SECTION J Under Revision - shoms.ccsd.netshoms.ccsd.net/files/ppt/Sec J Under Revision.pdf · TB...
Transcript of SECTION J Under Revision - shoms.ccsd.netshoms.ccsd.net/files/ppt/Sec J Under Revision.pdf · TB...
Rev. 4/11
SECTION J – Under Revision
CLARK COUNTY SCHOOL DISTRICT
HEALTH SERVICES PROGRAM
CONTAGIOUS AND INFECTIOUS DISEASES
Rev. 4/11
SECTION J CONTENTS
SECTION J – CONTAGIOUS AND INFECTIOUS DISEASES
J-3 Universal Precautions – Guidelines for Handling Body Fluids in the Schools
Hand washing Techniques
Guidelines for Wearing and Removing Gloves
J-3 Blood Glucose Meters
J-4 Equipment Cleaning
J-4 Contagious and Infectious Diseases
Role of the FASA
J-5 Communicable Disease Outbreak See updated individual policy
J-5 Pediculosis/Head Lice
Screening/Referral Procedures
Follow-Up
Documentation
Head Lice Treatments
Alternative Head Lice Treatments
J-8 Protocol for suspected Bed Bugs See updated individual policy
Description of Bed Bugs
Bed Bugs-General Information See updated individual policy
J-13 HIV/AIDS General Information
HIV/AIDS in the School Setting
Guidelines for Effective Home Visit/ Transition to School
Procedures
Home Visit Preparation
Home Visit Checklist
The Visit
Educational Implications
Documentation
Resources Available
J-16 Student to Student Exposure Procedure See updated individual policy
Bodily Fluid Exposure – Definitions
First Aid For Direct Possible Exposure
Parent/Guardian Notification
Documentation
J-17 Student to Employee Exposure
Initiate Appropriate First Aid
Report Incident
J-19 Tuberculosis
TB Medication Protocol (Medication Supplied by SNHD)
TB Medications-Administration
Rev. 4/11
Page J-3 of J-21
UNIVERSAL PRECAUTIONS
GUIDELINES FOR HANDLING BODY FLUIDS
IN THE SCHOOLS
Publication (PUB) 650 – Contagious and Infectious Disease Procedures, provides guidelines for the
management of suspected and/or confirmed contagious and infectious diseases. These procedures guide in the
management of suspected and/or confirmed contagious and infections diseases and are designed to ensure the
health and safety of students and staff. No distinction is made between body fluids from students with known
disease or those from students without symptoms or with an undiagnosed disease. (This publication is available
on InterAct→ District Link→ District Forms→ District Forms and Archives→ Publications)
The Clark County School District Exposure Control Plan-PUB-593 sets forth procedures, engineering
controls, personal protective equipment, work practices, and other methods that are capable of protecting
employees from exposures to bloodborne pathogens. (This plan is available on InterAct→ School Nurse icon→
Forms & Handbooks→ Manuals & Handbooks→ Exposure Control Plan, as well as InterAct→ District Link→
District Forms→ District Forms and Archives→ Publications)
Every health office must maintain a copy of the both the PUB-650 - Contagious and Infectious Disease
Procedures and the PUB-593 - CCSD Exposure Control Plan for reference.
HAND WASHING TECHNIQUES
Frequent hand washing is the single most important means of preventing the spread of infection.
Hands must be washed between contact with each student
The use of bar soap should be discouraged. Pump soap is best
Clean under fingernails
Scrub hands by using friction for at least 10-20 seconds
Rinse hands under warm running water
Dry hands well with paper towels and use paper towel to turn water off
Apply lotion, if available
Hand sanitizer may be used if water and soap is not accessible.
GUIDELINES FOR WEARING AND REMOVING GLOVES
Gloves should be worn to avoid skin contact with blood, blood-soiled items, body fluids, excretions, as well as
surfaces, materials, and objects exposed to them.
Gloves should be used only once, and then discarded after each contact and before leaving the contaminated
area. Proper hand washing techniques should be used after removing gloves. Wearing gloves does not replace
hand washing.
BLOOD GLUCOSE METERS
Many students use the same brand of blood glucose meter. If care is not taken, this can lead to one student
accidentally using another student’s meter. In order to prevent this occurrence, students are to be handed their
blood glucose meter and other personal testing supplies, and be constantly observed by staff while performing
blood glucose testing. Glucose and ketone testing materials or equipment are not to be shared by students at any
time. Student testing equipment and supplies should be stored in individually labeled containers.
Rev. 4/11
Page J-4 of J-21
EQUIPMENT CLEANING
Certain equipment, such as band instruments or gym mats, may be subject to contamination with body fluids. In
order to avoid cross contamination, equipment should be cleaned and appropriately disinfected. The nurse may
be consulted by staff for appropriate cleaning procedures. The nurse should direct staff to consult the Exposure
Control Plan (PUB-593), Risk Management, or their own departmental procedure regarding standard cleaning
procedure.
Additionally, the procedure for cleaning of musical recorders was recently revised. It has been posted on the
Elementary Music Conference under Important Memos. It also may be found on the School Nurse site→
SN Resources, in the drop down menu.
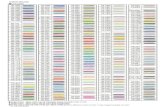
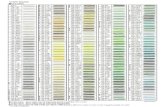
CONTAGIOUS AND INFECTIOUS DISEASES
Health Office protocols for specific contagious diseases can be found in First Aid/Emergency Guidelines for
School Personnel, PUB-648. It is important to limit any discussion of possible diseases to describing what is
observed and not diagnosing.
To prevent the spread of contagious and infectious diseases in the school setting, a student suspected of having
a contagious and/or infectious disease must not be allowed to attend school until the period of communicability
has passed or until appropriate treatment has been obtained. This is mandated by Clark County School District
Regulation 5150, Section V, and PUB-650 - Contagious and Infectious Disease Procedures.
The school nurse may initiate a Student Health Suspension, CCF-662. A copy of this form should be
maintained in the FASA Notebook in the Communicable Disease section. The school administrator/designee is
to be notified if a Student Health Suspension is issued. The FASA may not independently initiate a health
suspension.
The school nurse is required to take appropriate action for all suspected cases of contagious and infectious
diseases. For a description of contagious and infectious diseases, refer to the First Aid/Emergency Guidelines
for School Personnel, PUB-648. Conditions that require exclusion are listed on the Communicable Disease
Chart for Schools and Child Care Centers. These charts are available from the Southern Nevada Health
District (SNHD) and should be prominently displayed in the health office. This information may also be
accessed through the SNHD website www.southernnevadahealthdistrict.org.
If the condition appears suspicious, the parent/guardian must be notified. If indicated, the school nurse will
initiate a medical referral. There are informational sheets dealing with a variety of communicable and infectious
diseases that are available for distribution to parent/guardians. These can be found on the SNHD web site noted
above.
If it is not possible for the parent/guardian to come for their child, the student may remain at school, isolated
from other students. The attendance officer may be used to assist with transportation once appropriate home
supervision has been established. The student may return to school once the school nurse determines that the
student is no longer communicable, under appropriate medical treatment, or no longer considered contagious by
his/her licensed health care provider. Written documentation may be required.
Follow-up should be done on all referrals for contagious and infectious diseases generated by the health office
staff to determine diagnosis and treatment. If a student is noted to have a prolonged absence, the school nurse
should be notified for appropriate follow-up.
The FASA or school nurse are responsible to report communicable diseases noted on the List of Reportable
Diseases (refer to SNHD website for most current list), to SNHD on a case-by-case basis. The school nurse
serves as a resource to school personnel for all cases of suspected or confirmed cases of contagious or infectious
diseases. The school nurse may consult with the SNHD epidemiology department as needed.
Rev. 4/11
Page J-5 of J-21
ROLE OF THE FASA
FASAs, under the supervision of the school nurse, are also required to record communicable diseases on the
Communicable Disease Worksheet (HS). FASAs may record both confirmed and/or suspected cases on the
worksheet. They should note under comments “confirmed, suspected, or reported by parent”. SNHD has
recommended that the Chicken Pox Letter (HS), be sent home at the elementary level to parent/guardians of
students in a class where there is a confirmed case of chicken pox. This is recorded on the Communicable
Disease worksheet maintained in the FASA Notebook.
In the event of an unusual number of students with similar symptoms, the FASA shall notify the school nurse.
COMMUNICABLE DISEASE OUTBREAK
In the event of an outbreak of a communicable disease, notify the Area Nurse Coordinator, the SNHD
Epidemiology Department and the site administrator. An outbreak is considered to be an unusual number of
students with the same or similar symptoms, especially if the students are in the same class, have eaten the same
food, ride the same bus, etc. In the case of chickenpox, an outbreak is considered to be 30% of the school
population (SNHD). An action plan may be developed jointly with CCSD and SNHD personnel. Distribution of
letters to parents/guardians regarding reportable diseases MUST be approved by Director of Health Services in
conjunction with SNHD. It may be necessary to obtain immunization exemption information from SASI to
notify parents/guardians of students who may be exempt from immunizations or may have a health problem that
would be problematic in the event of possible exposure (pregnancy, immune problems, etc.)
Suspected cases of communicable and infectious diseases are to be recorded on the Communicable Disease
Worksheet (HS), which is kept in the FASA Notebook. Both confirmed and/or suspected cases are to be
recorded. In the comment section, it can be noted if the disease is confirmed, suspected, or reported by
parent/guardian.
PEDICULOSIS
HEAD LICE
Head lice infestation is probably one of the most challenging and frustrating problems in schools today. School
personnel are often called on to respond to suspected cases of head lice. Instruction will be provided by the
school nurse to educate school personnel about the signs/symptoms of infestation and Health Services’
procedures. Although head lice infestation is a nuisance, it is not an emergency. It is an infestation which must
be treated at home. School personnel are able to respond to suspected cases of head lice by notifying their
school nurse or FASA. It is imperative that confidentiality and privacy are provided to all students at all
times.
SCREENING/REFERRAL PROCEDURES
If there is a question or evidence of head lice, school personnel are to contact the school nurse and/or FASA.
Under the direction of the school nurse, the FASA and/or office personnel are to:
Complete a parasitic exam and document in Healthmaster
Notify parent/guardian
Send Head Lice Treatment/Suspension Notice, CCF-647 home with the infested student.
Note: suspended students may be allowed to ride the bus home when alternative methods of
transportation (e.g., parent, attendance officer), have been exhausted
Send home Checklist for Getting Rid of Head Lice (HS) (English/Spanish), with the infested
student(s). Optional: send home Head Lice-The Facts (HS), as well
Rev. 4/11
Page J-6 of J-21
Notify school nurse of infested student(s)
Send Head Lice Notice to Parents/Guardians, CCF-646, to parents/guardians of each classmate in the
affected classroom (elementary level only). Notification at the middle school and high school level may
vary depending upon circumstances
The student does not have to be “nit free” to return to school initially; however, repeated infestation must be
brought to the attention of the school nurse. A “no nit” policy may be implemented by the school nurse after the
second infestation within the school year. The Checklist for Students Experiencing Second Head Lice
Infestation (HS) is required to be completed by the school nurse and FASA for the second or subsequent lice
infestation in the school year. This checklist is to be maintained in the FASA Notebook in the Communicable
Disease section. Recurring, problematic cases should be discussed with Area Nurse Coordinator.
FOLLOW-UP
Students can return immediately after head lice treatment is completed. Information regarding treatment must
be provided by the parent/guardian at the time of return. Notification of required second treatments should be
confirmed by a telephone call to the FASA or school nurse after completion. The school nurse or FASA is to
recheck the infested student upon return and one (1) week later for new nits/live lice. Note: Students with
problematic cases may need to be checked daily to ensure eradication. Instruct the parent/guardian to follow the
manufacturer’s recommendations for treatment and follow-up treatment if required.
The school nurse or FASA is not required to check the entire classroom unless there are two or more cases
identified in the same classroom or if repeated cases within the same classroom occur. The custodial staff
should be instructed to vacuum the classroom.
The school nurse or FASA will check siblings, close friends and other students with recent close contact (e.g.,
sleep-overs) who attend the school. If siblings or close contacts are at another school, contact should be made
with the school nurse or FASA at that school so that the student(s) may be checked. The school nurse team may
be called on to assist the site school nurse if extraordinary circumstances exist (multiple classes/entire school
requiring screening). When additional cases are identified, information should be documented in Healthmaster
under parasitic exam and the same procedures followed.
Students should not be absent for more than two days when suspended for treatment. If the student is absent for
more than two days, the FASA should notify the school nurse. At this point, the school nurse should contact the
parent/guardian regarding the reason for the extended absence and offer assistance. The school nurse may
confer with the site administrator to formulate a plan for meeting with the parent/guardian, if the student does
not return. The school nurse should contact the Area Nurse Coordinator if additional assistance is required.
DOCUMENTATION
Record all screenings and referrals in Healthmaster either as an individual screening or a group screening. This
information will be included in any end of month reports provided to the school nurse. The school nurse must
be kept apprised of students with recurrent lice infestations or sensitive situations.
HEAD LICE TREATMENTS
There are many effective over-the-counter shampoos, cream rinses and lice egg looseners that a parent/guardian
can get for treatment of head lice. On occasion, a parent/guardian may choose to get a prescription for a head
lice treatment from their licensed health care provider. The school nurse may assist in locating sources for the
products.
ALTERNATIVE HEAD LICE TREATMENTS
Parents/guardians may choose to use alternative treatments such as mayonnaise, Vaseline, and olive oil. Olive
oil, mayonnaise, and Vaseline are smothering agents. Olive oil is the best smothering agent as it has been
laboratory tested and found to be effective in killing lice. Olive oil has few, if any, allergic properties and is
Rev. 4/11
Page J-7 of J-21
relatively inexpensive. Smothering lice is a safe and effective treatment if done properly. The procedures for
each of the treatments are available (English/Spanish) in the FASA Handbook, Chapter 9, Exhibits.
Rev. 4/11
Page J-8 of J-21
PROTOCOL FOR SUSPECTED BED BUGS
Addendum 8/13
When a bed bug is found, it can be difficult to determine the source. A bed bug found on a person or belongings may have
come from another person. Similar to head lice, it is very important to address the issue with care and sensitivity. There is
no association between cleanliness and bed bug infestations. Anyone can experience an infestation. If a suspected bed bug
is found in school, it should be collected for identification. Other bed bug-like species may be found in schools, including
bat bugs or swallow bugs. To collect the specimen, use a piece of tissue or forceps to place the bug in a plastic bag, double
bag, then tape the outer bag closed. Do not crush the specimen. If the specimen will not be identified immediately, place
the bag in a freezer for several hours to kill the bed bug and prevent escape. Do not mail or transport live specimens, as
they are skilled escape artists. Collect the following information for each specimen:
Date found, name and contact information of the person collecting the specimen, location found (e.g., on a
student, on student’s belongings or on walls or furniture), room number, school name, school principal name and
phone number.
If the specimen is confirmed to be a bed bug, the site administrator and school nurse should be notified and the following
steps are recommended:
1. The classroom or other area where the bed bug was found should be carefully inspected by a custodian.
Inspection should including desks, floors, walls and storage areas for student belongings.
2. A thorough cleaning may be needed including vacuuming with special attention to cracks and crevices in
furniture and equipment, walls and floors, and laundering washables in hot water and drying on the highest heat
setting. Vacuum bags should be sealed in a plastic bag for disposal before moving to another area. Delicate
fabrics can be soaked in warm water and laundry soap for several hours before rinsing. Infested items that cannot
be cleaned or treated with high heat (>120°F for several hours) should be disposed of in sealed plastic bags. If
necessary, the CCSD Facilities Department can perform a steam cleaning, as heat is effective in the eradication of
bed bugs. Additionally, a licensed pest management professional can treat infested areas.
3. If the bed bug was found on a student’s clothing or other belongings, the child’s parent/guardian should be
notified. There is no need to send the student home.
4. Similar to head lice, the school nurse should manage the case, including re-inspecting clothing and belongings
upon return to school and 10 days after the initial determination of bed bugs. Re-inspection by the custodians of
desks and classroom will also be done in 10 days. Student belongings such as backpacks can be isolated in tight-
sealing plastic containers or bags to reduce potential for bed bug dispersal, both at home and in school while the
problem is being resolved.
5. Parents of all children using the room where the bed bug was found should also be notified and provided with
basic information about bed bugs including description, signs and symptoms, strategies to monitor for and
eliminate infestations in homes including cleaning, laundering and specially designed mattress and box-spring
covers that can entrap bed bugs and reduce harborage opportunities. The information should include where to go
for additional help. Refer to “What you need to know about Bed Bugs” (Southern Nevada Health District
publication).
Adult Bed Bug Adult Bed Bug
Exhibit 3
Rev. 4/11
Page J-9 of J-21
DESCRIPTION OF BED BUGS
What are bed bugs?
Bed bugs are reddish-brown, oval, flattened six legged insects with two antennae, which feed on the
blood of people while they sleep. Adult bed bugs are oval, wingless and rusty red colored and have flat
bodies, antennae and small eyes. The dark-colored eyes stand out, and the sides of the collar-like
pronotum curve slightly around the head and is covered with long hairs. Female bed bugs lay their eggs
in secluded areas, depositing one or more eggs per day and hundreds during a lifetime. The eggs are
white, oval and about 1 mm long and are difficult to see on most surfaces without a magnifying glass.
Bed bugs do not fly but can move rapidly over floors, walls, ceilings and other surfaces. They are visible
to the naked eye but often hide in cracks and crevices. They feed on human blood using piercing sucking
mouthparts. They feed at night, hide by day and are shy, and develop from egg to adult in 5-8 weeks.
Although the bite does not hurt at the time, it may develop into an itchy welt similar to a mosquito bite.
Bed bugs do not transmit disease, but they can cause significant itchiness, anxiety and sleeplessness.
Exhibit 4
Rev. 4/11
Page J-10 of J-21
BED BUGS – GENERAL INFORMATION
School nurses are in a unique position to assist students, parents, and staff when bed bug bites or bed bugs are
found. The school nurse will need to determine what actions, if any, are necessary and handle the situation with
sensitivity.
Although bed bugs have nothing to do with cleanliness or socioeconomic status, there is still a stigma associated
with having bed bugs. As a result, parents may be hesitant to admit to having bed bugs, and students may not
want others to know they have an infestation at home.
Bed bug bite symptoms:
1. The most common symptom is a small, round red mark on the skin resembling a bite from a
mosquito,
ant, or flea.
2. Some bites will develop swelling around the site (welt) or blister.
3. Student may complain of itching.
4. Refer to “Pictures of Bed Bug Bites,” (exhibit 5).
Student with possible bed bug bite(s):
1. Treat insect bite per protocol (refer to Pub. 648 and see below).
2. The school nurse may ask the student/parent about exposure to insects.
3. If the school nurse suspects bed bugs, send home “What you need to know about Bed Bugs,”
(Southern Nevada Health District).
Treatment of bites:
1. Cleanse the skin with soap and water.
2. Apply benzalkonium chloride or Bactine and bandage if the area is bleeding from scratching
3. Apply ice pack to relieve itching. Calamine lotion can be applied to intact skin.
4. Inspect bites for secondary infection and, if present, the school nurse will make a medical
referral and the student will be sent home. Signs of secondary infection include:
a. Swelling
b. Pain
c. Heat
d. Pustules
e. Fever
Bed bug found on student:
1. Capture the bed bug, if possible, for identification. Refer to “Protocol for Suspected Bed Bug,”
(exhibit 3).
2. Inspect the student’s clothing and belongings.
3. Place belongings (backpack, jacket, etc.) in a sealed plastic bag or tub.
4. The school nurse will contact the parent/guardian and send information home with student,
“What you need to know about Bed Bugs,” (Southern Nevada Health District) and “Bed Bug
Treatment Verification” (exhibit 8). The student can return to class.
5. Send “Bed Bug Notice to Parent/Guardian” (exhibit 7) and “What you need to know about Bed
Bugs” (Southern Nevada Health District) home with other students in the classroom.
Rev. 4/11
Page J-11 of J-21
6. Maintain student confidentiality.
7. Notify custodial staff to conduct a thorough inspection and vacuuming/cleaning of classroom.
Bed bug found in classroom/other area of the school or suspicion of bed bugs:
1. Infestations of bed bugs in schools are rare.
2. If bed bugs are found in a classroom/other work area or two or more students present with
apparent
bed bug bites from the same classroom, the school nurse will be notified.
3. Health Office personnel will alert custodial staff to assist with area inspection.
4. Health Office personnel will instruct the teacher to place all student belongings in sealed plastic
bags.
5. “Bed Bug Notice to Parent/Guardian” (exhibit 7) and “What you need to know about Bed Bugs”
will be sent home with all classroom students.
6. School nurse will notify school administrator of the need for pest control (CCSD Facilities
Department).
Rev. 4/11
Page J-13 of J-21
HIV/AIDS
GENERAL INFORMATION
HIV/AIDS IN THE SCHOOL SETTING
It is the intent of the CCSD to provide its students with an education consistent with the laws of the State of
Nevada. As a general rule, a student with health problems should be allowed to attend school in a general
education classroom. In the case of a contagious or infectious disease, the District’s responsibility is to consider
the risk of transmission to others as well as the safety of the infected student. The school nurse and FASA play
an important role in ensuring a safe environment for all students. The Director of Health Services must be made
aware of all cases of HIV/AIDS in the school setting. Refer to PUB-650 – Contagious and Infectious Disease
Procedures for more information.
STUDENTS INFECTED WITH HIV/AIDS - GUIDELINES FOR EFFECTIVE HOME VISIT AND
TRANSITION TO SCHOOL
When an HIV/AIDS-infected student enrolls in school, the Director of Health Services is informed by the SNHD
and contacts the parent regarding disclosure. Permission is requested to disclose to the school nurse and site
administrator, however the parent/guardian has the option of refusing permission. If the school nurse is notified of a
student with HIV/AIDS, he/she must notify the Director of Health Services.
The school nurse works collaboratively with the Southern Nevada Health District (SNHD) and the Director of Health
Services. The primary role of the school nurse, when aware of the diagnosis, is to develop a health care plan (HCP) to
promote a safe school environment for the infected student, as well as protect the safety of the general school
population. The school nurse serves as a health advocate. The following is a guideline developed to assist the school
nurse in obtaining the necessary health information, developing a health care plan, establishing effective
communication with the family and protecting the privacy of the student and family while ensuring a safe school
environment for the general school population:
PROCEDURES
Be familiar with current HIV/AIDS information and have a basic understanding of the disease process
Be familiar with CCSD policy and procedures for HIV/AIDS-infected students (PUB-650)
Confer with Director of Health Services and/or liaison
Accompany district nurse liaison on home visit
Be familiar with home visit procedures
HOME VISIT PREPARATION
Set up individual folder
Gather necessary forms
Rev. 4/11
Page J-14 of J-21
Bring student’s immunization record
Bring student’s schedule or teacher information
Know how many absences the student has
Know current grades, school problems
Know if student is special education or general education
Confirm visit and time
THE VISIT
Dress professionally, wear ID, introduce yourself, have business card
Establish confidentiality; explain purpose of visit
Discuss who will be informed of student’s health status
Develop health care plan with parent/guardian
Discuss other health issues/concerns
Discuss student’s knowledge of disease process, transmission, etc.
Discuss academic and attendance concerns, if any, and determine if student needs any accommodations
or Supplemental Home Services
Gather pertinent medical information:
Current health status
Last medical evaluation, T-cell count
Medications
Current physician(s)
Recent hospitalizations
Immunization exemption, if any
EDUCATIONAL IMPLICATIONS
Teacher education, sharing HCP, and disclosure information as determined by parent and/or student
Staff development, bloodborne pathogen training
Student conference – Provide health education/counseling as necessary
Monitor school attendance
Supplementary Home Services Program in place, if needed
Ensure privacy of health records, notes or other documents
DOCUMENTATION
Home Visit Checklist
HS-78: Immunodeficiency - Health Information Supplement
CCF-503: Authorization to Release Confidential Information
PUB-650: Contagious and Infectious Disease Procedures
Supplementary Home Services Referral
Section 504 Referral/Accommodation Plan
CCF-529: Homebound Program Application for General Ed Students
HS-80: Medical Alert-Generic
CCF-649: Nurse Progress Notes
Current Immunization Requirements
Rev. 4/11
Page J-15 of J-21
For parents who will not permit disclosure for any CCSD staff, including the school nurse, a sensitive
Special Problem will not be created or included in HMS
If parents notify the school site, it is the responsibility of the school nurse to forward the information
to the Director of Health Services.
The school nurse will create a Special Problem under the generic “Immunodeficiency Disorder” in the
Special Problem name field. This Special Problem is not to be marked Sensitive and should not contain
specific information related to the diagnosis of HIV/AIDS.
A generic Immunodeficiency Disorder care plan can be created for the student and shared with staff.
For parents wanting full disclosure to school personnel, please contact the Director of Health Services
RESOURCES AVAILABLE
Healthy Schools: Someone at School has AIDS, 2001
The Body, Vaccinations and HIV
Information, Education, Action, CD4 (T-cells) Tests
Introduction to HIV and AIDS Treatment
HIV Treatment & Children: The Issues
Facts about AIDS and HIV
Southern Nevada Health District – Health District Office of AIDS
www.southernnevadahealthdistrict.org
Contagious and Infectious Disease Procedures (PUB-650)
Videos (At Seigle):
Effective Home Visiting Techniques
A Secret Called HIV
Preparing Schools for Children with HIV
Rev. 4/11
Page J-16 of J-21
STUDENT TO STUDENT
EXPOSURE PROCEDURE
Refer to Contagious and Infectious Disease Procedures PUB-650, the section labeled “Guidelines for
Handling Body Fluids”, regarding any exposure to potentially infectious body fluid, or refer to the CCSD
Exposure Control Plan PUB-593. Current copies must be kept in the health office at all times. (Refer to page
one of this handbook section for location of these two manuals)
BODILY FLUID EXPOSURE – DEFINITIONS
1. Exposure incident is defined as a specific exposure to the eye, mouth, other mucous membrane, or
non-intact skin, to blood or other potentially infectious materials by punctures, human bites and
abrasions.
2. The body fluids of all persons should be considered to contain potentially infectious agents. The
term body fluids includes blood, semen/vaginal secretions, urine, vomit, drainage (e.g., nasal
discharge) and saliva.
3. No distinction is made between body fluids from students with a known disease or those from
students without symptoms or with an undiagnosed disease.
FIRST AID FOR DIRECT POSSIBLE EXPOSURE
1. Hands and other affected skin areas should be routinely washed with soap and water immediately
after direct contact has ceased. Note: The area of the body which came in contact with the body fluid
should be carefully examined to see if there is a break in the skin. If there is no true exposure, no
further action is necessary.
2. If the exposure is to a mucous membrane (eyes, nose, mouth), the area should be flushed for 5-15
minutes with clean water.
3. Clothing contaminated with blood or other potentially infectious materials will be handled as little as
possible and with a minimum of agitation. CCSD utilizes Universal Precautions in the handling of
all soiled clothing.
4. Contaminated clothing is to be removed, bagged using universal precautions and sent home with the
student.
5. Adhere to the regular cleaning schedule, referenced in the CCSD Exposure Control Plan
PUB-593, using the appropriate CCSD procedure. Students cannot return to the classroom with any
blood stained clothes. Provide them with clean clothes if available.
PARENT/GUARDIAN NOTIFICATION
1. An on-site school representative should notify the parent/guardian by phone.
2. The Notification of Possible Infectious Contact letter, CCF-635 and CCF-635.1 should be printed
from Healthmaster and should be given to or mailed to parent/ guardian after phone contact is made.
A copy of the parent/guardian letter should be provided to the nurse. Details of the exposure should
be documented in Healthmaster using the global template Body Fluid Exposure. 3. For a true exposure, notify the school nurse that an incident has occurred and parent/guardian contact
has been made.
4. Advise the parent/guardian that he/she may want to seek medical advice concerning evaluation of
possible infectious exposure.
5. Do not give out the name or any information regarding the other student if requested by the
parent/guardian of the exposed student. All information needs to remain confidential.
6. Document information regarding all conversations with the parent/guardian.
7. If the parent/guardian or physician of the exposed person (e.g., the student who was bitten) requests
lab testing or health information on the source person (e.g., the biter):
Refer to Risk Management
Do not release any information to either party
Rev. 4/11
Page J-17 of J-21
Notify Risk Management, the Site Administrator and Area Nurse Coordinator
Do not get involved as a messenger between the parents. Reinforce that the parent should follow up
with their healthcare provider for guidance. Due to HIPAA and FERPA laws we cannot release
information regarding another student, nor request that a student undergo specific testing.
DOCUMENTATION
1. Utilize Bodily Fluid Exposure template in Healthmaster, complete Incident tab, checking “Risk
Management” box.
2. Be sure to include date and time exposure occurred.
3. Complete Notification of Possible Infectious Contact, CCF-635 – generate from Healthmaster
Forms tab. Do not include the name of the other student.
4. Copy of Notification Of Possible Infectious Contact letters should be maintained in the FASA
Notebook.
5. Notification of the Health Services Department should be made by phone for unusual circumstances.
STUDENT TO EMPLOYEE EXPOSURE
School Nurse’s are frequently called upon to handle employee exposure incidents and may assist with providing
first aid. In a non-emergency, direct the employee to follow these procedures. These guidelines are for both the
Employee and anyone (nurse/FASA) providing routine care. When a suspected exposure incident occurs at a
Clark County School District (CCSD) work site, employees will follow these procedures:
INITIATE APPROPRIATE FIRST AID
Clean the area with soap and warm water for 15 minutes. Examine the area of exposure for cuts or
breaks in the skin. If skin is intact, you will most likely not need further evaluation
For eye exposures, flush eye(s) with large amounts of clear water for 5 minutes
For mouth exposures, rinse vigorously with clear water and spit out. Repeat at least 5 times
REPORT INCIDENT
Report the incident to your supervisor (if you supervise students this should be done initially to
ensure supervision continues).
Contact the Employee Health Nurse at 799-0767 as soon as possible after the incident. The incident
must be reported within 24 hours of the occurrence. The Employee Health Nurse will be available to
answer questions, provide information, offer assistance, and determine whether the employee needs
to be seen by a physician. Risk Management personnel, at 799-6877, will assist you in his/her
absence. Report all needle-stick or injuries with a sharp object possibly contaminated with infectious
material to the Employee Health Nurse at 799-0767.
Complete form C-1 (if an emergency this form can be completed as soon as feasible). The supervisor
shall complete the CCF-99 (Supervisor’s Report of Injury). The Office Manager has copies of the
forms, or they can be downloaded from the District Link → District Forms → District Forms and
Archives, scroll to Risk Management – open “GAC-4963 – Notice of Injury…..”
Seek Medical Treatment from the District’s contracted medical provider for exposure follow up as
directed by the Employee Health Nurse. Immediate medical care should be sought if it is determined
that this is a possible exposure. The current provider is the Center for Occupational Health &
Wellness (Dr. Victor B. Klausner) at 801 S Rancho Ste F4, 474-4454 or 9005 S Pecos Rd Ste 2610,
Rev. 4/11
Page J-18 of J-21
474-0472. If the incident happens after 5pm or during weekend hours, report to Southwest Medical
Urgent Care at 888 S Rancho, 877-8600.
o Do not contact the parent/guardian of the student involved in this incident to
request that blood be drawn. That will be the responsibility of the CCSD’s
Employee Health Nurse, if the medical provider has determined the exposure
was valid.
For post-exposure prophylaxis employees should seek care within 2 hours particularly if there is a higher
probability of valid exposure.
The employee may also refer to the CCSD Exposure Control Plan PUB-593, which is located on InterAct →
District Link→ District Forms→ Forms and Archives→ Publications.
For all questions relating to bloodborne pathogen exposures for employees contact the Employee Health
Nurse at 799-0767.
Rev. 4/11
Page J-19 of J-21
TUBERCULOSIS
Tuberculosis (TB) is a communicable/infectious disease caused by the Mycobacterium Tuberculosis. It most
commonly affects the respiratory system, but other parts of the body may become infected. Tuberculosis is
found worldwide. Although the incidence has decreased, it is still prevalent in underdeveloped countries. There
has been an increased incidence of cases in the United States, which may be related to the large influx of
foreign-born individuals.
When a case of TB is confirmed by a positive chest x-ray in a student or staff member, the SNHD contacts the
Director of Health Services. If testing of contacts is advised, the SNHD will coordinate with the Director of
Health Services, the school nurse and site administrator.
Skin tests are the most important diagnostic test to confirm exposure to the tuberculosis germ. The Mantoux
Skin Test, Purified Protein Derivative (PPD), is the standard method used to screen for tuberculosis. The test is
administered to district employees when hired. Confirmation of active disease requires a chest x-ray and sputum
cultures. All employees with a positive reaction are referred to a contracted follow-up facility for a chest x-ray.
TB MEDICATION PROTOCOL
(MEDICATION SUPPLIED BY SOUTHERN NEVADA HEALTH DEPARTMENT)
The site school nurse may be supplied with TB medication for administration to a student when the SNHD
determines that this may be in the best interest of the child for consistency of treatment. The following protocol
should be followed.
I. PURPOSE/APPLICABILITY:
To define the roles and responsibilities of Southern Nevada Health District (SNHD) and the Clark
County School District (CCSD) in meeting the TB medications needs of the clients requiring medication
at school.
II. INDICATIONS:
Children who have been diagnosed with active or latent TB, and require medication during school hours.
III. PROCEDURE:
A. SNHD will determine what clients are appropriate for receiving medication at school:
1. Client has been diagnosed with latent or active TB disease
2. Client is not contagious as determined by:
a. 3 negative sputum’s obtained from patient and patient has been on medication for two weeks
b. Client is being treated for latent TB and is therefore not contagious
B. Establishing School Based Directly Observed Therapy (SBDOT)
1. SNHD will coordinate with the CCSD school nurse to establish a medication regimen at a Clark County
school. The regimen will include how frequently the school will be provided the medication and who will be
bringing the medication to the school.
2. SNHD will have on hand the school medication release form (CCF 643). SNHD staff will obtain from the
parent/legal guardian their authorization for medication assistance during the initial intake of the student for
SBDOT. On this form under “reason for medication” SNHD will cite if this is preventative or treatment for a
medical condition.
Rev. 4/11
Page J-20 of J-21
3. SNHD will make an appointment to visit the school to set up the program and bring the following to the
school nurse:
a. CCF 643 signed by parent/guardian
b. Clinician orders for each medication
c. The medication
d. Direct Observation Therapy (DOT) log to be signed each time the child receives DOT or for each
unsuccessful attempt of DOT with reason, such as absence or refusal of medications
e. Directions for giving the medications
f. Fact sheet with information that includes:
Name of the child’s licensed health care provider
Name of the child’s case manager
Phone number of the TB clinic
Phone number for SNHD clinic contact
Phone number of the parent/guardian
4. SNHD will provide the medication in small plastic bags. There will be only one type of medication in each
bag and each bag must be labeled with:
a. Name of student
b. Name of medication
c. Dosage of each pill and total dosage required
d. Schedule to be given (for example, twice per week with a minimum of one day between dosages or
daily)
e. Time to be given (once per day at lunch time)
f. Name of prescribing licensed healthcare provider
g. Date medication packaged
5. Medications are to be given all at the same time one time a day at lunch time
6. If the child cannot swallow the pill, it is to be crushed and mixed with juice, syrup or water. SNHD will
provide the juice or syrup if needed.
7. If the student vomits the medication, becomes ill or the medication is dropped, contact the SNHD TB
program for further direction.
8. If the student is absent on his/her scheduled day of administration, the school nurse may adjust the days of
administration to permit the required number of dosages. For example, the student normally receives medication
on a Monday/Thursday rotation and the student is absent on Monday. Designated school staff may administer
the medication on Tuesday and Thursday for that week, upon approval by the school nurse. Medication is not to
be given two days in a row - for example Thursday and Friday; there must be at least one day between doses.
9. CCSD School Nurse must contact the SNHD TB program if the student’s weekly absences prevent the
required number of medication administration days at school and for how long, for example: two weeks over
winter break, or ongoing absences due to the child being sick.
10. Medications must be entered into the school’s documentation system (HMS) and on the monthly DOT form
provided by SNHD. If the student is absent on a medication day, the school nurse or FASA will keep the
medications on the schedule log until it is given. The medication will show up as an overdue item on the day the
missed dose is given, and the school nurse or FASA will indicate in the comment section that the student was
absent on the due day and document when the medication was actually given.
11. At the end of each month the school nurse will provide the completed DOT log to SNHD
12. If needed, the client’s case manager can contact the school nurse and visit the school to discuss any issues
and assist with problem solving.
IV. QUALITY ASSURANCE
A. At the end of treatment an evaluation will be completed by the school nurse which will include:
Rev. 4/11
Page J-21 of J-21
1. Reports of success and barriers to DOT related to the client, the client’s family, school environment,
and the DOT procedure itself
2. The evaluation will be maintained and reviewed by management for QA purposes
B. Review and update protocol annually and revise as indicated based on current recommendations.
C. Provide in-service education to staff on initial orientation for new employees and as necessary.
TB MEDICATIONS-ADMINISTRATION
Rifampin Oral; this medication is best taken on an empty stomach with at least 8 ounces of water 1 hour before
or 2 hours after meals, or as directed
Pyrazinamide Oral: take by mouth with or without food, usually once daily or twice weekly, or as directed
Ethambutol Oral: take with or without food, usually once daily or as directed. May sometimes be taken twice
weekly
Priftin Oral: take with food, usually once or twice weekly or as directed. Taking with food will help decrease
side effects of stomach upset, nausea and vomiting, and help increase absorption of medication
Cycloserine Oral: take with or without food, usually twice daily or as directed
Levofloxacin Oral: take with or without food, usually once daily or as directed. Drink plenty of fluids while
taking this medication, unless otherwise directed
Moxifloxacin Oral: take with or without food, usually once daily or as directed