Special Report—Neonatal Resuscitation: 2010 American...
Transcript of Special Report—Neonatal Resuscitation: 2010 American...

Special Report—Neonatal Resuscitation:2010 American Heart Association Guidelines forCardiopulmonary Resuscitation and EmergencyCardiovascular Care
The following guidelines are an interpretation of the evidence present-ed in the 2010 International Consensus on Cardiopulmonary Resusci-tation and Emergency Cardiovascular Care Science With TreatmentRecommendations1). They apply primarily to newly born infants under-going transition from intrauterine to extrauterine life, but the recom-mendations are also applicable to neonates who have completed peri-natal transition and require resuscitation during the first fewweeks tomonths following birth. Practitioners who resuscitate infants at birthor at any time during the initial hospital admission should considerfollowing these guidelines. For the purposes of these guidelines, theterms newborn and neonate are intended to apply to any infant duringthe initial hospitalization. The term newly born is intended to applyspecifically to an infant at the time of birth.
Approximately 10% of newborns require some assistance to beginbreathing at birth. Less than 1% require extensive resuscitative mea-sures.2,3 Although the vastmajority of newly born infants do not requireintervention to make the transition from intrauterine to extrauterinelife, because of the large total number of births, a sizable number willrequire some degree of resuscitation.
Those newly born infants who do not require resuscitation can gener-ally be identified by a rapid assessment of the following 3characteristics:
● Term gestation?
● Crying or breathing?
● Good muscle tone?
If the answer to all 3 of these questions is “yes,” the baby does not needresuscitation and should not be separated from the mother. The babyshould be dried, placed skin-to-skin with the mother, and covered withdry linen to maintain temperature. Observation of breathing, activity,and color should be ongoing.
If the answer to any of these assessment questions is “no,” the infantshould receive one or more of the following 4 categories of action insequence:
A. Initial steps in stabilization (provide warmth, clear airway if neces-sary, dry, stimulate)
B. Ventilation
John Kattwinkel, Co-Chair*, Jeffrey M. Perlman, Co-Chair*,Khalid Aziz, Christopher Colby, Karen Fairchild, JohnGallagher, Mary Fran Hazinski, Louis P. Halamek, PraveenKumar, George Little, Jane E. McGowan, BarbaraNightengale, Mildred M. Ramirez, Steven Ringer, WendyM. Simon, Gary M. Weiner, Myra Wyckoff,Jeanette Zaichkin
KEY WORDScardiopulmonary resuscitation
The American Heart Association requests that this document becited as follows: Kattwinkel J, Perlman JM, Aziz K, Colby C,Fairchild K, Gallagher J, Hazinski MF, Halamek LP, Kumar P, LittleG, McGowan JE, Nightengale B, Ramirez MM, Ringer S, SimonWM, Weiner GM, Wyckoff M, Zaichkin J. Part 15: neonatalresuscitation: 2010 American Heart Association Guidelines forCardiopulmonary Resuscitation and Emergency CardiovascularCare. Circulation. 2010;122:S909–S919.
*Co-chairs and equal first co-authors.
(Circulation. 2010;122:S909–S919.)© 2010 American Heart Association, Inc.
Circulation is available at http://circ.ahajournals.org.
doi:10.1542/peds.2010-2972E
e1400 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

C. Chest compressions
D. Administration of epinephrine and/or volume expansion
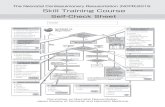
Approximately 60 seconds (“the GoldenMinute”) are allotted for completing theinitial steps, reevaluating, and beginningventilation if required (see Figure). Thedecision to progress beyond the initialsteps is determined by simultaneous
assessment of 2 vital characteristics:respirations (apnea, gasping, or laboredor unlabored breathing) and heart rate(whether greater than or less than 100beats per minute). Assessment of heartrate should be done by intermittentlyauscultating the precordial pulse. Whena pulse is detectable, palpation of theumbilical pulse can also provide a rapid
estimate of the pulse and is more accu-rate than palpation at other sites.4,5
A pulse oximeter can provide a contin-uous assessment of the pulse withoutinterruption of other resuscitationmeasures, but the device takes 1 to 2minutes to apply, and it may not func-tion during states of very poor cardiacoutput or perfusion. Once positive
FIGURE.Newborn Resuscitation Algorithm.
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1401
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

pressure ventilation or supplementaryoxygen administration is begun, as-sessment should consist of simulta-neous evaluation of 3 vital characteris-tics: heart rate, respirations, and thestate of oxygenation, the latter opti-mally determined by a pulse oximeteras discussed under “Assessment of Ox-ygen Need and Administration of Oxy-gen” below. The most sensitive indica-tor of a successful response to eachstep is an increase in heart rate.
ANTICIPATION OFRESUSCITATION NEEDAnticipation, adequate preparation,accurate evaluation, and prompt initi-ation of support are critical for suc-cessful neonatal resuscitation. At ev-ery delivery there should be at least 1person whose primary responsibilityis the newly born. This person must becapable of initiating resuscitation, in-cluding administration of positive-pressure ventilation and chest com-pressions. Either that person orsomeone else who is promptly avail-able should have the skills required toperform a complete resuscitation, in-cluding endotracheal intubation andadministration of medications.6 Sev-eral studies have demonstrated that acesarean section performed under re-gional anesthesia at 37 to 39 weeks,without antenatally identified risk fac-tors, versus a similar vaginal deliveryperformed at term, does not increasethe risk of the baby requiring endotra-cheal intubation.7–10
With careful consideration of risk fac-tors, the majority of newborns whowill need resuscitation can be identi-fied before birth. If the possible needfor resuscitation is anticipated, addi-tional skilled personnel should be re-cruited and the necessary equipmentprepared. Identifiable risk factors andthe necessary equipment for resusci-tation are listed in the Textbook ofNeonatal Resuscitation, 6th Edition
(American Academy of Pediatrics, inpress).11 If a preterm delivery (�37weeks of gestation) is expected, spe-cial preparations will be required. Pre-term babies have immature lungs thatmay be more difficult to ventilate andare also more vulnerable to injury bypositive-pressure ventilation. Pretermbabies also have immature blood ves-sels in the brain that are prone to hem-orrhage; thin skin and a large surfacearea, which contribute to rapid heatloss; increased susceptibility to infec-tion; and increased risk of hypovole-mic shock related to small bloodvolume.
INITIAL STEPSThe initial steps of resuscitation are toprovide warmth by placing the babyunder a radiant heat source, position-ing the head in a “sniffing” position toopen the airway, clearing the airway ifnecessary with a bulb syringe or suc-tion catheter, drying the baby, andstimulating breathing. Recent studieshave examined several aspects ofthese initial steps. These studies aresummarized below.
Temperature ControlVery low-birth-weight (�1500 g) pre-term babies are likely to become hypo-thermic despite the use of traditionaltechniques for decreasing heat loss.12
For this reasonadditionalwarming tech-niquesare recommended (eg, prewarm-ing the delivery room to 26°C,13 coveringthe baby in plastic wrapping (food ormedical grade, heat-resistant plastic)(Class I, LOE A14,15), placing thebaby onanexothermic mattress (Class IIb, LOE B16),and placing the baby under radiant heat(Class IIb, LOE C17). The infant’s tempera-ture must bemonitored closely becauseof the slight, but described risk of hyper-thermiawhen these techniquesareusedin combination (Class IIb, LOE B16). Othertechniques for maintaining tempera-ture during stabilization of the baby inthe delivery room have been used (eg,
prewarming the linen, drying and swad-dling, placing the baby skin-to-skin withthe mother and covering both with ablanket) andare recommended, but theyhave not been studied specifically (ClassIIb, LOE C). All resuscitation procedures,including endotracheal intubation, chestcompression, and insertion of intrave-nous lines, can be performed with thesetemperature-controlling interventions inplace (Class IIb, LOE C).
Infants born to febrile mothers havebeen reported to have a higher inci-dence of perinatal respiratory depres-sion, neonatal seizures, and cerebralpalsy and an increased risk of mortal-ity.18,19 Animal studies indicate that hy-perthermia during or after ischemia isassociated with progression of cere-bral injury. Lowering the temperaturereduces neuronal damage.20 Hyperther-mia should be avoided (Class IIb, LOE C).The goal is to achieve normothermia andavoid iatrogenic hyperthermia.
Clearing the Airway
When Amniotic Fluid Is ClearThere is evidence that suctioning of thenasopharynx can create bradycardiaduring resuscitation21,22 and that suc-tioning of the trachea in intubated ba-bies receiving mechanical ventilationin the neonatal intensive care unit(NICU) can be associated with deterio-ration of pulmonary compliance andoxygenation and reduction in cerebralblood flow velocity when performedroutinely (ie, in the absence of obviousnasal or oral secretions).23,24 However,there is also evidence that suctioningin the presence of secretions can de-crease respiratory resistance.25 There-fore it is recommended that suctioningimmediately following birth (includingsuctioning with a bulb syringe) shouldbe reserved for babies who have obvi-ous obstruction to spontaneous breath-ing or who require positive-pressureventilation (PPV) (Class IIb, LOE C).
e1402 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

When Meconium is PresentAspiration of meconium before deliv-ery, during birth, or during resuscita-tion can cause severe meconium aspi-ration syndrome (MAS). Historically avariety of techniques have been rec-ommended to reduce the incidence ofMAS. Suctioning of the oropharynx be-fore delivery of the shoulders was con-sidered routine until a randomizedcontrolled trial demonstrated it to beof no value.26 Elective and routine en-dotracheal intubation and direct suc-tioning of the trachea were initiallyrecommended for all meconium-stainednewborns until a randomized con-trolled trial demonstrated that therewas no value in performing this pro-cedure in babies who were vigorousat birth.27 Although depressed infantsborn tomotherswithmeconium-stainedamniotic fluid (MSAF) are at increasedrisk to developMAS,28,29 tracheal suction-ing has not been associated with reduc-tion in the incidence of MAS or mortalityin these infants.30,31 The only evidencethat direct tracheal suctioning of meco-niummay be of valuewas based on com-parisonof suctionedbabieswithhistoriccontrols, and there was apparent selec-tionbias in thegroupof intubatedbabiesincluded in those studies.32–34
In the absence of randomized, con-trolled trials, there is insufficient evi-dence to recommend a change in thecurrent practice of performing endo-tracheal suctioning of nonvigorousbabies with meconium-stained amni-otic fluid (Class IIb, LOE C). However, ifattempted intubation is prolongedand unsuccessful, bag-mask ventila-tion should be considered, particularlyif there is persistent bradycardia.
Assessment of Oxygen Needand Administration of OxygenThere is a large body of evidence thatblood oxygen levels in uncompromisedbabies generally do not reach extra-uterine values until approximately 10minutes following birth. Oxyhemoglo-
bin saturation may normally remain inthe 70% to 80% range for several min-utes following birth, thus resulting inthe appearance of cyanosis duringthat time. Other studies have shownthat clinical assessment of skin coloris a very poor indicator of oxyhemoglo-bin saturation during the immediateneonatal period and that lack of cyano-sis appears to be a very poor indicatorof the state of oxygenation of an un-compromised baby following birth.
Optimal management of oxygen duringneonatal resuscitation becomes par-ticularly important because of the evi-dence that either insufficient or exces-sive oxygenation can be harmful to thenewborn infant. Hypoxia and ischemiaare known to result in injury to multi-ple organs. Conversely there is grow-ing experimental evidence, as well asevidence from studies of babies receiv-ing resuscitation, that adverse out-comes may result from even brief ex-posure to excessive oxygen during andfollowing resuscitation.
Pulse OximetryNumerous studies have defined thepercentiles of oxygen saturation as afunction of time from birth in uncom-promised babies born at term (seetable in Figure). This includes satura-tions measured from both preductaland postductal sites, following bothoperative and vaginal deliveries, andthose occurring at sea level and ataltitude.35–40
Newer pulse oximeters, which employprobes designed specifically for neo-nates, have been shown to provide re-liable readings within 1 to 2 minutesfollowing birth.41–43 These oximetersare reliable in the large majority ofnewborns, both termand preterm, andrequiring resuscitation or not, as longas there is sufficient cardiac outputand skin blood flow for the oximeter todetect a pulse. It is recommended thatoximetry be used when resuscitation
can be anticipated,2 when positivepressure is administered for morethan a few breaths, when cyanosis ispersistent, or when supplementary ox-ygen is administered (Class I, LOE B).
To appropriately compare oxygen sat-urations to similar published data, theprobe should be attached to a preduc-tal location (ie, the right upper extrem-ity, usually the wrist or medial surfaceof the palm).43 There is some evidencethat attaching the probe to the babybefore connecting the probe to the in-strument facilitates the most rapid ac-quisition of signal (Class IIb, LOE C).42
Administration ofSupplementary OxygenTwo meta-analyses of several random-ized controlled trials comparing neo-natal resuscitation initiated with roomair versus 100% oxygen showed in-creased survival when resuscitationwas initiated with air.44,45 There are nostudies in term infants comparing out-comes when resuscitations are initi-ated with different concentrations ofoxygen other than 100% or room air.One study in preterm infants showedthat initiation of resuscitation with ablend of oxygen and air resulted in lesshypoxemia or hyperoxemia, as definedby the investigators, than when resus-citation was initiated with either airor 100% oxygen followed by titrationwith an adjustable blend of air andoxygen.46
In the absence of studies comparingoutcomes of neonatal resuscitationinitiated with other oxygen concentra-tions or targeted at various oxyhemo-globin saturations, it is recommendedthat the goal in babies being resusci-tated at birth, whether born at term orpreterm, should be an oxygen satura-tion value in the interquartile range ofpreductal saturations (see table in Fig-ure) measured in healthy term babiesfollowing vaginal birth at sea level(Class IIb, LOE B). These targets may be
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1403
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

achieved by initiating resuscitationwith air or a blended oxygen and titrat-ing the oxygen concentration toachieve an SpO2 in the target range asdescribed above using pulse oximetry(Class IIb, LOE C). If blended oxygen isnot available, resuscitation should beinitiated with air (Class IIb, LOE B). Ifthe baby is bradycardic (HR �60 perminute) after 90 seconds of resuscita-tion with a lower concentration of oxy-gen, oxygen concentration should beincreased to 100% until recovery of anormal heart rate (Class IIb, LOE B).
Positive-Pressure Ventilation (PPV)If the infant remains apneic or gasp-ing, or if the heart rate remains�100per minute after administering the ini-tial steps, start PPV.
Initial Breaths andAssisted VentilationInitial inflations following birth, eitherspontaneous or assisted, create a func-tional residual capacity (FRC).47–50 Theoptimal pressure, inflation time, andflow rate required to establish an effec-tive FRC when PPV is administered dur-ing resuscitation have not been deter-mined. Evidence from animal studiesindicates that preterm lungs are easilyinjured by large-volume inflations imme-diately after birth.51,52 Assisted ventila-tion rates of 40 to 60 breaths perminuteare commonly used, but the relative effi-cacy of various rates has not beeninvestigated.
The primary measure of adequate ini-tial ventilation is prompt improvementin heart rate.53 Chest wall movementshould be assessed if heart rate doesnot improve. The initial peak inflatingpressures needed are variable and un-predictable and should be individual-ized to achieve an increase in heartrate or movement of the chest witheach breath. Inflation pressure shouldbe monitored; an initial inflation pres-sure of 20 cm H2O may be effective, but�30 to 40 cm H2O may be required in
some term babies without spontane-ous ventilation (Class IIb, LOE C).48,50,54 Ifcircumstances preclude the use ofpressure monitoring, the minimal in-flation required to achieve an increasein heart rate should be used. There isinsufficient evidence to recommend anoptimum inflation time. In summary,assisted ventilation should be deliv-ered at a rate of 40 to 60 breaths perminute to promptly achieve or main-tain a heart rate �100 per minute(Class IIb, LOE C).
The use of colorimetric CO2 detectorsduring mask ventilation of small num-bers of preterm infants in the intensivecare unit and in the delivery room hasbeen reported, and such detectors mayhelp to identify airway obstruction.55,56
However, it is unclear whether the useof CO2 detectors during mask ventila-tion confers additional benefit aboveclinical assessment alone (Class IIb,LOE C).
End-Expiratory PressureMany experts recommend administra-tion of continuous positive airwaypressure (CPAP) to infants who arebreathing spontaneously, but with dif-ficulty, following birth, although itsuse has been studied only in infantsborn preterm. A multicenter random-ized clinical trial of newborns at 25 to28 weeks gestation with signs of respi-ratory distress showed no significantdifference in the outcomes of death oroxygen requirement at 36 weeks post-menstrual age between infants startedon CPAP versus those intubated andplaced onmechanical ventilation in thedelivery room. Starting infants onCPAP reduced the rates of intubationand mechanical ventilation, surfactantuse, and duration of ventilation, but in-creased the rate of pneumothorax.57
Spontaneously breathing preterm in-fants who have respiratory distressmay be supported with CPAP or withintubation and mechanical ventilation(Class IIb, LOE B). Themost appropriate
choice may be guided by local exper-tise and preferences. There is no evi-dence to support or refute the use ofCPAP in the delivery room in the termbaby with respiratory distress.
Although positive end–expiratory pres-sure (PEEP) has been shown to be ben-eficial and its use is routine duringme-chanical ventilation of neonates inintensive care units, there have beenno studies specifically examining PEEPversus no PEEP when PPV is used dur-ing establishment of an FRC followingbirth. Nevertheless, PEEP is likely to bebeneficial and should be used if suit-able equipment is available (Class IIb,LOE C). PEEP can easily be given with aflow-inflating bag or T-piece resuscita-tor, but it cannot be given with a self-inflating bag unless an optional PEEPvalve is used. There is, however, someevidence that such valves often deliverinconsistent end-expiratory pressures.58,59
ASSISTED-VENTILATION DEVICESEffective ventilation can be achievedwith either a flow-inflating or self-inflating bag or with a T-piece mechan-ical device designed to regulate pres-sure.60–63 The pop-off valves of self-inflating bags are dependent on theflow rate of incoming gas, and pres-sures generated may exceed the valuespecified by the manufacturer. Targetinflation pressures and long inspira-tory times are more consistentlyachieved in mechanical models whenT-piece devices are used rather thanbags,60,61 although the clinical implica-tions of these findings are not clear(Class IIb, LOE C). It is likely that infla-tion pressures will need to change ascompliance improves following birth,but the relationship of pressures to de-livered volume and the optimal volumeto deliver with each breath as FRC isbeing established have not been stud-ied. Resuscitators are insensitive tochanges in lung compliance, regard-less of the device being used (Class IIb,LOE C).64
e1404 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

Laryngeal Mask AirwaysLaryngeal mask airways that fit overthe laryngeal inlet have been shown tobe effective for ventilating newbornsweighing more than 2000 g or deliv-ered �34 weeks gestation (Class IIb,LOE B65–67). There are limited data onthe use of these devices in small pre-term infants, ie, � 2000 g or �34weeks (Class IIb, LOE C65–67). A laryn-geal mask should be considered dur-ing resuscitation if facemask ventila-tion is unsuccessful and trachealintubation is unsuccessful or not feasi-ble (Class IIa, LOE B). The laryngealmask has not been evaluated in casesof meconium-stained fluid, duringchest compressions, or for adminis-tration of emergency intratrachealmedications.
Endotracheal Tube PlacementEndotracheal intubation may be indi-cated at several points during neona-tal resuscitation:
● Initial endotracheal suctioning of non-vigorousmeconium-stained newborns
● If bag-mask ventilation is ineffectiveor prolonged
● When chest compressions areperformed
● For special resuscitation circum-stances, such as congenital dia-phragmatic hernia or extremely lowbirth weight
The timing of endotracheal intubationmay also depend on the skill and expe-rience of the available providers.
After endotracheal intubation and ad-ministration of intermittent positivepressure, a prompt increase in heartrate is the best indicator that the tubeis in the tracheobronchial tree andproviding effective ventilation.53 Ex-haled CO2 detection is effective for con-firmation of endotracheal tube place-ment in infants, including very low-birth-weight infants (Class IIa, LOEB68–71).A positive test result (detection of ex-haled CO2) in patientswith adequate car-
diac output confirms placement of theendotracheal tube within the trachea,whereas anegative test result (ie, no CO2detected) strongly suggests esophagealintubation.68–72 Exhaled CO2 detection isthe recommended method of confir-mation of endotracheal tube place-ment (Class IIa, LOE B). However, itshould be noted that poor or absentpulmonary blood flow may give false-negative results (ie, no CO2 detecteddespite tube placement in the tra-chea). A false-negative result may thuslead to unnecessary extubation and re-intubation of critically ill infants withpoor cardiac output.
Other clinical indicators of correct en-dotracheal tube placement are con-densation in the endotracheal tube,chest movement, and presence ofequal breath sounds bilaterally, butthese indicators have not been system-atically evaluated in neonates (Class11b, LOE C).
Chest CompressionsChest compressions are indicated fora heart rate that is �60 per minutedespite adequate ventilation with sup-plementary oxygen for 30 seconds. Be-cause ventilation is the most effectiveaction in neonatal resuscitation andbecause chest compressions are likelyto compete with effective ventilation,rescuers should ensure that assistedventilation is being delivered optimallybefore starting chest compressions.
Compressions should be delivered onthe lower third of the sternum to adepth of approximately one third of theanterior-posterior diameter of thechest (Class IIb, LOE C73–75). Two tech-niques have been described: compres-sion with 2 thumbs with fingers encir-cling the chest and supporting theback (the 2 thumb–encircling handstechnique) or compression with 2 fin-gers with a second hand supportingthe back. Because the 2 thumb–encir-cling hands technique may generate
higher peak systolic and coronaryperfusion pressure than the 2-fingertechnique,76–80 the 2 thumb–encirclinghands technique is recommended forperforming chest compressions innewly born infants (Class IIb, LOE C).The 2-finger technique may be prefer-able when access to the umbilicus isrequired during insertion of an umbil-ical catheter, although it is possibleto administer the 2 thumb–encirclinghands technique in intubated infantswith the rescuer standing at the baby’shead, thus permitting adequate accessto the umbilicus (Class IIb, LOE C).
Compressions and ventilations shouldbe coordinated to avoid simultaneousdelivery.81 The chest should be per-mitted to reexpand fully during relax-ation, but the rescuer’s thumbs shouldnot leave the chest (Class IIb, LOE C).There should be a 3:1 ratio of com-pressions to ventilations with 90 com-pressions and 30 breaths to achieveapproximately 120 events per minuteto maximize ventilation at an achiev-able rate. Thus each event will be allot-ted approximately 1/2 second, withexhalation occurring during the firstcompression after each ventilation(Class IIb, LOE C).
There is evidence from animals andnon-neonatal studies that sustainedcompressions or a compression ratioof 15:2 or even 30:2 may be more effec-tive when the arrest is of primary car-diac etiology. One study in childrensuggests that CPR with rescue breath-ing is preferable to chest compres-sions alone when the arrest is of non-cardiac etiology.82 It is recommendedthat a 3:1 compression to ventilationratio be used for neonatal resuscita-tion where compromise of ventilationis nearly always the primary cause, butrescuers should consider using higherratios (eg, 15:2) if the arrest is believedto be of cardiac origin (Class IIb, LOE C).
Respirations, heart rate, and oxygena-tion should be reassessed periodically,
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1405
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

and coordinated chest compressionsand ventilations should continue untilthe spontaneous heart rate is�60 perminute (Class IIb, LOE C). However, fre-quent interruptions of compressionsshould be avoided, as they will com-promise artificial maintenance of sys-temic perfusion and maintenance ofcoronary blood flow (Class IIb, LOE C).
MEDICATIONSDrugs are rarely indicated in resusci-tation of the newly born infant. Brady-cardia in the newborn infant is usuallythe result of inadequate lung inflationor profound hypoxemia, and establish-ing adequate ventilation is the mostimportant step toward correcting it.However, if the heart rate remains�60 per minute despite adequate ven-tilation (usually with endotracheal in-tubation) with 100% oxygen and chestcompressions, administration of epi-nephrine or volume expansion, or both,may be indicated. Rarely, buffers, anarcotic antagonist, or vasopressorsmay be useful after resuscitation, butthese are not recommended in the de-livery room.
Rate and Dose ofEpinephrine AdministrationEpinephrine is recommended to be ad-ministered intravenously (Class IIb,LOE C). Past guidelines recommendedthat initial doses of epinephrine begiven through an endotracheal tubebecause the dose can be administeredmore quickly than when an intra-venous route must be established.However, animal studies that showed apositive effect of endotracheal epi-nephrine used considerably higherdoses than are currently recommend-ed,83,84 and the one animal study thatused currently recommended dosesvia endotracheal tube showed no ef-fect.85 Given the lack of supportivedata for endotracheal epinephrine, theIV route should be used as soon as
venous access is established (ClassIIb, LOE C).
The recommended IV dose is 0.01 to0.03 mg/kg per dose. Higher IV dosesare not recommended because ani-mal86,87 and pediatric88,89 studies showexaggerated hypertension, decreasedmyocardial function, and worse neuro-logical function after administration ofIV doses in the range of 0.1 mg/kg. Ifthe endotracheal route is used, dosesof 0.01 or 0.03 mg/kg will likely be inef-fective. Therefore, IV administration of0.01 to 0.03 mg/kg per dose is the pre-ferred route. While access is being ob-tained, administration of a higher dose(0.05 to 0.1 mg/kg) through the endo-tracheal tube may be considered, butthe safety and efficacy of this prac-tice have not been evaluated (Class IIb,LOE C). The concentration of epineph-rine for either route should be 1:10,000(0.1 mg/mL).
VOLUME EXPANSIONVolume expansion should be consid-ered when blood loss is known or sus-pected (pale skin, poor perfusion, weakpulse) and the baby’s heart rate hasnot responded adequately to other re-suscitative measures (Class IIb, LOE C).90
An isotonic crystalloid solution orblood is recommended for volume ex-pansion in the delivery room (Class IIb,LOE C). The recommended dose is 10mL/kg, whichmay need to be repeated.When resuscitating premature infants,care should be taken to avoid givingvolume expanders rapidly, becauserapid infusions of large volumes havebeen associated with intraventricularhemorrhage (Class IIb, LOE C).
POSTRESUSCITATION CAREBabies who require resuscitation areat risk for deterioration after their vi-tal signs have returned to normal.Once adequate ventilation and circula-tion have been established, the infantshould be maintained in, or trans-ferred to an environment where close
monitoring and anticipatory care canbe provided.
NaloxoneAdministration of naloxone is not rec-ommended as part of initial resuscita-tive efforts in the delivery room fornewborns with respiratory depression.Heart rate and oxygenation should berestored by supporting ventilation.
GlucoseNewborns with lower blood glucoselevels are at increased risk for braininjury and adverse outcomes after ahypoxic-ischemic insult, although nospecific glucose level associated withworse outcome has been identified.91,92
Increased glucose levels after hypoxiaor ischemia were not associated withadverse effects in a recent pediatricseries93 or in animal studies,94 and theymay be protective.95 However, thereare no randomized controlled trialsthat examine this question. Due to thepaucity of data, no specific target glu-cose concentration range can be iden-tified at present. Intravenous glucoseinfusion should be considered as soonas practical after resuscitation, withthe goal of avoiding hypoglycemia(Class IIb, LOE C).
Induced Therapeutic HypothermiaSeveral randomized controlled multi-center trials of induced hypothermia(33.5°C to 34.5°C) of newborns �36weeks gestational age, with moderateto severe hypoxic-ischemic encepha-lopathy as defined by strict criteria,showed that those babies who werecooled had significantly lower mortal-ity and less neurodevelopmental dis-ability at 18-month follow-up than ba-bies who were not cooled.96–98 Therandomized trials produced similarresults using different methods ofcooling (selective head versus system-ic).96–100 It is recommended that infantsborn at �36 weeks gestation withevolving moderate to severe hypoxic-ischemic encephalopathy should be
e1406 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

offered therapeutic hypothermia. Thetreatment should be implemented ac-cording to the studied protocols, whichcurrently includecommencementwithin6 hours following birth, continuation for72 hours, and slow rewarming over atleast 4 hours. Therapeutic hypothermiashould be administered under clearlydefined protocols similar to those usedin published clinical trials and in facili-ties with the capabilities for multidisci-plinary care and longitudinal follow-up(Class IIa, LOE A). Studies suggest thatthere may be some associated adverseeffects, such as thrombocytopenia andincreased need for inotropic support.
GUIDELINES FOR WITHHOLDINGAND DISCONTINUINGRESUSCITATIONFor neonates at themargins of viabilityor those with conditions which predicta high risk of mortality or morbidity,attitudes and practice vary accordingto region and availability of resources.Studies indicate that parents desire alarger role in decisions to initiate re-suscitation and continue life supportof severely compromised newborns.Opinions among neonatal providersvary widely regarding the benefits anddisadvantages of aggressive therapiesin such newborns.
Withholding ResuscitationIt is possible to identify conditions as-sociated with high mortality and pooroutcome in which withholding resusci-tative efforts may be considered rea-sonable, particularly when there hasbeen the opportunity for parentalagreement (Class IIb, LOE C101,102).
A consistent and coordinated ap-proach to individual cases by the ob-stetric and neonatal teams and theparents is an important goal. Nonini-tiation of resuscitation and discontinu-ation of life-sustaining treatment dur-ing or after resuscitation are ethicallyequivalent, and clinicians should nothesitate to withdraw support when
functional survival is highly unlikely.103
The following guidelines must be inter-preted according to current regionaloutcomes:
● When gestation, birth weight, orcongenital anomalies are associ-ated with almost certain early deathand when unacceptably high mor-bidity is likely among the rare survi-vors, resuscitation is not indicated.Examples include extreme prematu-rity (gestational age �23 weeks orbirth weight �400 g), anencephaly,and some major chromosomal ab-normalities, such as trisomy 13(Class IIb, LOE C).
● In conditions associated with a highrate of survival and acceptable mor-bidity, resuscitation is nearly al-ways indicated. This will generallyinclude babies with gestational age�25 weeks and those with mostcongenital malformations (Class IIb,LOE C).
● In conditions associated with uncer-tain prognosis in which survival isborderline, the morbidity rate is rel-atively high, and the anticipatedburden to the child is high, parentaldesires concerning initiation of re-suscitation should be supported(Class IIb, LOE C).
Assessment of morbidity andmortalityrisks should take into considerationavailable data, and may be augmentedby use of published tools based ondata from specific populations. Deci-sions should also take into accountchanges in medical practice that mayoccur over time.
Mortality and morbidity data by gesta-tional age compiled from data col-lected by perinatal centers in the USand several other countries may befound on the Neonatal ResuscitationProgram (NRP) website (www.aap.org/nrp). A link to a computerized toolto estimate mortality and morbidityfrom a population of extremely low-
birth-weight babies born in a networkof regional perinatal centers may befound at that site. However, unless con-ception occurred via in vitro fertiliza-tion, techniques used for obstetric dat-ing are accurate to only�3 to 4 days ifapplied in the first trimester and toonly�1 to 2 weeks subsequently. Esti-mates of fetal weight are accurate toonly�15% to 20%. Even small discrep-ancies of 1 or 2 weeks between esti-mated and actual gestational age or a100- to 200-g difference in birth weightmay have implications for survival andlong-term morbidity. Also, fetal weightcan be misleading if there has beenintrauterine growth restriction, andoutcomes may be less predictable.These uncertainties underscore theimportance of not making firm com-mitments about withholding or provid-ing resuscitation until you have the op-portunity to examine the baby afterbirth.
Discontinuing Resuscitative EffortsIn a newly born baby with no detect-able heart rate, it is appropriate toconsider stopping resuscitation if theheart rate remains undetectable for 10minutes (Class IIb, LOE C104–106). The de-cision to continue resuscitation effortsbeyond 10 minutes with no heart rateshould take into consideration factorssuch as the presumed etiology of thearrest, the gestation of the baby, thepresence or absence of complications,the potential role of therapeutic hypo-thermia, and the parents’ previouslyexpressed feelings about acceptablerisk of morbidity.
STRUCTURE OF EDUCATIONALPROGRAMS TO TEACHNEONATAL RESUSCITATIONStudies have demonstrated that use ofsimulation-based learning methodolo-gies enhances performance in bothreal-life clinical situations and simu-lated resuscitations,107–110 although afew studies have found no differences
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1407
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

when compared to standard or othernonsimulated training.111,112 Also, stud-ies examining briefings or debriefingsof resuscitation team performancehave generally shown improved knowl-edge or skills.113–118 Interpretation of
data is complicated by the hetero-geneity and limitations of the studies,including a paucity of data aboutclinical outcomes. Based on availableevidence, it is recommended that theAAP/AHA Neonatal Resuscitation Pro-
gram adopt simulation, briefing, anddebriefing techniques in designing aneducation program for the acquisitionand maintenance of the skills neces-sary for effective neonatal resuscita-tion (Class IIb, LOE C).
REFERENCES
1. 2010 International Consensus on Cardio-pulmonary Resuscitation and EmergencyCardiovascular Care Science with Treat-ment Recommendations. Circulation.In Press
2. Perlman JM, Risser R. Cardiopulmonaryresuscitation in the delivery room: associ-ated clinical events. Arch Pediatr AdolescMed. 1995;149:20–25
3. Barber CA, Wyckoff MH. Use and efficacy ofendotracheal versus intravenous epi-nephrine during neonatal cardiopulmo-nary resuscitation in the delivery room.Pediatrics. 2006;118:1028–1034
4. Owen CJ, Wyllie JP. Determination of heartrate in the baby at birth. Resuscitation.2004;60:213–217
5. Kamlin CO, Dawson JA, O’Donnell CP, Mor-ley CJ, Donath SM, Sekhon J, Davis PG. Ac-curacy of pulse oximetry measurement ofheart rate of newborn infants in the deliv-ery room. J Pediatr. 2008;152:756–760
6. Am Academy of Pediatrics, Am College ofObstetricians and Gynecologists. In: Lock-wood C, Lemons J, eds. Guidelines for Peri-natal Care. 6th ed. Elk Grove Village, IL: AmAcademy of Pediatrics;2007:205
7. Annibale DJ, Hulsey TC, Wagner CL, South-gate WM. Comparative neonatal morbidityof abdominal and vaginal deliveries afteruncomplicated pregnancies. Arch PediatrAdolesc Med. 1995;149:862–867
8. Atherton N, Parsons SJ, Mansfield P. Atten-dance of paediatricians at elective Caesar-ean sections performed under regionalanaesthesia: is it warranted? J PaediatrChild Health. 2006;42:332–336
9. Gordon A, McKechnie EJ, Jeffery H. Pediat-ric presence at cesarean section: justifiedor not? Am J Obstet Gynecol. 2005;193(3 Pt1):599–605
10. Parsons SJ, Sonneveld S, Nolan T. Is a pae-diatrician needed at all Caesarean sec-tions? J Paediatr Child Health. 1998;34:241–244
11. Kattwinkel J, ed. Textbook of Neonatal Re-suscitation. 6th ed. Elk Grove Village: AmAcademy of Pediatrics; In Press
12. Cramer K, Wiebe N, Hartling L, Crumley E,Vohra S. Heat loss prevention: a system-atic review of occlusive skin wrap for pre-
mature neonates. J Perinatol. 2005;25:763–769
13. Kent AL, Williams J. Increasing ambient op-erating theatre temperature and wrap-ping in polyethylene improves admissiontemperature in premature infants. J Pae-diatr Child Health. 2008;44:325–331
14. Vohra S, Frent G, Campbell V, Abbott M,Whyte R. Effect of polyethylene occlusiveskin wrapping on heat loss in very lowbirth weight infants at delivery: a random-ized trial. J Pediatr. 1999;134:547–551
15. Vohra S, Roberts RS, Zhang B, Janes M,Schmidt B. Heat Loss Prevention (HeLP) inthe delivery room: A randomized con-trolled trial of polyethylene occlusive skinwrapping in very preterm infants. J Pedi-atr. 2004;145:750–753
16. Singh A, Duckett J, Newton T, Watkinson M.Improving neonatal unit admission tem-peratures in preterm babies: exothermicmattresses, polythene bags or a tradi-tional approach? J Perinatol. 2010;30:45–49
17. Meyer MP, Bold GT. Admission tempera-tures following radiant warmer or incuba-tor transport for preterm infants �28weeks: a randomised study. Arch Dis ChildFetal Neonatal Ed. 2007;92:F295–F297
18. Petrova A, Demissie K, Rhoads GG, SmulianJC, Marcella S, Ananth CV. Association ofmaternal fever during labor with neonataland infant morbidity and mortality. ObstetGynecol. 2001;98:20–27
19. Lieberman E, Lang J, Richardson DK, Frigo-letto FD, Heffner LJ, Cohen A. Intrapartummaternal fever and neonatal outcome. Pe-diatrics. 2000;105(1 Pt 1):8–13
20. Coimbra C, Boris-Moller F, Drake M, Wie-loch T. Diminished neuronal damage in therat brain by late treatment with the anti-pyretic drug dipyrone or cooling followingcerebral ischemia. Acta Neuropathol.1996;92:447–453
21. Gungor S, Kurt E, Teksoz E, Goktolga U, Cey-han T, Baser I. Oronasopharyngeal suctionversus no suction in normal and term in-fants delivered by elective cesareansection: a prospective randomized con-trolled trial. Gynecol Obstet Invest. 2006;61:9–14
22. Waltman PA, Brewer JM, Rogers BP, MayWL. Building evidence for practice: a pilotstudy of newborn bulb suctioning at birth.J Midwifery Womens Health. 2004;49:32–38
23. Perlman JM, Volpe JJ. Suctioning in thepreterm infant: effects on cerebral bloodflow velocity, intracranial pressure, andarterial blood pressure. Pediatrics. 1983;72:329–334
24. Simbruner G, Coradello H, Fodor M, Hav-elec L, Lubec G, Pollak A. Effect of trachealsuction on oxygenation, circulation, andlung mechanics in newborn infants. ArchDis Child. 1981;56:326–330
25. Prendiville A, Thomson A, Silverman M. Ef-fect of tracheobronchial suction on respi-ratory resistance in intubated preterm ba-bies. Arch Dis Child. 1986;61:1178–1183
26. Vain NE, Szyld EG, Prudent LM, Wiswell TE,Aguilar AM, Vivas NI. Oropharyngeal andnasopharyngeal suctioning of meconium-stained neonates before delivery of theirshoulders: multicentre, randomised con-trolled trial. Lancet. 2004;364:597–602
27. Wiswell TE, Gannon CM, Jacob J, GoldsmithL, Szyld E, Weiss K, Schutzman D, Cleary GM,Filipov P, Kurlat I, Caballero CL, Abassi S,Sprague D, Oltorf C, Padula M. Deliveryroom management of the apparently vig-orous meconium-stained neonate: resultsof the multicenter, international collabo-rative trial. Pediatrics. 2000;105(1 Pt 1):1–7
28. Rossi EM, Philipson EH, Williams TG, KalhanSC. Meconium aspiration syndrome: intra-partum and neonatal attributes. Am J Ob-stet Gynecol. 1989;161:1106–1110
29. Usta IM, Mercer BM, Sibai BM. Risk factorsfor meconium aspiration syndrome. Ob-stet Gynecol. 1995;86:230–234
30. Gupta V, Bhatia BD, Mishra OP. Meconiumstained amniotic fluid: antenatal, intrapar-tum and neonatal attributes. Indian Pedi-atr. 1996;33:293–297
31. Al Takroni AM, Parvathi CK, Mendis KB, Has-san S, Reddy I, Kudair HA. Selective tra-cheal suctioning to prevent meconium as-piration syndrome. Int J Gynaecol Obstet.1998;63:259–263
32. Carson BS, Losey RW, Bowes WA, Jr, Sim-
e1408 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

mons MA. Combined obstetric and pediat-ric approach to prevent meconium aspira-tion syndrome. Am J Obstet Gynecol. 1976;126:712–715
33. Ting P, Brady JP. Tracheal suction in meco-nium aspiration. Am J Obstet Gynecol.1975;122:767–771
34. Gregory GA, Gooding CA, Phibbs RH, TooleyWH. Meconium aspiration in infants—aprospective study. J Pediatr. 1974;85:848–852
35. Toth B, Becker A, Seelbach-Gobel B. Oxygensaturation in healthy newborn infants im-mediately after birth measured by pulseoximetry. Arch Gynecol Obstet. 2002;266:105–107
36. Gonzales GF, Salirrosas A. Arterial oxygensaturation in healthy newborns deliveredat term in Cerro de Pasco (4340 m) andLima (150 m). Reprod Biol Endocrinol.2005;3:46
37. Altuncu E, Ozek E, Bilgen H, Topuzoglu A,Kavuncuoglu S. Percentiles of oxygen sat-urations in healthy term newborns in thefirst minutes of life. Eur J Pediatr. 2008;167:687–688
38. Kamlin CO, O’Donnell CP, Davis PG, MorleyCJ. Oxygen saturation in healthy infantsimmediately after birth. J Pediatr. 2006;148:585–589
39. Mariani G, Dik PB, Ezquer A, Aguirre A, Es-teban ML, Perez C, Fernandez Jonusas S,Fustinana C. Pre-ductal and post-ductal O2saturation in healthy term neonates afterbirth. J Pediatr. 2007;150:418–421
40. Rabi Y, Yee W, Chen SY, Singhal N. Oxygensaturation trends immediately after birth.J Pediatr. 2006;148:590–594
41. Hay WW, Jr, Rodden DJ, Collins SM, MelaraDL, Hale KA, Fashaw LM. Reliability ofconventional and new pulse oximetry inneonatal patients. J Perinatol. 2002;22:360–366
42. O’Donnell CP, Kamlin CO, Davis PG, MorleyCJ. Feasibility of and delay in obtainingpulse oximetry during neonatal resuscita-tion. J Pediatr. 2005;147:698–699
43. Dawson JA, Kamlin CO, Wong C, te Pas AB,O’Donnell CP, Donath SM, Davis PG, MorleyCJ. Oxygen saturation and heart rate dur-ing delivery room resuscitation of infants�30 weeks’ gestation with air or 100% ox-ygen. Arch Dis Child Fetal Neonatal Ed.2009;94:F87–F91
44. Davis PG, Tan A, O’Donnell CP, Schulze A.Resuscitation of newborn infants with100% oxygen or air: a systematic reviewand meta-analysis. Lancet. 2004;364:1329–1333
45. Rabi Y, Rabi D, Yee W. Room air resuscita-
tion of the depressed newborn: a system-atic review and meta-analysis. Resuscita-tion. 2007;72:353–363
46. Escrig R, Arruza L, Izquierdo I, Villar G,Saenz P, Gimeno A, Moro M, Vento M.Achievement of targeted saturation valuesin extremely low gestational age neonatesresuscitated with low or high oxygenconcentrations: a prospective, random-ized trial. Pediatrics. 2008;121:875–881
47. Karlberg P, Koch G. Respiratory studies innewborn infants. III. Development of me-chanics of breathing during the first weekof life. A longitudinal study. Acta Paediatr.1962;(Suppl 135):121–129
48. Vyas H, Milner AD, Hopkin IE, Boon AW.Physiologic responses to prolonged andslow-rise inflation in the resuscitation ofthe asphyxiated newborn infant. J Pediatr.1981;99:635–639
49. Vyas H, Field D, Milner AD, Hopkin IE. Deter-minants of the first inspiratory volumeand functional residual capacity at birth.Pediatr Pulmonol. 1986;2:189–193
50. Boon AW, Milner AD, Hopkin IE. Lung expan-sion, tidal exchange, and formation of thefunctional residual capacity during resus-citation of asphyxiated neonates. J Pedi-atr. 1979;95:1031–1036
51. Hillman NH, Moss TJ, Kallapur SG, Bachur-ski C, Pillow JJ, Polglase GR, Nitsos I,Kramer BW, Jobe AH. Brief, large tidal vol-ume ventilation initiates lung injury and asystemic response in fetal sheep. Am J Re-spir Crit Care Med. 2007;176:575–581
52. Polglase GR, Hooper SB, Gill AW, Allison BJ,McLean CJ, Nitsos I, Pillow JJ, Kluckow M.Cardiovascular and pulmonary conse-quences of airway recruitment in pretermlambs. J Appl Physiol. 2009;106:1347–1355
53. Dawes GS. Foetal and Neonatal Physiology.A Comparative Study of the Changes atBirth. Chicago: Year Book Medical Publish-ers, Inc; 1968
54. Lindner W, Vossbeck S, Hummler H,Pohlandt F. Delivery room management ofextremely low birth weight infants: spon-taneous breathing or intubation? Pediat-rics. 1999;103(5 Pt 1):961–967
55. Leone TA, Lange A, RichW, Finer NN. Dispos-able colorimetric carbon dioxide detectoruse as an indicator of a patent airway dur-ing noninvasive mask ventilation. Pediat-rics. 2006;118:e202–204
56. Finer NN, Rich W, Wang C, Leone T. Airwayobstruction during mask ventilation ofvery low birth weight infants during neo-natal resuscitation. Pediatrics. 2009;123:865–869
57. Morley CJ, Davis PG, Doyle LW, Brion LP,
Hascoet JM, Carlin JB. Nasal CPAP or intu-bation at birth for very preterm infants.N Engl J Med. 2008;358:700–708
58. Kelm M, Proquitte H, Schmalisch G, RoehrCC. Reliability of two common PEEP-generating devices used in neonatal re-suscitation. Klin Padiatr . 2009;221:415–418
59. Morley CJ, Dawson JA, Stewart MJ, Hus-sain F, Davis PG. The effect of a PEEP valveon a Laerdal neonatal self-inflating resus-citation bag. J Paediatr Child Health.46(1–2):51–56, 2010
60. Oddie S, Wyllie J, Scally A. Use of self-inflating bags for neonatal resuscitation.Resuscitation. 2005;67:109–112
61. Hussey SG, Ryan CA, Murphy BP. Compari-son of threemanual ventilation devices us-ing an intubated mannequin. Arch Dis ChildFetal Neonatal Ed. 2004;89:F490–493
62. Finer NN, Rich W, Craft A, Henderson C.Comparison of methods of bag and maskventilation for neonatal resuscitation. Re-suscitation. 2001;49:299–305
63. Bennett S, Finer NN, Rich W, Vaucher Y. Acomparison of three neonatal resuscitationdevices. Resuscitation. 2005;67:113–118
64. Kattwinkel J, Stewart C, Walsh B, Gurka M,Paget-Brown A. Responding to compliancechanges in a lung model during manualventilation: perhaps volume, rather thanpressure, should be displayed. Pediatrics.2009;123:e465–470
65. Trevisanuto D, Micaglio M, Pitton M, Maga-rotto M, Piva D, Zanardo V. Laryngeal maskairway: is themanagement of neonates re-quiring positive pressure ventilation atbirth changing? Resuscitation. 2004;62:151–157
66. Gandini D, Brimacombe JR. Neonatal re-suscitation with the laryngeal mask air-way in normal and low birth weight in-fants. Anesth Analg. 1999;89:642–643
67. Esmail N, Saleh M, et al. Laryngeal maskairway versus endotracheal intubation forApgar score improvement in neonatal re-suscitation. Egyptian Journal of Anesthesi-ology. 2002;18:115–121
68. Hosono S, Inami I, Fujita H, Minato M, Taka-hashi S, Mugishima H. A role of end-tidalCO monitoring for assessment of trachealintubations in very low birth weight in-fants during neonatal resuscitation atbirth. J Perinat Med. 2009;37:79–84
69. Repetto JE, Donohue P-CP, Baker SF, Kelly L,Nogee LM. Use of capnography in the deliv-ery room for assessment of endotrachealtube placement. J Perinatol. 2001;21:284–287
70. Roberts WA, Maniscalco WM, Cohen AR,
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1409
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

Litman RS, Chhibber A. The use of capnog-raphy for recognition of esophageal intu-bation in the neonatal intensive care unit.Pediatr Pulmonol. 1995;19:262–268
71. Aziz HF, Martin JB, Moore JJ. The pediatricdisposable end-tidal carbon dioxide detec-tor role in endotracheal intubation in new-borns. J Perinatol. 1999;19:110–113
72. Garey DM, Ward R, Rich W, Heldt G, Leone T,Finer NN. Tidal volume threshold for color-imetric carbon dioxide detectors availablefor use in neonates. Pediatrics. 2008;121:e1524–1527
73. Orlowski JP. Optimum position for exter-nal cardiac compression in infants andyoung children. Ann Emerg Med. 1986;15:667–673
74. Phillips GW, Zideman DA. Relation of infantheart to sternum: its significance in car-diopulmonary resuscitation. Lancet. 1986;1:1024–1025
75. Braga MS, Dominguez TE, Pollock AN, NilesD, Meyer A, Myklebust H, Nysaether J, Nad-karni V. Estimation of optimal CPR chestcompression depth in children by usingcomputer tomography. Pediatrics. 2009;124:e69–e74
76. Menegazzi JJ, Auble TE, Nicklas KA, HosackGM, Rack L, Goode JS. Two-thumb versustwo-finger chest compression during CRPin a swine infant model of cardiac arrest.Ann Emerg Med. 1993;22:240–243
77. Houri PK, Frank LR, Menegazzi JJ, Taylor R.A randomized, controlled trial of two-thumb vs two-finger chest compression ina swine infant model of cardiac arrest.Prehosp Emerg Care. 1997;1:65–67
78. Udassi JP, Udassi S, Theriaque DW, Shus-ter JJ, Zaritsky AL, Haque IU. Effect of alter-native chest compression techniques ininfant and child on rescuer performance.Pediatr Crit Care Med. 2009;10:328–333
79. David R. Closed chest cardiac massage inthe newborn infant. Pediatrics. 1988;81:552–554
80. Thaler MM, Stobie GH. An improved tech-nique of external caridac compression ininfants and young children. N Engl J Med.1963;269:606–610
81. Berkowitz ID, Chantarojanasiri T, KoehlerRC, Schleien CL, Dean JM, Michael JR, Rog-ers MC, Traystman RJ. Blood flow duringcardiopulmonary resuscitation with simul-taneous compression and ventilation in in-fant pigs. Pediatr Res. 1989;26:558–564
82. Kitamura T, Iwami T, Kawamura T, Nagao K,Tanaka H, Nadkarni VM, Berg RA, Hiraide A.Conventional and chest-compression-onlycardiopulmonary resuscitation by by-standers for children who have out-of-
hospital cardiac arrests: a prospective,nationwide, population-based cohortstudy. Lancet. 2010;375:1347–1354
83. Mielke LL, Frank C, Lanzinger MJ, WilhelmMG, Entholzner EK, Hargasser SR, Hipp RF.Plasma catecholamine levels followingtracheal and intravenous epinephrine ad-ministration in swine. Resuscitation. 1998;36:187–192
84. Roberts JR, Greenberg MI, Knaub MA,Kendrick ZV, Baskin SI. Blood levels follow-ing intravenous and endotracheal epi-nephrine administration. JACEP. 1979;8:53–56
85. Hornchen U, Schuttler J, Stoeckel H, Eich-elkraut W, Hahn N. Endobronchial instilla-tion of epinephrine during cardiopulmo-nary resuscitation. Crit Care Med. 1987;15:1037–1039
86. Berg RA, Otto CW, Kern KB, Hilwig RW, Sand-ers AB, Henry CP, Ewy GA. A randomized,blinded trial of high-dose epinephrine ver-sus standard-dose epinephrine in a swinemodel of pediatric asphyxial cardiac ar-rest. Crit Care Med. 1996;24:1695–1700
87. Burchfield DJ, Preziosi MP, Lucas VW, FanJ. Effects of graded doses of epinephrineduring asphxia-induced bradycardia innewborn lambs. Resuscitation. 1993;25:235–244
88. Perondi MB, Reis AG, Paiva EF, NadkarniVM, Berg RA. A comparison of high-doseand standard-dose epinephrine in chil-dren with cardiac arrest. N Engl J Med.2004;350:1722–1730
89. Patterson MD, Boenning DA, Klein BL,Fuchs S, Smith KM, Hegenbarth MA, Carl-son DW, Krug SE, Harris EM. The use ofhigh-dose epinephrine for patients without-of-hospital cardiopulmonary arrestrefractory to prehospital interventions.Pediatr Emerg Care. 2005;21:227–237
90. Wyckoff MH, Perlman JM, Laptook AR. Useof volume expansion during delivery roomresuscitation in near-term and term in-fants. Pediatrics. 2005;115:950–955
91. SalhabWA,WyckoffMH, Laptook AR, PerlmanJM. Initial hypoglycemia and neonatal braininjury in term infants with severe fetal aci-demia. Pediatrics. 2004;114:361–366
92. Ondoa-Onama C, Tumwine JK. Immediateoutcome of babies with low Apgar score inMulago Hospital, Uganda. East Afr Med J.2003;80:22–29
93. Klein GW, Hojsak JM, Schmeidler J, Rapa-port R. Hyperglycemia and outcome in thepediatric intensive care unit. J Pediatr.2008;153:379–384
94. LeBlanc MH, Huang M, Patel D, Smith EE,Devidas M. Glucose given after hypoxic is-
chemia does not affect brain injury in pig-lets. Stroke. 25:1443–1447, 1994; discus-sion 1448
95. Hattori H, Wasterlain CG. Posthypoxic glu-cose supplement reduces hypoxic-ische-mic brain damage in the neonatal rat. AnnNeurol. 1990;28:122–128
96. Gluckman PD, Wyatt JS, Azzopardi D, Bal-lard R, Edwards AD, Ferriero DM, Polin RA,Robertson CM, Thoresen M, Whitelaw A,Gunn AJ. Selective head cooling with mildsystemic hypothermia after neonatalencephalopathy: multicentre randomisedtrial. Lancet. 2005;365:663–670
97. Shankaran S, Laptook AR, Ehrenkranz RA,Tyson JE, McDonald SA, Donovan EF, Fan-aroff AA, Poole WK, Wright LL, Higgins RD,Finer NN, Carlo WA, Duara S, Oh W, CottenCM, Stevenson DK, Stoll BJ, Lemons JA,Guillet R, Jobe AH. Whole-body hypother-mia for neonates with hypoxic-ischemicencephalopathy. N Engl J Med. 2005;353:1574–1584
98. Azzopardi DV, Strohm B, Edwards AD, DyetL, Halliday HL, Juszczak E, Kapellou O, Lev-ene M, Marlow N, Porter E, Thoresen M,Whitelaw A, Brocklehurst P. Moderate hy-pothermia to treat perinatal asphyxial en-cephalopathy. N Engl J Med. 2009;361:1349–1358
99. Eicher DJ, Wagner CL, Katikaneni LP, Hul-sey TC, Bass WT, Kaufman DA, Horgan MJ,Languani S, Bhatia JJ, Givelichian LM, San-karan K, Yager JY. Moderate hypothermiain neonatal encephalopathy: safety out-comes. Pediatr Neurol. 2005;32:18–24
100. Lin ZL, Yu HM, Lin J, Chen SQ, Liang ZQ,Zhang ZY. Mild hypothermia via selectivehead cooling as neuroprotective therapyin term neonates with perinatal asphyxia:an experience from a single neonatal in-tensive care unit. J Perinatol. 2006;26:180–184
101. Field DJ, Dorling JS, Manktelow BN, DraperES. Survival of extremely premature ba-bies in a geographically defined population:prospective cohort study of 1994–9 com-pared with 2000 –5. BMJ . 2008;336:1221–1223
102. Tyson JE, Parikh NA, Langer J, Green C, Hig-gins RD. Intensive care for extremeprematurity–moving beyond gestationalage. N Engl J Med. 2008;358:1672–1681
103. Paris JJ. What standards apply to resusci-tation at the borderline of gestational age?J Perinatol. 2005;25:683–684
104. Jain L, Ferre C, Vidyasagar D, Nath S, Shef-tel D. Cardiopulmonary resuscitation ofapparently stillborn infants: survival andlong-term outcome. J Pediatr. 1991;118:778–782
e1410 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

105. Casalaz DM, Marlow N, Speidel BD. Out-come of resuscitation following unex-pected apparent stillbirth. Arch Dis ChildFetal Neonatal Ed. 1998;78:F112–F115
106. Laptook AR, Shankaran S, Ambalavanan N,Carlo WA, McDonald SA, Higgins RD, Das A.Outcome of term infants using apgarscores at 10 minutes following hypoxic-is-chemic encephalopathy. Pediatrics. 2009;124:1619–1626
107. KnudsonMM, Khaw L, BullardMK, Dicker R,Cohen MJ, Staudenmayer K, Sadjadi J,Howard S, Gaba D, Krummel T. Traumatraining in simulation: translating skillsfrom SIM time to real time. J Trauma. 64:255–263, 2008; discussion 263–254
108. Wayne DB, Didwania A, Feinglass J, FudalaMJ, Barsuk JH, McGaghie WC. Simulation-based education improves quality of careduring cardiac arrest team responses atan academic teaching hospital: a case-control study. Chest. 2008;133:56–61
109. Kory PD, Eisen LA, Adachi M, Ribaudo VA,Rosenthal ME, Mayo PH. Initial airwayman-agement skills of senior residents: simula-
tion training compared with traditionaltraining. Chest. 2007;132:1927–1931
110. Schwid HA, Rooke GA, Michalowski P, RossBK. Screen-based anesthesia simulationwith debriefing improves performance ina mannequin-based anesthesia simulator.Teach Learn Med. 2001;13:92–96
111. Shapiro MJ, Morey JC, Small SD, LangfordV, Kaylor CJ, Jagminas L, Suner S, Salis-bury ML, Simon R, Jay GD. Simulationbased teamwork training for emergencydepartment staff: does it improve clinicalteamperformancewhen added to an exist-ing didactic teamwork curriculum? QualSaf Health Care. 2004;13:417–421
112. Cherry RA, Williams J, George J, Ali J. Theeffectiveness of a human patient simula-tor in the ATLS shock skills station. J SurgRes. 2007;139:229–235
113. Savoldelli GL, Naik VN, Park J, Joo HS, ChowR, Hamstra SJ. Value of debriefing duringsimulated crisis management: oral versusvideo-assisted oral feedback. Anesthesiol-ogy. 2006;105:279–285
114. Edelson DP, Litzinger B, Arora V, Walsh D,Kim S, Lauderdale DS, Vanden Hoek TL,
Becker LB, Abella BS. Improving in-hospitalcardiac arrest process and outcomeswithperformance debriefing. Arch Intern Med.2008;168:1063–1069
115. DeVita MA, Schaefer J, Lutz J, Wang H,Dongilli T. Improving medical emergencyteam (MET) performance using a novelcurriculum and a computerized humanpatient simulator. Qual Saf Health Care.2005;14:326–331
116. Wayne DB, Butter J, Siddall VJ, Fudala MJ,Linquist LA, Feinglass J, Wade LD, Mc-Gaghie WC. Simulation-based training ofinternal medicine residents in advancedcardiac life support protocols: a random-ized trial. Teach Learn Med. 2005;17:210–216
117. Clay AS, Que L, Petrusa ER, Sebastian M,Govert J. Debriefing in the intensive careunit: a feedback tool to facilitate bedsideteaching. Crit Care Med. 2007;35:738–754
118. Blum RH, Raemer DB, Carroll JS, DufresneRL, Cooper JB. A method for measuring theeffectiveness of simulation-based teamtraining for improving communicationskills. Anesth Analg. 2005;100:1375–1380
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1411
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

DISCLOSURES
GUIDELINES PART 15: Neonatal Resuscitation Writing Group DisclosuresWriting GroupMember
Employment Research Grant Other Research Support Speakers’ Bureau/ Honoraria OwnershipInterest
Consultant/ Advisory Board Other
JohnKattwinkel
University of Virginia–Professorof Pediatrics
None None None None None None
Jeffrey M.Perlman
Weill Cornell-Professor ofPediatrics
†NIH-NIH- Improving antimicrobialprescribing practices in the NICU
None None None None None
Khalid Aziz University of Alberta– AssociateProfessor of Pediatrics
None None None None None None
ChristopherColby
Mayo Clinic–physician None None None None None None
KarenFairchild
University of Virginia HealthSystem–Associate Professor of
Pediatrics
None None None None None None
JohnGallagher
Univ. Hosp of Cleveland-CritCare Coordinator of Ped.Resp
Care
None None None None None None
Mary FranHazinski
Vanderbilt University School ofNursing—Professor; AHA ECCProduct Development-Senior
Science Editor†Significant AHA compensationto write, edit and reviewdocuments such as the 2010AHA Guidelines for CPR and ECC.
None None None None None None
Louis P.Halamek
Stanford University–AssociateProfessor
†Laerdal Foundation: The LaerdalFoundation (not company)
provided a grant to the Center forAdvanced Pediatric and PerinatalEducation at Packard Children’sHospital at Stanford during theacademic years 2006–07, 2007–08,2008–09; I develop simulation-based training programs andconduct research at CAPE. Thissupport was provided directly to
my institution.
None *I have received� 10 honorariain amounts of $500 or less fromspeaking at various academicmeetings in the past 24 months;none of these meetings wereconducted by for-profit entities.
None *Laerdal Medical AdvancedMedical Simulation Both ofthese companies
reimburse me directly.
*I provide medicalconsultation to the legalprofession for which I amreimbursed directly.
PraveenKumar
PEDIATRIC FACULTY FOUNDATION-ATTENDING NEONATOLOGIST
None None None None None None
George Little Dartmouth College- Ped.Professor; Dartmouth HitchcockMedfont. Center Neonatologist
None None None None None None
Jane E.McGowan
St Christopher’s PediatricAssociate/
Tenet Healthcare–Attendingneonatologist; medical director,
NICU
None None None None None * reviewed records of casesinvolving neonatal
resuscitation on one or twooccasions over the past 5
years.*As co-editor for Textbook ofNeonatal Resuscitation 6thedition, to be published bythe AAP, being paid a totalof $4000 over 3 years by the
AAP.BarbaraNightengale
Univ.Health Assoc,NursePractitioner
None None None None None None
Mildred M.Ramirez
Univ of Texas Med SchoolHouston-Physician
None None *Signed as consultant for Cyto-kine Pharmasciences, Inc., for alecture in Mexico City. ProductPropress for cervical rippening.
$2,000 Money to Univ.
None None *Expert for Current expertcase of triplets and pretermdelivery. Money to theuniversity ’09
Steven Ringer Brigham and Women’sHospital–Chief, Newborn
Medicine
None None *Vermont Oxford NeonatalNetwork, $1000, comes to me
None *Alere $2000, consultationDey Pharamaceutical $1000Consultation ForrestPharmaceuticals $1500Grant Review Committee
†Several Attorneys, servingas expert witness in
Medical malpractice cases
Wendy M.Simon
American Academy ofPediatrics–Director, LifeSupport Programs
None None None None None None
Gary M.Weiner
St. Joseph Mercy Hospital-AnnArbor Michigan–Attending
Neonatologist
None †Received equipment on-loan(3 resuscitation mannequins,2 sets of video recordingequipment) from LaerdalMedical Corporation to beused to complete a research
project evaluatingeducational methods forteaching neonatal
resuscitation. The value of theon-loan equipment isapproximately $35,000.
None None None None
(Continued)
e1412 FROM THE AMERICAN ACADEMY OF PEDIATRICS
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

GUIDELINES PART 15: Neonatal Resuscitation Writing Group Disclosures, ContinuedWritingGroupMember
Employment Research Grant Other Research Support Speakers’ Bureau/ Honoraria OwnershipInterest
Consultant/ Advisory Board Other
MyraWyckoff
UT Southwestern MedicalCenter–Associate Professor of
Pediatrics
†American Academy of PediatricsNeonatal Research Grant-Ergonomics of Neonatal CPR
2008–2009
†Received a SimNewBneonatal simulator for help inBeta testing prior to final
production
*Speaker at Symposia onNeonatal Care from University ofMiami-honoraria paid to meSpeaker at Symposia on
Neonatal Care from Columbia/Cornell-honoraria paid directlyto me Speaker for Grand Roundsfrom University of Oklahoma-honoraria paid directly to me
None None None
JeanetteZaichkin
Seattle Children’sHospital–Neonatal Outreach
Coordinator
None None *I receive honoraria directly tome from the AAP as
compensation for editorialactivities for NRP instructor ms.
None None None
This table represents the relationships of writing groupmembers that may be perceived as actual or reasonably perceived conflicts of interest as reported on the Disclosure Questionnaire,which all members of the writing group are required to complete and submit. A relationship is considered to be “significant” if (a) the person receives $10 000 or more during any 12-monthperiod, or 5% or more of the person’s gross income; or (b) the person owns 5% or more of the voting stock or share of the entity, or owns $10 000 or more of the fair market value of theentity. A relationship is considered to be “modest” if it is less than “significant” under the preceding definition.*Modest.†Significant.
FROM THE AMERICAN ACADEMY OF PEDIATRICS
PEDIATRICS Volume 126, Number 5, November 2010 e1413
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

DOI: 10.1542/peds.2010-2972E originally published online October 18, 2010; 2010;126;e1400Pediatrics
Ringer, Wendy M. Simon, Gary M. Weiner, Myra Wyckoff and Jeanette ZaichkinGeorge Little, Jane E. McGowan, Barbara Nightengale, Mildred M. Ramirez, StevenFairchild, John Gallagher, Mary Fran Hazinski, Louis P. Halamek, Praveen Kumar,
John Kattwinkel, Jeffrey M. Perlman, Khalid Aziz, Christopher Colby, KarenCardiopulmonary Resuscitation and Emergency Cardiovascular Care
Neonatal Resuscitation: 2010 American Heart Association Guidelines for
ServicesUpdated Information &
http://pediatrics.aappublications.org/content/126/5/e1400including high resolution figures, can be found at:
References
-1http://pediatrics.aappublications.org/content/126/5/e1400.full#ref-listThis article cites 113 articles, 24 of which you can access for free at:
Subspecialty Collections
e_subhttp://classic.pediatrics.aappublications.org/cgi/collection/critical_carCritical Carefollowing collection(s): This article, along with others on similar topics, appears in the
Permissions & Licensing
https://shop.aap.org/licensing-permissions/in its entirety can be found online at: Information about reproducing this article in parts (figures, tables) or
Reprintshttp://classic.pediatrics.aappublications.org/content/reprintsInformation about ordering reprints can be found online:
. ISSN:60007. Copyright © 2010 by the American Academy of Pediatrics. All rights reserved. Print
American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,has been published continuously since . Pediatrics is owned, published, and trademarked by the Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from

Kattwinkel, et al. Special Report: Neonatal Resuscitation: 2010 American HeartAssociation Guidelines for Cardiopulmonary Resuscitation and EmergencyCardiovascular Care. Pediatrics. 2010;126(5):e1400–e1413
An error occurred in this article by Kattwinkel et al (doi:10.1542/peds.2010-2972E). On page e1401, in the figure, “Newborn Resuscitation Algorithm” it reads:“NO” between “Heart rate below 60” and “Consider intubation, Chest compres-sions, Coordinate with PPV.” This should have read: as a double pointed arrowbetween “Heart rate below 60” and “Take ventilation corrective steps” and dele-tion of the word, “no.” The corrected figure is below.
doi:10.1542/peds.2011-1260
FIGURE
E R R A T U M
176 ERRATUM

DOI: 10.1542/peds.2010-2972E originally published online October 18, 2010; 2010;126;e1400Pediatrics
Ringer, Wendy M. Simon, Gary M. Weiner, Myra Wyckoff and Jeanette ZaichkinGeorge Little, Jane E. McGowan, Barbara Nightengale, Mildred M. Ramirez, StevenFairchild, John Gallagher, Mary Fran Hazinski, Louis P. Halamek, Praveen Kumar,
John Kattwinkel, Jeffrey M. Perlman, Khalid Aziz, Christopher Colby, KarenCardiopulmonary Resuscitation and Emergency Cardiovascular Care
Neonatal Resuscitation: 2010 American Heart Association Guidelines for
http://pediatrics.aappublications.org/content/126/5/e1400located on the World Wide Web at:
The online version of this article, along with updated information and services, is
http://pediatrics.aappublications.org//content/128/1/176.full.pdf An erratum has been published regarding this article. Please see the attached page for:
. ISSN:60007. Copyright © 2010 by the American Academy of Pediatrics. All rights reserved. Print
American Academy of Pediatrics, 141 Northwest Point Boulevard, Elk Grove Village, Illinois,has been published continuously since . Pediatrics is owned, published, and trademarked by the Pediatrics is the official journal of the American Academy of Pediatrics. A monthly publication, it
by guest on May 6, 2018http://pediatrics.aappublications.org/Downloaded from