Spatial distribution of ventilation and perfusionin anesthetized dogs in lateral postures
description
Transcript of Spatial distribution of ventilation and perfusionin anesthetized dogs in lateral postures
-
Spatial distribution of ventilation and perfusionin anesthetized dogs in lateral postures
HUNG CHANG,1,5 STEPHEN J. LAI-FOOK,4 KAREN B. DOMINO,3
CARMEL SCHIMMEL,2 JACK HILDEBRANDT,1,2 H. THOMAS ROBERTSON,1,2
ROBB W. GLENNY,1,2 AND MICHAEL P. HLASTALA1,2
Departments of 1Physiology and Biophysics, 2Medicine, and 3Anesthesiology, University ofWashington, Seattle, Washington 98195; 4Center for Biomedical Engineering, University ofKentucky, Lexington, Kentucky 40506; and 5Division of Chest Surgery, Department of Surgery,Tri-Service General Hospital, National Defense Medical School, Taipei, TaiwanReceived 20 April 2001; accepted in final form 17 September 2001
Chang, Hung, Stephen J. Lai-Fook, Karen B. Domino,Carmel Schimmel, Jack Hildebrandt, H. Thomas Robert-son, Robb W. Glenny, and Michael P. Hlastala. Spatialdistribution of ventilation and perfusion in anesthetized dogs inlateral postures. J Appl Physiol 92: 745762, 2002; 10.1152/japplphysiol.00377.2001.We aimed to assess the influence oflateral decubitus postures and positive end-expiratory pres-sure (PEEP) on the regional distribution of ventilation andperfusion. We measured regional ventilation (VA) and regionalblood flow (Q) in six anesthetized, mechanically ventilated dogsin the left (LLD) and right lateral decubitus (RLD) postureswith and without 10 cmH2O PEEP. Q was measured by use ofintravenously injected 15-m fluorescent microspheres, and VAwas measured by aerosolized 1-m fluorescent microspheres.Fluorescence was analyzed in lung pieces 1.7 cm3 in volume.Multiple linear regression analysis was used to evaluate three-dimensional spatial gradients of Q, VA, the ratio VA/Q, andregional PO2 (PrO2) in both lungs. In the LLD posture, a gravity-dependent vertical gradient in Q was observed in both lungs inconjunction with a reduced blood flow and PrO2 to the dependentleft lung. Change from the LLD to the RLD or 10 cmH2O PEEPincreased local VA/Q and PrO2 in the left lung and minimizedany role of hypoxia. The greatest reduction in individual lungvolume occurred to the left lung in the LLD posture. We con-clude that lung distortion caused by the weight of the heart andabdomen is greater in the LLD posture and influences both Qand VA, and ultimately gas exchange. In this respect, thesmaller left lung was the most susceptible to impaired gasexchange in the LLD posture.
pulmonary gas exchange; spatial gradients; fluorescent mi-crospheres; mediastinal shift; regional blood flow; positiveend-expiratory pressure
STUDIES (11, 33) HAVE SUGGESTED that regional blood flow(Q) and ventilation (VA) are more uniform in the pronecompared with the supine posture. This was attributedto greater Q and VA to the dorsal lung regions, offset-ting the effects of gravity. Also, the reduction in thedependent lung volume by the weight of the heart
might contribute to differences in regional perfusionand VA (3). In the lateral decubitus posture, the com-pression of the dependent lung by the heart might begreater than that in either supine or prone posture.Furthermore, the dependent lung has a smaller lungvolume in the left (LLD) than in the right lateraldecubitus (RLD) posture (35), consistent with differingeffects of the heart between the two postures.
Q increases from the nondependent to dependentlung in the lateral decubitus posture in the human (6,25, 28) and the dog (20, 37). In addition, the intrapul-monary ventilation distribution is altered in the lateralposture after anesthesia and mechanical ventilation(38, 39). Impaired gas exchange after anesthesia andmechanical ventilation has been attributed to a mis-match between ventilation and perfusion. The relativematching of pulmonary blood flow and ventilation dis-tribution in lateral decubitus postures remains uncer-tain.
Positive end-expiratory pressure (PEEP) is often ap-plied to improve arterial oxygenation during anesthe-sia with mechanical ventilation (28, 38, 39). In thelateral posture, PEEP has been shown to reduce thedifference in ventilation between the two lungs (39). Inthese studies (28, 38, 39), ventilation was measured inrelatively large regions, such as a single lobe or lung.Accordingly, direct evidence using a high spatial reso-lution measure of the VA distribution in the lateraldecubitus posture after induction of anesthesia withPEEP is lacking.
We hypothesize that the distributions of VA and Qare different between the LLD and RLD posturebecause of differences in lung distortion caused bythe weight of the heart and abdominal contents.PEEP reduces lung distortion due to heart weight,may affect the smaller left dependent lung to agreater degree, and produces a larger decrease inpulmonary vascular resistance in the LLD posture.
Address for reprint requests and other correspondence: M. P.Hlastala, Div. of Pulmonary and Critical Care Medicine, Box 356522,Univ. of Washington, Seattle, WA 98195-6522 (E-mail: [email protected]).
The costs of publication of this article were defrayed in part by thepayment of page charges. The article must therefore be herebymarked advertisement in accordance with 18 U.S.C. Section 1734solely to indicate this fact.
J Appl Physiol 92: 745762, 2002;10.1152/japplphysiol.00377.2001.
8750-7587/02 $5.00 Copyright 2002 the American Physiological Societyhttp://www.jap.org 745
-
PEEP may increase both VA and Q to dependent lungregions, particularly to the dependent left lung in theLLD posture.
This study examines the effect of posture and PEEPon Q, ventilation, and gas exchange in the lateraldecubitus posture in anesthetized, mechanically venti-lated dogs, using both aerosolized and intravenouslyinjected fluorescent microspheres.
METHODS
Animal Preparation and Physiological Measurements
This study was approved by the University of WashingtonAnimal Care Committee. Six healthy mongrel dogs of eithersex [22.8 2.8 (SD, n 6) kg] were anesthetized withpentobarbital sodium (48 mg/kg iv) and maintained witha pentobarbital infusion sufficient to achieve a surgical planeof anesthesia and eliminate spontaneous ventilation (1017 mg kg1 h1). Dogs were mechanically ventilated withair via tracheostomy [tidal volume (VT) of 15 ml/kg]. Therespiratory rate was adjusted to maintain arterial PCO2(PaCO2) between 35 and 40 Torr. Minute ventilation wasmeasured with a spirometer. Catheters were placed in onefemoral artery and both femoral veins. A pulmonary arterycatheter was introduced into the right external jugular veinand used for measuring cardiac output (QT; thermal dilution)and core temperature (Tc). Systemic arterial (Pa), pulmonaryarterial (Ppa), pulmonary capillary wedge (Ppcw), and air-way pressure (Paw) were recorded continuously on a datamanagement system (Western Graphic Mach 12 DMS 1000).For determination of anatomic dead space (VD), exhaledend-tidal PCO2 was digitally sampled with an infrared CO2detector (Perkin-Elmer, Plumsteadville, PA), and expiratoryairflow (V) was measured by pneumotachograph. Arterialand mixed venous blood gases were measured with an auto-mated blood-gas analyzer (ABL 300, Radiometer, Copenha-gen, Denmark) and corrected for temperature. Body temper-ature was maintained by using heat lamps and pads.
Study Protocol
Animals were studied in the right and left lateral decubi-tus postures with 0 or 10 cmH2O PEEP, in random order. Thelungs were fully inflated (3040 cmH2O) 5 min before eachexperimental measurement to remove atelectasis. In eachtrial, we measured Pa, Ppa, Ppcw, QT, Tc, VT, and arterialand venous blood gas composition immediately before fluo-rescent microsphere administration. Q was measured withintravenously injected microspheres, and VA was measuredwith fluorescent aerosols as described below. Functional re-sidual capacity (FRC) was measured by He dilution duringeach experimental condition.
Multiple Inert Gas Measurements
Pulmonary gas exchange was characterized and analyzedby MIGET, the multiple inert gas elimination technique (46,47). Distributions of ventilation-perfusion ratio (VA/Q) wereestimated by use of a 50-compartment model (47). Inert gasshunt (QS/QT) and dead space (VD/VT) were obtained from themodel. Data from five of six animals are presented since oneanimal was rejected because of the presence of technicalerrors.
Fluorescent-labeled Microsphere Technique
VA was measured in both the LLD and RLD posture withand without PEEP by delivering aerosolized orange, orange-
red, yellow, or yellow-green 1-m-diameter fluorescent mi-crospheres (FluoSpheres, Molecular Probes, Eugene, OR)into the ventilator circuit during a 5-min period (40). Simul-taneously, Q was measured by injecting blue-green, green,crimson, or red 15-m-diameter fluorescent microspheres viathe femoral venous catheter, in five increments over the 5min. To avoid clumping, microspheres were sonicated andvortexed before administration. Microsphere colors were ran-domly varied across experiments.
Terminally, the animals were deeply anesthetized withpentothal (150 mg/kg iv); then saline, heparin (20,000 units),and papaverine (2 mg/kg) were administered. The animalswere exsanguinated via the arterial cannula. After a mediansternotomy, the left atrium and pulmonary artery were can-nulated, the aorta was tied off, and the lungs were perfusedwith 2% dextran solution to remove the blood. The lungswere removed and dried by inflation (25 cmH2O) to totallung capacity (TLC). The pleura was pierced in several loca-tions with a needle to facilitate drying. To maintain a normalanatomic configuration, the apical and most ventrocaudalrims of the left and right lungs were joined by tissue glue.
After 7 days, the dried lungs were coated with polyure-thane foam (Kwik Foam, DAP, Dayton, OH) and placed in aplastic-lined square box with the caudal-cranial axis of thelung parallel to the wall of box. The box was filled with arapidly setting foam (Polyol and isocyanate, InternationalSales, Seattle, WA). The solid block was sliced into 1.2-cm-thick slices. With use of a miter box, the lung slices werediced into cubes with 1.2-cm sides. Each lung piece wasweighed and assigned x0, y0, and z0 coordinates measuredfrom the left, dorsal, and caudal lung edges, representing theleft-right, dorsal-ventral, and caudal-cranial axes, respec-tively. Samples 0.008 g were discarded. Fluorescent dyewas extracted by soaking each piece in 1.5 ml 2-ethoxy ethylacetate (Cellosolve, Aldrich Chemical, Milwaukee, WI) for 4days. Dye concentrations were measured with an automatedluminescence spectrophotometer (Perkin-Elmer, model LS-50B, Norwalk, CT) at the dye-specific excitation and emissionwavelength. A matrix inversion method (42) was used tocorrect the fluorescent signal spillover from adjacent colors.
Data Processing
Adjusting cube dimensions from TLC back to in situ FRCconditions. To estimate spatial gradients in blood flow andventilation per regional lung volume at the time of micro-sphere injection, the dimensions of each cube were adjustedfrom their TLC measurements to estimated in vivo valuesusing previous measurements from anesthetized dogs (20,37). In the LLD posture, the ratios of the maximum lunglengths at FRC to those at TLC measured radiographicallywere 0.68 (0.85 in RLD posture), 0.76, and 0.84 in the vertical(x), dorsal-ventral (y), and caudal-cranial (z) axis, respec-tively. Adjusted vertical heights at FRC averaged 11.1 0.9and 14.0 1.2 cm in the LLD and RLD posture, respectively,without PEEP; and 16.4 1.5 cm for both postures withPEEP. The adjusted dorsal-ventral and caudal-craniallengths averaged 13.1 1.1 and 23.9 2.3 cm, respectively.
A second adjustment was made for the nonuniform defor-mation caused by the vertical gradient in transpulmonarypressure (Ptp). At the adjusted lung height xi measured fromthe bottom of the lung, (Ptp)i is given by
PtpiGxi (1)
where G is the vertical Ptp gradient (0.5 cmH2O/cm height)measured in the lateral posture in the dog (1) and i refers tothe ith piece. (Ptp)min is 0 cmH2O at the bottom of the lung at
746 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
xmin 0 (1) and increases linearly to (Ptp)max at the top of thelung at xmax, where min and max refer to minimum andmaximum, respectively. Typically, xmax at FRC was 13 cmand (Ptp)max was 6.5 cmH2O. We used the Ptp-lung volume(PV) curve of an isolated dog lung (27) to determine thechanges in length corresponding to different values of Ptpalong the height of the lung (xi). Lung volume (Vi) at each xiis given by
Vi Vmin Vmax VminPtpi/Ptpmax (2)
where (Ptp)i is the Ptp change from the value at Vmin and(Ptp)max is the maximum change in Ptp from Vmin to Vmax.We assumed that the PV curve is linear in this Ptp range.Vmin (20% TLC) is the lung volume at (Ptp)min at the bottomof the lung xmin. Vmax (65%TLC) is the lung volume at(Ptp)max. The cube at mid-lung height (xmid), equal to (xmax
xmin)/2, is assumed to remain undistorted (u) with a cubelength equal to the value after the reduction from TLC toFRC (xu). The deformed length (xi) for the ith cube at xi isassumed to vary as V1/3, given by the PV curve, at each (Ptp)i
xi/xu Vi/Vmid1/3 (3)
Vmid equals (Vmax Vmin)/2. The cube lengths were reducedbelow and expanded above the undeformed mid-lung height.The x positions of the deformed cubes were obtained bysumming the deformed cube lengths starting from the bot-tom. The y and z dimensions of all cubes at each xi wereadjusted by multiplying the values obtained after adjustmentfrom TLC to FRC by xi/xu (Eq. 3).
We assumed no vertical Ptp gradient in the lateral positionwith PEEP (2). In addition, lung volume at 10 cmH2O PEEPwas 85% TLC; thus cube length (proportional to V1/3) was
0.95 times the cube length at TLC. Accordingly, no adjust-ment was made to the dried lung lengths at 10 cmH2O PEEP.
Volume normalization of blood flow. Fluorescent intensityof each color microsphere representing Q or VA to each piece(cube) was converted to units of blood flow (ml/min) by divid-ing the fluorescence intensity of each piece by the sum of thefluorescent intensities of all pieces and then multiplying byQT (ml/min). Q and VA of each piece were then converted tounits of milliliters per minute per unit regional lung volumeat FRC by dividing by its volume (Vi). Vi at xi was calculatedfrom its dry weight Wi, mean lung density (), and thedeformed cube length (Eq. 3)
Vi 4.7Wixi/xu3/ (4)
The term (xi/xu)3 adjusts the mean density for changesdue to the Ptp gradient. The product of Wi and 4.7, lungwet-to-dry-weight ratio (43), is the wet weight. Mean lungdensity at FRC was equal to total lung wet weight (total dryweight 4.7) divided by total lung volume at FRC (airvolume; FRC volume of tissue mass). Tissue density was 1g/ml. The measured FRC values are summarized in Table 1.Lung dry weight averaged 10.1 0.7 and 13.6 0.95 g forthe left and right lung, respectively. Left lung weight was24% smaller than right lung weight. Mean lung densityaveraged 0.14 0.02 and 0.08 0.01 g/ml at FRC and 10cmH2O PEEP, respectively.
VD was obtained by using Fowlers method (13) from theplot of exhaled CO2 concentration vs. exhaled volume. VD wasestimated by averaging results from three consecutive con-centration-volume plots. Total ventilation was calculated bymultiplying frequency by VT after subtracting VD.
Table 1. Effect of position and PEEP on physiological variables
ZEEP PEEP
LLD RLD LLD RLD
Psa, mmHg 89.89.6 81.811.1 87.910.4 7515.5Ppa, cmH2O 19.55.5 16.24.7 26.45.4 25.13.2Ppcw, cmH2O 8.62.8 6.03.9 13.04.2* 11.62.7Paw, cmH2O 9.71.2 11.31.2 20.21.7 20.81.3QT, l/min 3.71.2 3.70.7 3.70.7 3.50.8RT, cmH2O l1 min1 3.01.2 2.61.4 3.81.1 4.41.5*RL, cmH2O l1 min1 8.34.0 7.34.0 8.32.5 13.13.5*RR, cmH2O l1 min1 4.81.8 4.02.3 7.22.6 6.62.6*HR, beats/min 12919 12835 12513 12723PaO2, Torr 1118 1039 1086 11419PaCO2, Torr 364 362 393* 383A-aDO2, Torr 45 129 44 55PaO2, Torr, FMS 10311 10411 1069 1068PaCO2, Torr, FMS 354 353 373 373A-aDO2, Torr, FMS 97 74 53 52pH 7.390.05 7.330.02 7.370.03 7.340.02PvO2, Torr 48.06.9 48.05.5 47.35.4 47.05.5Hb, g/dl 10.60.8 11.20.6 9.90.7 10.82.2VT, ml 34558 34458 34168 33962VD/VT, % 32.53.4 29.25.6 33.11.6 33.24.6VE, l/min 5.91.1 5.71.1 5.90.8 5.70.5RR, breaths/min 185 174 165 174FRC, ml 625212 599215 1,009271 1,053317
Values are means SD (n 6). ZEEP, zero end-expiratory pressure; PEEP, 10 cmH2O end-expiratory pressure; LLD, left lateraldecubitus; RLD, right lateral decubitus; Psa, systemic arterial pressure; Ppa, main pulmonary artery pressure; Ppcw, pulmonary capillarywedge pressure; Paw, peak airwary pressure; QT, cardiac output; R, pulmonary vascular resistance (Ppa Ppcw)/Q ; T, total lung; L, leftlung; R, right lung; HR, heart rate; PaO2, arterial O2 tension; PaCO2, arterial CO2; FMS, microsphere predicted; A-aDO2, alveolar-arterial O2differences; PvO2, mixed venous O2 tension; Hb, blood hemoglobin; VD/VT, Fowlers dead space; VT, tidal volume; VE, minute ventilation; RR,respiratory rate; FRC, functional residual capacity. *P 0.05; P 0.01; P 0.001 compared with ZEEP in the same posture. P 0.05, compared with LLD in the same PEEP condition.
747LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
Gas exchange parameters: VA/Q and PO2. The VA/Q wasused to calculate end-capillary PO2. We used the methoddescribed by Altemeier et al. (4) to calculate arterial PO2,PCO2, alveolar-arterial O2 differences (A-aDO2), and regionalPO2 (PrO2) from the measured VA and Q fluorescent intensi-ties, Hb concentration, body temperature, and mixed venousblood gases. With the measured VA/Q for each piece, the massbalance equations for O2, CO2, and N2, end-capillary O2, andCO2 contents were solved to obtain regional alveolar PO2 andPCO2 for each piece. Regional alveolar gas tensions of eachpiece were ventilation weighted, and end-capillary gas con-tents were perfusion weighted and summed to yield mixedalveolar gas tension and mixed arterial gas content.
Statistical Analysis
Q and VA per unit regional lung volume were used for allanalyses. Values were presented as means SD. A pairedt-test was used to evaluate a difference between two groups.ANOVA was used to evaluate differences among more thantwo groups. A P value 0.05 was considered significant.
Spatial variations using multiple linear regression analy-sis. A multiple linear regression model (StatView v. 5.0.1,SAS) was used to characterize the magnitude of Q (and othervariables VA, VA/Q, and PrO2) as a linear function of therectangular coordinates, x [vertical height in the left (orright) lateral posture, left-to-right (or right-to-left) direction],y (dorsal-ventral direction), and z (caudal-cranial direction)
Q I ax by cz dxy eyz fzx gxyz (5)
We subtracted the distances of the center of mass in the x, y,and z directions from the original coordinate system used forlocating each lung cube to describe blood flow in relation tothe center of mass (x y z 0). The x, y, z coordinatedistances of the center of mass of left, right, and whole lung,relatively to the original coordinate axes (x0, y0, z0) aresummarized in the APPENDIX. The intercept (I) represents themean blood flow at the center of mass. The center of bloodflow was located near (1 cm) the center of mass. Thecoefficients (ag) and intercept in the linear equation (Eq. 6)describe the mean blood flow at an arbitrary position (x, y, z)within the lung. The coefficients a, b, and c define the bloodflow gradients with respect to the x, y, and z coordinate axes,respectively, at the center of mass. The coefficients d, e, andf describe the variation of a gradient in one coordinate axiswith respect to another axis, for example, the partial deriv-ative of Q with respect to x results in the following equationdescribing the blood flow gradient in the x direction
Q/x a dy fz gyz (6)
For y z 0 and at any x, the vertical gradient is equal tothe coefficient a. At y 0, the vertical gradient is equal to
Q/x a fz (7)
That is, it varies linearly with z, and the coefficient f is theslope of the vertical gradient in the z direction. Thus bothblood flow and blood flow gradient in any coordinate axis canbe calculated for any arbitrary position within the lung.Inclusion of the xy, xz, and yz terms avoids analyzing sepa-rate lung regions to obtain regional spatial gradients.
The regression analysis provides a P value, a measure ofthe reliability, for each constant in best-fit linear equation.The coefficient of determination (R2) represented the degreeof variability due to spatial variation.
VA/Q heterogeneity. We evaluated the heterogeneity of VA,Q and VA/Q distributions using the coefficient of variation(), the standard deviation of regional VA and Q values
divided by mean values. Variance (2) of VA/Q was computedfrom the variances of VA and Q with Pearsons correlationcoefficient (c) between VA and Q (50)
2VA/Q 2VA 2Q 2VA Q (8)
Heterogeneity in VA/Q measured by the log-normal standarddeviations (lnSDVA and lnSDQ) of VA- and Q-VA/Q distribu-tion curves was obtained from MIGET and the fluorescentmicrospheres (FMS) data.
To separate the heterogeneity in VA, Q, and VA/Q due tospatial variations from that due to other factors (residualvariation), the variance (mean summed squares) of the meansummed square of the residuals, (measured predictedvalues)/mean value (50), was obtained from the multiplelinear regression analysis. This analysis was repeated usinga fourth-order regression equation (31 terms) with terms upto third order in each coordinate and up to fourth order ineach term (xpyqzr, p q r 4). Preliminary analysisindicated no further decrease in the residual variance (orincrease in R2) with a higher order regression equation. Theresidual variance/total variance equals 1 R2, where R2 isthe adjusted coefficient of determination from the regressionanalysis.
RESULTS
Physiological Data
Table 1 summarizes the physiological data. Bodyposition and PEEP had no effect on QT, heart rate,temperature, respiration rate, pH, mixed venous PO2,and hemoglobin. PEEP decreased Psa and increasedPpa, Ppcw, and peak Paw in both LLD and RLD pos-tures. Arterial PO2 (PaO2) was greater in the LLD thanRLD posture, whereas A-aDO2 was less in the LLDthan RLD posture. The addition of PEEP increasedPaCO2 by 2 Torr in both postures. PEEP increasedFRC by 65 and 76% in the LLD and RLD postures,respectively.
QS/QT and VD/VT showed no change between theLLD (0.15 0.3 and 43.5 4.8%) and RLD (0.18 0.24 and 43.6 4.6%) postures. PEEP increased VD/VTin both the LLD (49.1 8.5%) and RLD (48.9 6.7%)postures and decreased QS/QT in the LLD (0.03 0.05%) but not the RLD (0.15 0.24%) posture. QS/QTwas similar to that measured by the FMS data. VD/VTwas greater than that measured by Fowlers method(Table 1).
Microsphere data. In total, 1,3781,654 lung piecesper animal were processed for Q and VA. We dis-carded lung pieces (135 49) with 25% pulmonaryairways and with fluorescent intensity (11 10) out-side the range of 4 SD of any of the mean values.Analysis of blood flow and ventilation was carried outon 90.4 5% of the total lung pieces. For the analysisof VA/Q and PrO2, we accepted data with the range ofmean 3 SD of ln(VA/Q). This eliminated the piecesassociated with dead space (very large VA/Q) and withshunt (very low VA/Q). The number of pieces elimi-nated averaged 3 4% of the total.
Spatial Gradients in Q, VA, VA/Q, and PrO2Multiple regression analyses revealed systematic
variations of blood flow in the three coordinates. Be-
748 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
cause the blood flow distribution described by the mul-tiple linear regression equation (Eq. 5) for each animalshowed that most (6 of 7) coefficients were significant,we used the equation to describe Q, VA, VA/Q, and PrO2for all conditions. The use of the equation was furtherjustified because R2 for the best-fit regression waslower when only terms of one or two coordinates wereincluded. The coefficients of the six animals werepooled for each condition, and the significance wastested to determine its validity in describing the bloodflow distribution. In many instances, coefficients thatwere significant in a single animal proved to be notsignificant among the six animals. Coefficients were con-sidered meaningful only if the coefficients of the sixanimals were significant. The present study showed val-ues of R2 of 0.40, indicating that 40% of the vari-ability in blood flow was attributed to spatial variations.
Significant vertical, dorsal-ventral and caudal-cra-nial spatial gradients of Q, VA, VA/Q, and PrO2 aresummarized in Table 2. The complete set of pooledcoefficients are given in Tables A2 and A3 (APPENDIX).Figure 1 shows Q plotted vs. vertical height (x coordi-nate) up the lung in the LLD and RLD postures withand without PEEP for a representative animal. Thelines represent Q vs. height (x) at the center of mass (yz 0), determined from the regression analysis. Figures2, 3, and 4 are equivalent data for VA, VA/Q, and PrO2.
Effect of Posture Without PEEP
Regional distribution of Q. As indicated by the xcoefficient (a) for the whole lung, there was a signifi-cant negative (gravity-dependent) vertical gradient(Table 2, 0.27 and 0.42 ml min1 ml1 cm1) in Qthat was greater in the RLD posture (0.42) than in
the LLD posture (0.27), implying that blood flow inthe dependent lung was less in the LLD than in theRLD posture.
A smaller blood flow in the dependent lung in theLLD than RLD posture was verified by the fact thattotal blood flow (% total) was less in the dependentleft lung (37%) than in the nondependent lung (63%)in the LLD posture but was greater in the dependentright lung (64%) than in the nondependent lung(36%) in the RLD posture (Table 3). Given the sameQT in both postures (Table 1), the fraction of the QTadjusted for tissue mass to either lung did not change withbody position.
In both left and right lung, the vertical gradients(0.60 and 0.37) observed in the LLD posture wereeliminated with body inversion to the RLD posture.These gradients represented a 70150% change in themean blood flow over the height of the lung (15 cm) or510% cm1.
In the left lung, there was a positive dorsal-ventralgradient (0.26 and 0.18) in the LLD and RLD posture,with the ventral regions having the greater blood flow.The dorsal-ventral gradient in the left lung was accom-panied with a negative caudal-cranial gradient in theLLD posture (0.18), with blood flow greatest in thecaudal regions.
Regional distribution of VA. For the whole lung, thelargest vertical gradient in VA was observed in theRLD posture (Table 2, 0.58) and occurred in conjunc-tion with a positive dorsal-ventral gradient (0.31) thatwas eliminated with inversion to the LLD posture. Inthe LLD posture, the only substantial gradient oc-curred in the dorsal-ventral direction (0.27).
Table 2. Significant* spatial gradients and intercepts of regression equation
Lung Position Intercept Vertical (a) Dorsal-Ventral (b) Caudal-Cranial (c)
Q Whole LLD 5.02.1 0.270.11 0.0790.032RLD 5.21.5 0.420.39 0.0740.049
Q Left LLD 5.82.2 0.600.40 0.260.24 0.180.11RLD 3.91.4 0.180.15
Q Right LLD 4.62.2 0.370.22RLD 5.83.8
VA Whole LLD 5.11.4 0.270.25RLD 5.51.4 0.580.34 0.310.25
VA Left LLD 4.61.8 0.410.22RLD 3.20.9 0.200.16 0.270.20
VA Right LLD 5.51.7 0.500.21RLD 6.92.3 0.640.58
VA/Q Whole LLD 1.210.50RLD 1.080.43 0.0350.02
VA/Q Left LLD 0.920.38 0.0530.03RLD 1.020.53
VA/Q Right LLD 1.400.6RLD 1.090.39 0.0350.022
PrO2 Whole LLD 113.46.7 1.301.2 1.150.89 0.500.26RLD 111.38.7 1.430.73
PrO2 Left LLD 104.912 2.802.60 0.850.67RLD 109.212 1.981.70
PrO2 Right LLD 118.64.3RLD 112.67.3
Values are means SD (n 6). Q, perfusion; VA, ventilation; PrO2, regional PO2. *P 0.05, compared with zero by 1-tailed t-test.Equation: Variable I ax by cz dxy eyz fzx gxyz. All intercepts are significant.
749LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
Similar to the behavior in QT, total ventilation wassmaller in the dependent lung than in the nondepen-dent lung in the LLD posture but larger in the depen-dent lung in the RLD posture (Table 3). For constantventilation in both postures, body position had no effecton ventilation in either lung. In the left lung in theRLD posture, significant vertical (0.20) and dorsal-ventral (0.27) gradients were observed.
Relationship between regional and total blood flowand ventilation for each lung. The vertical gradients inQ and VA (Table 2) measured in this study mightappear at first sight to be at odds with the total bloodflow and ventilation values measured for each lung(Table 3). For the whole lung, the vertical gradient in Qin the LLD posture would suggest a greater blood flowin the dependent lung than in the nondependent lung(Table 2). On the other hand, the total blood flow to thedependent left lung in the LLD posture was clearlylower than that to the nondependent lung. This appar-ent discrepancy is due to the fact that the total bloodflow to the lung is the product of the mean regional Qand the total lung volume. This relationship allowed theestimate of FRC to each lung. The smallest FRC waspredicted to occur in the left lung in the LLD posture.
In the LLD posture, mean Q (Table A2) averaged 5.8and 4.6 ml min1 ml1 in the left and right lungpieces, respectively. QT (3.6 l/min) was distributed 1.3
l/min (37%) to the left lung and 2.3 l/min (67%) to theright lung (Table 3). Thus the estimated FRC was 220ml in the left lung and 500 ml in the right lung,resulting in a total FRC of 720 ml. This value was closeto the measured value (758 ml) equal to the air volume(645 ml, Table 1) and wet tissue volume (113 ml) basedon lung wet weight (4.7 24 g dry weight). Thepredicted left lung FRC was 31% total FRC. The ex-pected FRC of a uniformly inflated left lung based ontissue mass was 43% total FRC. This value was re-duced by 25% via the vertical Ptp gradient, resultingin a left lung FRC of 32%, near the predicted value of31%. Accordingly, the reduced blood flow to the depen-dent left lung in the LLD posture was consistent witha reduced FRC caused by the vertical Ptp gradient.Evidently vertical gradients in Q require knowing re-gional lung volume to accurately predict relative bloodflow to each lung. A similar argument applies to VAmeasurements.
Regional distribution of PrO2 and VA/Q. The largestgradient in PrO2 (1.3, Table 2) was observed in thevertical direction for the whole lung in the LLD postureand was positive, indicating that PrO2 was smaller inthe dependent (left) lung than in the nondependent(right) lung (intercepts, Table A3). This vertical gradi-ent was abolished with inversion to the RLD posture
Fig. 1. Blood flow (Q) per unit regionallung volume (ml min1 ml1) vs. lungheight for a representative dog in theleft lateral decubitus (LLD) posturewithout positive end-expiratory pres-sure (PEEP; A), LLD with 10 cmH2OPEEP (B), right lateral decubitus(RLD) posture without PEEP (C), andRLD with 10 cmH2O PEEP (D). R,right lung (E); L, left lung ({). Linesrepresent best-fit values from multiplelinear regression analysis. R2 indi-cated that 40% of the variability inblood flow was spatially determined.WL, whole lung; RL, right lung; LL,left lung. Independent and dependentaxes have been interchanged for pre-sentation.
750 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
and was accompanied with positive dorsal-ventral andcaudal-cranial gradients.
To determine whether PrO2 observed in the depen-dent lung in the LLD posture was low enough to triggera hypoxic vasoconstriction response, the minimum PrO2value was obtained from regression analysis for the sixanimals studied. Substituting into Eq. 5, the linearequation with mean intercept and coefficients for thewhole lung was as follows (Table A3)
PrO2 113 1.3x 1.15y 0.5z 0.14xy 0.16yz
0.06zx 0.03xyz
The minimum value of PrO2 (81 21 Torr) occurred inthe dependent (x 4 cm), dorsal (y 5 cm), andcaudal (z 8 cm) regions of the lung (Fig. 6). Themaximum value of PrO2 (124 5 Torr) was located inthe nondependent (x 4 cm), ventral (y 5 cm),and cranial (z 8 cm) region of the lung. In the RLDposture, minimum and maximum PrO2 values evalu-ated at similar (x, y, z) values used for the LLD posturewere 96 10 and 117 8 Torr, respectively (Fig. 6).Note that PrO2 was reduced below 100 Torr only in thedependent lung in the LLD posture.
The low PrO2 originating from the dependent caudal-dorsal regions of the dependent left lung in the LLDposture without PEEP was increased by inversion tothe RLD posture (Fig. 4). That body inversion from theLLD to the RLD posture increased PrO2 in the caudal
regions was consistent with the reduction or eliminationof significant positive vertical, dorsal-ventral, and cau-dal-cranial PrO2 gradients for the whole lung (Table 2).
In the left and right lung, small but significant gra-dients in PrO2 and VA/Q were observed in all threecoordinates (Table 2). However, the detection of a sig-nificant VA/Q (PrO2) gradient was associated with asignificant PrO2 (VA/Q) gradient only in the left depen-dent lung in the LLD posture. In the left (dependent)lung in the LLD posture, a dorsal-ventral VA/Q gradi-ent (0.053) was associated with significant PrO2 gradi-ents (2.8).
Comparison Between Predicted and MeasuredGas Exchange
Predicted PaO2 and PaCO2 calculated from regionalVA/Q data did not differ from measured PaO2 and PaCO2in both the LLD and RLD posture (Table 1), and themeasured A-aDO2 was well predicted from the micro-sphere data in the LLD posture. However, the pre-dicted values of A-aDO2 were significantly (P 0.05)less in the LLD than in the RLD posture (Table 1).
Mean VA/Q and PrO2 Changes of Nondependentand Dependent Lung
In the LLD posture (intercepts, Table 2), VA/Q wasgreater in the nondependent right lung (1.42 0.45)
Fig. 2. Ventilation (VA) per unit regionallung volume (ml min1 ml1) vs. lungheight for representative animal in LLDwithout PEEP (A), LLD with 10 cmH2OPEEP (B), RLD without PEEP (C), andRLD with 10 cmH2O PEEP (D). Lines rep-resent best-fit values from multiple linearregression analysis.
751LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
than in the dependent lung (0.93 0.37). In the rightlung, PrO2 increased with body inversion from the RLD(113 7 Torr) to the LLD (119 4 Torr) posture. Thiswas associated with an increase in VA/Q from 1.09
0.39 in the RLD posture to 1.40 0.60 in the LLDposture. This behavior was accompanied with a dorsal-ventral VA/Q gradient that was significant (0.035) onlyin the RLD posture.
Fig. 3. VA-to-Q ratio vs. lung height forrepresentative animal in LLD withoutPEEP (A), LLD with 10 cmH2O cmPEEP (B), RLD without PEEP (C), andRLD with 10 cmH2O PEEP (D). Linesrepresent best-fit values from multiplelinear regression analysis.
Fig. 4. Regional PO2 (PrO2) vs. lung height forrepresentative animal in LLD without PEEP(A), LLD with 10 cmH2O cm PEEP (B), RLDwithout PEEP (C), and RLD with 10 cmH2OPEEP (D). Lines represent best-fit valuesfrom multiple linear regression analysis.Note that the low PCO2 values in the depen-dent lung in the LLD posture (A) was elimi-nated with the addition of PEEP (B).
752 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
Regional Variations in the Spatial Gradients
The significant coefficients d, e, and f, shown inTables A2 and A3 indicated that the spatial gradientsvaried along an orthogonal axis. These are discussed inthe APPENDIX.
Effect of PEEP
Regional distribution of Q. In general, PEEP eitherreduced or eliminated the spatial gradients in Q and VAthat occurred without PEEP (Table A2). The decrease inthe vertical gradient with PEEP was associated with adecrease (3050%) in the mean blood flow (intercepts,Table A2). With PEEP, the dependent right lung in theRLD posture had the greater blood flow, similar to thebehavior without PEEP (Table 3). By contrast, in theLLD posture PEEP eliminated the left-right lung differ-ence in blood flow measured without PEEP.
PEEP increased the low PrO2 originating from thedependent caudal-dorsal regions of the dependent leftlung in the LLD posture (intercepts, Table A3). The lattereffect of PEEP was consistent with the PEEP-inducedreduction of the caudal-cranial VA/Q gradient (from 0.053to 0.03, Table A3) and 50% reduction of the caudal-cranial PrO2 gradient (from 0.85 to 0.40) in the left lung.
Similar to the data without PEEP, with PEEP PaO2and PaCO2 calculated from VA/Q data did not differ frommeasured PaO2 and PaCO2 in both the LLD and RLD
posture, and the measured A-aDO2 was well predictedfrom the microsphere data (Table 1).
PEEP reduced the relatively high VA/Q of the non-dependent right lung to a value closer to 1 (Table A3,1.22 0.24). In the right lung with PEEP, VA/Q in-creased with body inversion from the RLD posture(1.13 0.24) to the LLD posture (1.22 0.24).
In the left lung in the LLD posture, PEEP increasedPrO2 from 105 12 to 112 7 Torr (Table A3). Thisbehavior was associated with a PEEP-induced verticalPrO2 gradient (0.83) in conjunction with reduced dor-sal-ventral and caudal-cranial PrO2 gradients.
Regional Perfusion Correlation Between PosturesWith and Without PEEP
Figure 5 shows Q to each lung piece in the LLD postureplotted against blood flow of the same piece in the RLDposture of one representative animal without PEEP (Fig.5A) and with PEEP (Fig. 5B). Except for the left lungwithout PEEP (R 0.66), blood flow to each piece waspoorly correlated (R 0.0440.22) between LLD andRLD posture. In other words, lung pieces with high (orlow) blood flow in the LLD posture received low (or high)blood flow in the RLD posture. This behavior was consis-tent with the gravity-dependent vertical gradients ob-served for both right and left lungs and for the whole lungin both postures, opposite to that found between thesupine and prone position (19).
Q and VA heterogeneity. The mean coefficients ofvariation of Q and VA (3060%) were similar to re-ported values (19, 21, 29, 33, 40). Table 4 summarizesthe heterogeneity in VA and Q evaluated by threemethods: total and residual variances of VA, Q, andVA/Q; widths (lnSDVA and lnSDQ) of the VA-VA/Qand Q-VA/Q distribution curves measured by FMS andMIGET. The variance of the data based on regionalvalues was similar to that based on uncorrected data.The coefficients of correlation (c) between VA and Q(Pearsons method) were similar to those computed byuse of VA, Q, and 2VA/Q in Eq. 8 (33). The totalvariance data showed that in the LLD posture PEEPreduced the variance in VA and VA/Q but not in Q,
Table 3. Percent cardiac output and ventilation toleft and right lung from microsphere data
PEEP, cmH2O
LLD RLD
0 10 0 10
Q, % Left lung 376 498* 364 325Q, % Right lung 636 518* 644 685VA, % Left lung 286 436* 349 377VA, % Right lung 726 576* 669 637
Values are means SD (n 6). *P 0.05, significant changewith PEEP; P 0.05, significant difference with change in pos-ture; P 0.05, significant difference between left lung and rightlung.
Fig. 5. Correlation between pulmonaryblood flow in the LLD and RLD measuredin 1 representative animal without PEEP(A) and with PEEP (B). Dotted line is lineof identity. Note that lung pieces with high(low) blood flow in the LLD posture re-ceived low (high) blood flow in the RLDposture, consistent with a gravity-depen-dent vertical gradient measured by multi-ple linear regression analysis (Fig. 1B).
753LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
consistent with a more uniformly inflated lung at thehigher lung volume. This PEEP-induced change invariance was undetected by the other two methods.Neither body position nor PEEP affected the totalvariance in Q. Neither PEEP nor body positionchanged the correlation between VA and Q. There wasa tendency for heterogeneity measured by lnSDVA andlnSDQ to be greater with MIGET than with FMS, butthe difference was only significant for Q in the LLDposture without PEEP. The broader distribution mea-sured with MIGET than with topographical data hasbeen noted in previous studies (15, 45). The differencehas been attributed to the coarse scale of the VA/Qdistribution inherent in MIGET (4, 5).
Heterogeneity in VA, Q, and VA/Q that was attrib-uted to residual variation as measured by the residualsof the regression analysis was reduced from 65 16%of the total variance in the linear regression analysis to41 6% of the total variance in the fourth-orderregression analysis (Table 4). These values are in linewith the coefficients of determination (R2) of 40 and60% that implicated 60 and 40% of the variability toresidual variation. Similar to the total variance, PEEPreduced the residual variance of VA in the RLD posture.Neither body position nor PEEP affected the residualvariance in Q. There was a tendency for PEEP to in-crease the residual-to-total variance fraction in VA andVA/Q, but this was only significant in the LLD posture.
The coefficient of correlation (c) between VA and Qcalculated by using the residual variances (0.590.75,Table 4) in Eq. 8 was similar to the correlation coeffi-cient between VA and Q (0.570.71).
DISCUSSION
In this study we used a high-resolution technique todescribe the distribution of Q, VA, VA/Q, and PrO2 in thelateral decubitus posture. The high resolution in con-junction with multiple linear regression analysis al-lowed the spatial description of these variables at anyarbitrary position relative to the three rectangularcoordinate axes.
The major findings of this study are as follows. First,the gravity-dependent vertical gradient in Q wasgreater in the RLD than LLD posture (Fig. 1, A and B;Table 2). This was attributed to a reduced blood flow inthe dependent left lung in the LLD posture (Table 3).Second, PEEP reduced the vertical gradient in bothpostures and eliminated the difference between pos-tures (Fig. 1). PEEP or body inversion from the LLD tothe RLD posture abolished the positive vertical, dorsal-ventral, and caudal-cranial gradients in PrO2 observedin the LLD posture (Table A3). Third, a positive verti-cal gradient in PrO2 was observed in the LLD posturewith the dependent dorsal-caudal regions of the depen-dent lung having values below that (100 Torr) needed
Table 4. Effect of position and PEEP on heterogeneity of VA and Q distribution: FMS and MIGET
Method 2, lnSD or c
ZEEP PEEP
LLD RLD LLD RLD
FMS (total)2VA 0.220.05 0.390.22 0.160.01* 0.140.022Q 0.150.07 0.230.12 0.130.05 0.160.052VA/Q 0.310.16 0.260.12 0.110.04* 0.130.03c(VA:Q) 0.570.16 0.710.17 0.660.14 0.650.14
Residual (linear)2VA 0.140.04 0.210.07 0.140.04 0.120.052Q 0.090.02 0.120.04 0.090.04 0.100.062VA/Q 0.080.04 0.090.06 0.070.02 0.080.03c(VA:Q) 0.650.12 0.750.12 0.710.10 0.610.12
Residual/total (%), linear2VA 6616 6626 8922 90442Q 6517 7145 6921 64352VA/Q 3217 4226 6316* 6515
Residual (4th order)2VA 0.080.03 0.090.06 0.070.04 0.080.052Q 0.140.04 0.180.12 0.110.04 0.100.042VA/Q 0.090.04 0.090.05 0.070.02 0.090.05c(VA:Q) 0.590.16 0.710.06 0.640.12 0.500.18
Residual/total (%), 4th order2VA 3413 3718 4816 47352Q 3513 328 4717 45312VA/Q 3613 3715 4813 4531
FMSlnSDVA 0.400.07 0.360.07 0.300.04 0.360.07lnSDQ 0.450.16 0.480.18 0.350.07 0.360.08
MIGETlnSDVA 1.070.60 1.040.59 1.000.57 1.240.54lnSDQ 0.710.24 0.600.14 0.680.40 0.520.17
Data are means SD (n 6), except for multiple inert gas elimination technique (MIGET, n 5). 2, variance; c, correlation coefficientbetween VA and Q; lnSDVA and lnSDQ, log-normal standard deviation of VA- and Q-VA/Q distributions. *P 0.05 compared with ZEEP inLLD; P 0.05 compared with ZEEP in RLD; P 0.02 compared with MIGET.
754 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
to invoke a hypoxic vasoconstriction response (31). Thisbehavior was consistent with the reduced blood flow tothe dependent lung in the LLD posture.
Methodological Issues
Fluorescent microsphere technique. The microspheretechnique as implemented in this study has been val-idated in previous studies (17, 40). Regional depositionof aerosolized and injected microspheres allowed si-multaneous measurements of ventilation and perfu-sion distribution that predicted regional gas exchangewith high spatial resolution.
Volume adjustment to FRC and vertical Ptp gradi-ent. Injected and aerosolized fluorescent microsphereswere delivered in vivo near FRC, whereas the fluores-cent signals were measured in vitro in the dried lunginflated to TLC. Accordingly, we made several adjust-ments to the weight of each piece to extrapolate topiece volume in vivo and to determine Q and VA perunit regional lung volume at FRC.
First, the lung volume of each piece was adjustedfrom TLC to FRC by reducing the cube lengths in thethree dimensions. This adjustment resulted in ananisotropically inflated lung (20) and a homogeneous(constant) deformation along each axis. Second, weimposed a distortion to the vertical dimension (x) ofeach lung piece to produce a vertical Ptp gradient aspreviously measured (1). This distortion in the x di-mension at each height was based on the PV curve ofan isolated lung (27) and was applied to all y and zdimensions at the same height. This preserved thehomogeneous deformation in the y and z coordinatesand the anisotropy in regional volume at FRC, in effectproducing changes in regional volume identical tothose given by the PV curve (Eq. 2). These adjustmentsfor the vertical Ptp gradient increased the (maximum)dependent (D)-to-nondependent (N) ratio (D/N) for Qby a factor of 3, N/D in regional lung volume, andD/N in regional lung density (16). Implicit in thisadjustment for lung density is the scaling of tissuemass to capillary density. Accordingly, regional lungdensity changes caused by the vertical Ptp gradientwere the dominant contributor to the vertical gradientin Q and VA.
Prior studies have reported the vertical gradients ofperfusion relative to the number of alveoli or pieceweight at TLC. This paper presents perfusion gradi-ents relative to the regional lung volume at the time ofmicrosphere injections. The adjustment for the verticalchanges in regional lung density produced verticalgradients in regional Q that were greater than thoseestimated in previous studies using TLC-measuredregional volume (18, 19, 21, 22, 33, 34). These normal-ization issues need further evaluation, particularly inthe supine and upright body positions under both nor-mal and increased acceleration loads with relativelylarge Ptp gradients (1, 2).
We made no adjustment for Ptp gradients in theother two axes (y and z), in the absence of reporteddata. Blood volume was ignored in the calculation of
lung density and regional lung volume because the dryweight used in the calculation of mean lung densitywas blood free.
Distribution of Regional Perfusion
Effect of gravity. The effects of gravity on the verticalgradient in blood flow in the lung have been describedin terms of the relation among the Ppa and pulmonaryvenous (Ppv) and alveolar (Palv) pressures (48, 49).This theory predicts a decreasing blood flow up theheight of the lung (in our nomenclature, a negativevertical gradient). Most of the vertical gradients mea-sured in the present study are explainable, at leastqualitatively, with the gravitational model. The verti-cal gradients in blood flow measured in the LLD andRLD posture with and without PEEP were expectedand confirmed previous findings (6, 20, 25, 28, 37).
Effect of lung volume and vascular resistance. Thefact that the gravity-dependent vertical gradients in Qdecreased with a change from RLD to LLD posture andwith PEEP indicates that factors other than gravitycontributed to the blood flow distribution. A majorfactor was the lung volume-induced vascular resis-tance that changed with body position and PEEP. Pul-monary vascular resistance depends on lung volume(24); its changes with lung volume are different forzone 2 (Ppa Palv Ppv) and zone 3 (Ppa Ppv Palv) conditions (9). By this theory (24), Q is propor-tional to Ppa Palv in zone 2 and Ppa Ppv in zone3. The increased flow down the lung is due to Ppaincreasing down the lung in zone 2 and to Ppv-inducedcapillary recruitment or vascular distention in zone 3.
In the latter study (9), pulmonary blood flow andvascular resistance were measured vs. lung volume(%TLC) at constant values of Ppa Palv and Ppv Palv under both zone 2 and zone 3 conditions in iso-lated rabbit lungs. In zone 3, for Ppa-Palv of 18 mmHg,blood flow increased linearly with a decrease in lungvolume from TLC to residual volume. In zone 2, bloodflow increased as lung volume decreased from TLC to50% TLC but decreased from 60% TLC to residualvolume, a behavior consistent with the U-shape curvedescribing the relationship between vascular resis-tance and lung volume (44). Whatever the lung vol-ume-induced differences in blood flow, blood flow wasgreater in zone 3 than in zone 2.
In the present study, without PEEP, Ppv averaged8.4 cmH2O in the LLD posture and 6.1 cmH2O in theRLD posture (Table 1, Ppcw) relative to mid-heartlevel. With a mean Paw of 5 cmH2O (Table 1), thedependent lung was in zone 3 in both postures whereasthe nondependent lung was predominantly in zone 2,more so in the RLD than in the LLD posture. PEEPincreased Ppv to 10 cmH2O and mean Paw to 15cmH2O in both postures, placing the nondependentlung and half of the dependent lung in zone 2. Pulmo-nary vascular resistance, (Ppa Ppcw)/blood flow, wasgreater in the dependent than nondependent lung inboth postures and increased with PEEP (Table 1).
755LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
The gravity-dependent vertical gradients in bloodflow measured in both postures for the whole lungwithout PEEP (Table 2, Fig. 1, A and C) were consis-tent with the shift from zone 2 to zone 3 conditionsdown the lung, but these gradients were accentuatedby the threefold increase in lung density down thelung. The removal of the density gradient with PEEPreduced the gradients to 44 and 33% in the LLD andRLD posture, respectively (Table 2, Fig. 1, B and D).Thus the two- to threefold increase in the gradient withthe removal of PEEP was attributed almost entirely tothe lung density gradient. A similar behavior was ob-served for both left and right lungs in the LLD posture(Fig. 1, A and B).
Blood flow was lower in the dependent left lung thanin the nondependent lung (Table 3), consistent with theresults of a previous study (28). This behavior wasopposite to that predicted by gravity, indicating thatfactors other than gravity contributed to blood flowdistribution in the LLD posture. One factor has beenassociated with the vascular structure (17, 28). Thereduced blood flow to the dependent left lung was notcaused by a heart weight induced lower lung volumeper se because a reduced lung volume is associatedwith a lower vascular resistance in zone 3 (9). It ispossible that a nonuniform lung distortion due to heartand abdominal weight might conceivably cause an in-creased vascular resistance. Another mechanism suchas hypoxic vasoconstriction remains an alternative ex-planation in vivo, particularly in view of the positivegradient in PrO2 measured (see below).
Nongravitational gradients in Q. An important find-ing of this study relates to other nongravitational gra-dients in Q. Specifically, in the isogravitational ( y-z)plane (x 0), a positive dorsal-ventral gradient in Qoccurred in the left dependent lung in the LLD posture,with blood flow maximal in the ventral regions (Table2, 0.26). The smaller blood flow in the dorsal regionswas opposite to that observed in the supine dog (10) inwhich the dorsal lung regions had the larger blood flow.Thus the present measurements would not support anintrinsic greater vascular conductance postulated forthe dorsal lung regions (10). Thus extrinsic factorssuch as hypoxic vasoconstriction and lung distortioncaused by the weight of the heart and abdomen mightbe crucial.
The positive dorsal-ventral gradient in Q observed inthe left lung in the LLD posture occurred in conjunc-tion with a negative caudal-cranial gradient in Q withQ increasing in the caudal region, in the absence of anygradient in the right lung. Both these gradients wereabolished with PEEP, indicating a lung volume-in-duced relative shift of blood flow from the ventral-caudal to the dorsal-cranial regions.
The decrease in blood flow in the caudal-cranialdirection for the whole lung in the LLD posture isconsistent with the results of Greenleaf et al. (20) inthe mechanically ventilated anesthetized dog. Thiscontrasts to the absence of a caudal-cranial gradient inspontaneously breathing humans in the lateral decub-itus posture (6).
Distribution of Ventilation
Effect of posture without PEEP. In contrast to theabsence of a vertical VA gradient in the LLD posture(Table 2), total ventilation was greater in the nonde-pendent than dependent lung in the LLD posture (Ta-ble 3). This difference was similar to the behavior inblood flow and was most likely due to a smaller FRC inthe dependent left lung. Body inversion from LLD toRLD posture produced a substantial negative gradientin VA (0.58) that was consistent with the greater totalventilation measured in the right dependent lung thanin the nondependent lung. This behavior in the anes-thetized dog is consistent with results from the anes-thetized human in the lateral decubitus posture (38,39). These results with anesthesia differed substan-tially from those in awake humans, showing greaterventilation in the dependent than nondependent lungin both the LLD and RLD posture (7, 25, 32). The latterbehavior was explained by the vertical Ptp gradientcausing a lower lung volume and greater lung compli-ance in the dependent lung regions. The absence of acaudal-cranial gradient in VA in the lateral decubitusposture in the anesthetized dog was consistent withthe results in awake humans measured by using radio-active gas inhalation and external scintillationcounters (7, 25). This behavior was attributed to auniform Ptp in the horizontal direction.
The differences in ventilation measured between theanesthetized and awake state might be related to theanesthesia-induced reduction in FRC observed in bothlungs (38, 39). The following factors might be involved.First, the nondependent lung would move from theupper low-compliant part of its PV curve during awakebreathing to the lower high-compliant part after anes-thesia, resulting in better ventilation. Second, the clos-ing volume of the dependent lung might be greaterthan its FRC (36), consistent with the absence of ven-tilation to part of the dependent lung and with reducedventilation. Third, atelectasis and small airway closurein the dependent lung with its lower Ptp and greaterclosing volume would serve to shunt ventilation to thenondependent lung. Fourth, in addition to the anesthe-sia-induced reduction in FRC, the weight of the heartand abdomen would compress the dependent lung andexpand the nondependent lung. This effect of gravitywould be greater in the smaller dependent left lung inthe LLD posture than the relatively larger dependentright lung in the RLD posture, accounting for thedifference between the two postures.
Except for the left lung in the LLD posture, signifi-cant negative vertical VA gradients were observed inthe left lung in the RLD posture and in the right lungin both postures. These gradients were accentuated bythe imposed vertical gradient in regional volume. Inaddition, a positive dorsal-ventral gradient in VA wasobserved in the left lung in both postures. The reasonfor this gradient was not apparent.
Effects of PEEP. Like the blood flow distribution,PEEP reduced the difference in Q between the depen-dent and nondependent lung in the LLD posture (Fig.
756 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
2, A and B, Table 3), similar to the behavior found inthe anesthetized human (39) and dog (36). The PEEP-induced change in the vertical gradient in VA in theLLD posture occurred in conjunction with the elimina-tion of the positive dorsal-ventral gradient in VA (TableA2). PEEP eliminated or reduced the negative gradientin VA observed for the whole lung and left lung in theRLD posture and in the right lung in both postures. Asimilar effect was observed for dorsal-ventral gradientsfor the whole lung and for the left lung in both pos-tures. Accordingly, in general the effect of PEEP was toreduce the spatial variations in ventilation by increas-ing regional lung volume to a less compliant part of thePV curve where tidal-volume induced changes in air-way resistance are minimal.
Distribution of Regional VA/Q
The VA/Q ratio was greater in the nondependentlung than in the dependent lung in the LLD posture(Table A3). There was a tendency (not significant) forthis behavior to be reversed in the RLD posture withthe dependent lung having the greater VA/Q, consis-tent with the results in the anesthetized human sub-jected to positive airway pressure (28). The latter re-sult is supported by the PEEP-induced increase in thevertical VA/Q gradient in the RLD posture (Table A3).Furthermore, PEEP produced a positive vertical gra-dient in VA/Q in the dependent lung in both postures.By contrast, in keeping with the PEEP-induced reduc-tion in the spatial variation in VA, PEEP eliminated orreduced the dorsal-ventral gradient in VA/Q observedfor the whole lung in the RLD posture and in thedependent lung in both postures. These nongravita-tional gradients measured in the anesthetized dog withPEEP were not observed in the awake human (6).
Distribution of PrO2A major advantage of the fluorescent microsphere
technique over other techniques is the ability to mea-sure regional values and spatial gradients in PrO2.Estimated PaO2 values, determined from a perfusion-weighted sum of PrO2, calculated by using microspheremeasures of Q and VA, were consistent with measuredPaO2 values in the anesthetized dog in the presentstudy, confirming similar results in the pig (4). How-ever, in the present study, microsphere data underes-timated A-aDO2. This might be attributed to moreheterogeneous perfusion and ventilation with thegreater spatial resolution (4).
On the basis of multiple linear regression analysis ofthe PrO2 data and the calculated spatial gradients, PrO2in the LLD posture was greater in the nondependentventral and cranial lung regions than in the dependentdorsal and caudal lung regions, respectively. Thesedifferences were either eliminated or reduced withPEEP.
In the left lung in the LLD posture, PEEP increasedPrO2 from a mean value of 106 11 to 112 7 Torr(Table A3). This was accompanied with a PEEP-in-duced reduction of significant dorsal-ventral and cau-
dal-cranial PrO2 gradients (Table A3). Accordingly, thedependent lung in the LLD posture without PEEP hadthe lowest VA/Q (Table A3) and the lowest PrO2. Inver-sion of the dependent lung to the nondependent posi-tion and PEEP both served to increase VA/Q and PrO2.
In general, the PrO2 distribution was less uniform inthe left lung than in the right lung, especially in thedependent LLD posture, and PEEP produced a moreuniform PrO2 distribution in the dependent left lung.Compared with the dependent right lung in RLD posi-tion, the greater lung distortion caused by the weightof the heart and abdomen acting on the smaller depen-dent left lung in the LLD posture might contribute to aless uniform PrO2 distribution.
Hypoxic Pulmonary Vasoconstriction and Zone 4
Many studies (19, 20, 24, 26, 36) have demonstratedthat blood flow decreased in the most dependent lungregions (zone 4), opposite to the behavior predictedfrom the effects of gravity in zone 3 (49). This behaviorhas been attributed to increased vascular resistancecaused by hypoxic pulmonary vasoconstriction (19, 20,26, 36) or reduced vascular diameter in the most de-pendent lung regions (19, 20, 26, 36). The latter effectwas attributed either to a low lung volume or perivas-cular cuff formation due to increased transvascularfluid flux (24).
Hypoxic pulmonary vasoconstriction might regulateregional perfusion to match VA to achieve efficient gasexchange (30). Our estimates of VA/Q and PrO2 pro-vided evidence that this mechanism might be at workin the left dependent lung in the LLD posture. In thepresent study, some lung pieces of the dependent lungin the LLD posture showed relatively low PrO2 values(Fig. 4, A and C) that were consistent with values(PrO2 100 Torr) associated with hypoxic pulmonaryvasoconstriction (8, 12, 30). Estimates of PrO2 from thedata analysis (Fig. 6) provided evidence that in the
Fig. 6. Minimum and maximum PrO2 values from best-fit multiplelinear regression equation in the LLD and RLD postures. *P 0.05,LLD vs. RLD posture. The minimum PrO2 values in the LLD postureare consistent with a hypoxic vasoconstriction response that wouldaccount for the reduced blood flow measured in the dependent leftlung (Table 3). x, y, and z, Vertical, dorsal-ventral, and caudal-cranial axes, respectively.
757LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
LLD posture hypoxic vasoconstriction occurred in thedependent lung, where total blood flow was reducedrelative to the nondependent lung (Table 3). PEEPincreased both VA/Q and PrO2 in the dependent leftlung (Figs. 3 and 4) and eliminated the hypoxic vaso-constriction, resulting in a gravity dependent greaterblood flow in the dependent lung than in the nonde-pendent lung.
Effect of Heart and Abdominal Weight on BloodFlow Distribution
Many studies (3, 23, 35, 38, 41) have suggested thatlung volume and blood flow of the dependent lung arereduced in the lateral decubitus posture because of amediastinal shift due to heart and abdominal weight.In the dog, the weight of the heart compressed thedependent lung regions to a greater extent in thesupine than in the prone position (23). The heartweight-induced change in lung volume was greaterwith body inversion from LLD to RLD posture thanfrom the prone to supine posture (35).
Mean Q calculated by the regression analysis indicatedthat the PEEP-induced reduction in regional perfusionat the center of mass near the heart was greater in thenondependent than in the dependent lung (Table 2,intercepts). This effect was greater in the left than inthe right lung. Thus the effect of PEEP on the bloodflow distribution was greater in the left lung in theLLD posture than in the right lung in the RLD posture.The difference in the preinspiratory lung volume be-tween the left and right lung may be involved, in viewof studies in anesthetized humans (38) showing thatFRC of the right lung in the RLD posture was largerthan FRC of left lung in the LLD posture, whereas FRCof the nondependent right lung was similar to thedependent right lung in the RLD posture. Thus thePEEP-induced lung expansion might be greater in theright dependent lung than in the left dependent lungthat was closer to its closing volume. The reduced effectof PEEP in the left dependent lung in the LLD posturemight be exacerbated during anesthesia, which might
reduce diaphragmatic tone and reduce the diaphrag-matic support of abdominal weight (14, 41). Thus thenonuniform ventilation distribution observed in theLLD posture can be alleviated by inversion to the RLDor with PEEP.
Q and VA Heterogeneity
The Q and VA heterogeneity in this study as mea-sured by the coefficient of variation of Q and VA (3060%) is consistent with previous studies using fluores-cent microspheres (18, 19, 21, 29, 33, 34, 40). However,on the basis of a one-dimensional linear regressionanalysis, the latter studies concluded that 90% of theheterogeneity in Q was due to factors other than spa-tial variation. By contrast, the multiple regressionanalysis in the present study indicated that 40% ofthe variability in Q, VA, and VA/Q distributions wasattributed to spatial variation (Table 4). The contribu-tion (60%) by the residual variance in the Q distribu-tion is near to that measured in the supine dog (11).
The factors that contributed to the residual varianceinclude heterogeneity on a scale that was smaller than1 cm, the dimension of the lung cube in which Q andVA were measured (50). The variances of VA, Q, andVA/Q attributed to residual variation produced a corre-lation between VA and Q similar to that produced bythe total variability (0.65). This behavior in conjunc-tion with the 40% of the total variance in VA/Q attrib-uted to residual variability suggests that matching ofVA and Q is not predominantly associated with randomvariability. The relative contribution of residual vari-ability using multiple regression analysis in previousstudies (18, 19, 21, 22, 29, 33, 34, 40) needs furtherevaluation.
In conclusion, blood flow to the dependent left lung inthe LLD posture was lower than that expected becauseof gravity. The reduced blood flow resulted from hy-poxic vasoconstriction that occurred because of a re-duced ventilation to the dependent lung compressed bythe mediastinal contents. These effects were abolished
Table A1. x, y, z Coordinate distances between center of mass and original coordinate system at caudal edge(z0 0), left edge (x0 0), dorsal edge (y0 0) of the lung
PEEP, cmH2O
LLD
L (%)
RLD
L (%)0 10 0 10
Whole lungx 6.10.7 9.60.9 50 7.90.2 9.50.5 20y 6.50.4 8.60.5 30 6.50.4 8.60.5 30z 11.50.9 13.61.0 20 11.50.8 13.61.0 20
Right lungx 8.30.9 12.71.3 50 5.10.3 6.30.5 20y 7.30.4 9.00.6 20 6.60.5 9.00.6 30z 12.20.9 13.71.0 12 10.90.8 13.71.0 20
Left lungx 3.20.4 5.30.6 65 11.60.6 13.70.9 20y 5.50.3 8.00.6 45 6.50.4 8.00.6 20z 10.50.9 13.51.0 30 12.20.9 13.51.0 10
Values are means SD; n 6. LPEEP0 x,y,z coordinate distances (cm) between center of mass and original coordinate system at caudaledge at PEEP 0 cmH2O in lung; LPEEP10 x,y,z coordinate distances (cm) between center of mass and original coordinate system at caudaledge at PEEP 10 cmH2O in lung. L (LPEEP10LPEEP0)/LPEEP0 for x, y, z respectively.
758 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
Tab
leA
2.C
oeffi
cien
tsan
dR
2of
mu
ltip
leli
nea
rre
gres
sion
equ
atio
n
fit
toQ
and
VA
dat
afo
rw
hol
e,le
ft,
and
righ
tlu
ng,
resp
ecti
vely
Lu
ng
Pos
itio
nP
EE
PIn
terc
ept
ab
cd
ef
gR
2
QW
hol
eL
LD
05.
0
2.1
0.
27
0.11
*0.
078
0.09
0
0.07
9
0.03
2*
0.03
7
0.03
8
0.02
4
0.00
4*0.
046
0.02
4*0.
006
0.00
5*0.
44
0.12
LL
D10
2.8
0.7
0.
12
0.08
*
0.02
4
0.01
7*
0.02
1
0.01
6*
0.00
7
0.00
9
0.00
6
0.00
5*0.
005
0.00
5*0.
002
0.00
1*0.
42
0.13
RL
D0
5.2
1.5
0.
42
0.39
*0.
010
0.01
5
0.07
4
0.04
9*0.
035
0.02
8*
0.03
5
0.02
2*0.
011
0.01
40.
001
0.00
50.
23
0.13
RL
D10
2.5
0.8
0.
14
0.07
*
0.00
01
0.04
0.
021
0.02
70.
0001
0.00
2
0.00
4
0.00
6
0.00
1
0.00
6
0.00
02
0.00
10.
56
0.15
QL
eft
LL
D0
5.8
2.2
0.
60
0.40
*0.
26
0.24
*
0.18
0.11
*0.
11
0.14
0.
074
0.03
*0.
041
0.04
60.
020
0.01
6*0.
52
0.14
LL
D10
4.0
1.1
0.
15
0.12
*0.
09
0.05
0.
012
0.02
0.02
0.01
5*
0.01
9
0.00
8*
0.00
3
0.00
60.
003
0.00
2*0.
37
0.09
RL
D0
3.9
1.4
0.
04
0.19
0.18
0.15
*
0.04
0.06
0.
037
0.02
*
0.03
3
0.02
1*0.
007
0.00
8
0.00
02
0.00
30.
39
0.11
RL
D10
1.9
0.8
0.
06
0.04
*0.
006
0.04
5
0.02
4
0.01
9*
0.02
4
0.01
9
0.00
7
0.00
5*0.
004
0.05
0.
0000
7
0.00
20.
27
0.11
QR
igh
tL
LD
04.
6
2.2
0.
37
0.22
*
0.06
0.09
0.00
6
0.03
0.
001
0.02
0.
014
0.01
40.
015
0.01
2*0.
005
0.00
4*0.
39
0.06
LL
D10
2.4
0.7
0.
12
0.05
*
0.07
0.04
3*
0.00
8
0.02
0.
005
0.00
2*
0.00
2
0.00
40.
007
0.00
5*0.
001
0.00
10.
37
0.1
RL
D0
5.8
3.8
0.
56
0.68
0.
006
0.2
0.
065
0.11
0.03
0.05
3
0.04
6
0.05
70.
064
0.06
10.
1
0.24
0.47
0.17
RL
D10
3.4
1.2
0.
14
0.11
*
0.01
5
0.04
2
0.01
6
0.04
60.
001
0.07
0.
006
0.00
90.
004
0.01
50.
001
0.00
20.
37
0.18
VA
Wh
ole
LL
D0
5.1
1.4
0.
068
0.27
0.27
0.25
*
0.03
0.10
0.
053
0.04
*
0.04
3
0.02
6*0.
04
0.02
*0.
009
0.00
9*0.
39
0.11
LL
D10
2.9
0.7
0.
072
0.06
*
0.00
3
0.02
30.
013
0.02
4
0.02
1
0.01
5*
0.01
1
0.00
9*0.
006
0.00
5*0.
002
0.00
1*0.
28
0.10
RL
D0
5.5
1.4
0.
58
0.34
*0.
31
0.25
*
0.05
5
0.14
0.02
4
0.04
0.
049
0.02
*0.
006
0.01
90.
005
0.00
50.
47
0.17
RL
D10
2.8
0.6
0.
079
0.08
90.
016
0.06
7
0.00
1
0.02
8
0.00
4
0.00
9
0.00
6
0.00
9
0.00
3
0.00
7
0.00
04
0.00
10.
32
0.15
VA
Lef
tL
LD
04.
6
1.8
0.
45
0.49
0.41
0.22
*
0.07
0.13
0.08
3
0.12
0.
088
0.07
6*0.
049
0.04
6*0.
015
0.02
20.
50
0.14
LL
D10
3.1
1.0
0.
03
0.1
0.13
0.09
7*
0.00
2
0.00
90.
014
0.02
3
0.02
5
0.01
7*0.
001
0.01
30.
001
0.00
10.
43
0.17
RL
D0
3.2
0.9
0.
20
0.16
*0.
27
0.20
*
0.03
8
0.11
0.
003
0.03
0.
023
0.02
1
0.00
5
0.02
50.
007
0.00
6*0.
55
0.12
RL
D10
2.5
0.7
0.
08
0.04
*
0.01
7
0.06
7
0.01
6
0.01
2
0.00
3
0.02
0.
009
0.00
90.
01
0.00
3*0.
002
0.00
40.
27
0.08
VA
Rig
ht
LL
D0
5.5
1.7
0.
50
0.21
*0.
09
0.20
0.02
1
0.09
20.
032
0.07
3
0.02
7
0.02
0*0.
004
0.02
50.
012
0.00
8*0.
42
0.15
LL
D10
2.8
0.7
0.
22
0.04
*
0.11
0.05
*0.
018
0.03
4
0.01
1
0.01
3
0.00
7
0.00
70.
007
0.00
6*0.
001
0.00
1*0.
43
0.14
RL
D0
6.9
2.3
0.
64
0.58
*0.
27
0.35
0.
03
0.16
0.03
8
0.05
0.
084
0.05
*0.
099
0.09
2*0.
001
0.01
30.
38
0.14
RL
D10
3.3
1.7
0.
09
0.11
0.01
6
0.07
20.
018
0.04
9
0.00
7
0.01
9
0.01
0.01
20.
009
0.01
3
0.00
1
0.00
20.
23
0.1
Val
ues
are
mea
ns
SD
(n
6).*
P
0.05
com
pare
dw
ith
zero
by1-
tail
edu
npa
ired
t-te
st.
Equ
atio
n:v
aria
ble
I
ax
by
cz
dxy
eyz
fxz
gxyz
.All
inte
rcep
tsar
esi
gnifi
can
t.
759LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
Tab
leA
3.C
oeffi
cien
tsan
dR
2of
mu
ltip
leli
nea
rre
gres
sion
equ
atio
n
fit
toV
A/
Qan
dP
c O2
dat
afo
rw
hol
e,le
ft,
and
righ
tlu
ng,
resp
ecti
vely
Lu
ng
Pos
itio
nP
EE
PIn
terc
ept
ab
cd
ef
gR
2
VA/Q
Wh
ole
LL
D0
1.21
0.50
0.04
7
0.05
0.04
2
0.03
70.
019
0.02
3
0.00
1
0.00
7
0.00
5
0.00
5
0.00
2
0.00
30.
001
0.00
20.
43
0.10
LL
D10
1.10
0.24
0.01
8
0.03
20.
015
0.03
20.
011
0.01
4
0.00
3
0.00
5
0.00
2
0.00
2*0.
0000
9
0.00
20.
0000
04
0.00
10.
30
0.19
RL
D0
1.08
0.43
0.
008
0.05
60.
035
0.02
*0.
015
0.02
70.
004
0.00
3*
0.00
4
0.00
4
0.00
1
0.00
1*0.
0000
5
0.00
20.
50
0.37
RL
D10
1.25
0.32
0.03
5
0.02
7*0.
003
0.01
20.
014
0.01
7
0.00
2
0.00
4
0.00
1
0.00
30.
0000
8
0.00
20.
0001
0.00
10.
26
0.10
VA/Q
Lef
tL
LD
00.
92
0.38
0.
004
0.04
0.05
3
0.03
*0.
038
0.03
70.
013
0.02
0.
01
0.01
70.
002
0.00
5
0.00
02
0.00
30.
48
0.10
LL
D10
0.99
0.27
0.03
0.01
*0.
03
0.02
*0.
014
0.01
3
0.00
02
0.00
5
0.00
3
0.00
30.
002
0.00
3
0.00
1
0.00
1*0.
46
0.19
RL
D0
1.02
0.53
0.
15
0.06
0.04
2
0.03
60.
009
0.02
60.
013
0.01
5
0.00
1
0.00
9
0.00
3
0.00
40.
002
0.00
1*0.
54
0.20
RL
D10
1.42
0.45
0.
001
0.04
6
0.01
1
0.03
20.
013
0.01
80.
004
0.00
6
0.00
1
0.00
30.
002
0.00
60.
001
0.00
20.
21
0.11
VA/Q
Rig
ht
LL
D0
1.40
0.6
0.
022
0.03
50.
032
0.04
50.
01
0.03
20.
011
0.02
0
0.00
4
0.00
6
0.00
4
0.00
4*0.
001
0.00
20.
31
0.05
LL
D10
1.22
0.24
0.
03
0.04
5
0.01
5
0.02
20.
014
0.00
6*
0.00
2
0.00
5
0.00
1
0.00
20.
0002
0.00
30.
0003
0.00
10.
27
0.15
RL
D0
1.09
0.39
0.01
4
0.02
20.
035
0.02
2*0.
023
0.02
50.
006
0.01
1
0.00
6
0.00
60.
005
0.00
8
0.00
02
0.00
10.
48
0.09
RL
D10
1.13
0.24
0.04
0.02
*0.
012
0.01
20.
017
0.02
0.
003
0.00
7
0.00
2
0.00
30.
003
0.00
3*
0.00
034
0.00
10.
35
0.06
Pr O
2W
hol
eL
LD
011
3.4
6.7
1.30
1.2*
1.15
0.89
*0.
50
0.26
*
0.14
0.19
0.
16
0.15
*
0.06
0.05
10.
03
0.04
0.51
0.15
LL
D10
113.
8
4.2
0.43
0.82
0.45
0.8
0.33
0.23
*
0.08
0.14
0.
074
0.05
4*
0.00
4
0.04
80.
006
0.01
70.
30
0.17
RL
D0
111.
3
8.7
0.
59
1.1
1.43
0.73
*0.
59
0.70
0.20
0.23
0.
21
0.13
0.
013
0.02
80.
003
0.02
90.
57
0.09
RL
D10
113.
8
5.2
0.65
0.45
*0.
06
0.24
0.31
0.33
0.
05
0.07
0.
017
0.05
7
0.01
8
0.03
50.
004
0.01
30.
30
0.14
Pr O
2L
eft
LL
D0
104.
9
120.
21
2.4
2.8
2.6*
0.85
0.67
*0.
50
0.57
0.
42
0.50
0.07
9
0.32
0.
04
0.15
0.52
0.16
LL
D10
112.
3
6.8
0.83
0.77
*1.
07
0.85
*0.
40
0.30
*0.
05
0.13
0.
15
0.13
*0.
02
0.06
7
0.02
0.02
*0.
47
0.22
RL
D0
109.
2
12
0.61
1.0
1.98
1.7*
0.45
0.87
0.13
0.20
0.
20
0.21
0.
04
0.13
0.03
6
0.03
70.
60
0.21
RL
D10
117.
2
5.9
0.
25
0.84
0.
23
0.66
0.19
0.37
0.02
0.09
0.
025
0.05
60.
06
0.09
0.01
8
0.03
10.
24
0.12
Pr O
2R
igh
tL
LD
011
8.6
4.3
0.
25
0.36
0.55
0.57
0.2
0.3
0.17
0.23
0.
087
0.11
0.
065
0.07
80.
013
0.02
80.
35
0.14
LL
D10
117.
9
3.2
0.
75
0.76
0.
4
0.47
0.34
0.16
*
0.04
5
0.09
5
0.01
3
0.04
50.
043
0.06
60.
002
0.00
80.
30
0.15
RL
D0
112.
6
7.3
0.
03
0.4
0.88
0.64
0.67
0.55
0.19
0.16
0.
26
0.16
0.22
0.26
0.
011
0.02
50.
50
0.08
RL
D10
111.
6
4.7
0.90
0.34
*0.
23
0.34
0.44
0.49
0.
075
0.17
0.
054
0.07
40.
06
0.07
0.
007
0.01
90.
38
0.06
Val
ues
are
mea
ns
SD
(n
6).
*P
0.05
com
pare
dw
ith
zero
by1-
tail
edt-
test
.
Equ
atio
n:
Var
iabl
e
I
ax
by
cz
dxy
eyz
fxz
gxyz
.A
llin
terc
epts
are
sign
ifica
nt.
760 LATERAL POSTURE AND PEEP ON VA AND Q
J Appl Physiol VOL 92 FEBRUARY 2002 www.jap.org
-
with 10 cmH2O PEEP and inversion to the RLD pos-ture.
APPENDIX
Table A1 summarizes the x, y, and z coordinate distances(cm) of the center of mass of left, right, and whole lung,relatively to the original coordinate axes (x0, y0, z0) orientedat the edges of the lung. As lung volume increased withPEEP, the coordinate distances between the center of massand original coordinate axes increased. The increase in dis-tance was greatest (50%) in the LLD posture and least(10%) in the RLD posture.
Regional Variation in the Spatial Gradients
The coefficients df of the independent variable xy, yz, andzx in the linear equation (Eq. 5) are measures of the variationof the spatial gradients in any one coordinate along anorthogonal coordinate (Tables A2 and A3). For the whole lungwithout PEEP in the LLD posture, the vertical gradient(Q/x) in blood flow increased linearly with z (coefficient f,0.046)
Q/x0.27 0.046z (A1)
At y 0, the vertical blood flow gradient increase from avalue of 0.59 Q ml1 cm1 in the caudal region at z 7cm to a value of 0.05 in the cranial regions at z 7 cm. Thusthe vertical gradient was maximal in the caudal regions andvanished in the cranial regions. The application of PEEPreduced this z variation of the vertical gradient to 9% (coef-ficient f, 0.005).
Similarly, taking the left lung separately in the LLD pos-ture, the significant coefficient e (0.074, Table 2) impliesthat the dorsal-ventral gradient in Q also varied linearlywith z (x 0)
Q/y 0.26 0.074z (A2)
Thus the dorsal-ventral gradient decreased to 0.26 in thecranial regions (z 7 cm) and became positive (0.78) in thecaudal regions (z 7 cm). Similar variations in otherspatial gradients were present for both Q and VA. Variationsin the gradients in VA were substantial only in the LLDposture without PEEP.
We thank Bill Altemeier and Wayne Lamm for helpful sugges-tions and criticism and Ian Starr, Jenny Souders, Erin Shade,Dowon An, Shen Sheng Wang, and Emily Anderson for excellenttechnical assistance.
This research was supported by National Heart, Lung, and BloodInstitute Grant HL-12174, a fellowship (to H. Chang) from theTri-Service General Hospital at Taiwan, and a sabbatical leave (S. J.Lai-Fook) from the University of Kentucky.
REFERENCES
1. Agostoni E and DAngelo E. Comparative features of thetranspulmonary pressure. Respir Physiol 11: 7683, 1970.
2. Agostoni E, DAngelo E, and Bonanni MV. Topography ofpleural surface pressure above resting volume in relaxed ani-mals. J Appl Physiol 29: 297306, 1970.
3. Albert RK and Hubmayr RD. The prone position eliminatescompression of the lungs by the heart. Am J Respir Crit CareMed 161: 16601665, 2000.
4. Altemeier WA, Robertson HT, and Glenny RW. Pulmonarygas-exchange analysis by using simultaneous deposition of aero-solized and injected microspheres. J Appl Physiol 85: 23442351,1998.
5. Altemeier WA, Robertson HW, McKinney S, and GlennyRW. Pulmonary embolization causes hypoxemia by redistribut-ing regional blood flow without changing ventilation. J ApplPhysiol 85: 23372343, 1998.
6. Amis TC, Jones HA, and Hughes JM. Effect of posture oninter-regional distribution of pulmonary perfusion and VA/Qratios in man. Respir Physiol 56: 169182, 1984.
7. Amis TC, Jones HA, and Hughes JM. Effect of posture oninter-regional distribution of pulmonary ventilation in man. Re-spir Physiol 56: 145167, 1984.
8. Barer GR, Howard P, and Shaw JW. Stimulus-responsecurves for the pulmonary vascular bed to hypoxia and hypercap-nia. J Physiol (Lond) 211: 139155, 1970.
9. Beck KC and Lai-Fook SJ. Pulmonary blood flow vs. gasvolume at various perfusion pressures in rabbit lung. J ApplPhysiol 58: 20042010, 1985.
10. Beck KC and Rehder K. Differences in regional vascularconductances in isolated dog lungs. J Appl Physiol 61: 530538,1986.
11. Beck KC, Vettermann J, and Rehder K. Gas exchange indogs in the prone and supine positions. J Appl Physiol 72:22922297, 1992.
12. Domino KB, Wetstein L, Glasser SA, Lindgren L, MarshallC, Harken A, and Marshall BE. Influence of mixed venousoxygen tension (PvO2) on blood flow to atelectatic lung. Anesthe-siology 59: 428434, 1983.
13. Fowler WS. Lung function studies. II. The respiratory deadspace. Am J Physiol 154: 405416, 1948.
14. Froese AB and Bryan AC. Effects of anesthesia and paralysison diaphragmatic mechanics in man. Anesthesiology 41: 242255, 1974.
15. Gerbino AJ, McKinney S, and Glenny RW. Correlation be-tween ventilation and perfusion determines VA/Q heterogeneityin endotoxemia. J Appl Physiol 88: 19331942, 2000.
16. Glazier JB, Hughes JM, Maloney JE, and West JB. Verticalgradient of alveolar size in lungs of dogs frozen intact. J ApplPhysiol 23: 694705, 1967.
17. Glenny RW, Bernard S, and Brinkley M. Validation of fluo-rescent-labeled microspheres for measurement of regional organperfusion. J Appl Physiol 74: 25852597, 1993.
18. Glenny RW, Bernard S, Robertson HT, and Hlastala MP.Gravity is an important but secondary determinant of regionalpulmonary blood flow in upright primates. J Appl Physiol 86:623632, 1999.
19. Glenny RW, Lamm WJ, Albert RK, and Robertson HT.Gravity is a minor determinant of pulmonary blood flow distri-bution. J Appl Physiol 71: 620629, 1991.
20. Greenleaf JF, Ritman EL, Sass DJ, and Wood EH. Spatialdistribution of pulmonary blood flow in dogs in left decubitusposition. Am J Physiol 227: 230244, 1974.
21. Hlastala MP, Bernard SL, Erickson HH, Fedde MR,Gaughan EM, McMurphy R, Emery MJ, Polissar N, andGlenny RW. Pulmonary blood flow distribution in standinghorses is not dominated by gravity. J Appl Physiol 81: 10511061, 1996.
22. Hlastala MP, Chornuk MA, Self DA, Kallas HJ, Burns JW,Bernard S, Polissar NL, and Glenny RW. Pulmonary bloodflow redistribution by increased gravitational force. J ApplPhysiol 84: 12781288, 1998.





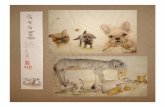







![12. MODULE Postures [OWAS]](https://static.fdocuments.net/doc/165x107/61766639dafcc70db85fc2b3/12-module-postures-owas.jpg)




