007) An ecological assessment of
bisphenol-A: evidence from comparative biology. Reprod
Toxicol 24:225239.
Evenson D, Jost L (2000) Sperm chromatin structure assay is
useful for fertility assessment. Meth Cell Sci 22:169189.
Flint S, Markle T, Thompson S, Wallace E (2012) Bisphenol A
exposure, effects, and policy: a wildlife perspective. J Environ
Manage 104:1934.
Fu P, Kawamura K (2010) Ubiquity of bisphenol A in the
atmosphere. Environ Pollut 158:31383143.
Geens T, Aerts D, Berthot C, Bourguignon JP, Goeyens L,
Lecomte P, Maghuin-Rogister G, Pironnet AM, Pussemier
L, Scippo ML, Van Loco J, Covaci A (2012) A review of
dietary and non-dietary exposure to bisphenol-A. Food
Chem Toxicol 50:37253740.
Gupta C (2000) Reproductive malformation of the male
offspring following maternal exposure to estrogenic
chemicals. Proc Soc Exp Biol Med 224:6168.
Harrison RAP, Vickers SE (1990) Use of fluorescent probes to
assess membrane integrity in mammalian spermatozoa.
J Reprod Fertil 88:343352.
Huang YQ, Wong CK, Zheng JS, Bouwman H, Barra R,
Wahlstrom B, Neretin L, Wong MH (2012) Bisphenol A
(BPA) in China: a review of sources, environmental levels,
and potential human health impacts. Environ Int 42:9199.
6 2013 Blackwell Verlag GmbHAndrologia 2013, xx, 18
Sperm damage in mice by in utero exposure to BPA J. Vilela et al.
-
Iwamuro S, Sakakibara M, Terao M, Ozawa A, Kurobe C,
Shigeura T, Kato M, Kikuyama S (2003) Teratogenic and
anti-metamorphic effects of bisphenol A on embryonic and
larval Xenopus laevis. Gen Comp Endocr 133:189198.
Jimenez I, Gonzalez-Marquez H, Ortiz R, Herrera JA, Garcii
A, Betancourt M, Fierro R (2003) Changes in the
distribution of lectin receptors during capacitation and
acrosome reaction in boar spermatozoa. Theriogenology
59:11711180.
Johnson LV, Walsh ML, Chen LB (1980) Localization of
mitochondria in living cells with rhodamine 123. Proc Nat
Acad Sci USA 77:990994.
Kaput J, Rodriguez RL (2004) Nutritional genomics: the next
frontier in the postgenomic era. Physiol Genom 16:166177.
Kobayashi K, Miyagawa M, Wang RS, Sekiguchi S, Suda M,
Honma T (2002) Effects of in utero and lactational
exposure to bisphenol A on somatic growth and anogenital
distance in F1 rat offspring. Ind Health 40:375381.
Kuwada M, Kawashima R, Nakamura K, Kojima H, Hasumi H,
Maki J, Sugano S (2002) Neonatal exposure to endocrine
disruptors suppresses juvenile testis weight and
steroidogenesis but spermatogenesis is considerably restored
during puberty. Biochem Biophysl Res commun 295:193197.
Lagadic L, Coutellec M-A, Caquet T (2007) Endocrine
disruption in aquatic pulmonate molluscs: few evidences,
many challenges. Ecotoxicology 16:4559.
LaRocca J, Boyajian A, Brown C, Smith SD, Hixon M (2011)
Effects of in utero exposure to Bisphenol A or
diethylstilbestrol on the adult male reproductive system.
Birth defects research Part B. Dev Reprod Toxicol 92:526
533.
Lasserre A, Cebral E, Vitullo AD (2000) Successful
capacitation and homologous fertilization in vitro in
Calomys musculinus and Calomys laucha (Rodentia -
sigmodontinae). J Reprod Fertil 120:4147.
Laurent S, Lanoue M, Lecomte C, Bourgeois L, Lecomte P
(1998) Female fertility prognosis and diethylstilbestrol.
Personal data and review of the literature. J Gynecol Obstet
Biol Reprod 27:277284.
Lenzi A, Picardo M, Gandini L, Dondero F (1996) Lipids of
the sperm plasma membrane: from polyunsaturated fatty
acids considered as markers of sperm function to possible
scavenger therapy. Hum Reprod Update 2:246256.
Li DK, Zhou Z, Miao M, He Y, Wang J, Ferber J, Herrinton
LJ, Gao E, Yuan W (2011) Urine bisphenol-A (BPA) level in
relation to semen quality. Fertil Steril 95:e621e624.
Maffini MV, Rubin BS, Sonnenschein C, Soto AM (2006)
Endocrine disruptors and reproductive health: the case of
bisphenol-A. Mol Cell Endocrinol 254255:179186.
Meeker JD, Ehrlich S, Toth TL, Wright DL, Calafat AM,
Trisini AT, Ye X, Hauser R (2010) Semen quality and sperm
DNA damage in relation to urinary bisphenol A among
men from an infertility clinic. Reprod Toxicol 30:532539.
Mills JN, Ellis BA, Childs JE, McKee KT Jr, Maiztegui JI,
Peters CJ, Ksiazek TG, Jahrling PB (1994) Prevalence of
infection with Junin virus in rodent populations in the
epidemic area of Argentine hemorrhagic fever. Am J Trop
Med Hyg 51:554562.
Nagao T, Saito Y, Usumi K, Kuwagata M, Imai K (1999)
Reproductive function in rats exposed neonatally to bisphenol
A and estradiol benzoate. Reprod Toxicol 13:303311.
Nieminen P, Lindstrom-Seppa P, Juntunen M, Asikainen J,
Mustonen AM, Karonen SL, Mussalo-Rauhamaa H,
Kukkonen JV (2002a) In vivo effects of bisphenol A on the
polecat (mustela putorius). J Toxicol Environ Health A
65:933945.
Nieminen P, Lindstrom-Seppa P, Mustonen AM, Mussalo-
Rauhamaa H, Kukkonen JV (2002b) Bisphenol A affects
endocrine physiology and biotransformation enzyme
activities of the field vole (Microtus agrestis). Gen Comp
Endocr 126:183189.
Pawlowski S, Ternes TA, Bonerz M, Rastall AC, Erdinger L,
Braunbeck T (2004) Estrogenicity of solid phase-extracted
water samples from two municipal sewage treatment plant
effluents and river Rhine water using the yeast estrogen
screen. Toxicol In Vitro 18:129138.
Pei XR, Li Y, Long DX, Chen X, Gao LF, Chen XG (2003) In
vitro study of bisphenol-A toxicity on the early embryo
development of mice. Chin J Reprod Health 14:3437.
Reis NR, Peracchi AL, Pedro WA, Lima IP (2006) Mamferos
do Brasil. Universidade Estadual de Londrina, Londrina.
Rodriguez-Mozaz S, de Alda ML, Barcelo D (2005) Analysis of
bisphenol A in natural waters by means of an optical
immunosensor. Water Res 39:5079.
vom Saal FS, Welshons WV (2006) Large effects from small
exposures. II. The importance of positive controls in low-
dose research on bisphenol A. Environ Res 100:5076.
Salian S, Doshi T, Vanage G (2009) Perinatal exposure of rats
to Bisphenol A affects the fertility of male offspring. Life Sci
85:742752.
Salian S, Doshi T, Vanage G (2011) Perinatal exposure of rats
to Bisphenol A affects fertility of male offspringan
overview. Reprod Toxicol 31:359362.
Siegel S, Castellan NJ (1988) Nonparametric Statistics for the
Behavioral Sciences. McGraw-Hill, New York.
Takao T, Nanamiya W, Nazarloo HP, Matsumoto R, Asaba K,
Hashimoto K (2003) Exposure to the environmental
estrogen bisphenol A differentially modulated estrogen
receptor-alpha and -beta immunoreactivity and mRNA in
male mouse testis. Life Sci 72:11591169.
Tayama K, Fujita H, Takahashi H, Nagasawa A, Yano N,
Yuzawa K, Ogata A (2006) Measuring mouse sperm
parameters using a particle counter and sperm quality
analyzer: a simple and inexpensive method. Reprod Toxicol
22:92101.
Timms BG, Howdeshell KL, Barton L, Bradley S, Richter CA,
vom Saal FS (2005) Estrogenic chemicals in plastic and oral
contraceptives disrupt development of the fetal mouse
prostate and urethra. Proc Natl Acad Sci USA 102:7014
7019.
2013 Blackwell Verlag GmbH 7Andrologia 2013, xx, 18
J. Vilela et al. Sperm damage in mice by in utero exposure to BPA
-
Toyama Y, Yuasa S (2004) Effects of neonatal administration
of 17b-estradiol, bestradiol 3-benzoate, or bisphenol A onmouse and rat spermatogenesis. Reprod Toxicol 19:181188.
Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV
(2007) Human exposure to bisphenol A (BPA). Reprod
Toxicol 24:139177.
Vandenbergh JG (2004) Animal models and studies of in
utero endocrine disruptor effects. ILAR J 45:438442.
Welshons WV, Nagel SC, vom Saal FS (2006) Large effects
from small exposures. III. Endocrine mechanisms mediating
effects of bisphenol A at levels of human exposure.
Endocrinology 147:S56S69.
Wetherill YB, Akingbemi BT, Kanno J, McLachlan JA, Nadal
A, Sonnenschein C, Watson CS, Zoeller RT, Belcher SM
(2007) In vitro molecular mechanisms of bisphenol A
action. Reprod Toxicol 24:178198.
8 2013 Blackwell Verlag GmbHAndrologia 2013, xx, 18
Sperm damage in mice by in utero exposure to BPA J. Vilela et al.








![The Vesper Martini€¦ · · 2016-08-22The Vesper Martini "A dry martini," [Bond] said. ... Rachmaninoff’s incredibly inspired “Vespers” on the turntable ... Microsoft Word](https://static.fdocuments.net/doc/165x107/5b0976d37f8b9abe5d8ca703/the-vesper-vesper-martini-a-dry-martini-bond-said-rachmaninoffs-incredibly.jpg)






![El casamiento de Laucha [microform]robertopayrÓ elcasamientodelaucha buenosaires compaÑÍasid-americanadeb1i,t.ktesdlíÜancÜ calleschile,263ycangallo,55759 1906](https://static.fdocuments.net/doc/165x107/5f40f259a311c47e3d795398/el-casamiento-de-laucha-microform-robertopayr-elcasamientodelaucha-buenosaires.jpg)



