RUSH-GI Bleeding
-
Upload
mark-price -
Category
Documents
-
view
44 -
download
1
description
Transcript of RUSH-GI Bleeding
Slide 1 of 21
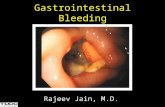
RUSH-GI BleedingArie E Pelta, MD FACS FASCRS
Kaplan Medical CenterDepartment of General Surgery
Colon & Rectal Surgery
Slide 3 of 21
Risk Factors for Morbidity and Mortality in Acute
Gastrointestinal Hemorrhage Age >60 yr
Comorbid disease
Renal failure
Liver disease
Respiratory insufficiency
Cardiac disease
Magnitude of the hemorrhage
Systolic blood pressure <100 mm Hg on presentation
Transfusion requirement
Persistent or recurrent hemorrhage
Onset of hemorrhage during hospitalization
Need for surgery
Slide 5 of 21
Common Causes of Upper Gastrointestinal Hemorrhage
NONVARICEAL BLEEDING* PORTAL HYPERTENSIVE BLEEDING[†]
30%-50% Peptic ulcer disease Gastroesophageal varices >90
15%-20% Mallory-Weiss tears
Hypertensive portal gastropathy, <5
10%-15% Gastritis or duodenitis
Isolated gastric varices, rare
5%-10% Esophagitis
5% Arteriovenous malformations
2% Tumors 5% Others
Slide 10 of 21
Indications for Surgery in Gastrointestinal Hemorrhage
Hemodynamic instability despite vigorous resuscitation (>6 U transfusion)
Failure of endoscopic techniques to arrest hemorrhage
Recurrent hemorrhage after initial stabilization (with up to two attempts at obtaining endoscopic hemostasis)
Shock associated with recurrent hemorrhage
Continued slow bleeding with a transfusion requirement >3 U/day
Slide 12 of 21
A, Gastric antral vascular ectasia (GAVE) can be seen in the gastric antrum, giving the stomach a watermelon
appearance. B, APC therapy of a GAVE. C, Post-therapy appearance of the GAVE.
Slide 15 of 21
LGIBCOLONIC BLEEDING*
SMALL BOWEL BLEEDING[†]
30%-40% Diverticular disease
Angiodysplasias
5%-10% Ischemia
Erosions, ulcers (e.g., from potassium, NSAIDs)
5%-15% Anorectal disease
Crohn's disease
5%-10% Neoplasia
Radiation
3%-8% Infectious colitis
Meckel's diverticulum
3%-7% Postpolypectomy
Neoplasia
3%-4% Inflammatory bowel disease
Aortoenteric fistula
3% Angiodysplasia
1%-3% Radiation colitis, proctitis
1%-5% Other 10%-25% Unknown
Slide 21 of 21
1) A 50 yo pt is brought to ED with retching followed by
hematemesis
A. Treatment is by balloon tamponadeB. Bleeding often stops spontaneouslyC. It is caused by vomitingD. There is air in the mediastinumE. Diagnosis is made by physical examination
Slide 22 of 21
1) A 50 yo pt is brought to ED with retching followed by
hematemesis (B.)
A. Treatment is by balloon tamponade arterial bleed worse with ballon cause perfororationB. Bleeding often stops spontaneously – 1929 Mallory and Weiss. Tx: gastrotomy and oversew; endoscopic inject epi/cauteryC. It is caused by forceful vomiting against closed cardiaD. There is air in the mediastinumE. Diagnosis is made by endoscopic examination
Slide 23 of 21
2) With regard to hemorrhage complicating duodenal ulcer,
which is true ?
A. It is a more common common complication of DU than is perforationB. Endoscopic treatment before operation decreases mortalityC. Endoscopic treatment decreases the need for operation D. Operative management is indicated only if endoscopic treatment failsE. Operative management should not include an acid-reducing procedure
Slide 24 of 21
2) With regard to hemorrhage complicating duodenal ulcer,
which is true ? (A.)
A. It is a more common common complication of DU than is perforation – melena/hematemesis; eroded GDUB. Endoscopic treatment before operation decreases mortalityC. Endoscopic treatment decreases the need for operation D. Operative management is indicated only if endoscopic treatment fails – active arterial spurting/visible vessel predict recurrent bleedE. Operative management should not include an acid-reducing procedure – suture ligate GDA vessels. Truncal vagotomy + pyloroplasty; parietal cell vagotomy + antrectomy
Slide 25 of 21
3) Concerning “stress” bleeding from acute erosive gastritis, which of the
following statements is true ?A. Prophylactic treatments with H2 blockers and anatacids are equally effectiveB.The incidence of such bleeding has been decreasingC. The site of hemorrhage is most often in the antrumD. There is minimal recurrent bleeding after treatment by oversewing of bleeding sites, vagotomy, and pyloroplastyE. Effective surgical treatment necessitates total gastrectomy
Slide 26 of 21
3) Concerning “stress” bleeding from acute erosive gastritis, which of the following statements is true ? (B.)
A. Prophylactic treatments with H2 blockers and anatacids are equally effective antacids best titrated to gastric pH; sucralfate works in acid environmentB.The incidence of such bleeding has been decreasingC. The site of hemorrhage is most often in the antrum. - proximal fundus D. There is minimal recurrent bleeding after treatment by oversewing of bleeding sites, vagotomy, and pyloroplasty – superficial bleedingE. Effective surgical treatment necessitates total gastrectomy – only IF not controlled by vagotomy and pyloroplasty
Slide 27 of 21
4) Concerning Mallory-Weiss syndrome, which of the following
statements is true ?
A. It is a complication of GE refluxB. It involves esophageal rupture near the GE junctionC. Profuse hemorrhage is the most common manifestationD. Bleeding can generally be managed medically E. Vagotomy is indicated for patients requiring surgical treatment
Slide 28 of 21
4) Concerning Mallory-Weiss syndrome, which of the following
statements is true ? (D.)
A. It is a complication of GE reflux retchingB. It involves tear mucosa submucosa GE jct esophageal rupture near the GE junction. Tear gastric side lesser curveC. Profuse hemorrhage is 10% the most common manifestationD. Bleeding can generally be managed medically E. Vagotomy is indicated for patients requiring surgical treatment – oversew site of tear no acid reducing operation
Slide 29 of 21
5) With regard to Meckel’s diverticula, which of the following
statements are true ?
A. They are found in various anatomic forms and clinical presentations in 50% of the populationB. They are true diverticulaC. All can be visualized on technetium 99m pertechnetate (99mTc) scansD. Most complications occur in the elderlyE. Diverticulitis is the most common complication
Slide 30 of 21
5) With regard to Meckel’s diverticula, which of the following
statements are true ? (B.)
A. They are found in various anatomic forms and clinical presentations in 50% 2% of the populationB. They are true diverticula – antimesenteric border 50cm from IC valve, band to umbilicusC. Some All can be visualized on technetium 99m pertechnetate (99mTc) scans – ectopic gastric mucosa peptic ulcer and bleedD. Most complications occur in the elderly pediatricsE. Diverticulitis bleeding, intussusception, obstruction are is the most common complication – diverticulitis is the least complication. Tx: diverticulectomy for diverticulitis; SBR for bleeding. NO prophylactic diverticulectomy for incidental finding unless gastric mucosa or narrow neck
Slide 31 of 21
6) Which is true regarding capsule endoscopy of the SB ?
A. It is a simple, complication free, outpatient procedure that allows examination of the entire length of small intestineB. Capsule endoscopy is not well tolerated by pts since the capsule is attached to a thin wire externalized through the nose to power the device and transmit imagesC. Capsule endoscopy of the SB may be completed in 1 dayD. The capsule endoscope is reusableE. Endoscopic images are viewed using existing endoscopic imaging systems
Slide 32 of 21
6) Which is true regarding capsule endoscopy of the SB ?
A. It is a simple, complication free, outpatient procedure that allows examination of the entire length of small intestine – 1.cm in diameter can cause SBOB. Capsule endoscopy is not well tolerated by pts since the capsule is attached to a thin wire externalized through the nose to power the device and transmit imagesC. Capsule endoscopy of the SB may be completed in 1 day - reach colon in 7hrsD. The capsule endoscope is not reusableE. Endoscopic images are viewed using existing endoscopic imaging systems
Slide 33 of 21
7) Which of the following is true regarding SB enteroscopy ?
A. Capsule endoscopy has replaced push enteroscopy in the evaluation of the SBB. Capsule endoscopy is available only in specialized centers participating in clinical trialsC. Intraoperative enteroscopy is a simple, safe technique that eliminates the need for the less sensitive technique of capsule endoscopyD. Push enteroscopy is more sensitive and specific than capsule endoscopy in the area that can be examined by push enteroscopy
Slide 34 of 21
7) Which of the following is true regarding SB enteroscopy ? (D.)
A. Capsule endoscopy has replaced push enteroscopy in the evaluation of the SB – enteroscopy only examine 50cm from prox or distal direction miss central SBB. Capsule endoscopy is available only in specialized centers participating in clinical trialsC. Intraoperative enteroscopy is a simple, safe technique that eliminates the need for the less sensitive technique of capsule endoscopy - laparotomyD. Push enteroscopy is more sensitive and specific than capsule endoscopy in the area that can be examined by push enteroscopy
Slide 35 of 21
8) Which 2 of the following are the most common causes of massive
colonic bleeding ?
A. Cancer B. UCC. DiverticulosisD. DiverticulitisE. Angiodysplasia
Slide 36 of 21
8) Which 2 of the following are the most common causes of massive
colonic bleeding ?
A. Cancer – occult bleedB. UC – mild bleedingC. **Diverticulosis ** – ruptured vasa rectaD. Diverticulitis – mild bleedingE. Angiodysplasia – equal frequency with diverticulosis. Aging, intramural muscular hypertrophy obstructs the submucosal veins cause dilatation and bleed
Slide 37 of 21
9) A 69 yo M admitted having 3 maroon colored stools. On arrival he passes more bloody stool
and clots. He is pale, orthostatic, and tachycardic. NGT aspirate are bilious. After resuscitation, which is the most appropriate
initial test ?
A. Angiography B. Nuclear medicine RBC scanC. Rigid proctoscopy D. Colonoscopy E. BE
Slide 38 of 21
9) A 69 yo M admitted having 3 maroon colored stools. On arrival he passes more bloody stool
and clots. He is pale, orthostatic, and tachycardic. NGT aspirate are bilious. After resuscitation, which is the most appropriate
initial test ? (C.)
A. Angiography – 1 ml/min. #1SMA most bleeds R colon, #2 IMA , #3 celiac. Embolize, 25% rebleed, 5% ischemia/infarction. Vasopressin intra-arterial, cause arrythmia; when stop 30% rebleed.B. Nuclear medicine RBC scan – sulfur colloid cleared rapid. Technetium detect 0.1 ml/min can repeat scanC. Rigid proctoscopy – anorectal source, UC mucosaD. Colonoscopy – not use when bleed briskly. No bowel prepE. BE – barium will obscure angio; not show bleeding
Slide 39 of 21
With regard to LGIB. Match L column with R.
A. 50% cases bleed Right colonB. Bleeding is arterial and severeC. After 1st episode, rate of recurrent bleed is 25%D. Extravasation of dye during angio can be seen in MOST casesE. Total colectomy is the procedure of choice
a. Diverticulosisb. Angiodysplasia c. Both d. Neither
Slide 40 of 21
With regard to LGIB. Match L column with R.
A. 50% cases bleed Right colon – (c) 80% of tics in sigmoid but R side bleeds moreB. Bleeding is arterial and severe – (a). Angiodyslasia is Venous.C. After 1st episode, rate of recurrent bleed is 25% - (c) rebleed after 2nd episode is 50%. Angiodysplasia 85% rebleedD. Extravasation of dye during angio can be seen in MOST cases – (a) angiodysplasia extravasate only 10%. Dense slowly emptying vein, vascular tuft, early filling vein E. Total colectomy is the procedure of choice – (d) prefer limited resection
a. Diverticulosisb. Angiodysplasia c. Both d. Neither